Abstract
Background
Selection of the best lymph node for dissection is a controversial topic in clinical stage-I non-small cell lung cancer (NSCLC). Here, we sought to identify the clinicopathologic predictors of regional lymph node metastasis in patients intraoperatively diagnosed with stage-I NSCLC.
Methods
A retrospective review of 595 patients intraoperatively diagnosed as stage I non-small-cell lung cancer who underwent lobectomy with complete lymph node dissection was performed. Univariate and multivariable logistic regression analysis was performed to determine the independent predictors of regional lymph node metastasis.
Results
Univariate logistic regression and multivariable analysis revealed three independent predictors of the presence of metastatic hilar lymph nodes, five independent predictors for lobe specific mediastinal lymph nodes, two independent predictors for lobe nonspecific mediastinal lymph nodes and two independent predictors for skipping mediastinal lymph nodes.
Conclusions
A complete mediastinal lymph node dissection may be considered for patients suspected of nerve invasion and albumin (> 43.1 g/L) or nerve and vascular invasions. Lobe-specific lymph node dissection should probably be performed for patients suspected of pulmonary membrane invasion, vascular invasion, CEA (> 2.21 ng/mL), and tumor (> 1.6 cm) in the right lower lobe or mixed lobes. Hilar lymph node dissection should probably be performed for patients suspected of having bronchial mucosa and cartilage invasion, vascular invasion, and CEA (> 2.21 ng/mL).
Similar content being viewed by others
Background
Patients diagnosed with stage-I non-small cell lung cancer (NSCLC) are most likely to be cured by surgical radical resection. Lymph node dissection is an important part of this procedure that can improve the prognosis of the patients in stage-I [1]. However, selection of the best strategy for lymph node dissection remains controversial.
In general, lymph nodes with short-axis diameters of > 1 cm as seen on CT scan are considered by the radiologists to represent metastasis when other reasons causing lymph node enlargement, such as chronic inflammation and tuberculosis, are excluded. Unfortunately, the diagnostic accuracy of CT scan for the preoperative lymph node stage is only 45–79% [2,3,4,5,6]. Also, 12–17% of patients pathologically diagnosed as N2 are preoperatively considered as N0. Skipping metastasis is also found in a part of these patients, as their CT scan results revealed lymph nodes with short-axis diameters of < 1 cm [4, 5, 7]. With technological developments, many methods, such as positron emission tomography, mediastinoscopy, and endoscopic ultrasound-guided fine-needle aspiration, are used to make accurate diagnosis when the surgeon ambiguously confirms preoperative lymph node metastasis. However, owing to the invasive nature of the procedure and the associated expenses, these diagnostic methods could not be routinely used for screening patients with clinical stage-I disease. Also, these procedures yield a considerable number of false-negative results and complications [8,9,10].
Although systematic nodal dissection can guarantee an accurate pathological nodal (pN) staging with a sufficient quantity of lymphatic tissue, the occurrence of postoperative complications will increase. For early stage patients, getting accurate patterns of lymph node dissection will decrease the postoperative complications and speed-up the patient recovery.
Regional lymph nodes attract attention for less invasive intraoperative lymph node dissection in early stage patients. We can classify the lymph nodes into four regional lymph nodes: Interlobar lymph node, Hilar lymph nodes, Lobe-specific mediastinal lymph nodes and Lobe non-specific mediastinal lymph nodes. Skipping mediastinal metastasis is defined as the metastasis of lobe nonspecific mediastinal lymph nodes, and it is confirmed pathologically by the absence of lobe specific mediastinal lymph node metastasis. The concept of lobe specific mediastinal lymph node is based on the lobe specificity of the lymphatic spread, and the characteristic lymph nodal metastasis patterns could be derived from different primary tumor locations [11, 12]. Surgeons can design an accurate strategy for lymph node dissection according to the regulation of regional lymph node metastasis.
However, each patient exhibits different clinical and pathological characteristics. Several studies have demonstrated that the incidence of lymph node metastasis differs according to individual clinical parameters and histologic components within the tumor [13,14,15,16,17]. This patient heterogeneity finally affects the pattern of regional lymph node metastasis in early stage lung cancer.
The goal of this study was to identify the clinicopathologic characteristics that could predict the differences in metastasis among the various regional lymph nodes and to discuss the patterns for patients intraoperatively diagnosed with stage-I NSCLC. These clinicopathologic predictors will probably provide surgeons with useful information to select the appropriate lymph node dissections, especially for early stage patients.
Methods
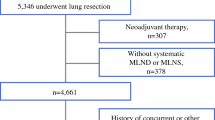
Patient selection
A total of 595 patients who consecutively underwent surgical resection for primary lung cancer at our hospital from January 2015 to December 2017 were reviewed retrospectively. The records of patients intraoperatively diagnosed with stage-I NSCLC who underwent lobectomy or segmentectomy with complete lymph node dissection as per the nomenclature were selected for this study. All patients met the criteria for stage-I NSCLC based on the new International Staging System for NSCLC (National Comprehensive Cancer Network (NCCN) Guidelines Version 3.2014: Staging Non-Small Cell Lung Cancer) [12]. We excluded patients who exhibited any one of the following conditions: 1) preoperative tumor size > 4 cm and lymph node > 1 cm at the largest diameter on CT imaging or evidence of distant metastasis; 2) preoperative chemotherapy or radiotherapy; 3) previous or coexistent tuberculosis or malignant disease; 4) complete lymph node dissection that did not meet the current standards (i.e., all lymph node stations, including right-hand stations 2–4 and 7–9 and left-hand stations 2–9); 5) synchronous lung cancers, or 8) intraoperative frozen rapid pathological results depicting tumor size > 4 cm in the largest diameter.
Patients were preoperatively assessed with chest X-ray, chest and upper abdominal CT scan, brain magnetic resonance imaging, and bone scintigraphy. CT scan was used for preoperative N-staging. The approach for primary lung cancer resection was video-assisted thoracic surgery.
Tissue specimens contained pulmonary nodules and lymph nodes. Pulmonary nodules were analyzed using rapid frozen section in the pathology department of our medical center. The remaining nodules and lymph nodes were fixed using 10% formalin, and conventional formalin-fixed, paraffin-embedded pathological tests were performed.
Statistical analysis
The baseline patient characteristics were summarized in percent for categorical variables. The significance of associations with the outcome of lymph nodal metastases was first evaluated using a univariate logistic analysis (P < 0.20). These significant variables were further analyzed by multivariable analysis as independent predictors for lymph node metastasis (P < 0.05). Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated. Statistical analyses were performed using STATA software, release 13.
Results
Patient characteristics
A total of 595 patients intraoperatively diagnosed with stage-I NSCLC were included in this study. Table 1 displays the patient demographics and clinical characteristics. The mean age was 60 years (range 25–87 years). Among the patients, 304 (51.1%) patients had a maximum tumor diameter of ≤1.6 cm and 284 (47.7%) had a diameter of > 1.6 cm. The tumor originated in the right upper lobe in 181 patients (30.4%), right middle lobe in 28 (4.7%), right lower lobe in 84 (14.1%), left upper lobe in 135 (22.7%), left lower lobe in 87 (14.6%), ipsilateral mixed lobes in 48 (8.1%), and bilateral mixed lobes in 26 (4.4%). Histologically, the tumors in 442 patients (74.3%) were identified as adenocarcinoma, in 62 (10.4%) as squamous cell carcinoma, in 73 (12.3%) as in situ adenocarcinoma, and in 16 (2.7%) as others. The tumor differentiation included stage-I (125 patients, 21.0%), I–II (82 patients, 13.8%), II (139 patients, 23.4%), II–III (137 patients, 23.0%), and III (61 patients, 10.3%). Pulmonary membrane invasion was present in 58 patients (9.7%), bronchial mucosa and cartilage invasion in 54 (9.1%), vascular invasion in 44 (7.4%), and nerve invasion in 13 (2.2%). The number of patients with CEA ≤ 2.21 ng/mL was 253 (42.5%) and > 2.21 ng/mL was 254 (42.7%); albumin ≤43.1 g/L was 289 (48.6%) and > 43.1 g/L was 288 (48.4%).
Association of Individual clinicopathologic characteristics with metastasis of different regional lymph nodes
For the interlobar lymph node, univariate analysis showed that sex (OR = 1.95, 95% CI 0.88–4.30; P = 0.098, male patients 9.0% and female patients 4.8%), maximum diameter of the tumor (OR = 2.75, 95% CI 1.19–6.36; P = 0.018, > 1.6 cm 10.0%, ≤1.6 cm 3.9%), position (P < 0.0001, right lower lobe 26.2%, left lower lobe 9.0%, and bilateral mixed lobes 11.8% were higher than the other lobes), pulmonary membrane invasion (OR = 2.88, 95% CI 0.98–8.47; P = 0.055, present 12.5% and absent 4.7%), bronchial mucosa and cartilage invasion (OR = 2.81, 95% CI 1.07–7.40; P = 0.036, present 15.4% and absent 6.1%), vascular invasion (OR = 2.23, 95% CI 0.72–6.88; P = 0.164, present 13.3% and absent 6.5%), CEA (OR = 4.61, 95% CI 1.53–13.91; P = 0.007, > 2.21 ng/mL 9.9% and ≤ 2.21 ng/mL 2.3%), and albumin (OR = 0.27, 95% CI 0.11–0.64; P = 0.003, ≤43.1 g/L 11.3% and > 43.1 g/L 3.3%) were the 8 significant risk factors associated with metastasis (Table 2).
In the case of hilar lymph node, univariate analysis exposed that sex (OR = 1.83, 95% CI 1.06–3.16; P = 0.029, male patients 16.4% and female patients 9.7%), maximum tumor diameter (OR = 5.42, 95% CI 2.68–10.97; P < 0.0001, > 1.6 cm 19.9% and ≤ 1.6 cm 4.4%), position (P = 0.122, right lower lobe 19.1%, right middle lobe 25.0%, and ipsilateral mixed lobes 21.2% were higher than the other lobes), tumor differentiation (OR = 6.36, 95% CI 1.95–20.74; P = 0.002, present 16.3% and absent 3.0%), pulmonary membrane invasion (OR = 3.20, 95% CI 1.58–6.47; P = 0.001, present 25.5% and absent 9.6%), bronchial mucosa and cartilage invasion (OR = 5.57, 95% CI 2.94–10.56; P < 0.0001, present 38.5% and absent 10.1%), vascular invasion (OR = 7.68, 95% CI 3.86–15.26; P < 0.0001, present 46.3% and absent 10.1%), nerve invasion (OR = 5.90, 95% CI 1.75–19.95; P = 0.004, present 45.5% and absent 12.4%), CEA (OR = 9.66, 95% CI 3.74–24.90; P < 0.0001, > 2.21 ng/mL 20.1% and ≤ 2.21 ng/mL 2.5%), and albumin (OR = 0.27, 95% CI 0.11–0.64; P = 0.003, ≤43.1 g/L 18.2% and > 43.1 g/L 7.0%) were the 10 significant risk factors associated with metastasis (Table 3).
For the lobe specific mediastinal lymph node, univariate analysis established that sex (OR = 1.97, 95% CI 1.08–3.59; P = 0.028, male patients 11.1% and female patients 6.0%), maximum tumor diameter (OR = 4.76, 95% CI 2.33–9.74; P < 0.0001, > 1.6 cm 14% and ≤ 1.6 cm 3.3%), position (P = 0.096, right lower lobe 16.7% and right middle lobe 14.3% were higher than the other lobes), tumor differentiation (OR = 9.93, 95% CI 2.38–41.37; P = 0.002, present 11.6% and absent 1.3%), pulmonary membrane invasion (OR = 3.95, 95% CI 1.87–8.34; P < 0.0001, present 21.1% and absent 6.3%), bronchial mucosa and cartilage invasion (OR = 4.84, 95% CI 2.41–9.71; P < 0.0001, present 25.9% and absent 6.7%), vascular invasion (OR = 7.49, 95% CI 3.68–15.26; P < 0.0001, present 34.1% and absent 6.5%), nerve invasion (OR = 3.75, 95% CI 0.98–14.33; P = 0.053, present 25.0% and absent 8.2%), CEA (OR = 6.53, 95% CI 2.69–15.82; P < 0.0001, > 2.21 ng/mL 13.8% and ≤ 2.21 ng/mL 2.4%), and albumin (OR = 0.46, 95% CI 0.25–0.85; P = 0.013, ≤43.1 g/L 11.5% and > 43.1 g/L 5.6%) were the 10 significant risk factors associated with metastasis (Table 4).
For the lobe nonspecific mediastinal lymph node, univariate analysis indicated that tumor differentiation (OR = 2.68, 95% CI 0.79–9.11; P = 0.115, present 5.1% and absent 2.0%), bronchial mucosa and cartilage invasion (OR = 3.58, 95% CI 1.36–9.45; P = 0.010, present 11.1% and absent 3.4%), vascular invasion (OR = 7.31, 95% CI 2.93–18.21; P < 0.0001, present 18.2% and absent 3.0%), and nerve invasion (OR = 8.81, 95% CI 2.22–34.93; P = 0.002, present 25.0% and absent 3.6%) were the 4 significant risk factors associated with metastasis (Table 5).
As for skipping mediastinal lymph node, univariate analysis disclosed that age (OR = 0.38, 95% CI 0.10–1.44; P = 0.153, ≤60 2.7% and > 60 0%), sex (OR = 0.39, 95% CI 0.10–1.47; P = 0.162, female patients 2.7% and male patients 1.0%), nerve invasion (OR = 12.60, 95% CI 2.41–65.93; P = 0.003, present 16.7% and absent 1.6%), and albumin (OR = 0.34, 95% CI 0.19–0.62; P < 0.0001, > 43.1 g/L 2.8% and ≤ 43.1 g/L 1.0%) were the 4 significant risk factors associated with metastasis (Table 6).
Multivariable analysis of clinicopathologic characteristics associated with metastasis of different regional lymph nodes
For the interlobar lymph node, multivariate analysis of the 8 risk factors obtained from univariate analysis suggested that none of them were significant predictors of interlobar lymph node metastasis (Table 2).
For the hilar lymph node, multivariate analysis of the 10 risk factors acquired from univariate analysis showed that only bronchial mucosa and cartilage invasion (absent vs. present, OR = 3.11, 95% CI 1.19–8.13; P = 0.021), vascular invasion (absent vs. present, OR = 2.98, 95% CI 1.14–7.81; P = 0.026), and CEA (≤2.21 ng/mL vs. > 2.21 ng/mL, OR = 8.49, 95% CI 2.49–28.97; P = 0.001) were the 3 independent predictors associated with metastasis (Table 3).
For the lobe specific mediastinal lymph node, multivariate analysis of the 10 risk factors resulting from univariate analysis indicated that only the maximum diameter of the tumor (≤1.6 cm vs. > 1.6 cm, OR = 3.18, 95% CI 1.15–8.87; P = 0.026), position (P = 0.019), pulmonary membrane invasion (absent vs. present, OR = 4.60, 95% CI 1.60–13.23; P = 0.005), vascular invasion (absent vs. present, OR = 3.85, 95% CI 1.26–11.78; P = 0.018), and CEA (≤2.21 ng/mL vs. > 2.21 ng/mL, OR = 6.01, 95% CI 1.86–19.44; P = 0.003) were the 5 independent predictors associated with metastasis (Table 4).
For the lobe nonspecific mediastinal lymph node, multivariate analysis of the 4 risk factors obtained from univariate analysis revealed that only vascular (absent vs. present, OR = 4.89, 95% CI 1.78–13.40; P = 0.002) and nerve invasions (absent vs. present, OR = 4.73, 95% CI 1.05–21.35; P = 0.043) were the 2 independent predictors associated with the presence of metastasis (Table 5).
For the skipping mediastinal lymph node, multivariate analysis of the 4 risk factors derived from univariate analysis established that only nerve invasion (absent vs. present, OR = 29.11, 95% CI 3.81–222.61; P = 0.001) and albumin (≤43.1 g/L vs. > 43.1 g/L, OR = 5.09, 95% CI 0.99–26.20; P = 0.051) were the 2 independent predictors associated with the presence of metastasis (Table 6).
Discussion
Evaluation of regional lymph node metastasis is important for surgeons to determine the treatment and prognosis [18]. Accordingly, regional lymph node maps have been created to standardize the assessment of metastasis. In these maps, lymph nodes are labeled using a system of numerical levels and assigned names based on their anatomical location [19, 20]. The International Association for the Study of Lung Cancer (IASLC) lymph node map is employed in the eighth edition of the TNM staging system [21]. According to the sequence of the lymph node map, lung cancer cells initially spread to the ipsilateral interlobar lymph nodes, then to the hilar lymph nodes, and finally to the mediastinal lymph nodes.
The concept of lobe specific mediastinal lymph nodes is based on the lobe specificity of the lymphatic spread [22]. In literature, lobe specific MLNs have been defined as 2R, 3, and 4R for the right upper lobe; 3, 7, and 8 for the right lower lobe; 4 L, 5, and 7 for the left upper lobe; and 4 L, 7, and 8 for the left lower lobe. However, Kotoulasa et al. and Shapiro et al. proposed a simpler pattern. Right upper lobe tumors mainly metastasize to 4R, right middle lobe to 4R and 7, right lower lobe to 7, left upper lobe to 5, and left lower lobe to 7 and 9 [11, 12]. An analysis of the recent literature led to our definitions of lobe specific lymph nodes: 2, 3, and 4 for the right upper lobe; 4 and 7 for the right middle lobe; 7 and 8 for the right lower lobe; 5 and 7 for the left upper lobe; and 7, 8, and 9 for the left lower lobe.
A complete mediastinal lymph node dissection which removes all ipsilateral mediastinal lymph nodes [23], can provide more accurate pathological staging and improved clinical outcomes for some patients. This approach is considered a standard surgical treatment for patients diagnosed preoperatively with mediastinal lymph node metastases. However, complete mediastinal lymph node dissection is not considered a routine surgical treatment for patients with stage-I NSCLC because of the increased incidence of postoperative complications including increase in blood loss, median operative time, total chest-tube drainage and occurrence rate of chylothorax. The rapid pathological results would help surgeons to make decisions about which patterns should be performed; wedge resection, segmentectomy, or lobectomy. However, surgeons do not know which pattern should be chosen for lymph node dissection and we need some guidance from clinical research. Mark Shapiro et al. further demonstrated the importance of lobe specific MLN regarded as sentinel lymph nodes in mediastinal position in the surgical treatment of early stage lung cancer [12]. Each patient exhibits different clinicopathologic characteristics that determine the risk for regional lymph node metastasis in early stage lung cancer. We attempted to identify the risk factors to predict lymph node metastasis and allow surgeons to make appropriate decisions on the extent of the dissection. For some early patients, surgeon can remove regional lymph nodes such as lobe specific MLN that are most likely to contain metastases and avoid unnecessary systemic complete lymph nodes dissection in order to accelerate patients’ postoperative recovery.
First, we used univariate analysis to ascertain the associations between clinicopathologic factors and regional lymph node metastasis. The results disclosed that sex (male patients), maximum diameter of the tumor (> 1.6 cm), position (right lower lobe, left lower lobe, and bilateral mixed lobes), pulmonary membrane invasion, bronchial mucosa and cartilage invasion, vascular invasion, CEA (> 2.21 ng/mL), and albumin (≤43.1 g/L) were the 8 significant risk factors associated with the presence of metastatic interlobar lymph nodes.
Sex (male patients), maximum diameter of the tumor (> 1.6 cm), position (right lower lobe, right middle lobe, and ipsilateral mixed lobes), tumor differentiation, pulmonary membrane invasion, bronchial mucosa and cartilage invasion, vascular invasion, nerve invasion, CEA (> 2.21 ng/mL), and albumin (≤43.1 g/L) were the 10 significant risk factors associated with the presence of metastatic hilar lymph nodes.
Sex (male patients), maximum diameter of the tumor (> 1.6 cm), position (right lower lobe, and right middle lobe), tumor differentiation, pulmonary membrane invasion, bronchial mucosa and cartilage invasion, vascular invasion, nerve invasion, CEA (> 2.21 ng/mL), and albumin (≤43.1 g/L, 11.5%) were the 10 significant risk factors associated with the presence of metastatic lobe specific mediastinal lymph nodes.
Tumor differentiation, bronchial mucosa and cartilage invasion, vascular invasion, and nerve invasion were the 4 significant risk factors associated with the presence of metastatic lobe nonspecific mediastinal lymph nodes.
Age (≤60), sex (female patients), nerve invasion, and albumin (> 43.1 g/L) were the 4 significant risk factors associated with the presence of metastatic skipping mediastinal lymph nodes.
Furthermore, multivariate analysis of these factors identified using univariate analysis suggested that all the risk factors were not significant predictors of interlobar lymph node metastasis.
Only bronchial mucosa and cartilage invasion, vascular invasion, and CEA (> 2.21 ng/mL) were the three independent predictors associated with the presence of metastatic hilar lymph nodes. Therefore, when patients are suspected of having bronchial mucosa and cartilage invasion, vascular invasion, and CEA (> 2.21 ng/mL), hilar lymph node dissection should probably be performed.
Only maximum diameter of the tumor (> 1.6 cm), position (right lower lobe, ipsilateral mixed lobes, and bilateral mixed lobes), pulmonary membrane invasion, vascular invasion, and CEA (> 2.21 ng/mL) were the 5 independent predictors associated with the presence of metastatic lobe specific mediastinal lymph nodes. Hence, when patients are suspected of pulmonary membrane invasion, vascular invasion, CEA (> 2.21 ng/mL), and tumor (> 1.6 cm) in the right lower lobe or mixed lobes, lobe specific lymph node dissection should probably be performed.
Only nerve and vascular invasions were the two independent predictors associated with the presence of metastatic lobe nonspecific mediastinal lymph nodes. Hence, when patients are suspected of nerve and vascular invasions, complete mediastinal lymph node dissection should probably be performed.
Only nerve invasion and albumin (> 43.1 g/L) were the two independent predictors associated with the presence of metastatic skipping mediastinal lymph nodes. Therefore, when patients are suspected of nerve invasion and albumin (> 43.1 g/L), complete mediastinal lymph node dissection should probably be performed.
These results demonstrate the possibility of changes to lymph node metastasis when a tumor invades different tissues. In early-stage metastasis, the tumor invades bronchial mucosa and cartilage, pulmonary membranes, and vascular tissue only. During this stage, the CEA level (> 2.21 ng/mL) is likely to be an important predictor indicating that the tumor began to metastasize from the lymphatic system. Therefore, hilar and lobe-specific mediastinal lymph nodes, which are most likely to become the first metastatic stations, should be surgically removed. In later stages of lymph node metastasis, when the tumor begins to invade vascular and neural tissues, the albumin level (> 43.1 g/L) is likely to be an important predictor that indicates and promotes skip metastasis. When there is an increased possibility of broad mediastinal metastases, a complete mediastinal lymph-node dissection is required to ensure that all suspected metastatic lymph nodes are removed.
However, our study has some limitations. This study was conducted at a single institution with retrospective methods and demonstrated the necessity of further prospective study. Further prospective study with multicenter trial should be performed to comprehensively evaluate clinicopathologic predictors of metastasis of different regional lymph nodes in patients intraoperatively diagnosed with stage-I non-small cell lung cancer.
Conclusions
After a comprehensive analysis of results concerning the different clinicopathologic factors, we conclude that complete mediastinal lymph node dissection should probably be performed for patients suspected of nerve invasion and albumin (> 43.1 g/L) or nerve and vascular invasions; lobe specific lymph node dissection should probably be performed for patients suspected of pulmonary membrane invasion, vascular invasion, CEA (> 2.21 ng/mL), and tumor (> 1.6 cm) in the right lower lobe or mixed lobes; hilar lymph node dissection should probably be performed for patients suspected of having bronchial mucosa and cartilage invasion, vascular invasion, and CEA (> 2.21 ng/mL).
Abbreviations
- CEA:
-
Carcinoembryonic antigen
- CI:
-
Confidence intervals
- CT:
-
Computed tomography
- IASLC:
-
Association for the study of lung cancer
- MLN:
-
Mediastinal lymph node
- NCCN:
-
National comprehensive cancer network
- NSCLC:
-
Non-small-cell lung cancer
- OR:
-
Odds ratio
- pN:
-
pathological nodal
- TNM:
-
Tumor, Node Metastases
References
De Leyn P, Dooms C, Kuzdzal J, Lardinois D, Passlick B, Rami-Porta R, et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg. 2014;45:787–98.
Gdeedo A, Van Schil P, Corthouts B, Van Mieghem F, Van Meerbeeck J, Van Marck E. Prospective evaluation of computed tomography and mediastinoscopy in mediastinal lymph node staging. Eur Respir J. 1997;10:1547–51.
Gupta NC, Graeber GM, Bishop HA. Comparative efficacy of positron emission tomography with fluorodeoxyglucose in evaluation of small (<1 cm), intermediate (1 to 3 cm), and large (>3 cm) lymph node lesions. Chest. 2000;117:773–8.
Prenzel KL, Monig SP, Sinning JM, Baldus SE, Brochhagen HG, Schneider PM, et al. Lymph node size and metastatic infiltration in non-small cell lung cancer. Chest. 2003;123:463–7.
Sioris T, Jarvenpaa R, Kuukasjarvi P, Helin H, Saarelainen S, Tarkka M. Comparison of computed tomography and systematic lymph node dissection in determining TNM and stage in non-small cell lung cancer. Eur J Cardiothorac Surg. 2003;23:403–8.
Steinert HC, Hauser M, Allemann F, Engel H, Berthold T, von Schulthess GK, et al. Non-small cell lung cancer: nodal staging with FDG PET versus CT with correlative lymph node mapping and sampling. Radiology. 1997;202:441–6.
Izbicki JR, Passlick B, Pantel K, Pichlmeier U, Hosch SB, Karg O, et al. Effectiveness of radical systematic mediastinal lymphadenectomy in patients with resectable non-small cell lung cancer: results of a prospective randomized trial. Ann Surg. 1998;227:138–44.
Hermens FH, Van Engelenburg TC, Visser FJ, Thunnissen FB, Termeer R, Janssen JP. Diagnostic yield of transbronchial histology needle aspiration in patients with mediastinal lymph node enlargement. Respiration. 2003;70:631–5.
Annema JT, Veselic M, Versteegh MI, Willems LN, Rabe KF. Mediastinal restaging: EUS-FNA offers a new perspective. Lung Cancer. 2003;42:311–8.
Freixinet Gilart J, Garcia PG, de Castro FR, Suarez PR, Rodriguez NS, de Ugarte AV. Extended cervical mediastinoscopy in the staging of bronchogenic carcinoma. Ann Thorac Surg. 2000;70:1641–3.
Kotoulas CS, Foroulis CN, Kostikas K, Konstantinou M, Kalkandi P, Dimadi M, et al. Involvement of lymphatic metastatic spread in non-small cell lung cancer accordingly to the primary cancer location. Lung Cancer. 2004;44:183–91.
Shapiro M, Kadakia S, Lim J, Breglio A, Wisnivesky JP, Kaufman A, et al. Lobe-specific mediastinal nodal dissection is sufficient during lobectomy by video-assisted thoracic surgery or thoracotomy for early-stage lung cancer. Chest. 2013;144:1615–21.
Yanagawa N, Shiono S, Abiko M, Ogata SY, Sato T, Tamura G. The correlation of the International Association for the Study of Lung Cancer (IASLC)/American Thoracic Society (ATS)/European Respiratory Society (ERS) classification with prognosis and EGFR mutation in lung adenocarcinoma. Ann Thorac Surg. 2014;98:453–8.
Kadota K, Villena-Vargas J, Yoshizawa A, Motoi N, Sima CS, Riely GJ, et al. Prognostic significance of adenocarcinoma in situ, minimally invasive adenocarcinoma, and nonmucinous lepidic predominant invasive adenocarcinoma of the lung in patients with stage I disease. Am J Surg Pathol. 2014;38:448–60.
Ito M, Miyata Y, Kushitani K, Yoshiya T, Mimae T, Ibuki Y, et al. Prediction for prognosis of resected pT1a-1bN0M0 adenocarcinoma based on tumor size and histological status: relationship of TNM and IASLC/ATS/ERS classifications. Lung Cancer. 2014;85:270–5.
Zhang J, Wu J, Tan Q, Zhu L, Gao W. Why do pathological stage IA lung adenocarcinomas vary from prognosis?: a clinicopathologic study of 176 patients with pathological stage IA lung adenocarcinoma based on the IASLC/ATS/ERS classification. J Thorac Oncol. 2013;8:1196–202.
Moon Y, Kim KS, Sung SW, Lee KY, Kim YK, Kang JH, et al. Correlation of histological components with tumor invasion in pulmonary adenocarcinoma. World J Surg Oncol. 2014;12:388.
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The eighth edition AJCC Cancer staging manual: continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging. CA Cancer J Clin. 2017;67:93–9.
Ishikawa S, Suematsu K, Naruke T, Shimozato Y. Lung cancer. Gan No Rinsho. 1967;13:227–38.
Naruke T, Suemasu K, Ishikawa S. Lymph node mapping and curability at various levels of metastasis in resected lung cancer. J Thorac Cardiovasc Surg. 1978;76:832–9.
Rusch VW, Asamura H, Watanabe H, Giroux DJ, Rami-Porta R, Goldstraw P. The IASLC lung cancer staging project: a proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol. 2009;4:568–77.
Riquet M, Rivera C, Pricopi C, Arame A, Mordant P, Foucault C, et al. Is the lymphatic drainage of lung cancer lobe-specific? A surgical appraisal. Eur J Cardiothorac Surg. 2015;47:543–9.
Martini N. Mediastinal lymph node dissection for lung cancer. The memorial experience. Chest Surg Clin N Am. 1995;5:189–203.
Acknowledgements
We thank Dr. Quan Zhu and Dr. Wei-Bing Wu for their constructive suggestions and comments.
Funding
This work was supported by Natural Science Foundation of Jiangsu Province (BK20151589) which provided funds for collection and analysis of clinical data.
Availability of data and materials
We presented raw data within Additional file 1.
Author information
Authors and Affiliations
Contributions
ZF collected, analyzed and interpreted data and ZFX drafted, substantively revised the manuscript. ZY, HCJ, YY, LJ, LQF, ZCX, YXY, YSH, WQG, QXY, and LY participated in collecting clinical data and performed the statistical analysis. WW and CL conceived the study and participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the amended Declaration of Helsinki. The approval of the Ethical Committee of Nanjing Medical University was obtained (project approval no. 2012-SRFA-161). The written informed consent from either the patients or their representatives was waived due to the retrospective nature of this study in accordance with the American Medical Association.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Support file containing the Age (G), cigarettes (0:negative, 1:positive), Alcohol (0:negative, 1:positive), chronic bronchitis (0:negative, 1:positive), diabetes (0:negative, 1:positive), tumor history (0:negative, 1:positive), tumor family history (0:negative, 1:positive), blood type (0:A,1:B,2:O,3:AB), Neutrophil(G), Lymphocyte(G), N/L(G), Platelet(G), Serum Albumin(G), ALP(G), Serum Globulin(G), Al/Gl ratio(G), APTT(G), PT(G), CEA(G), CYFRA211(G), NSE(G), Tumor size(G), Tumor location (0:right upper,1:right middle,2:right lower,3:left upper,4:left lower,5:Ipsilateral), Tumor location(G), Pathology (0:AdCa,1:SqCa,2:Adenocarcinoma in situ,3:other), Pathology(G),Grade (G), Pathological morphology (1:lepidic, 2:Acinar, 3:Micropapillary, 4:Papillary, 5:solid), Pathological morphology(G), Pulmonary membrane invasion (0:negative, 1:positive), Bronchial mucosa and cartilage invasion (0:negative, 1:positive), Vascular invasion (0:negative, 1:positive), Nerve invasion (0:negative, 1:positive), Lobe-specific mediastinal lymph nodes (1:metastasis 0:no metastasis),Lobe non-specific mediastinal lymph nodes (1:metastasis 0:no metastasis), skiping mediastinal lymph nodes (1:metastasis 0:no metastasis),2, 4station(1:metastasis 0:no metastasis),5, 6station(1:metastasis 0:no metastasis),7station(1:metastasis 0:no metastasis),8station(1:metastasis 0:no metastasis), 9station(1:metastasis 0:no metastasis), hilar lymph nodes (10 station)(1:metastasis 0:no metastasis), interlobe lymph nodes (11 station)(1,metastasis 0,no metastasis) described in categorical variables and Age ranges (yrs), number of cigarettes, Tumor size (cm). Neutrophil, Lymphocyte, N/L, Platelet, Serum Albumin, ALP, Serum Globulin, Al/Gl ratio, APTT, PT, CEA, CYFRA211, NSE described in continuous variables. (XLSX 173 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhao, F., Zhen, FX., Zhou, Y. et al. Clinicopathologic predictors of metastasis of different regional lymph nodes in patients intraoperatively diagnosed with stage-I non-small cell lung cancer. BMC Cancer 19, 444 (2019). https://doi.org/10.1186/s12885-019-5632-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-019-5632-2