Abstract
Background
This analysis was undertaken to evaluate the practice patterns of Japanese physicians regarding curative-intent chemotherapy, especially in outpatient settings, and to define factors negatively affecting the maintenance of relative dose intensity (RDI).
Methods
We performed a web-based questionnaire survey of Japanese physicians involved in malignant lymphoma chemotherapy (Group ML) or in breast cancer chemotherapy (Group BC). The questionnaire inquired how they manage low-risk febrile neutropenia (FN) caused by initial chemotherapy for diffuse large B-cell lymphoma(DLBCL) or by adjuvant chemotherapy for breast cancer in an outpatient setting.
Results
Valid responses were obtained from 185 physicians in Group ML and 160 in Group BC. In Group ML, 76 % (n = 141) of the physicians were board-certified hematologists, while 82 % (n = 131) of the physicians in Group BC were board-certified surgeons. A significantly higher proportion of physicians in Group ML responded that “dose reduction is not required for the subsequent course of chemotherapy after the first episode of FN” than in Group BC (ML versus BC; 77 % versus 31 %; P < 0.001). Significantly higher proportions of physicians in Group ML were more likely to prophylactically administer antibiotics or granulocyte-colony stimulating factor (G-CSF; ML versus BC; antibiotics: 36 % versus 26 %, P = 0.049; G-CSF: 25 % versus 16 %, P = 0.047). Eighty six percent (n = 159) of Group ML and 70 % (n = 112) of Group BC responded that “emergency outpatient unit is open at all hours”.
Conclusions
Japanese physicians are more likely to administer reduced doses of chemotherapy to patients with breast cancer than to patients with malignant lymphoma. Supportive infrastructures should be improved to ensure the provision of adequate chemotherapy to all cancer patients.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Maintaining dose intensity is important for achieving the full benefits of chemotherapy in patients with potentially curable non-Hodgkin’s lymphoma and breast cancer. In 1990, Epelbaum et al. reported a strong association between the relative dose intensity (RDI) of a standard CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone) regimen and 5-year survival among 95 patients with diffuse large-cell lymphoma (DLCL) [1]. The 5-year survival rate was 80 % in patients who received more than the median average RDI, whereas it was only 32 % in those who received less than the median average RDI (P < 0.001). Similarly, analysis of the RDIs of three doxorubicin-based regimens (including CHOP) in 115 patients with DLCL revealed that RDI of doxorubicin greater than 75 % was the most important predictor of survival [2]. A recently published retrospective analysis by Bosly et al. showed that survival of patients with diffuse large B-cell lymphoma (DLBCL) improved with an increasing average RDI (ARDI) of CHOP-21. Median survival was 7.08 years in those who received >90 % of the ARDI, significantly longer than in those who received ≤90 % of the ARDI (P = 0.002) [3]. In 1981, Bonadonna et al. reported a clear dose–response effect for CMF (cyclophosphamide, methotrexate, and 5-fluorouracil [5-FU]) chemotherapy in 449 women with breast cancer [4]. Their results showed that patients receiving ≥85 % of the planned CMF dose had a 5-year relapse-free survival (RFS) rate of 77 %, compared with 48 % in patients receiving <65 % of the planned dose. In 1995, 20-year follow-up data from the same group confirmed that RFS and overall survival (OS) were substantially better in patients who received ≥85 % of their planned dose than in those who received lower doses [5].
In 1998, Budman et al. reported the results of a randomized trial of adjuvant CAF (cyclophosphamide, doxorubicin, 5-FU) for stage II breast cancer patients. In total, 1,550 breast cancer patients were randomly assigned to one of three treatment arms: high-, moderate-, or low-dose intensity treatments [6]. The results revealed that the patients who received high- or moderate-dose intensity had significantly longer disease-free survival (P < 0.001) and OS (P = 0.004) than those who received low-dose intensity.
Recently, some study protocols specify that patients who have an initial episode of febrile neutropenia (FN) should additionally receive granulocyte-colony stimulating factor (G-CSF) or prophylactic antibiotics in subsequent cycles, and dose modification of chemotherapy is unnecessary [7–9]. If there is a second FN episode despite G-CSF or antibiotic support, the protocols recommend a reduction in chemotherapy dose.
However, studies of patients with aggressive non-Hodgkin’s lymphoma and early-stage breast cancer in the United States have reported that nearly half of such patients receive reduced dose-intensity chemotherapy [10, 11]. Additionally, how Japanese physicians manage outpatient chemotherapy and apply supportive measures to maintain RDI remains largely unknown. In Japan, chemotherapy for malignant lymphoma has been traditionally administered by hematologists, while chemotherapy for breast cancer is administered mainly by surgeons. This study was designed to clarify physicians’ attitudes and practice patterns with respect to curative-intent chemotherapy and to define factors that negatively affect RDI maintenance in Japan.
Methods
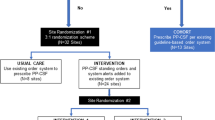
We posted a questionnaire on a Japanese web site for physicians. Registration was required to access the questionnaire and those who completed the questionnaire could receive points from the web site as an incentive. The target respondents were physicians involved in the treatment of malignant lymphoma (Group ML) and those involved in the treatment of breast cancer (Group BC). Respondents in Group ML had to: 1) be a member of the Japanese Society of Hematology; 2) work at a hospital with more than 20 beds; 3) attend more than five patients with Non-Hodgkin’s lymphoma who receive chemotherapy; and 4) attend at least one patient who received R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone) in the past year. Respondents in Group BC had to: 1) be a member of the Japanese Breast Cancer Society; and 2) attend more than 15 patients who received neoadjuvant or adjuvant chemotherapy in the past year. The number of current members of the Japanese Society of Hematology is around 6,400, whereas number of current members of the Japanese Breast Cancer Society is around 9,800, 68 % of which are surgeons.
In the questionnaire, we described a patient who received first-line chemotherapy for DLBCL in Group ML and a patient who received adjuvant chemotherapy for early breast cancer in Group BC. In the clinical scenarios, the patients suffer from low risk FN with The Multinational Association for Supportive Care in Cancer (MASCC) scores ≥21 [12, 13] and in Talcott group 4 [14]. The questionnaire inquired about the management of FN and subsequent cycles of chemotherapy. The questions asked in the survey are listed in Table 1. This survey was administered in Japanese. The surveillance period was from November 30 through December 11, 2012.
All survey data were coded and analyzed with the use of standard EZR (Saitama Medical Center, Jichi Medical University), which is a graphical user interface for R (The R Foundation for Statistical Computing, version 2.13.0) [15]. More precisely, it is a modified version of R commander (version 1.6–3) that includes statistical functions that are frequently used in biostatistics. For comparisons of categorical variables, Fisher’s exact tests were used.
The execution of the survey followed the ethical principles outlined in the Declaration of Helsinki regarding human clinical research. The approval of the Ethics Committee of Nippon Medical School Musashikosugi Hospital was not required. This is because the regulation of the Ethics Committee of Nippon Medical School does not stipulate that a questionnaire survey for physicians requires ethical committee approval. Moreover, this is an anonymous questionnaire survey and we only use pseudonymized data.
Results
Table 2 lists the participant characteristics. Valid responses were obtained from 185 respondents in Group ML and 160 in Group BC; there were no invalid responses. In Group ML, 76 % (n = 141) of the respondents were board-certified hematologists, and 10 % (n = 18) were board-certified oncologists. In Group BC, 82 % (n = 131) were board-certified surgeons and 36 % (n = 58) were board-certified breast surgeons. Overall, 11 % (n = 17) of the respondents in Group BC were board-certified oncologists. In Group ML, 32 % (n = 59) of the respondents were working at academic medical centers, 32 % (n = 59) at cancer centers or public hospitals, and 36 % (n = 67) at private hospitals. In Group BC, 21 % (n = 33) were working at academic medical centers, 29 % (n = 46) at cancer centers or public hospitals, and 43 % (n = 69) at private hospitals.
Table 3 summarizes how the respondents manage low-risk FN. 50 % (n = 93) of the physicians in Group ML chose outpatient treatment for FN as compared with 65 % (n = 104) in Group BC (P = 0.006). Among the respondents who chose outpatient treatment, a higher proportion of physicians chose both oral antibiotics and G-CSF in Group ML than in Group BC (82 % versus 53 %, P < 0.001). However, intravenous antibiotics and G-CSF were preferred among physicians who chose inpatient treatment for FN.
Table 4 summarizes how the respondents modify the dose of chemotherapy in patients who have FN and their attitudes toward the use of antibiotics and G-CSF for subsequent cycles of chemotherapy. In Group ML, 77 % (n = 143) of the physicians responded that “dose reduction is not required” compared with 31 % (n = 49) in Group BC (P < 0.001). In Group BC, approximately one third of the physicians responded that “dose reduction is required if FN was treated by intravenous antibiotics” and another third responded that “dose reduction is required at any rate”. Thirty-six percent (n = 67) of Group ML and 26 % (n = 42) of Group BC responded that “antimicrobial prophylaxis deserves consideration” (P = 0.049). Approximately half of the physicians in each group responded that “antibiotics are taken into account on the next episode of FN”. Twenty-five percent (n = 47) of Group ML and 16 % (n = 26) of Group BC responded that “G-CSF prophylaxis deserves consideration” (P = 0.047). Approximately half of the physicians in each group responded that “G-CSF is taken into account when neutropenia occurs”. About one third of Group BC responded that “G-CSF is taken into account when the next episode of FN occurs”.
Table 5 shows the details of the systems used to manage adverse effects of outpatient chemotherapy. For this analysis, physicians who work at clinics with less than 12 beds were not included in Group ML, but were included in Group BC. Eight percent (n = 12) of physicians in Group BC worked at clinics with less than 20 beds. Eighty-six percent (n = 159) of Group ML and 70 % (n = 112) of Group BC responded that the “emergency outpatient unit is open at all hours”. Sixty-nine percent (n = 128) of Group ML and 41 % (n = 66) of Group BC responded that the “clinical laboratory is open at all hours”. Moreover, 63 % (n = 117) of Group ML and 33 % (n = 52) of Group BC responded that the “diagnostic imaging unit is open at all hours”. Only 15 % (n = 27) of physicians in Group ML and 16 % (n = 26) of those in Group BC group responded that a “chemotherapy telephone helpline is available”.
Discussion
The most important finding of our study is that many Japanese physicians reduce the dose of chemotherapeutic agents after the first episode of low-risk FN in patients with potentially curable aggressive non-Hodgkin’s lymphoma or early-stage breast cancer. In the questionnaire, we presented the case of a patient who had FN during treatment for aggressive non-Hodgkin’s lymphoma or early-stage breast cancer in an outpatient setting (Table 1). She was clinically stable without significant medical comorbidity on presentation. Her MASCC score [12, 13] was 24, and she was classified as Talcott’s Group 4 [14], indicating low-risk FN. As for the subsequent course of chemotherapy, a higher proportion of physicians in Group BC responded that “dose reduction is required at any rate” or that “dose reduction is required if FN was treated by intravenous antibiotics” than in Group ML.
As mentioned in the introduction, there is well-established evidence supporting the clinical significance of RDI and its impact on survival in patients with aggressive non-Hodgkin’s lymphoma or early stage breast cancer [1–6]. This is why reducing the dose and delaying chemotherapy should be avoided. FN and severe prolonged neutropenia can lead to the decision to reduce chemotherapy dose and delay subsequent treatment cycles. In addition, the risk of fatal infection rises as the absolute neutrophil count falls below 500/mm3 and is higher in those with a prolonged neutropenia duration (>7 days) [16]. Therefore, management of afebrile and febrile neutropenia is significant. The Cochrane Haematological Malignancies Group published a review that compare the effectiveness of prophylactic administration of G-CSF or Granulocyte Macrophage Colony-Stimulating Factor (GM-CSF) with antibiotics in cancer patients receiving chemotherapy [17]. Two randomized controlled trials were eligible. This review showed non-significant results favoring antibiotics for preventing fever or hospitalization for FN compared with G-CSF. However, in one of the two trials, the chemotherapy dose intensity received by the antibiotic comparison group was much lower than in the GM-CSF group [18], which may explain the increased incidence of infections in the GM-CSF group. A non-randomized comparison within a randomized controlled trial (GEPARTRIO study) lead to a different outcome [19]. In breast cancer patients receiving TAC (docetaxel, doxorubicin and cyclophosphamide) pegfilgrastim alone or pegfilgrastim plus antibiotics provided suboptimal protection against FN and antibiotics alone was least effective.
Our results showed that that G-CSF and antibiotics are not commonly administered as prophylaxis against FN by Japanese physicians. G-CSF use for the management of established afebrile neutropenia was preferred in both groups. Guidelines recommend against the use of G-CSF in patients with afebrile neutropenia [20–23]. A randomized, double blind, placebo-controlled trial of G-CSF has been performed in afebrile outpatients with severe chemotherapy-induced neutropenia [24]: G-CSF shortened the duration of neutropenia, but did not decrease the hospitalization rate for FN, length of hospital stay, the number of days of antibiotic therapy, and the likelihood of having a positive culture.
Guidelines support the use of G-CSF in patients with FN who are at high risk for infection-associated complications [20–23]. A randomized, open-label, non-placebo-controlled trial has evaluated the effectiveness of adding G-CSF to antibiotic therapy in patients with solid tumors and chemotherapy-induced high-risk FN [25]. Adding G-CSF to antibiotic therapy was found to shorten the duration of neutropenia and reduce the duration of antibiotic therapy and hospitalization, but the treatment success rate, time to fever resolution, and mortality rate were similar in both treatment arms. Contrary to such evidence, many physicians use G-CSF with therapeutic intent.
In Japan, the majority of cancer care, including chemotherapy for solid tumors, has been historically performed by surgeons. Moreover, there is a shortage of medical oncologists in Japan. As of 2015, only 954 physicians have become Board-Certified Medical Oncologists of the Japanese Society of Medical Oncology (JSMO) [26]. Oncology education and training system in Japan needs much improvement. In addition, pegfilgrastim was not available in Japan until November 2014, and hospital visits on successive days were required. These factors may have a negative impact on outpatient management of chemotherapy and supportive care.
The Japanese Breast Cancer Society has developed Clinical Practice Guidelines for the systemic treatment of breast cancer [27]. These guidelines do not report how to use G-CSF or antibiotics as curative-intent chemotherapy. Including information about RDI and supportive measures into these guidelines may be an effective way to improve maintenance of dose-intensity.
About 50 % of Group ML and 35 % of Group BC chose to have the patient admitted to hospital for the treatment of FN. The American Society of Clinical Oncology (ASCO) clinical practice guidelines recommends outpatient management of low-risk FN as an option for carefully selected patients [28]. Based on the ASCO’s members’ expert opinion, “access to a telephone and transportation 24 h a day” is one of the requirements for outpatient treatment. However, our survey revealed that support systems for outpatient chemotherapy have not been adequately established in many hospitals and clinics in Japan.
Our study has several important limitations. First, the respondents may have been forgetful or may have responded without understanding the full context of the situation presented in the survey. In addition, eligible respondents were limited to physicians who had access to the website, potentially introducing self-selection bias. Despite these limitations, we believe that our study represents an important step in the improvement of cancer chemotherapy in Japan.
Conclusions
In summary, our results suggest that supportive measures to deliver full dose-intensity chemotherapy are not widely used by Japanese physicians. Systems to support outpatient chemotherapy should thus be improved.
Abbreviations
- RDI:
-
Relative dose intensity
- ML:
-
Malignant lymphoma
- BC:
-
Breast cancer
- FN:
-
Febrile neutropenia
- DLBCL:
-
Diffuse large B-cell lymphoma
- G-CSF:
-
Granulocyte-colony stimulating factor
- DLCL:
-
Diffuse large-cell lymphoma
- ARDI:
-
Average relative dose intensity
- 5-FU:
-
5-fluorouracil
- RFS:
-
Relapse-free survival
- OS:
-
Overall survival
- MASCC:
-
Multinational Association for Supportive Care in Cancer
- GM-CSF:
-
Granulocyte Macrophage Colony-Stimulating Factor
- ASCO:
-
American Society of Clinical Oncology
References
Epelbaum R, Faraggi D, Ben-Arie Y, Ben-Shahar M, Haim N, Ron Y, et al. Survival of diffuse large cell lymphoma. A multivariate analysis including dose intensity variables. Cancer. 1990;66(6):1124–9.
Kwak LW, Halpern J, Olshen RA, Horning SJ. Prognostic significance of actual dose intensity in diffuse large-cell lymphoma: results of a tree-structured survival analysis. J Clin Oncol. 1990;8(6):963–77.
Bosly A, Bron D, Van Hoof A, De Bock R, Berneman Z, Ferrant A, et al. Achievement of optimal average relative dose intensity and correlation with survival in diffuse large B-cell lymphoma patients treated with CHOP. Ann Hematol. 2008;87(4):277–83.
Bonadonna G, Valagussa P. Dose-response effect of adjuvant chemotherapy in breast cancer. N Engl J Med. 1981;304(1):10–5.
Bonadonna G, Valagussa P, Moliterni A, Zambetti M, Brambilla C. Adjuvant cyclophosphamide, methotrexate, and fluorouracil in node-positive breast cancer: the results of 20 years of follow-up. N Engl J Med. 1995;332(14):901–6.
Budman DR, Berry DA, Cirrincione CT, Henderson IC, Wood WC, Weiss RB, et al. Dose and dose intensity as determinants of outcome in the adjuvant treatment of breast cancer. The Cancer and Leukemia Group B. J Natl Cancer Inst. 1998;90(16):1205–11.
Slamon D, Eiermann W, Robert N, Pienkowski T, Martin M, Press M, et al. Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med. 2011;365(14):1273–83.
von Minckwitz G, Blohmer JU, Costa SD, Denkert C, Eidtmann H, Eiermann W, et al. Response-guided neoadjuvant chemotherapy for breast cancer. J Clin Oncol. 2013;31(29):3623–30.
Martin M, Seguí MA, Antón A, Ruiz A, Ramos M, Adrover E, et al. Adjuvant docetaxel for high-risk, node-negative breast cancer. N Engl J Med. 2010;363(23):2200–10.
Lyman GH, Dale DC, Crawford J. Incidence and predictors of low dose-intensity in adjuvant breast cancer chemotherapy: a nationwide study of community practices. J Clin Oncol. 2003;21(24):4524–31.
Lyman GH, Dale DC, Friedberg J, Crawford J, Fisher RI. Incidence and predictors of low chemotherapy dose-intensity in aggressive non-Hodgkin’s lymphoma: a nationwide study. J Clin Oncol. 2004;22(21):4302–11.
Klastersky J, Paesmans M, Rubenstein EB, Boyer M, Elting L, Feld R, et al. The Multinational Association for Supportive Care in Cancer risk index: A multinational scoring system for identifying low-risk febrile neutropenic cancer patients. J Clin Oncol. 2000;18(16):3038–51.
Uys A, Rapoport BL, Anderson R. Febrile neutropenia: a prospective study to validate the Multinational Association of Supportive Care of Cancer (MASCC) risk-index score. Support Care Cancer. 2004;12(8):555–60.
Talcott JA, Siegel RD, Finberg R, Goldman L. Risk assessment in cancer patients with fever and neutropenia: a prospective, two-center validation of a prediction rule. J Clin Oncol. 1992;10(2):316–22.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
Bodey GP, Buckley M, Sathe YS, Freireich EJ. Quantitative relationships between circulating leukocytes and infection in patients with acute leukemia. Ann Intern Med. 1966;64(2):328–40.
Herbst C, Naumann F, Kruse EB, Monsef I, Bohlius J, Schulz H, Engert A. Prophylactic antibiotics or G-CSF for the prevention of infections and improvement of survival in cancer patients undergoing chemotherapy. Cochrane Database Syst Rev 2009, CD007107.
Sculier JP, Paesmans M, Lecomte J, Van Cutsem O, Lafitte JJ, Berghmans T, et al. A three-arm phase III randomised trial assessing, in patients with extensive-disease small-cell lung cancer, accelerated chemotherapy with support of haematological growth factor or oral antibiotics. Br J Cancer. 2001;85(10):1444–51.
von Minckwitz G, Kümmel S, du Bois A, Eiermann W, Eidtmann H, Gerber B, et al. Pegfilgrastim +/- ciprofloxacin for primary prophylaxis with TAC (docetaxel/doxorubicin/cyclophosphamide) chemotherapy for breast cancer. Results from the GEPARTRIO study. Ann Oncol. 2008;19(2):292–8.
Smith TJ, Khatcheressian J, Lyman GH, Ozer H, Armitage JO, Balducci L, et al. 2006 update of recommendations for the use of white blood cell growth factors: an evidence-based clinical practice guideline. J Clin Oncol. 2006;24(19):3187–205.
Aapro MS, Bohlius J, Cameron DA, Dal Lago L, Donnelly JP, Kearney N, et al. 2010 update of EORTC guidelines for the use of granulocyte-colony stimulating factor to reduce the incidence of chemotherapy-induced febrile neutropenia in adult patients with lymphoproliferative disorders and solid tumours. Eur J Cancer. 2011;47(1):8–32.
National Comprehensive Cancer Network (NCCN) guidelines. Myeloid Growth factors. Available at: www.nccn.org. Accessed 25 September 2015.
Guidelines of the Japanese Society of Medical Oncology on the management of febrile neutropenia (in Japanese). http://www.nankodo.co.jp/g/g9784524268863/, http://www.jsmo.or.jp/.
Hartmann LC, Tschetter LK, Habermann TM, Ebbert LP, Johnson PS, Mailliard JA, et al. Granulocyte colony-stimulating factor in severe chemotherapy-induced afebrile neutropenia. N Engl J Med. 1997;336(25):1776–80.
Garcia-Carbonero R, Mayordomo JI, Tornamira MV, López-Brea M, Rueda A, Guillem V, et al. Granulocyte colony-stimulating factor in the treatment of high-risk febrile neutropenia: a multicenter randomized trial. J Natl Cancer Inst. 2001;93(1):31–8.
The Japanese Society of Medical Oncology. Available at: http://www.jsmo.or.jp/ Accessed 25 September 2015.
Mukai H, Aihara T, Yamamoto Y, Takahashi M, Toyama T, Sagara Y, et al. The Japanese Breast Cancer Society Clinical Practice Guideline for systemic treatment of breast cancer. Breast Cancer. 2015;22(1):5–15.
Flowers CR, Seidenfeld J, Bow EJ, Karten C, Gleason C, Hawley DK, et al. Antimicrobial prophylaxis and outpatient management of fever and neutropenia in adults treated for malignancy: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2013;31(6):794–810.
Acknowledgements
We express our gratitude to all the physicians who agreed to answer our questionnaire.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
HS, NK and GK conceived of and designed the study. HS performed statistical analysis and drafted the manuscript. HS and NK carried out the questionnaire survey. NK helped to draft the manuscript. NK and GK participated throughout the study and critically reviewed the manuscript. All authors read and approved the final manuscript.
Authors’ information
Not applicable.
Availability of data and materials
Not applicable.
All authors contributed equally to this work
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sakai, H., Katsumata, N. & Kadokura, G. Attitudes and practice patterns for maintaining relative dose intensity of chemotherapy in outpatient clinics: results of a Japanese web-based survey. BMC Cancer 15, 651 (2015). https://doi.org/10.1186/s12885-015-1651-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-015-1651-9