Abstract
Background
BRAF and MEK are component of the MAPK/ERK pathway and inhibitors of these proteins have significantly improved the outcome of metastatic melanoma. We report for the first time two sequential episodes of pneumonitis presumably induced by trametinib (a MEK inhibitor) and vemurafenib (a BRAF inhibitor) in a 50 year-old man.
Case presentation
While receiving trametinib for a metastatic melanoma, the patient developed non-febrile acute respiratory failure in the context of bilateral ground-glass opacities and sub pleural reticulations on high resolution computed tomography. An excess of lymphocytes was found in the bronchoalveolar lavage fluid. Outcome was favorable after simple drug discontinuation. He subsequently developed a similar clinical-imaging picture 6 months into vemurafenib. A transthoracic lung biopsy disclosed interstitial lymphocytic infiltrate, poorly-formed granulomas with multinucleated giant cells and scattered eosinophils. Outcome was again favorable after simple drug discontinuation.
Conclusion
These two episodes in the same patient suggest that MAPK/ERK inhibitors may cause interstitial lung disease and may exert cross toxicity. This side effect is of particular interest for physicians in charge of patients with melanoma but this drug family is currently under development for several other solid tumors.
Similar content being viewed by others
Background
The novel BRAFV600 (vemurafenib, dabrafenib) and MEK (trametinib) inhibitor are structurally-unrelated small molecules targeting two critical proteins which belong to the MAPK/ERK pathway. These drugs have transformed the prognosis of metastatic melanoma harboring BRAFV600 mutation improving both disease-free and overall survival [1–3]. We report a patient who developed trametinib and vemurafenib induced reversible pneumonitis.
Case presentation
Case
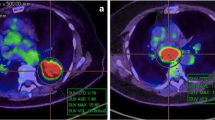
A 50 year-old non-smoking man was diagnosed with BRAFV600E mutation-positive metastatic melanoma in 2010. Evaluation following two courses of a dacarbazine-based regimen showed progression of the cutaneous lesions and new metastases in both the lung parenchyma and mediastinal lymph nodes. After informed consent, he entered clinicaltrial.gov NCT01245062 phase III study and received trametinib 2 mg daily. Pretherapy high resolution computed tomography (HRCT) showed no evidence of interstitial lung disease (ILD). Five months into treatment, he complained of dyspnea and mild hemoptysis. There was no fever. Progressive dyspnea led to admission. Clinical examination showed bilateral crackles. Arterial blood gases results (room air) were PaO2 58 mmHg, PaCO2 40 mmHg, pH 7.47. On HRCT, melanoma metastases were no longer present. There were bilateral ground glass shadowing and subpleural reticulations (Fig. 1a). Blood eosinophils were 640 × 106 × L−1. Bronchoalveolar lavage (BAL) fluid yielded 20 × 106 cells.mL−1, of which 87 % were lymphocytes (CD4+/CD8+ ratio: 0.4) and 1 % of all cells were eosinophils. No Pneumocystis jiroveci (PJ) cysts were visualized. Trametinib was discontinued, while the remainder of drugs (bisoprolol, valsartan, rosuvastatin, allopurinol, paracetamol, oxazepam) was kept unchanged. Corticosteroids were not given. Patient improved clinically and radiologically (Fig. 1b).
Vemurafenib (1920 mg/d) was started 2 months later. Three months into treatment, patient reported recurrence of hemoptysis and dyspnea. Although HRCT revealed new ground-glass opacities in both lungs, vemurafenib was continued. Respiratory status and HRCT slowly worsened (Fig. 1c). Fifteen months into treatment with vemurafenib, a new BAL disclosed lymphocytic alveolitis (730 × 103 cells.mL−1, 68 % lymphocytes, CD4/CD8 ratio: 0.4, eosinophils were 3 %). There was no peripheral eosinophilia. A CT-guided transthoracic lung biopsy disclosed an interstitial and alveolar lymphocytic infiltrate, scattered eosinophils associated with poorly-formed epithelioid granulomas and multinucleated giant cells (Fig. 2). Necrosis, vasculitis, malignant cells or refractive foreign body under polarized light were absent. Special stains for PJ were negative. Polymerase chain reaction on BAL for PJ was nondiagnostic with 33.5 replication cycles indicating colonization or low burden. No anti-Pneumocystis drugs were given. Vemurafenib-induced pneumonitis was suspected and the drug was withheld. Respiratory symptoms progressively waned. Six months later, infiltrates and reticulations had cleared but metastatic disease progression was noted (Fig. 1d). The patient currently is on dabrafenib a BRAF inhibitor and is monitored serially and carefully as regards pulmonary signs and symptoms.
Discussion
We report here two episodes of subacute pneumonitis that are chronologically compatible with a drug etiology. BAL findings and pathology, although not entirely specific, supported a drug reaction. Pathology findings were compatible with hypersensitivity pneumonitis to inhaled antigens, but there was no exposure to organic environmental sources. The drug etiology was also supported by improvement following drug discontinuation while corticosteroids were not given [4, 5]. Cardiogenic, infectious and neoplastic causes were considered unlikely on the basis of clinical, imaging, BAL and pathology data and because our patient’s condition improved upon drug stoppage.
Several pathological patterns have been described in patients with drug-induced pneumonitis [6]. A lymphocytic interstitial infiltrate with poorly-formed granulomas and giant cells has been described in patients with methotrexate, nitrofurantoin, BCG therapy, anti-TNF agents and mTOR inhibitor-induced lung reactions [6–8]. However, in patients with drug-induced pneumonitis, changes on pathology are rarely specific and correlate poorly with findings on imaging [9].
The present case is one of five trametinib-induced pneumonitis cases mentioned to date in the US marketing authorization file (www.accessdata.fda.gov/drugsatfdadocs/label/2014/204114s001lbl.pdf). There is no report in the literature yet. As of vemurafenib, our case is the second one described [10] but it is the first one with histological documentation. Our patient is also unique in that ILD developed while he was being treated with either one agent.
Both trametinib and vemurafenib target effectors of the MAPK/ERK pathway. Other drugs targeting upstream proteins involved in this pathway such as the tyrosine kinase inhibitors erlotinib, gefitinib, cetuximab and sorafenib may also cause pulmonary toxicity [11]. The pathophysiology of these disorders is currently unclear, but involvement of the MAPK/ERK pathway itself is one hypothesis [11].
Conclusion
The dual inhibition of BRAF and MEK is currently one of the most promising therapeutic options to improve survival in melanoma patients [12]. Moreover, these drugs are under development for the treatment of several other solid tumors. We feel it is important to alert clinicians to the potential severe pulmonary toxicity of these two drugs targeting the MAPK/ERK pathway and to their possible class effect.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Abbreviations
- HRCT:
-
High Resolution Computed Tomography
- ILD:
-
Interstitial Lung Disease
- BAL:
-
Bronchoalveolar Lavage
- PJ:
-
Pneumocystis jiroveci
References
Chapman PB, Hauschild A, Robert C, Haanen JB, Ascierto P, Larkin J, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364(26):2507–16.
Hauschild A, Grob JJ, Demidov LV, Jouary T, Gutzmer R, Millward M, et al. Dabrafenib in BRAF-mutated metastatic melanoma: a multicentre, open-label, phase 3 randomised controlled trial. Lancet. 2012;380(28):358–65.
Flaherty KT, Robert C, Hersey P, Nathan P, Garbe C, Milhem M, et al. Improved Survival with MEK Inhibition in BRAF-Mutated Melanoma. N Engl J Med. 2012;367(2):107–14.
Lacasse Y, Girard M, Cormier Y. Recent advances in hypersensitivity pneumonitis. Chest. 2012;142(1):208–17.
Xu JF, Shen L, Zhang Y, Zhang P, Qu JM, Li HP. Lung biopsy proved hypersensitivity pneumonitis without known offending antigen: characteristics and follow up. Clin Respir J. 2014;8(3):297–304.
Flieder DB, Travis WD. Pathologic characteristics of drug induced lung disease. Cli Chest Med. 2004;25(1):37–45.
Myers J, Limper A, Swensen S. Drug-Induced lung disease: a pragmatic classification incorporating HRCT appearance. Sem Respir Crit Care Med. 2003;24(4):445–54.
www.pneumotox.com. v2.0. Producer: Ph Camus 2013. Accessed July 12, 2014.
Cleverley J, Screaton N, Hiorns M, Flint J, Muller N. Drug-induced lung disese: high –resolution CT and histologic findings. Clin Radiol. 2002;57:292–9.
Schmitt L, Schumann T, Löser C, Dippel E. Vemurafenib-induced pulmonary injury. Onkologie. 2013;36(11):685–6.
Min JH, Lee HY, Lim H, Ahn MJ, Park K, Chung MP, et al. Drug-induced interstitial lung disease in tyrosine kinase inhibitor therapy for non small cell lung cancer: a review on current insight. Cancer Chemother Pharmacol. 2011;68(5):1099–109.
Flaherty KT, Infante JR, Daud A, Gonzalez R, Kefford RF, Sosman J, et al. Combined BRAF and MEK inhibition in melanoma with BRAF V600 mutations. N Engl J Med. 2012;367(18):1694–703.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
V. Giraud, C. Longvert, S. Houlle-Crepin, C. Danel, S. Labrune, Ph. Camus and Th. Chinet have no competing interests. Ph. Saiag received research grants and clinical research or consultancy fees from GSK, Roche-Genentech, BMS and Novartis. None of the authors have any non-financial competing interests.
Authors’ contributions
VG and CL wrote the manuscript, SL, PC, PS and TC revisited it critically for important intellectual content, SHC and CD did the pathologic interpretation. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Giraud, V., Longvert, C., Houlle-Crepin, S. et al. Relapsing pneumonitis due to two distinct inhibitors of the MAPK/ERK pathway: report of a case. BMC Cancer 15, 732 (2015). https://doi.org/10.1186/s12885-015-1754-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-015-1754-3