Abstract
Background
Recently studies have demonstrated that the long non-coding RNA (lncRNA) metastasis associated lung adenocarcinoma transcript 1 (MALAT1) may participate in the development and progression of lung cancer. In this study, we hypothesized that genetic variant of this lncRNA may affect the prognosis of lung cancer patients.
Methods
We conducted a follow-up study for 538 patients with non–small cell lung carcinoma (NSCLC), including 140 early-staged (stage I and II) and 398 advanced staged (stage III and IV) patients. The genetic variant rs3200401 in MALAT1 was then genotyped among this population by using TaqMan assay. The association of this variant with overall survival of these patients was further analyzed.
Results
It was shown that among the advanced lung adenoma patients, subjects carrying rs3200401 CT and CT + TT genotypes had significantly longer median survival time (MST = 29.9, 28.9 vs. 19.3 month, Long-rank P = 0.019 and 0.024, respectively) and decreased death risks [crude HR (95% CI) = 0.65 (0.43–0.98) and 0.64 (0.44–0.95), P = 0.040 and 0.025, respectively], when compared to subjects wtih the MALAT1 rs3200401 CC genotype. However, the beneficial effect of rs3200401 was not seen among early NSCLC and advanced lung squamous cell carcinoma patients. We further tested the TCGA data, and found that a higher expression of MALAT1 was associated with metastatic of advanced lung adenocarcinoma but not with lung squamous cell carcinoma.
Conclusions
The rs3200401 T allele located on the lncRNA MALAT1 was associated with a better survival for advanced lung adenocarcinoma patients, which may offer a novel prognostic biomarker for this patient subgroup. However, these results need to be validated in larger populations of lung cancer and the biological function of this variant still warrants further investigation.
Similar content being viewed by others
Background
Lung cancer was the most common cancer and one of the leading cause of cancer-related death worldwide, and it contributed to 13.0% of new cancer cases diagnosed in 2012 [1]. The non-small cell lung cancer (NSCLC) represents almost 85 to 90% of total diagnosed lung cancer, while lung adenocarcinoma is the most common histological subtype. The 5-year survival rate of advanced NSCLC is less than 5% based on the Surveillance, Epidemiology, and End Results (SEER) Program data [2].
Long non-coding RNAs are RNA genes larger than 200 bps, which do not code for proteins but regulate gene expression and protein synthesis [3]. Several lncRNAs were reported to be associated with tumorigenesis, tumor progression, and tumor metastasis [4–7]. In general, most lncRNAs are expressed at low levels. Metastasis associated lung adenocarcinoma transcript 1 (MALAT1), also known as noncoding nuclear-enriched abundant transcript 2 (NEAT2), is one of the most abundant and highly conserved lncRNAs, indicating its potential functional importance [8]. MALAT1 is broadly expressed in normal human tissues and overexpressed in numerous cancers as well as NSCLC [9]. It has been proposed that MALAT1 can regulate gene expression and alternative splicing. MALAT1 is localized in nucleus speckles at SRSF2 splicing domain in several cell lines and can interact with pre-mRNA-splicing factor SF2/ASF and CC3 antigen [10–14]. In vitro studies revealed that MALAT1 can regulate cell proliferation, migration, and vessel growth [15–17].
MALAT1 was originally identified as a marker for predicting metastasis and prognosis of early-staged NSCLC patients [9, 18]. Many researches also indicated that MALAT1 is linked to other cancer types or diseases as a negative prognosis factor, such as glioma, pancreatic cancer, colorectal cancer, etc. [19–25]. However, the associations between genetic polymorphisms of lncRNA MALAT1 and lung cancer prognosis were less investigated.
In this study, we genotyped the single nucleotide polymorphism (SNP) rs3200401 located in lncRNA MALAT1 and aimed to investigate its association with the survival outcome of 398 advanced NSCLC patients.
Methods
Study patients
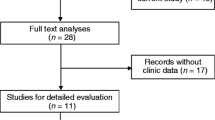
The study enrolled 538 patients who were diagnosed as NSCLC and treated at the Department of Oncology at Wuhan Iron and Steel (Group) Corporation Staff-Worker Hospital between January 2003 and December 2012. Patients who were still alive on December 31, 2013 (132 patients) were considered as censored, and the survival time for each patient was calculated from the date when they were confirmed diagnosed of lung cancer until the date of death or the last follow-up. The demographic data, lifestyle risk factors (e.g. smoking status, drinking), medical history, and clinical features were gathered by interview or from the patients’ medical records. A large part of study patients has been studied and reported in our previous study [26].
SNP selection and genotyping
The NCBI dbSNP database were used to select the SNP of MALAT1 (https://www.ncbi.nlm.nih.gov/snp/). It was indicated by the dbSNP database that there are 16 SNPs located on MALAT1 gene with the MAF > 0.01, however, only rs3200401 had the MAF > 0.10 in all the 1000 Genome, the NHLBI “Grand Opportunity” Exome Sequencing Project (GO-ESP), and Exome Aggregation Consortium (ExAC) projects (https://www.ncbi.nlm.nih.gov/variation/view/) (Additional file 1: Table S1). Thus, to acquire adequate statistical power, the SNP rs3200401 was investigated in the present study, while the other SNPs with MAF < 0.10 were not selected. Genomic DNA samples were extracted from blood cells by using Gentra Puregene Blood Kit (QIAGEN, Hilden, Germany) following manufacturer’s instructions. The MALAT1 polymorphism, rs3200401 C > T, was genotyped by TaqMan assay among all study subjects using ABI 7900HT Sequence Detection System (Applied Biosystems, Waltham, Massachusetts, USA) and each sample was analyzed in duplicate. The primers and probes were purchased from Life Technologies (Catalog No. C___3246069_10). The genotyping call rate was 98.1% and the concordance rate was 100%.
Statistical analysis
Kaplan-Meier analysis and log-rank test were used to assess the associations between survival time and demographic characteristics, clinical features, and MALAT1 rs3200401 genotypes. We use dominant model to assess the association of SNP rs3200401 genotypes and survival outcome of early and advanced NSCLC patients, respectively. The multivariate Cox regression models, with adjustment for age, sex, smoking status, histology, TNM stage, and therapy treatments of surgical resection, chemotherapy, and radiotherapy, were used to estimate the adjusted hazard ratio (HR) and 95% CIs for the effect of MALAT1 rs3200401 genotypes on death risk for NSCLC patients. All data analyses were performed in SPSS software (version 22, IBM SPSS Statistics, IBM Corporation, Chicago, IL). Power analysis was performed by using Power and Sample Size version 13.2 application in SAS (version 9.4, SAS Institute Inc., Cary, NC).
Results
Patient characteristics
The demographic information and clinical features for NSCLC patients were presented in Table 1. Among these patients, a total of 78 early-staged and 328 advanced NSCLC patients were confirmed death of lung cancer until the date of the last follow-up. Among these NSCLC patients, there are 450 males (84%) and 88 (16%) females, with a median age of 66.5 years (range, 40–87). Log-rank test and univariate cox-regression showed that NSCLC patients with age > 65, advanced stage (stage III or IV), and without surgical treatment had lower median survival time (MST) and higher death risks than their counterparts (all log-rank P < 0.05). However, there were no significant effects of smoking, chemotherapy, and radiotherapy on the MST and death risk of these NSCLC patients. The statistical power analysis showed that, as for the SNP rs3200401 (MAF = 0.187) analyzed in this study, it had the statistical power of 0.913 to detect the association with HR = 1.4 by using 398 subjects in the survival analysis.
Patients with age > 65 or with advanced staging had a significantly shorter survival time and higher risk of death when comparing with patients with age ≤ 65 or diagnosed at early stage [MST = 16.4 vs. 29.9 months, log-rank P < 0.001, HR (95% CI) = 1.54 (1.27–1.88); MST = 17.9 vs. 57.6 months, log-rank P < 0.001, HR (95% CI) = 2.43 (1.89–3.12), respectively] (Table 1). In addition, NSCLC patients who underwent surgical treatment had a longer survival time and a lower risk of death [MST = 36.1 vs.17.6 months, log-rank P <0.01, HR (95% CI) = 0.53 (0.43–0.65)] (Table 1). However, there were no significant associations of smoking status, chemotherapy, and radiotherapy (all log-rank P > 0.05) with the survival outcomes among NSCLC patients.
Association of genetic variant rs3200401 with survival outcome among NSCLC patients
The associations between lncRNA MALAT1 rs3200401 genotypes and survival outcome of early-staged NSCLC patients were shown in Table 2. No significant associations were found between rs3200401 genotypes and the MST and death risk of early NSCLC patients, either in adenocarcinoma or squamous cell carcinoma. (Table 2).
Among the advanced NSCLC patients, those carrying MALAT1 rs3200401 CT and rs3200401 CT + TT genotypes have significantly longer MST than those with rs3200401 CC genotype (MST = 22.6, 21.8 vs.15.9 months, and log-rank P = 0.045 and 0.034, respectively) (Table 3). The univariate cox proportional hazard models showed that, when compared to the rs3200401 CC genotype, the rs3200401 CT and CT + TT genotypes were associated with significant lower death risk for advanced NSCLC patients [crude HR (95% CI) = 0.78 (0.61–0.99) and 0.78 (0.61–0.98), P = 0.046 and 0.034, respectively]. But after adjusted by potential confounders, no statistically significant associations were found between CT [adjusted HR (95% CI) = 0.82 (0.64–1.05), P = 0.119] and CT + TT genotypes [adjusted HR (95% CI) = 0.81 (0.64–1.04), P = 0.094] with death risk of advanced NSCLC patients.
We further analyzed the associations of MALAT1 rs3200401 with survival outcomes among advanced patients with lung adenocarcinoma and squamous cell carcinoma separately (Table 3). Compared to advanced lung adenocarcinoma patients carrying the rs3200401 CC genotype, those with rs3200401 CT and CT + TT genotypes had significant longer MST and lower risk of death (MST = 29.9 and 28.9 months vs. 19.3 months, log-rank P = 0.019 and 0.024) [crude HR (95% CI) = 0.62 (0.41–0.93) and 0.65 (0.44–0.95); adjusted HR (95% CI) = 0.65 (0.43–0.98) and 0.64 (0.44–0.95), respectively] (Table 3) (Fig. 1a). However, this effect was not seen among advanced lung squamous cell carcinoma patients (Fig. 1b).
Stratified analysis for advanced NSCLC patients
We then stratified the advanced lung adenocarcinoma and squamous cell carcinoma patients by age, sex, smoking, TNM stage, surgical operation, chemo- or radio-therapy, respectively (Table 4). We found the rs3200401 CT + TT genotype was associated with a decreased death risk at a borderline significance among lung adenocarcinoma patients with age ≤ 65 [HR (95% CI) = 0.59 (0.35–1.00), P = 0.054]) and stage IIIA-IIIB [HR (95% CI) = 0.54 (0.29–1.01), P = 0.053]. No significant associations between rs3200401 genotypes and survival were seen among squamous cell carcinoma patients in each stratum.
Discussion
In this follow-up study for case-only survival analysis, we investigated the association of the genetic variation rs3200401 in lncRNA MALAT1 with the survival outcome of NSCLC patients. We found that among advanced lung adenocarcinoma patients, those carrying MALAT1 rs3200401 CT or CT + TT genotypes had significant longer survival time and decreased death risks than those carrying rs3200401 CC genotype. This finding suggested that rs3200401 C > T variant of MALAT1 might be a potential prognostic biomarker for predicting the survival of advanced lung adenocarcinoma patients.
Metastasis is the major cause of death from lung cancer [27], and MALAT1 was significantly associated with metastasis of early-stage NSCLC patients [9]. The in vitro cell and in vivo animal studies had revealed that the expression level of lncRNA MALAT1 is related to cell migration potential and tumor growth. Increased MALAT1 expression in tumor tissues of NSCLC patients is associated with an unfavorable overall survival [19], while the high expression of MALAT1 in tumor tissues was also found to be associated with an increased risk of metastasis and a poor overall survival among colorectal cancer [21], pancreatic cancer [22], glioma [23], and clear cell renal cell carcinoma [24]. MALAT1 can induce metastasis through various mechanisms. The in vitro siRNA-mediated MALAT1 silencing resulted in impaired lung cancer cell motility by altering the expression levels of cell motility-related genes, such as HMMR at pre-mRNA transcriptional level and CTHRC1, CCT4 and ROD1 at post-transcriptional level [15]. Inhibition of MALAT1 was seen to have an anti-proliferative effect and controls phenotypic switch in endothelial cells, indicating that MALAT1 may regulate angiogenesis and result in metastasis [17, 28]. More researches suggested that upregulated MALAT1 can induce an epithelial-to-mesenchymal transition (EMT) and bladder cancer cell migration [29] and promote brain metastasis [30].
Although MALAT1 expression in lung cancer tissue was reported to be associated with poor prognosis in lung squamous cell carcinoma [19], our findings indicated that the SNP rs3200401 cannot affect the survival outcome of lung squamous cell carcinoma patients. Ji et al. found that the association of MALAT1 with metastasis of NSCLC was distinct among different histological subtypes: MALAT1 expression in metastatic lung adenocarcinoma was several fold higher than in non-metastatic adenocarcinoma, but no significant differences were found between metastatic and non-metastatic lung squamous cell carcinoma patients [9]. We obtained the clinical data and MALAT1 gene expression data from the cancer genome atlas (TCGA) using cBioPortal [31]. A total of 654 patients with primary lung cancer (359 lung adenocarcinoma and 295 lung squamous cell carcinoma) and available MALAT1 expression data from white population were included. Among them, a total of 117 patients were diagnosed at an advanced stage. The demographic data for these advanced NSCLC patients was presented in Additional file 1: Table S2. We found significant higher MALAT1 expression levels in lung adenocarcinoma tissues than in lung squamous cell carcinoma tissues (P <0.001, Fig. 2a). In 75 tumors with advanced lung adenocarcinoma, higher expression levels of MALAT1 were seen in tissues from M1 or Mx patients than those from M0 patients (P = 0.049). However, this difference was not shown in 42 patients with advanced lung squamous cell carcinoma (Fig. 2b). Considering the different characteristics of these two major subtypes of NSCLC, the lncRNA MALAT1 may induce tumor metastasis through different mechanisms between adenocarcinoma and squamous cell carcinoma.
Regarding the biological function for lncRNA MALAT1, it was found to localize to nuclear speckles and interact with serine/arginine-rich (SR) proteins like serine/arginine-rich splicing factor 1 (SRSF1), SRSF2 (SC35) and RNA-binding protein with serine-rich domain 1 (RNPS1) that controls alternative splicing of pre-mRNA, a transcriptional level regulation of gene expression [10, 13, 32–35]. Large studies have reported that genetic polymorphisms on certain genes may affect the susceptibility of lung cancer [36, 37], sensitivity of chemo- or radiotherapy [38–40], and length of survival or prognosis [41–44]. Liu et al. found a borderline significant association between rs619586 in MALAT1 and decreased hepatocellular carcinoma risk [45]. Another study carried out by Gong et al. did not found any association between rs619586 genotype and lung cancer risk, but patients with rs619586 A allele had more chance of response to platinum-based chemotherapy [40]. In this study, we did not investigate the rs619586 of MALAT1 because the dbSNP database suggested it is a low-frequency SNP. Further studies with larger sample sized populations could investigate the low-frequency SNPs of MALAT1 with higher detection power, and the biological functions for the positive variants of MALAT1 also warrant further deep investigation.
The interaction between lncRNA and other molecules was probably determined by its structure rather than by its sequence. The polymorphism within lncRNA sequence may exert its function through alternative splicing of the transcript or lncRNA secondary structure change, resulting in gain or loss of function [46]. The SNP rs3200401 C > T variant locates in the region M of MALAT1 (6008–7011 nt), which is one of the binding sites to SRSF2 [34]. We use lncRNASNP database to predict potential functions of this SNP [47], such as structure change and miRNA-lncRNA interaction. We found that the C > T variation of rs3200401 caused 1.62 kcal/mol minimal free energy (MFE, ΔG) change, which may alter structural features of MALAT1 (Additional file 2: Figure S1), resulting in weaken interaction between MALAT1 and its binding protein SRSF2. MALAT1 can modulate phosphorylation of SRSF2, interact with SR proteins as a “molecular sponge” and influence their stability, and regulate the alternative splicing of pre-mRNAs [10, 13]. SRSF2 and phosphorylated SRSF2 were reported to correlate with aggressive features of lung adenocarcinoma but not with lung squamous cell carcinoma patients [48]. It was biologically possible that SNP rs3200401 C > T variant may cause MALAT1-SRSF2 binding loss, affect phosphorylation of SRSF2, down-regulate phosphorylation of SRSF2, change the alternative splicing of pre-mRNAs, and then alter the expression levels of metastasis associated genes. These effects may result in a lower aggressive feature and a better survival for lung adenocarcinoma but not for squamous cell carcinoma patients.
Although this is the first study to describe lncRNA SNP and lung adenocarcinoma survival, some limitations should be taken into consideration. First, this study used a single-institution cohort to investigate the association between MALAT1 variant and the survival outcome of lung cancer patients for practical reason. It would be ideal to have a multi-center based replication to validate our findings. Without such replication, our findings should be considered preliminary. Second, to get adequate statistical power by using this moderate cohort of lung cancer patients, we only choose the SNP with MAF > 0.1 (rs3200401) to investigate in the present study. The other low-frequency SNPs in MALAT1 were also needed to be investigated in further large sample-sized populations. Finally, it is a pity that there were no rs3200401 genotype data in the TCGA database, except for the expression of MALAT1 in lung tumor tissues. To give a clue for further interpretation and explanation of the biological function of rs3200401, we still analyzed the TCGA data and found that a higher MALAT1 expression level was associated with a worse survival outcome among advanced lung adenocarcinoma patients. But the biological function of this SNP and its effect on MALAT1 expression level need to be deep investigated by further biological studies.
Conclusions
In conclusion, this study revealed that the genetic variation SNP rs3200401 T allele located on lncRNA MALAT1 was associated with a better survival of advanced lung adenocarcinoma patient, while this effect was not seen among lung squamous cell carcinoma patients. The protective effect of rs3200401 T allele may because it can influence the secondary structure of lncRNA MALAT1, or influence the interaction between MALAT1 and SR proteins thus by altering the expression levels of metastasis associated genes. The MALAT1 rs3200401 T allele may serve as a novel biomarker for predicting clinical outcomes of lung adenocarcinoma. Further large population based survival analysis and mechanistic studies are required to confirm our findings.
Abbreviations
- lncRNA:
-
Long non-coding RNA
- MALAT1:
-
Metastasis associated lung adenocarcinoma transcript 1
- NSCLC:
-
Non–small cell lung carcinoma
- SNP:
-
Single nucleotide polymorphism
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108.
Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA. SEER cancer statistics review, 1975–2013. Bethesda: National Cancer Institute; 2015. http://seer.cancer.gov/csr/1975_2013/. Accessed 21 May 2016.
Rinn JL, Chang HY. Genome regulation by long noncoding RNAs. Annu Rev Biochem. 2012;81:145–66.
Prensner JR, Chinnaiyan AM. The emergence of lncRNAs in cancer biology. Cancer Discov. 2011;1:391–407.
Mitra SA, Mitra AP, Triche TJ. A central role for long non-coding RNA in cancer. Front Genet. 2012;3:17.
Zhang H, Chen Z, Wang X, Huang Z, He Z, Chen Y. Long non-coding RNA: a new player in cancer. J Hematol Oncol. 2013;6:37.
Fatima R, Akhade VS, Pal D, Rao SM. Long noncoding RNAs in development and cancer: potential biomarkers and therapeutic targets. Mol Cell Ther. 2015;3:5.
Gezer U, Özgür E, Cetinkaya M, Isin M, Dalay N. Long non-coding RNAs with low expression levels in cells are enriched in secreted exosomes. Cell Biol Int. 2014;38:1076–9.
Ji P, Diederichs S, Wang W, Böing S, Metzger R, Schneider PM, et al. MALAT-1, a novel noncoding RNA, and thymosin beta4 predict metastasis and survival in early-stage non-small cell lung cancer. Oncogene. 2003;22:8031–41.
Hutchinson JN, Ensminger AW, Clemson CM, Lynch CR, Lawrence JB, Chess A. A screen for nuclear transcripts identifies two linked noncoding RNAs associated with SC35 splicing domains. BMC Genomics. 2007;8:39.
Clemson CM, Hutchinson JN, Sara SA, Ensminger AW, Fox AH, Chess A, et al. An architectural role for a nuclear noncoding RNA: NEAT1 RNA is essential for the structure of paraspeckles. Mol Cell. 2009;33:717–26.
Bernard D, Prasanth KV, Tripathi V, Colasse S, Nakamura T, Xuan Z, et al. A long nuclear-retained non-coding RNA regulates synaptogenesis by modulating gene expression. EMBO J. 2010;29:3082–93.
Tripathi V, Ellis JD, Shen Z, Song DY, Pan Q, Watt AT, et al. The nuclear-retained noncoding RNA MALAT1 regulates alternative splicing by modulating SR splicing factor phosphorylation. Mol Cell. 2010;39:925–38.
Cheetham SW, Gruhl F, Mattick JS, Dinger ME. Long noncoding RNAs and the genetics of cancer. Br J Cancer. 2013;108:2419–25.
Tano K, Mizuno R, Okada T, Rakwal R, Shibato J, Masuo Y, et al. MALAT-1 enhances cell motility of lung adenocarcinoma cells by influencing the expression of motility-related genes. FEBS Lett. 2010;584:4575–80.
Tripathi V, Shen Z, Chakraborty A, Giri S, Freier SM, Wu X, et al. Long noncoding RNA MALAT1 controls cell cycle progression by regulating the expression of oncogenic transcription factor B-MYB. PLoS Genet. 2013;9:e1003368.
Michalik KM, You X, Manavski Y, Doddaballapur A, Zörnig M, Braun T, et al. Long noncoding RNA MALAT1 regulates endothelial cell function and vessel growth. Circ Res. 2014;114:1389–97.
Roth A, Diederichs S. Long noncoding RNAs in lung cancer. Curr Top Microbiol Immunol. 2016;394:57–110.
Schmidt LH, Spieker T, Koschmieder S, Schäffers S, Humberg J, Jungen D, et al. The long noncoding MALAT-1 RNA indicates a poor prognosis in non-small cell lung cancer and induces migration and tumor growth. J Thorac Oncol. 2011;6:1984–92.
Gutschner T, Hämmerle M, Diederichs S. MALAT1 -- a paradigm for long noncoding RNA function in cancer. J Mol Med (Berl). 2013;91:791–801.
Zheng HT, Shi DB, Wang YW, Li XX, Xu Y, Tripathi P, et al. High expression of lncRNA MALAT1 suggests a biomarker of poor prognosis in colorectal cancer. Int J Clin Exp Pathol. 2014;7:3174–81.
Pang E-J, Yang R, Fu X-B, Liu Y-F. Overexpression of long non-coding RNA MALAT1 is correlated with clinical progression and unfavorable prognosis in pancreatic cancer. Tumour Biol. 2015;36:2403–7.
Ma K-X, Wang H-J, Li X-R, Li T, Su G, Yang P, et al. Long noncoding RNA MALAT1 associates with the malignant status and poor prognosis in glioma. Tumour Biol. 2015;36:3355–9.
Zhang H-M, Yang F-Q, Chen S-J, Che J, Zheng J-H. Upregulation of long non-coding RNA MALAT1 correlates with tumor progression and poor prognosis in clear cell renal cell carcinoma. Tumour Biol. 2015;36:2947–55.
Zhang J, Zhang B, Wang T, Wang H. LncRNA MALAT1 overexpression is an unfavorable prognostic factor in human cancer: evidence from a meta-analysis. Int J Clin Exp Med. 2015;8:5499–505.
Guo H, Deng Q, Wu C, Hu L, Wei S, Xu P, et al. Variations in HSPA1B at 6p21.3 are associated with lung cancer risk and prognosis in Chinese populations. Cancer Res. 2011;71:7576–86.
McGuire S. World Cancer Report 2014. Geneva, Switzerland: World Health Organization, International Agency for Research on Cancer, WHO Press, 2015. Adv Nutr. 2016;7:418–9.
Thum T, Fiedler J. LINCing MALAT1 and angiogenesis. Circ Res. 2014;114:1366–8.
Ying L, Chen Q, Wang Y, Zhou Z, Huang Y, Qiu F. Upregulated MALAT-1 contributes to bladder cancer cell migration by inducing epithelial-to-mesenchymal transition. Mol Biosyst. 2012;8:2289–94.
Shen L, Chen L, Wang Y, Jiang X, Xia H, Zhuang Z. Long noncoding RNA MALAT1 promotes brain metastasis by inducing epithelial-mesenchymal transition in lung cancer. J Neurooncol. 2015;121:101–8.
Cerami E, Gao J, Dogrusoz U, Gross BE, Sumer SO, Aksoy BA, et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2:401–4.
Sakashita E, Endo H. SR and SR-related proteins redistribute to segregated fibrillar components of nucleoli in a response to DNA damage. Nucleus. 2010;1:367–80.
Tripathi V, Song DY, Zong X, Shevtsov SP, Hearn S, Fu X-D, et al. SRSF1 regulates the assembly of pre-mRNA processing factors in nuclear speckles. Mol Biol Cell. 2012;23:3694–706.
Miyagawa R, Tano K, Mizuno R, Nakamura Y, Ijiri K, Rakwal R, et al. Identification of cis- and trans-acting factors involved in the localization of MALAT-1 noncoding RNA to nuclear speckles. RNA. 2012;18:738–51.
Wang J, Su L, Chen X, Li P, Cai Q, Yu B, et al. MALAT1 promotes cell proliferation in gastric cancer by recruiting SF2/ASF. Biomed Pharmacother. 2014;68:557–64.
Pei N, Cao L, Liu Y, Wu J, Song Q, Zhang Z, et al. XAB2 tagSNPs contribute to non-small cell lung cancer susceptibility in Chinese population. BMC Cancer. 2015;15:560.
Shen W, Yin R, Wang C, Zhu M, Zhou W, Qin N, et al. Polymorphisms in alternative splicing associated genes are associated with lung cancer risk in a Chinese population. Lung Cancer. 2015;89:238–42.
Zhang X, Fan J, Li Y, Lin S, Shu P, Ni J, et al. Polymorphisms in epidermal growth factor receptor (EGFR) and AKT1 as possible predictors of clinical outcome in advanced non-small-cell lung cancer patients treated with EGFR tyrosine kinase inhibitors. Tumour Biol. 2016;37:1061–9.
Xu F, Han J-C, Zhang Y-J, Zhang YJ, Zhang Y-J, Liu X-C, et al. Associations of LIG4 and HSPB1 Genetic Polymorphisms with Risk of Radiation-Induced Lung Injury in Lung Cancer Patients Treated with Radiotherapy. Biomed Res Int. 2015;2015:860373.
Gong WJ, Yin JY, Li XP, Fang C, Xiao D, Xiao D, et al. Association of well-characterized lung cancer lncRNA polymorphisms with lung cancer susceptibility and platinum-based chemotherapy response. Tumour Biol. 2016;37:8349–58.
González-Arriaga P, Pascual T, García-Alvarez A, Fernández-Somoano A, López-Cima MF, Tardón A. Genetic polymorphisms in MMP 2, 9 and 3 genes modify lung cancer risk and survival. BMC Cancer. 2012;12:121.
Zhang ZY, Tian X, Wu R, Liang Y, Jin XY. Predictive role of ERCC1 and XPD genetic polymorphisms in survival of Chinese non-small cell lung cancer patients receiving chemotherapy. Asian Pac J Cancer Prev. 2012;13:2583–6.
Kong J, Xu F, Qu J, Wang Y, Gao M, Yu H, et al. Abstract 4601: genetic polymorphisms in the vitamin D pathway in relation to lung cancer risk and survival. Oncotarget. 2015;6:2573–82.
Guo X, Li D, Wu Y, Chen Y, Zhou X, Wang X, et al. Genetic variants in genes of tricarboxylic acid cycle key enzymes are associated with prognosis of patients with non-small cell lung cancer. Lung Cancer. 2015;87:162–8.
Liu Y, Pan S, Liu L, Zhai X, Liu J, Wen J, et al. A genetic variant in long Non-coding RNA HULC contributes to risk of HBV-related hepatocellular carcinoma in a Chinese population. PLoS One. 2012;7:e35145.
Hrdlickova B, de Almeida RC, Borek Z, Withoff S. Genetic variation in the non-coding genome: Involvement of micro-RNAs and long non-coding RNAs in disease. Biochim Biophy Acta. 1842;2014:1910–22.
Gong J, Liu W, Zhang J, Miao X, Guo AY. lncRNASNP: a database of SNPs in lncRNAs and their potential functions in human and mouse. Nucleic Acids Res. 2015;43:D181–6.
Gout S, Brambilla E, Boudria A, Drissi R, Lantuejoul S, Gazzeri S, et al. Abnormal expression of the Pre-mRNA splicing regulators SRSF1, SRSF2, SRPK1 and SRPK2 in non small cell lung carcinoma. PLoS One. 2012;7:e46539.
Acknowledgements
The authors thank all volunteers and medical assistants from cooperating hospitals.
Funding
This study was supported by the funds from Wuhan municipality Health and family planning commission Scientific Research Project (Grant No. WX14C27), the Natural National Scientific Foundation of China (Grant No. 81272589), Program for New Century Excellent Talents in University of Ministry of Education of China, 2012 (Grant No. NCET-12-0209), and Foundation for the Author of National Excellent Doctoral Dissertation of PR China (Grant No. 201484). The funders had no roles in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
Not applicable.
Authors’ contributions
XQY and QW provided study materials or patients. LGW, WHG and YP carried out clinical information and sample collection. LGW, YSB and ZWC performed genotyping and data analysis. JZW, JJX, HG and PX participated in study design and helped draft the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The protocol of this study was approved by the ethical committees of Tongji Medical College, Huazhong University of Science and Technology. All participants provided written informed consent.
Author information
Authors and Affiliations
Corresponding authors
Additional file
Additional file 1: Table S1.
The SNPs located on the lncRNA MALAT1 gene (data source: the dbSNP database). Table S2. Demographic and clinical characteristics of 117 advanced NSCLC patients from TCGA. (DOCX 24.8 kb)
Additional file 2: Figure S1.
Predicted secondary structures of lncRNA MALAT1. C > T variation of rs3200401 caused 1.62 kcal/mol minimal free energy (MFE, ΔG) change, which may alter structural features of MALAT1, resulting in weaken interaction between MALAT1 and its binding protein SRSF2. (TIF 215 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wang, JZ., Xiang, JJ., Wu, LG. et al. A genetic variant in long non-coding RNA MALAT1 associated with survival outcome among patients with advanced lung adenocarcinoma: a survival cohort analysis. BMC Cancer 17, 167 (2017). https://doi.org/10.1186/s12885-017-3151-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-017-3151-6