Abstract
Background
Over the last 20 years, global healthcare has placed a major focus on improving the survival rates of mothers and children, recognizing the potential to prevent a significant number of deaths resulting from pregnancy and childbirth. Nevertheless, there remains an ongoing obstacle to the insufficient utilization of critical obstetric services to achieve optimal health outcomes for pregnant women. This study aimed to assess the magnitude and determinants of maternal healthcare use in the Jimma Zone, Ethiopia.
Methods
Data were obtained from a household survey as part of the baseline assessment of a cluster randomized controlled trial. The study participants comprised 588 women in early pregnancy, specifically those with a gestational age of less than 20 weeks. Logistic regression analysis was employed to identify factors associated with the use of maternal health services. Adjusted odds ratios (AORs) were used to assess the strength of the associations, with significance level set at a p-value ≤ 0.05.
Results
The overall prevalence of maternal health service utilization was 87.9% (CI: 85.1, 90.4) for antenatal care, 74.7% (CI: 73.2, 79.9) for health facility delivery, and 60.4% (CI: 56.4, 64.3) for postnatal care. Multivariable logistic analysis revealed that maternal health service use was significantly influenced by access to health facilities (AOR: 6.6; 95% CI: 2.39, 18.16), financial hardship (AOR: 3; 95% CI: 1.97, 4.61), perceived respectful care (AOR: 2.3; 95% CI: 1.07, 5.11), perceived privacy of service provisions (AOR: 2.4; 95% CI: 1.47, 4.06), and attitudes toward maternal service use (AOR: 2.2; 95% CI: 1.48, 3.24).
Conclusions
The study revealed slightly higher rates of antenatal care, facility delivery, and postpartum care utilization. However, there was a low proportion of early antenatal care initiation, and high rates of antenatal care dropout. Mobile phone-based messaging intervention may enhance maternal health service use by addressing factors such as lack of access, economic challenges, disrespectful care, no privacy of procedures, and unfavorable attitudes.
Similar content being viewed by others
Background
Maternal health is a pillar within the broader landscape of global health concerns. It serves as an essential indicator that shapes the overall health and developmental trajectory of a society [1, 2]. Most maternal deaths worldwide occur in sub-Saharan Africa, with 70% of the burden in this region. The estimated maternal mortality ratio (MMR) is 542 deaths per 100,000 live births, which exceeds the target set in the Sustainable Development Goal (SDG) of 70 per 100,000 live births by 2030 [3,4,5,6].
Reducing maternal mortality is critical to achieving Sustainable Development Goal 3 (SDG3), which aims to ensure good health and well-being for people of all ages [7]. Experts predict that the target of reducing maternal mortality as part of the SDGs can be met by ensuring that 91% of women receive their first antenatal care visit (ANC1), 78% receive their fourth antenatal care visit (ANC4), eighty-one percent opt for institutional delivery, and 87% have skilled birth attendance by 2030 [5, 8,9,10]. Despite remarkable efforts, maternal death rates continue to be high in settings with limited resources. Ethiopia has one of the most alarming rates of maternal mortality worldwide [11, 12].
Although the effective use of maternal health services is a proven strategy to reduce maternal mortality, the utilization of maternal and neonatal health services and the level of health practices are very limited in many developing regions of the world [13]. According to the 2019 Ethiopia Demographic and Health Survey (EDHS), 74% of women receive antenatal care from skilled providers, 51% of births occur in health facilities, 38.5% receive postnatal check-ups, and 34% have four or more antenatal care visits [11].
There have been reports of discrepancies in local access to vital maternal health services. For instance, a study conducted by Mussie Alemayehu in the Tigray region showed that 58.2% of women attended antenatal care 4+, 87.9% opted for institutional delivery, and only 40.3% received postnatal care within 42 days of giving birth [14]. A study conducted in Ambo town, Oromia Regional State, revealed that the utilization of maternal health services was 39.7% for antenatal care, 28.7% for delivery services, and 19% for postnatal care [15]. Similarly, a study in the Amhara region revealed a low prevalence of maternal healthcare service utilization, with only 77% of women receiving Antenatal care (ANC) and 37% receiving postnatal care [16].
Multilevel factors, including sociocultural beliefs and practices, socioeconomic conditions, access to healthcare services, maternal education, lengthy wait times at healthcare facilities, inadequate referral procedures, poor staff interpersonal interactions, lack of privacy, and mothers' prior unfavorable experiences with the health system [17,18,19,20,21,22], influence the uptake of key maternal health services.
Research has shown a correlation between household wealth [23], health insurance [24], and maternal health service use. Education is an individual-level factor that consistently predicts service maternal health service uptake [25]. Middle-aged women are more likely to visit healthcare facilities during childbirth [26], and women's occupations, knowledge, and attitudes significantly influence maternal care practices [27, 28]. Inadequate social support prevents women from making appointments with healthcare providers [29]. Women with strong superstitious beliefs are less likely to utilize all three types of maternal health care [30]. Cultural beliefs and practices also affect care-seeking behavior, with women having limited rights to make decisions and limited time available to them [31]. Negative perceptions and poor attitudes discourage women from using intended services [32]. The extent of time available to women is also significant; in less-developed countries, more than two-thirds of women spend time caring for children and fetching water or fuel, leaving hardly any time for their health [33]. This study aimed to assess the magnitude of maternal health service use and associated factors.
Methods and materials
Study setting and design
We conducted a household survey as part of the baseline assessment of a cluster randomized controlled trial in three selected districts of the Jimma Zone, located 352 km from the capital, Addis Ababa in southwest Ethiopia. According to the projection of the 2007 population census, the three districts have an estimated population of 624,534 (49.32% women) by 2024. Of the total population, 144,267 (23.1%) were women of childbearing age. In the three districts, there are a total of 9 small urban and 75 rural gandas (lowest administrative units). The study was conducted from March 5 to March 20, 2023, as part of the baseline assessment in an ongoing cluster randomized controlled trial (cRCT). The trial protocol has been accepted for publication [34] and the trial was registered on January 4, 2022 with Clinical Trials (trial identifier PACTR202201753436676) and can be accessed at https://pactr.samrc.ac.za.
Study population
We considered Gandas with functional health posts and mobile network coverage as inclusion criteria for this study. However, throughout the selection process, almost all health posts were functional, had access to mobile networks, and were eligible for selection. The study population included pregnant women in the selected ganda of the three districts. A woman was included in the study if her Gestational Age (GA) was less than 20 weeks, as determined by the midwives through a thorough house-to-house registration process using the last menstrual period (LMP) and/or fundal height measurement technique. In Ethiopia, for frontline health facilities like health posts and health centers, gestational age (GA) is primarily determined using the last menstrual period (LMP). When women are unable to recall their LMP, health professionals use the fundal height measurement technique based on guidelines from the Federal Ministry of Health. Although these techniques are less accurate than ultrasound, they serve as primary methods for GA estimation in frontline health facilities because of their practicality and feasibility. In addition, the participant was included if she or one of her family members owned a mobile phone and provided written informed consent showing a willingness to participate in the study. Informed consent was obtained only from those randomly selected participants. The study excluded women who fulfilled the enrollment criteria but were critically ill at the time of enrollment and women with psychological disorder.
Sample size determination
We used methods proposed by Hooper and Bourke for sample size calculation [35] assuming a simple parallel group with a baseline outcome assessment and one follow-up assessment. Three trial arms (Gain framed, loss-framed, and the control arms) were assumed. The sample size, assuming individual randomization, was calculated with the following assumptions: for P1, the proportion of women attending ANC4 + among the control group was 23.27% [36], the power (1-β) was set at 0.8, and the two-sided alpha was 0.025. The effect size/absolute difference in the proportions of antenatal care visits > 4 was 0.15, and Zα/2 was adjusted for multiple comparisons using a Bonferroni correction = 2.24. The initial sample size (no) was calculated as follows: [no = DE* (Zα/2 + Zβ)2 * (P1(1 − P1) + P2(1 − P2))/(P1 − P2)2, where no was 175. Two design effects were used to inflate the sample size under individual randomization, considering the within-period intracluster correlation coefficient (ICC) and the between-period ICC. The design effect (dc) due to cluster randomization was calculated by considering the following parameters: within-period ICC (p) of 0.003 [37] and number of clusters per arm (n × dc × dr) ÷ m = 7. We calculated the design effect as dc = 1 + (m − 1)ρ = 1.12. The design effect (dr) due to repeated assessments was calculated using the following assumptions: within-period ICC and a cluster (0.003), autocorrelation coefficient (π) of 0.8 to allow for a 20% decay of the correlation from within to between different periods [38], and correlation between sample means from the same cluster at different times (r) determined as r = mpΠ/1 + (m-1)p. The design effect due to repeated assessment was calculated as dr = (1-r2) = 0.996. To obtain the final sample size per arm, we multiplied the sample size for individual randomization with both design effects as (no × dc × dr) = 188. Considering a 4% loss to follow-up, the final sample size for each arm was 196. This resulted in twenty-eight women per health post for a total sample size of five hundred eighty-eight.
Sampling technique
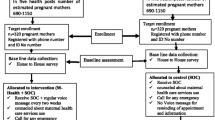
We randomly selected two primary healthcare units (PHCUs) per district from the three districts identified for mobile phone-based messaging interventions. Seven health posts per district were randomly selected for the trial using an Excel random number generator. A simple random sampling technique was used to select pregnant women. An individual who was not involved in the implementation of the trial used an Excel number generator to allocate pregnant women to the three intervention arms (Fig. 1).
Measurements
A structured questionnaire was used to measure maternal health service uptake and associated factors. The questionnaire was developed based on a review of the literature and presented in Afan Oromo language. The internal consistency of the key constructs was checked using Cronbach’s alpha, and all constructs showed acceptable Cronbach alpha coefficient values. The Cronbach’s alpha coefficient scores for knowledge, attitude, and self-efficacy were 0.81, 0.92, and 0.86 respectively. The outcome of the study was maternal health service utilization practices, which included giving birth in a health facility, making eight ANC follow-up appointments, and attending Postnatal Care (PNC) follow-up seven days after giving birth [39].
The study assessed knowledge of maternal health care practices using 16 questions covering knowledge related to pregnancy, labor, delivery, and postpartum periods, with correct answers indicating greater understanding and a higher score indicating greater knowledge when the correct answers' scores were combined. Attitude toward maternal care practice was measured by 10 items with a 5-point Likert scale ranging from 1 for strongly disagree to 5 for strongly agree. The cumulative scores were used in the analysis once negatively phrased items were reverse-coded. A higher composite score indicated a more favorable attitude toward maternal care.
Self-efficacy in practicing maternal care refers to an individual`s belief in their ability to perform maternal care practices. It was measured by 10 items designed on a 5-point Likert scale ranging from 1 for strongly disagree to 5 for strongly agree. Once negatively worded items were reverse-coded, the sum score was used in the analysis. A higher score indicated greater self-efficacy in practicing maternal care.
The household wealth level was calculated using principal component analysis, taking into account 15 household asset properties and categorizing the household wealth index into wealth quintiles (lowest, second, middle, fourth, and highest).
Data collection methods
The data were collected via an interviewer-administered questionnaire by 21 (seven per district) data collectors who held at least a bachelor’s degree, were nursing school graduates with working experience in obstetric care, and were trained for three days. Each interview lasted for 45 min and was conducted based on the woman's preference. The data were checked for inconsistencies and errors during the data collection period by dedicated supervisors. To ensure accuracy and consistency, data collectors and supervisors received extensive preparatory training.
Data processing and analysis
The data were checked, cleaned, and entered into Epidata version 4.6 (released in 2020, Denmark) and exported to SPSS version 25 (released in 2017, USA) for analysis. The Hosmer and Lemeshow test was used to examine the model's goodness of fit; p-values greater than 0.05 indicated a good fit. We used descriptive statistics to summarize the data. Bivariate analysis was performed, and variables with p values less than 0.25 identified as candidates for inclusion in the multivariable logistic regression. A multivariable logistic regression model was used to identify the associations of independent variables with the study outcomes. A 95% confidence interval and p-value less than 0.05 were considered to indicate a statistically significant association.
Results
Demographic characteristics
The study included 588 women with a gestational age of 16–20 weeks (100% response rate). The individuals' background characteristics are shown in Table 1. Over three-quarters (85.4%) of the participants were between the ages of 20 and 34, and 66.2% resided in rural areas. Regarding occupations; 67.9% of the pregnant women were unemployed, while 85.4$ of their male partners were self-employed. The wealth distribution skewed toward the medium category, comprising 80.4% of the surveyed population.
Access factors and knowledge, attitudes, and self-efficacy (KASE)
Only 6.3% of the participants reported having immediate access to health facilities, whereas 30.8% reported moderate access (15–30 min). Additionally, 40.1% reported having reasonable access (30–60 min), and the remaining participants reported limited (60–90 min) and challenging (90 + minutes) access to health facilities.
Overall, for 59.2% of the women, walking was the primary mode of transportation to reach healthcare facilities; however, 31.1% had to pay for transportation. The majority (82.7%) of respondents had community-based health insurance. Most participants (93.2%) shared their opinions about not receiving respectful treatment, and approximately three-fourths (83.5%) reported having privacy when receiving services. However, 41% of respondents reported lengthy wait times. Only 42% of the respondents expressed a favorable attitude toward maternal health care.
Concerning the study participants' knowledge levels, 63.8% lacked adequate knowledge about maternal health care, and nearly half (53.1%) showed a high level of self-efficacy toward maternal health care.
A total of 6.1% of those in the gain frame, 4.6% in the loss frame, and 8.2% in the control arm had immediate access to healthcare facilities. Regarding the pattern of transportation, walking was widely relied upon by all groups. The control group had higher expenditures for transportation (41.3%) and healthcare services (53.6%). The gain-framed arm had a higher percentage of members with community-based health insurance (86.7%). Perceived respectful care was high (93.9%) among the gain-framed arms. More privacy experiences were found in the control group (92.9%). A greater percentage of participants in the loss-framed arm reported short waiting times (66.8%), whereas 51.5% of participants in the control arm experienced long waiting times (Table 2).
Literacy in using mobile phones
This relevant finding was from an accepted manuscript entitled `pregnant mother’s intention to use mobile phone-based messaging interventions for improving maternal and newborn health practices in Jimma Zone, Ethiopia’ which was part of cRCT. The study indicates a high level of literacy in mobile phone usage among pregnant women in Jimma Zone, Ethiopia. A substantial majority (79.9%) of the participants demonstrated the ability to read, with about half (54.1%) capable of sending mobile phone text messages. The majority (69.5%) of respondents had been using a mobile phone for 1 to 4 years. More than three-fourths (77.4%) of the respondents stated that a family member shares information they receive through their phone. Furthermore, nearly all respondents (98.9%) expressed a preference for receiving health information in Afan Oromo via text messages [40].
Experience in prenatal care
The majority (95.1%) of the study participants were multigravida. Regarding pregnancy outcomes, 93.4% of the pregnant mothers gave birth to live children, 3.6% to stillbirths, 2.0% to miscarriages, and 1.0% to abortions. The prevalence of antenatal care (ANC) attendance was 87.9% CI (73.2, 79.9). Concerning early ANC initiation, more than three-quarters (77.4%) of the women sought healthcare before 16 weeks. A limited frequency of ANC (≤ 4 times) was reported by the majority (88.2%) of the research participants.
Regarding counseling during ANC, 70% of respondents reported receiving information about delivery preparation, 63.4% about breastfeeding, 56.3% about spacing children, 61.9% about immunization, 60.0% about danger signs of pregnancy, and 58.8% about nutrition. The majority (82%) reported having received a tetanus toxoid (TT) vaccination. Only 31.5% of participants stated that they always use insecticide-treated nets (ITNs), 23.3% reported using them occasionally, 12.2% seldom, and 33.0% never.
Regarding the range of services offered to pregnant mothers during routine antenatal care, 81.2% of the women reported having their blood pressure taken, 65.8% had urine samples collected, 61.1% had blood samples taken, 73.9% listened to the baby's heartbeat, and 62.5% reported assessing danger signs. A majority of respondents (90.1%) reported logistical challenges as their reason for not using ANC, and 87.3% mentioned perceived inefficiency or lack of necessity. The majority (97.1%) of the women received fewer than 90 tablets of iron folate.
When we compared ANC attendance among the three arms, the gain-framed arm had lower attendance (85.7%) than both the control arm (86%) and the loss-framed arm (91.8%). In terms of when the first ANC visit occurred, 68.5% of the participants in the gain-framed arm, 83.3% in the loss-framed arm, and 79.9% in the control arm started before 16 weeks. In terms of ANC frequency, 81.5% of the gain-framed arms, 95% of the loss-framed arms, and 87.6% of the control arms had limited ANC (≤ 4 times).
Regarding reasons for ANC nonattendance, logistical barriers were high across arms: gain-framed (96.4%), loss-framed (87.5%), and control (85.2%). Resource limitations were another challenge, with the gain-framed arm at 82.1%, the loss-framed arm at 81.3%, and the control arm at 88.9%. Conversely, perceived ineffectiveness was high for the loss-framed arm (93.8%) and control arm (92.6%) (Table 3).
Experience in intrapartum care
Most (74.7%) CI (73.2, 79.9) births occurred in a health facility. The majority of births (97.1%) were vaginal, with 1.5% and 1.4% born via cesarean section (CS) and forceps/vacuum extraction, respectively. The top three reasons women chose not to give birth in a health institution were financial challenges (94.0%), personal/informational barriers (84.6%), and logistical barriers (92.6%). The majority (95.4%) of respondents reported that they prepared for birth, mainly by saving money. Less than half (30.1%) of the women experienced serious health problems during pregnancy, labor, or birth, with severe bleeding (11.9%) and severe headaches (9.2%) being the most commonly reported issues.
Health centers were the preferred location for deliveries, with the gain-framed arm at 65.3%, the loss-framed arm at 62.8%, and the control arm at 71.4%. The gain-framed arm had a greater percentage of home deliveries (31.6%) than did the control arm (17.3%) and loss-framed arm (27%). Logistic barriers to giving birth at health facilities were more prominent in the gain-framed arm (89.3%) than in the loss-framed arm (67.7%) and control arm (72%). Informational barriers were greater in the control arm (33.1%) than in the gain-framed arm (15%) and the loss-framed arm (16.8%). Birth preparedness was greater in the control arm (79.6%) than in the gain-framed arm (61.7%) and the loss-framed arm (74%). Serious health problems during pregnancy, labor, or birth were comparable across arms; 25% of the participants were in the gain-framed arm, 32.7% in the loss-framed arm, and 32.1%in the control arm. Unweighted births were more prevalent in the gain-framed arm (51%) than in the loss-framed arm (40.3%) and control arm (36.2%) (Table 4).
Experience in postpartum care
Most (60.4%) of the respondents reported having received postnatal check-ups. Regarding the length of stay in the health facility for postnatal care (PNC), approximately half (51.5%) stayed less than 24 h. The majority (81.1%) of the participants received postnatal check-ups within the first 24 h. This study showed that only 28% of those who gave birth at home received postnatal check-ups. The most noted postnatal services mentioned by women were; taking temperature (43.0%), recognizing the baby's urgent needs (36.2%), observing breastfeeding (39.1%), measuring blood pressure (42.3%), assessing vaginal bleeding (43.4%), and family planning (42.3%).
By comparing postnatal care checks along the three arms, we found that the gain-framed arm had the highest proportion (64.8%), followed by the loss-framed arm (58.7%) and the control arm (57.7%). Regarding the timing of postnatal checks, immediate postnatal checks were notably more frequent in the gain-framed arm (30.7%) than in the loss-framed (8.7%) and control (13.3%) arms (Table 5).
Experiences with messages on maternal health
Most (66%) study participants reported that they had heard of maternal health (MH) messages. Traditional media was the primary source of health messages for approximately 63.8% of the study participants, followed by healthcare professionals (46.9%), community health workers (33.2%), family members (24.3%), friends (24.7%), and other sources (23%). Regarding exposure frequency, 31.5% reported frequent exposure, 16.2% sometimes, 16.2% occasionally, 32.5%, rarely, and 19.9% never. Approximately 29.6% of respondents actively sought information, 37.4% relied heavily on incoming sources, and 33% utilized both approaches.
In comparing the three arms regarding maternal health message exposure and information-seeking behavior, similar exposure rates were observed, with 67.9% in the gain-framed group, 65.8% in the loss-framed group, and 64.3% in the control group. Conventional media was the primary source across all arms, reaching 67.9%, 70.9%, and 52.6% in the gain-framed, loss-framed, and control arms, respectively. The frequency of message exposure varied significantly, with 42.9% in the gain-framed group, 18.9% in the loss-framed group, and 32.7% in the control group reporting frequent exposure. Information-seeking behavior showed disparities, as 41.3% of participants in the gain-framed group actively sought information, whereas 28.6% of those in the loss-framed group and 18.9% of those in the control group did (Table 6).
Factors associated with maternal health service use
Twenty-three variables were independently entered into the bivariable logistic regression analysis using an enter method, and 11 of them demonstrated an association with the dependent variable at a p-value < 0.25. Variables that were associated with the dependent variable at the bivariate level were simultaneously adjusted in binary logistic regression. The educational level of pregnant women, wealth category, means of transportation, knowledge of maternal healthcare, self-efficacy in maternal healthcare, and exposure to maternal health messages didn’t show significant association with the dependent variable. On the other hand, proximity to the health facility, transportation cost, perceived respectful care, privacy during procedures, and attitude toward maternal health service showed significant association.
Multivariable logistic regression results showed that women with immediate access were significantly more likely to utilize maternal health services. They had 6.6 times higher odds of using these services compared to those with challenging access [AOR = 6.6, 95% CI: 2.39, 18.16], with a highly significant p-value of less than 0.001. This indicates that proximity to health facilities greatly increases the likelihood of maternal health service utilization. Women with moderate access had 2.2 times higher odds of utilizing maternal health services compared to those with challenging access [AOR = 2.2, 95% CI: 1.00, 5.32], with a marginally significant p-value of 0.08. Although the relationship is not as strong as for immediate access, moderate proximity still positively influences service utilization. Reasonable access was also positively associated with maternal health service utilization. Women in this category were 2.6 times more likely to use maternal health services compared to those with challenging access [AOR = 2.6, 95% CI: 1.10, 6.27], with a significant p-value of 0.02.
Women who did not experience economic hardship were three times more likely to utilize maternal health services than those who did [AOR = 3, (95% CI: 1.97, 4.61)], with a highly significant relationship (p < 0.001). Women who received respectful care were 2.3 times more likely to use maternal health services compared with those who reported non-respectful care [AOR = 2.3, (95% CI: 1.07, 5.11)], with a significant relationship (p = 0.03). Women who received private care had 2.4 times higher odds of utilizing maternal health services compared to those who did not have private care [AOR = 2.4, 95% CI: 1.47, 4.06], with a highly significant p-value of less than 0.001. This indicates the importance of privacy in healthcare settings to promote service use.
Women with a favorable attitude towards maternal healthcare were 2.2 times more likely to utilize maternal health services compared to those with an unfavorable attitude [AOR = 2.2, 95% CI: 1.48, 3.24], with a highly significant p-value of less than 0.001. A positive attitude towards healthcare is thus a significant motivator for service utilization (Table 7).
Discussion
The utilization of maternal health services plays a crucial role in decreasing maternal mortality rates. Research has indicated that improved utilization of maternal health services, such as receiving care from skilled attendants during childbirth, is strongly linked to improved maternal survival rates [41,42,43].
According to the current study, the overall maternal health service utilization was 54.4%, 87.9% of mothers attended antenatal care, 74.7% used institutional delivery, and 60.4% used postnatal care. Higher utilization rates are observed for antenatal care compared with the global average (81%), whereas institutional delivery and postnatal care show lower utilization rates compared with the global average (81%) [44]. Additionally, a pooled analysis of demographic and health surveys across 32 sub-Saharan African countries revealed varying levels of skilled antenatal care service utilization, ranging from 99.2% in Gambia to 8.4% in Burundi [45]. Furthermore, a study in Ethiopia showed that 62% of pregnant women received antenatal care, 48% opted for institutional delivery, and 34% received postnatal care [46]. The data suggest a relatively high utilization of maternal health services, low early ANC utilization, and a high service dropout rate in the Jimma Zone, which could be attributed to challenges related to accessibility, geographical disparities, infrastructure limitations, or sociocultural factors influencing healthcare-seeking behavior.
The result from the complementary study showed that 79.9% of the respondents can read mobile text messages, while only 54.1% of them can send them. This finding is comparable with a study conducted in India, where only 52.5% of the participants could type and send text messages [47]. However, it is lower than the finding of study conducted in northern Ethiopia, where 91% and 87.3% of participants could read and send mobile text messages, respectively [48]. The difference might be due to variations in educational status of study participants. Although only about half of the participants in the study were able to send a text message, four out of five could read them, which would make a mobile phone-based messaging intervention feasible. The complementary study also showed that nearly all respondents (98.9%) preferred receiving health information in Afan Oromo via text messages, underscoring the importance of language and cultural relevance in mobile health interventions. The preference for receiving message in the common language of their locality was also reported by the majority of participants in other studies [47, 48]. The findings suggests the widespread accessibility and acceptance of mobile technology among pregnant women in Jimma Zone.
Addressing challenges such as network issues and costs is crucial for maximizing the effectiveness of mobile health interventions. In contexts where network reliability can be a barrier, employing alternative communication methods such as volunteers and health extension workers could significantly enhance the effectiveness of the intervention. These strategies can facilitate direct communication with pregnant women in local communities, ensuring that health information reaches those who may have limited access to mobile networks or digital literacy. Volunteers and health extension workers can also provide personalized support, answer questions, and reinforce health messages in culturally appropriate ways, thereby enhancing engagement and adherence to health advice. Integrating these additional support mechanisms into existing mobile health strategies not only addresses infrastructural challenges but also strengthens community-based healthcare delivery, ultimately improving maternal and child health outcomes.
The current study revealed that proximity to health facilities was an independent predictor of maternal health service utilization; hence, women with immediate access, reasonable access, moderate, and limited access were more likely to utilize maternal health services than women with challenging access. This result aligns with a study in Nepal which found that geographical barriers significantly affected the utilization of maternal health services, with women living in mountainous and remote areas less likely to access antenatal care and skilled birth attendance compared to those in more accessible areas [49], a study in India, which showed that distance to health facilities was a major determinant of whether women opted for institutional deliveries, with those residing in rural areas facing greater challenges in accessing these services [50], findings from a systematic review on maternal care barriers in African low-income countries [51], a study in sub-Saharan Africa [52], a study in Tanzania which showed that women residing more than five kilometers from a healthcare facility were notably less likely to attend four or more antenatal care visits [53], findings from Kenya, where proximity to healthcare facilities was one of the strongest predictors of maternal health service utilization [54]; these studies highlighted the significant impact of access on the utilization of maternal health services. This suggests that as the distance to health facility increases, the likelihood of women utilizing maternal health services decreases. It also stresses the critical role of addressing geographical inequities and enhancing access to health facilities to improve maternal health service use.
Limited financial resources can affect the ability to access maternal health services. The current study revealed that women without a financial burden demonstrated greater odds of using maternal health services than those who experienced economic hardship. This finding aligns with earlier studies that have recognized economic hardships as a major obstacle in obtaining maternal healthcare in low- and middle-income nations [51, 55], a study in Bangladesh, found that financial constraints significantly influenced the decision to seek maternal health services, with many women unable to afford the costs associated with healthcare visits, medications, and necessary tests [56], a study in India, found that financial limitations were a critical barrier to maternal health service utilization. Women from poorer households were less likely to access institutional deliveries and postnatal care due to the costs associated with these services [57], a study in Uganda highlighted that economic hardship was a major factor affecting maternal health service utilization [58], and research in Pakistan also demonstrated that financial barriers were a major obstacle to accessing maternal health services [59]. Improving access to maternal healthcare services requires addressing these barriers and empowering women through education and equitable healthcare access. This challenge could be attributed to male dominance and a lack of autonomous decision-making among the study population. Overcoming these obstacles and ensuring equal access to healthcare are crucial steps in enhancing maternal healthcare services.
Respectful care was another significant factor in maternal health service use. Based on the results of the current study conducted in the Jimma Zone, women who experienced respectful care had greater odds of utilizing maternal health services. This finding supports a study conducted by Sheferaw ED [60], where the absence of respectful maternity care was recognized as restrictive to the utilization of maternity services, another study conducted by Kawish AB [61] also showed that the provision of respectful care plays a crucial role in promoting health-seeking behaviors among pregnant women. A study in Ethiopia found that respectful maternity care, including effective communication, emotional support, and maintaining the dignity of the mother, significantly increased the likelihood of women seeking skilled birth attendance and postnatal care [62]. In Tanzania, research revealed that women who experienced disrespectful care, including being scolded or ignored by healthcare providers, were less likely to return to health facilities for postnatal care or future deliveries [63]. A study in Kenya identified disrespectful and abusive care during childbirth as a major barrier to maternal health service utilization, with instances of verbal abuse, physical mistreatment, and lack of informed consent, discouraging women from seeking care at health facilities for subsequent pregnancies [64]. Similarly, a study In Latin America, Mexico reported that women who felt respected and valued during their interactions with healthcare providers were more likely to attend antenatal care and deliver in health facilities [65]. The absence of respectful care in the area may have contributed to a lack of discharge accountability by healthcare providers. Therefore, ensuring a dignified and respectful working environment could contribute to an increase in health facility delivery and a reduction in maternal mortality.
Maintaining privacy and confidentiality during examinations and procedures is one of the 12 domains of respectful maternity care [66]. According to the current study, women who reported private procedures had 2.4 times greater odds of using maternal health services. This finding is supported by, another study in Ethiopia, which found that women who perceived their consultations and procedures as private and confidential were more likely to seek skilled birth attendance and complete their postnatal care regimen [67]. In Nepal maintaining privacy during maternity care was a key factor influencing women's decisions to seek institutional delivery and postnatal care [68]. Similarly, a study in Brazil showed that women who experienced respectful care with maintained privacy during childbirth had higher odds of utilizing maternal health services [69]. In Nigeria women who reported that their privacy was maintained during childbirth were more likely to return for postnatal care and recommend institutional delivery to others [70], A cross-sectional study conducted in the Kingdom of Saudi Arabia that explored the occurrence of respect perceived by women giving birth and its effect on maternal health service utilization [71]. This study highlights the importance of ensuring privacy and confidentiality in healthcare services, particularly in maternity care.
Finally, women with a favorable attitude toward maternal healthcare demonstrated greater odds of using maternal health services. Similarly, a study in rural Ethiopia revealed that women's attitudes toward maternal health services were significantly associated with their intentions to use maternal health services [72]. In Bangladesh, women’s attitudes toward maternal health services played a crucial role in their utilization, with positive attitudes were associated with increased attendance at antenatal care visits and higher rates of institutional deliveries [73]. A study in Kenya found that women with positive attitudes toward maternal health services were more likely to utilize antenatal, delivery, and postnatal care. Health education programs aimed at improve perceptions of maternal health services were shown to be effective in increasing service utilization [74]. Poor attitudes toward maternal health services might have been due to the low literacy rate in the area and previous negative experiences. This underscores the importance of addressing factors that that shape women`s attitudes toward maternal healthcare.
Limitation of the study
This study has some limitations that should be considered when interpreting its findings. Gestational age was determined based on the last menstrual period (LMP) and fundal height, which may be inaccurate due to irregular menstrual periods, oligohydramnios, or polyhydramnios. Additionally, the research did not investigate maternal–fetal diseases and abnormal placental transplantation, potentially limiting the comprehensive understanding of maternal health outcomes. Another limitation is the focus on pregnant mothers or pregnant mother’s families who own a mobile phone, which may overlook those without access to mobile technology.
Conclusion
Although antenatal care attendance was high, early initiation of antenatal care was low with high dropout rates. Most births occurred at healthcare facilities, and postnatal service utilization was relatively high; however, some mothers gave birth at home and did not attend postnatal care. Factors significantly affecting maternal health service utilization included access to health facilities, economic hardship, perceived respectful care, privacy, and attitudes toward maternal health.
A knowledge gap in maternal health care was evident, with many participants lacking sufficient information. Additionally, a large percentage of pregnant mothers had unfavorable attitudes and low self-efficacy regarding maternity care. Conventional media was the primary source of maternal health information, highlighting the need for tailored communication strategies. Addressing barriers such as distance, transportation costs, respectful care, privacy, knowledge gaps, attitudes, and self-efficacy is crucial for improving maternal healthcare services, requiring tailored interventions to meet the unique needs of diverse groups.
Future research should include an assessment of materno-fetal characteristics and consider studies in which all pregnant women are provided with mobile phones, which would minimize selection bias and allow for a more equitable assessment of maternal health care across socioeconomic groups.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- ANC:
-
Antenatal care
- ANC1:
-
First antenatal care visit
- ANC4:
-
Fourth antenatal care visit
- CI:
-
Confidence interval
- CS:
-
Cesarean section
- DE:
-
Design effect
- GA:
-
Gestational age
- ICC:
-
Interclass correlation
- KASE:
-
Knowledge, attitude and self-efficacy
- LLITN:
-
Long lasting integrated treated nets
- LMP:
-
Last menstrual period
- MH:
-
Maternal health
- MMR:
-
Maternal mortality ratio
- PHCU:
-
Primary health care unit
- PNC:
-
Postnatal care
- SDG:
-
Sustainable development goal
- SPSS:
-
Software package for social science
- TBA:
-
Traditional birth attendance
- TT:
-
Tetanus toxoid
- WHO:
-
World health organization
References
Sajedinejad S, Majdzadeh R, Vedadhir AA, Tabatabaei MG, Mohammad K. Maternal mortality: A cross-sectional study in global health. Global Health. 2015;11(1):1–13.
WHO. Maternal, newborn, child and adolescent health, and ageing. Geneva: World Health Organization; 2022:23–4.
Musarandega R, Nyakura M, Machekano R, Pattinson R, Munjanja SP. Causes of maternal mortality in SubSaharan Africa: A systematic review of studies published from 2015 to 2020. J Glob Health. 2021;11:1–11.
Onambele L, Ortega-Leon W, Guillen-Aguinaga S, Forjaz MJ, Yoseph A, Guillen-Aguinaga L, et al. Maternal Mortality in Africa: Regional Trends (2000–2017). Int J Environ Res Public Health. 2022;19(20):13146.
WHO. Africa’s advances in maternal, infant mortality face setbacks: WHO report. 2023;(December 2022):1–6. Available from: https://www.afro.who.int/news/africas-advances-maternal-infant-mortality-face-setbacks-who-report.
Wilson Center. Approximately 70 percent of all maternal deaths occur in sub-Saharan Africa. 2023.
United Nations. The sustainable development goals report 2023 special edition. Sustain Dev Goals Rep. 2023:37–9. Available from: https://sdgs.un.org/sites/default/files/2023-07/The-Sustainable-Development-Goals-Report-2023_0.pdf.
Emi Suzuki, Charles K, Samuel M. Progress in reducing maternal mortality has stagnated and we are not on track to achieve the SDG target: new UN report. World Bank Blogs; 2023. p. 1–8. Available from: https://blogs.worldbank.org/opendata/progress-reducing-maternal-mortality-has-stagnated-and-we-are-not-track-achieve-sdg-target.
World Health Organization. SDG Target 3.1 Maternal mortality. Who. 2023;1–7. Available from: https://www.who.int/data/gho/data/themes/topics/sdg-target-3-1-maternal-mortality
Huck W. Goal 3 Ensure healthy lives and promote well-being for all at all ages. Sustain Dev Goals. 2023;2–4.
Ethiopian Public Health Institute (EPHI), ICF. Ethiopia mini demographic and health survey 2019: final report. 2021. p. 1–207. Available from: https://dhsprogram.com/pubs/pdf/FR363/FR363.pdf.
Alamirew WG, Belay DB, Zeru MA, Derebe MA, Adegeh SC. Prevalence and associated factors of neonatal mortality in Ethiopia. Sci Rep. 2022;12(1):1–11. https://doi.org/10.1038/s41598-022-16461-3.
Stevens GA, Finucane MM, Paciorek CJ. Levels and trends in low height-for-age. In: Dis control priorities, third ed (volume 2) reprod matern newborn, child heal. 2016. p. 85–93.
Alemayehu M, Gebrehiwot TG, Medhanyie AA, Desta A, Alemu T. Utilization and factors associated with antenatal, delivery and postnatal Care Services in Tigray Region, Ethiopia: a community-based cross-sectional study. BMC Pregnancy and Childbirth. 2020;20(1):1–13.
Berri KM, Adaba YK, Tarefasa TG, Bededa ND, Fekene DB. Maternal health service utilization from urban health extension professionals and associated factors among women who gave birth in the last one year in Ambo town, Oromia regional state, Ethiopia, 2018. 2020. p. 1–10.
Shiferie F, Abate FW, Shifraw T, Eglovitch M, Amanuel H, Chan GJ, et al. Health care seeking behaviors of pregnant women in rural Amhara, Ethiopia: a qualitative study of perceptions of pregnant women, community members, and health care providers. Pan Afr Med J. 2023;45:142.
The ETO. Maternal and obstetric care challenges in rural America; policy brief and recommendations to the secretary. 2020.
CMS. Improving access to maternal health care in rural communities; issue brief. 2022.
March T, Maternity D, Desert C. Barriers to improving rural maternal health. 2022. p. 3–5.
Dantas JAR, Singh D, Lample M. Factors affecting utilization of health facilities for labour and childbirth: A case study from rural Uganda. BMC Pregnancy Childbirth. 2020;20(1):1–10.
World Health Organization. Standards for improving quality of maternal and newborn care in health facilities. Geneva: Who; 2016. p. 73.
Tanou M, Kishida T, Kamiya Y. The effects of geographical accessibility to health facilities on antenatal care and delivery services utilization in Benin: a cross-sectional study. Reprod Health. 2021;18(1):1–11. https://doi.org/10.1186/s12978-021-01249-x.
Id RK. Adopting Andersen’s behavior model to identify factors influencing maternal healthcare service utilization in Bangladesh. 2021. p. 1–18. https://doi.org/10.1371/journal.pone.0260502.
Bain LE, Aboagye RG, Malunga G, Amu H, Dowou RK, Saah FI, et al. Individual and contextual factors associated with maternal healthcare utilisation in Mali: A cross-sectional study using Demographic and Health Survey data. BMJ Open. 2022;12(2):1–10.
Huda TM, Chowdhury M, El AS, Dibley MJ. Individual and community level factors associated with health facility delivery: A cross sectional multilevel analysis in Bangladesh. PLoS ONE. 2019;14(2):1–13.
Adedokun ST, Uthman OA. Women who have not utilized health Service for Delivery in Nigeria : who are they and where do they live ? 2019;6:1–14.
National Academies of Sciences Engineering and Medicine. Systemic influences on outcomes in pregnancy and childbirth. In: Birth Settings in America: outcomes, quality, access, and choice. 2020. https://doi.org/10.17226/25636.
HRSA Health Workforce. State of the maternal health workforce brief. 2022. Available from: https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/maternal-health-workforce-brief-2022.pdf.
Hagaman A, Rodriguez HG, Barrington C, Singh K, Estifanos AS, Keraga DW, et al. “Even though they insult us, the delivery they give us is the greatest thing”: a qualitative study contextualizing women’s experiences with facility-based maternal health care in Ethiopia. BMC Pregnancy Childbirth. 2022;22(1):1–15. https://doi.org/10.1186/s12884-022-04381-z.
Konlan KD, Saah JA, Amoah RM, Doat AR, Mohammed I, Abdulai JA, et al. Factors influencing the utilization of Focused antenatal care services during pregnancy, a study among postnatal women in a tertiary healthcare facility. Ghana Nurs Open. 2020;7(6):1822–32.
Omer S, Zakar R, Zakar MZ, Fischer F. The influence of social and cultural practices on maternal mortality: a qualitative study from South Punjab, Pakistan. Reprod Health. 2021:1–12. https://doi.org/10.1186/s12978-021-01151-6.
Mahiti GR, Mkoka DA, Kiwara AD, Mbekenga CK, Hurtig A karin, Goicolea I, et al. Women’s perceptions of antenatal, delivery, and postpartum services in rural Tanzania. 2015. p. 9716.
UNICEF. UNICEF: collecting water is often a colossal waste of time for women and girls. 2020. p. 1–7.
Bulcha G, Abdissa HG, Noll J, Sori DA, Birhanu Z. Effectiveness of mobile phone messaging based message framing intervention for improving maternal health service uptake and new-born care practice in Rural Jimma Zone, Ethiopia: protocol for cluster randomized controlled trial. HMIR Res Protoc. 2024. Available from: https://preprints.jmir.org/preprint/52395.
Bourke L, Hooper R, Bourke L. Cluster randomised trials with repeated cross sections: alternatives to cluster randomised trials with repeated cross sections: alternatives to parallel group designs. 2015.
Atnafu A, Otto K, Herbst CH. The role of mHealth intervention on maternal and child health service delivery: findings from a randomized controlled field trial in rural Ethiopia. mHealth. 2017;3:39.
Taljaard M, Donner A, Villar J, Wojdyla D, Velazco A, Bataglia V, et al. Intracluster correlation coefficients from the 2005 WHO Global Survey on Maternal and Perinatal Health: Implications for implementation research. Paediatr Perinat Epidemiol. 2008;22(2):117–25.
Hooper R, Teerenstra S, de Hoop E, Eldridge S. Sample size calculation for stepped wedge and other longitudinal cluster randomised trials. Stat Med. 2016;35(26):4718–28.
Dettrick Z, Gouda HN, Hodge A, Jimenez-Soto E. Measuring quality of maternal and newborn care in developing countries using demographic and health surveys. PLoS ONE. 2016;11(6):1–20.
Hordofa Gutema Abdissa, GB Duguma, Fira Abamecha Ababulgu, Kebede Lemu, Mulusew Gerbaba JN, Demisew Amenu Sori, ZBK. Pregnant mother’s intention to use mobile phone-based messaging interventions for improving maternal and newborn health practices in Jimma Zone, Ethiopia. BMC. 2024. https://doi.org/10.1186/s44247-024-00094-9.
Vizheh M, Rapport F, Braithwaite J, Zurynski Y. The Impact of Women’s Agency on Accessing and Using Maternal Healthcare Services: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2023;20(5):3966.
Elmusharaf K, Byrne E, Donovan DO. Strategies to increase demand for maternal health services in resource-limited settings : challenges to be addressed. BMC Public Health. 2015:1–10. https://doi.org/10.1186/s12889-015-2222-3.
Howell. Reducing disparities in severe maternal morbidity and mortality. Clin Obstet Gynecol. 2018;61(2): 387–399. https://doi.org/10.1097/GRF.0000000000000349. Physiol Behav. 2016;176(1):100–106.
WHO. Coverage of skilled birth attendance, observatory, global health. 2024. p. 1–2.
Dickson KS, Okyere J, Ahinkorah BO, Seidu AA, Salihu T, Bediako V, et al. Skilled antenatal care services utilisation in sub-Saharan Africa: a pooled analysis of demographic and health surveys from 32 countries. BMC Pregnancy Childbirth. 2022;22(1):831.
Kitaw TA, Haile RN. Time to first antenatal care booking and its determinants among pregnant women in Ethiopia: survival analysis of recent evidence from EDHS 2019. BMC Pregnancy Childbirth. 2022;22(1):1–11. https://doi.org/10.1186/s12884-022-05270-1.
Datta SS, Ranganathan P, Sivakumar KS. A study to assess the feasibility of text messaging service in delivering maternal and child healthcare messages in a rural area of Tamil nadu, India. Australas Med J. 2014;7(4):175–80.
Mekonnen ZA, Gelaye KA, Were MC, Tilahun B. Mothers intention and preference to use mobile phone text message reminders for child vaccination in Northwest Ethiopia. BMJ Heal Care Informatics. 2021;28(1):1–9.
Simkhada B, Van Teijlingen ER, Porter M, Simkhada P. Major problems and key issues in maternal health in Nepal. Kathmandu Univ Med J. 2006;4 NO. 2(14):258–63.
Kumar S, Dansereau EA, Murray CJL. Does distance matter for institutional delivery in rural India? Appl Econ. 2014;46(33):4091–103.
Dahab R, Sakellariou D. Barriers to accessing maternal care in low income countries in Africa: A systematic review. Int J Environ Res Public Health. 2020;17(12):1–17.
Doctor HV, Nkhana-salimu S. Health facility delivery in sub-Saharan Africa: successes, challenges , and implications for the 2030 development agenda. 2018. p. 1–12.
Kibesa SJ, Kitua YW, Kitua DW. Determinants of Antenatal Healthcare Services Utilisation: A Case of Dodoma, Tanzania. East Afr Health Res J. 2022;6(2):155–61. https://doi.org/10.24248/eahrj.v6i2.701.
Gitonga E, Muiruri F. Determinants of health facility delivery among women in Tharaka Nithi county, Kenya. Pan Afr Med J. 2016;25(Supp 2):9.
Yadav AK, Sahni B; Jena PK. Education, employment, economic status and empowerment: Implications for maternal health care services utilization in India. J Public Aff. 2020. https://doi.org/10.1002/pa.2259.
Hajizadeh M, Alam N, Nandi A. Social inequalities in the utilization of maternal care in Bangladesh: Have they widened or narrowed in recent years? Int J Equity Health. 2014;13(1):1–11.
Singh S, Rajak R. Barriers in utilization and provisioning of obstetric care services (OCS) in India: a mixed-methods systematic review. BMC Pregnancy Childbirth. 2024;24(1):1–14.
Rutaremwa G, Wandera SO, Jhamba T, Akiror E, Kiconco A. Determinants of maternal health services utilization in Uganda. BMC Health Serv Res. 2015;15(1):1–8.
Midhet F, Hanif M, Khalid SN, Khan RS, Ahmad I, Khan SA. Factors associated with maternal health services utilization in Pakistan: Evidence from Pakistan maternal mortality survey, 2019. PLoS One. 2023;18(11 November):1–11. https://doi.org/10.1371/journal.pone.0294225.
Sheferaw ED, Mengesha TZ, Wase SB. Development of a tool to measure women’s perception of respectful maternity care in public health facilities. BMC Pregnancy Childbirth. 2016;16(1):1–8. https://doi.org/10.1186/s12884-016-0848-5.
Kawish AB, Umer MF, Arshed M, Khan SA, Hafeez A, Waqar S. Respectful maternal care experience in low- and middle-income countries: a systematic review. Medicina (B Aires). 2023;59(10). Available from: https://www.mdpi.com/1648-9144/59/10/1842.
Habte A, Tamene A, Woldeyohannes D, Endale F, Bogale B, Gizachew A. The prevalence of respectful maternity care during childbirth and its determinants in Ethiopia: A systematic review and meta-analysis. PLoS One. 2022;17(11 November):1–23. https://doi.org/10.1371/journal.pone.0277889.
Kruk ME, Kujawski S, Mbaruku G, Ramsey K, Moyo W, Freedman LP. Disrespectful and abusive treatment during facility delivery in Tanzania: A facility and community survey. Health Policy Plan. 2018;33(1):e26-33.
Abuya T, Warren CE, Miller N, Njuki R, Ndwiga C, Maranga A, et al. Exploring the prevalence of disrespect and abuse during childbirth in Kenya. PLoS ONE. 2015;10(4):1–13.
Makdisse M, Ramos P, Malheiro D, Katz M, Novoa L, Cendoroglo Neto M, et al. Value-based healthcare in Latin America: a survey of 70 healthcare provider organisations from Argentina, Brazil, Chile, Colombia and Mexico. BMJ Open. 2022;12(6):e058198.
Esan OT, Maswime S, Blaauw D. A qualitative inquiry into pregnant women’s perceptions of respectful maternity care during childbirth in Ibadan Metropolis, Nigeria. Sex Reprod Health Matters. 2022;30(1):2056977. https://doi.org/10.1080/26410397.2022.2056977.
Zeleke AM, Bayeh GM. Compassionate and respectful maternity care for mothers who gave birth in public health facilities in North Gondar, Ethiopia: a cross-sectional study. Afr J Midwifery Womens Health. 2022;16(3):1–14.
Khatri RB, Karkee R. Social determinants of health affecting utilisation of routine maternity services in Nepal: a narrative review of the evidence. Reprod Health Matters. 2018;26(54):32–46. https://doi.org/10.1080/09688080.2018.1535686.
Leite TH, Carvalho TDG, Marques ES, Pereira APE, da Silva AAM, Nakamura-Pereira M, et al. The association between mistreatment of women during childbirth and postnatal maternal and child health care: Findings from “Birth in Brazil.” Women and Birth. 2022;35(1):e28-40. Available from: https://www.sciencedirect.com/science/article/pii/S1871519221000354.
Idris S, Sambo M, Ibrahim M. Barriers to utilisation of maternal health services in a semi-urban community in northern Nigeria: The clients′ perspective. Niger Med J. 2013;54(1):27.
Alghamdi RS, Perra O, Boyle B, Stockdale J. Perceived treatment of respectful maternity care among pregnant women at healthcare facilities in the Kingdom of Saudi Arabia: A cross-sectional study. Midwifery. 2023;123:103714 . Available from: https://www.sciencedirect.com/science/article/pii/S0266613823001171.
Taye BT, Kebede AA, Wondie KY. Intention to use maternal health services and associated factors among women who gave birth at home in rural Sehala Seyemit district: a community-based cross-sectional study. BMC Pregnancy Childbirth. 2022;22(1):1–12. https://doi.org/10.1186/s12884-022-04447-y.
Afroz S, Sutopa TS, Haque MR. Young mothers’ attitudes towards domestic violence and their maternal healthcare services utilization in Bangladesh: A multilevel cluster analysis. PLoS ONE. 2022;17(8):e0268062.
Njuguna J, Kamau N, Muruka C. Impact of free delivery policy on utilization of maternal health services in county referral hospitals in Kenya. BMC Health Serv Res. 2017;17(1):1–6.
Acknowledgements
The study team extends heartfelt gratitude to the Jimma Zone Health Office for their unwavering support. We also appreciate the study participants for their valuable contributions and the time they generously dedicated to this research.
Funding
This work was carried out with grants from Jimma University for postgraduate students and small grants from institute of health, department of health, behaviour and society; it does not necessarily reflect the interest of these organizations.
Author information
Authors and Affiliations
Contributions
GB contributed to the inception, design, data acquisition, analysis, and manuscript writing. HG was involved in the inception, design, data acquisition, and critical review of the manuscript. DA participated in the design, data collection, and review of the manuscript. ZB was involved in the design process, data acquisition, and critical review of the manuscript. The final manuscript was read and approved by all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approvals were obtained from the Ethical Review Committee of Jimma University and Jimma Zonal Health Office to conduct a baseline survey research on pregnant women between 16–20 gestational age as part of a cluster randomized controlled trial (cRCT). Every study participant provided written consent prior to data collection and their individual information remains confidential. The consent procedure for all pregnant women has been approved by the Ethical Review Committee. This assessment is the initial step in a mobile phone messaging intervention study, with no negative impact on the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bulcha, G., Gutema, H., Amenu, D. et al. Maternal health service utilization in the Jimma Zone, Ethiopia: results from a baseline study for mobile phone messaging interventions. BMC Pregnancy Childbirth 24, 485 (2024). https://doi.org/10.1186/s12884-024-06683-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06683-w