Abstract
Background
The Continuum of care for reproductive, maternal, newborn, and child health includes integrated service delivery for mothers and children from pre-pregnancy to delivery, the immediate postnatal period, and childhood. In Ethiopia, the magnitude of antenatal care, skilled delivery, postnatal care, and immunization for children have shown improvement. Despite this, there was limited research on the percentage of mothers who have completed maternal and child continuum care.
Objective
To assess the Completion of Maternal and Child Health Continuum of Care and Associated Factors among women in Gode District, Shebele Zone, Eastern Ethiopia ,2022.
Method
A community-based cross-sectional study design applied from November 1–15, 2022. A stratified sampling method was applied. A woman who had two 14–24 months child preceding the data collection period were included in the study. An interviewer-administered semi-structured questioner had been used for data collection. Data collected by using kobo collect and analyzed using STATA version 17. Both Bivariable and multivariable logistic regression analyses were done. In multivariable analysis, variables having P-values ≤ 0.05 were taken as factors associated with the completion of the maternal and child health continuum of care.
Result
The Completion of maternal and child continuum of care was 13.5% (10.7-17.0%) in Gode district,2022. Accordingly, Husband occupation (Government employee) [AOR = 2.3, 95%CI 1.2–4.7] and perceived time to reach health facility (less than 30 min) [AOR = 2.96, 95%CI 1.2–7.5] were factors showing significant association with maternal and child health continuum of care among mothers in Gode district, Somali regional State;2022 at P-value ≤ 0.05.
Conclusion and recommendation
Only 13.5% of mothers in Gode district received all of the recommended maternal and child health services during their pregnancy, childbirth, and postpartum period. The study found that two factors were associated with a higher likelihood of receiving Maternal and child continuum of care: Government employed husband and perceived time to reach a health facility. Governments can play a key role in increasing the maternal and child health continuum of care by investing by making health care facility accessible.
Similar content being viewed by others
Introduction
The Continuum of Care for reproductive, maternal, newborn, and child health (RMNCH) includes integrated service delivery for mothers and children from pre-pregnancy to delivery, the immediate postnatal period, and childhood [1]. Continuum of care(COC) is one of the important long-term plans for reducing maternal and neonatal deaths and improving the health and well-being of mothers and newborns [2, 3].
Despite global advocacy by the World Health Organization (WHO) and its allies for a continuum of care (CoC) approach to improve maternal, newborn, and child health (MNCH) outcomes, with policies like Ethiopia’s emphasizing staged, evidence-based interventions [4,5,6,7], significant gaps remain [1, 8]. This is a critical issue as the world strives to drastically reduce maternal and child deaths by 2030. Achieving this ambitious goal, with targets like lowering maternal mortality from 216 to less than 70 per 100,000 live births, hinges on ensuring accessible, high-quality care throughout pregnancy, childbirth, and the postpartum period [9]. The current disparity in CoC completion highlights the need for further efforts to bridge this gap and optimize maternal and child health outcomes globally [10, 11].
While global statistics show a high proportion of women accessing antenatal care at least once (86%), only two-thirds complete the recommended minimum of four visits [12]. This disparity is particularly stark in regions with high maternal mortality rates, such as Sub-Saharan Africa and South Asia, where even fewer women receive adequate prenatal care and deliver in health facilities [12]. Despite some improvements in Ethiopia, evidenced by increased utilization of various maternal health services (32–43% for prenatal care, 28–50% for skilled delivery assistance, 17–34% for postnatal care, and 39–43% for full childhood immunization), the gap in completing the entire continuum of care remains significant, highlighting the need for further progress in low and middle-income countries [13,14,15,16].
The maternity continuum of care has a plethora of advantages; that is why different scholars tried to address the issue and factors associated with it. The overall literature review; ranges from 60% in Cambodia to 27% in Pakistan [17, 18]. In Africa, it ranges from 8% in Ghana to 31% in Nigeria [4, 19]. According to a study done in Ethiopia, the magnitude of maternal, newborn, and child health continuum of care in 2019 was 9.1% [20].
The respondent’s age, educational status, essential ANC components, occupational status, parity, women who planned for pregnancy, mothers who use contraceptives before pregnancy, and wealth status were the factors associated with the maternity continuum of care [21,22,23]. But some variables require further investigation.
There is a significant drop in maternal and child health continuum of care and still, little progress has been made in closing the gap between maternal and child health services [24]. This lack of quality of care reflects lost opportunities and a risk factor for adverse results in maternal and child health [25]. Significant gaps exist in achieving the recommended continuum of maternal healthcare services across Ethiopia, including the Gode district. This lack of research on completion rates and the factors influencing them in Gode specifically could hinder the development of effective, context-based interventions that are crucial for reducing maternal and child mortality.
Methods
Study area and period
This study was conducted in Gode district, Shebelle Zone, Ethiopia, from November 1–15, 2022. Based on 2022 population projections, Gode district has over 163,894 residents with a nearly even gender distribution (45.6% male and 54.4% female). The district encompasses an area of 7,700 square kilometers and experiences a 2.7% annual population growth.
Gode city, the main town in the district, has limited healthcare facilities. These include 2 health centers, 1 general hospital, and 4 health posts. Gode’s location is roughly 1225 km from Addis Ababa, Ethiopia’s capital city, and 600 km from Jigjiga, the capital of the Somali Regional State.
Study design
A community-based cross-sectional study design was employed.
Population
Source population
All women who had 14–24 months child preceding the data collection period in Gode district, Shebelle zone, Eastern Ethiopia.
Study population
Randomly selected women who had 14–24 months child preceding the data collection period in Gode district, Shebelle zone, Eastern Ethiopia.
Inclusion and exclusion criteria
Inclusion criteria
Women whose child is alive at the time of data collection.
Exclusion criteria
Mothers are unable to communicate due to severe illness, limiting the speaking and responding activity of the respondents at the time of data collection.
Sample size calculation
Researchers initially calculated a sample size using the single population proportion formula. This method assumed a 5% margin of error, a 95% confidence level, and a 50% completion rate for the maternal and childcare continuum. To account for potential participants who wouldn’t respond, a 20% non-response rate was added, resulting in a sample size of 461.
However, to explore factors potentially influencing MCH continuum completion, researchers employed the double population proportion formula. By applying the following assumptions: a 95% confidence level, 80% power, and a roughly equal number of participants in groups with and without the factor being investigated. The formula was applied to various factors identified from existing literatures: Exposure to media (n = 152), Place of residence (n = 189), Birth preparedness and complication readiness (n = 222), Wealth index (n = 152), Danger signs of pregnancy (sample n = 114), using Epi Info software version 7 (Table 1).
However, the sample size calculated using single population proportion formula was higher than the sample sizes obtained when using the double population proportion formula for specific factors. So, the final sample size was 461.
Sampling procedure
A stratified sampling technique was used. In the initial stage, Kebeles was discovered in the Gode district, which was divided into urban and rural areas. Then, A random sampling methodology, specifically a lottery, was employed to select six kebeles. For selected kebeles, the determined sample size is distributed proportionally. Before data collection, a list of women who gave birth in the previous year was gathered from kebeles, as well as the delivery and immunization registration book of health extension workers Finally, each study participant was chosen at random.
From a total 946 mothers who had a child 14–24 months. Within Gode city, a sample of six kebeles was drawn: Kebele Two (n = 53), Kebele Five (n = 33), Kebele Six (n = 31), Kebele Seven (n = 57), Kebele Eleven (n = 43), and Kebele Thirteen (n = 51). Four additional kebeles were selected from rural areas: Hadhawe (n = 60), Ilan (n = 55), Badila’ad (n = 40), and Barsan (n = 38).
Data collection tool and procedure
The questionnaire was prepared in English and translated into Somali language. The questioner incorporates socio-demographic, household-related, community, reproductive and obstetric, and institutional factors. The tool was first pretested in the Kebridhar district. Data collected by a semi-structured questionnaire through face-to-face interviews using a kobo collect toolbox. Ten midwives for data collection and four public health officers with a bachelor’s degree as supervisors were involved. The data collectors and supervisors got training for one day about the objective of the study, study design, and the content of the questionnaires.
Study variables
Dependent variable
Maternal and child health continuum of care (completed, not completed).
Independent variable
Socio-Demographic Characteristics. age, marital status, mother’s educational status, mother’s occupation, and husband’s occupation.
Reproductive and Obstetric factors. Parity of women, age at 1st birth, planned Pregnancy, pre-pregnancy contraceptive utilization, birth preparedness, and complication readiness, preconception contraceptives utilization, the timing of ANC, knowledge on key danger signs of pregnancy, delivery and postpartum and mode of delivery.
Households related factors. Wealth index, information on maternal and child health services, Decision-making autonomy.
Community factors. means of transportation to the health facility, distance from the district hospital, place of residence.
Institutional related factors. the behavior of health professionals, satisfaction with service delivery, and availability of drug and medical equipment.
Data quality control
The questionnaire was first prepared in English and then translated to Somali language and finally back translated to English by different individuals to check its accuracy and consistency. Before data collection, the aim of the study was told to the study participants. Intensive training has been given to data collectors and supervisors. The questionnaire was pretested outside the study area at Kebridhar district with 5% of the sample size to check the language clarity and appropriateness of the questionnaire, and corrections was taken. The data collection process was supervised daily, and each questionnaire was checked for completeness.
Operational definition and definition of terms
Maternal and Child Health Continuum of Care. A woman and her child were considered having completed the continuum of care when a woman; had four or more ANC visits by skilled health personnel (medical doctors, midwives, nurses, health officers) and childbirth by SBA at health institution and PNC at least once after discharge from the health facilities within six weeks by skilled health personnel at the health facility or with in the first week by community health extension workers during their home visit, and her child completed the immunization. Otherwise, a woman-child pair is not considered or classified as completed the continuum of care if they miss any one of the above visits or attendance at any level of care [26, 27].
Fully Vaccinated Child. A child is considered fully vaccinated when a child receives one dose of BCG, three doses of pentavalent, Pneumococcal Conjugate (PCV), Oral Polio Vaccines (OPV), two doses of Rotavirus, and one dose of measles vaccines [28].
Not Immunized. A child aged 14–24 months who did not receive any vaccine before this study is considered not immunized [27].
Data processing and analysis
Data collected by using kobo collect and exported to Stata 17 for analysis. Descriptive statistics was done to quantify the proportion of women who complete the continuum of care for maternal and child health services. Findings summarized in tables and graphs using frequencies and percentages.
Initially, Bivariable logistic regression analysis was performed between the dependent variable and each of the independent variables in sequence. Variables having a p-value of < 0.20 in Bivariable logistic regression selected as candidates for multivariable logistic regression analysis. Model fitness was checked by Hosmer and Lemeshow goodness of test and multicollinearity between the explanatory variables checked using a variance inflation factor. Association between an outcome variable and explanatory variables are reported by using adjusted odds ratio and its 95% CI, and variables having p-values ≤ 0.05 in the multivariable logistic regression model were considered as statistically significant.
Ethical clearance
Ethical clearances with this reference number (RERC/075/2022) obtained from the Ethics research review committee of Jigjiga University and further approval gained from Shebelle zone health office and the purpose or aim of the study be briefly explained for the respondents and written informed consent obtained from each respondent. We obtained parental permission for all participants under the age of 18, as is standard practice for research involving minors and assent from them.
During data collection, we assured participants that all information collected would be kept anonymous and confidential. Mothers had the right to withdraw from the study at any point or decline participation altogether. Their involvement was entirely voluntary.
Result
Sociodemographic characteristics
Out of 461 samples a total of 459 mothers were interviewed making a response rate of 99.6%. Regarding an age, 86 (17. %) of the women were under 24 years old, while 210 (45.6%) were between 25 and 34 years old. The mean age with standard deviation of the participant was 31.4(± 7.5) years. The study participants were predominantly Somali 454(98.9%) and Muslim 456 (99.4%). Most were married 433 (95.6%) and lacked formal education 236(51.5%). In most households (92.2%), the husband was the head and breadwinner 307 (66.9%). The average family size was 5.9, with 262(85.6%) having two children under five (Table 2).
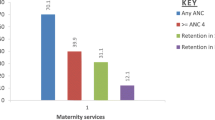
MCH continuum of care
A high proportion of women (90.9%) reported attending ANC visits during their previous pregnancy. The distribution of antenatal care (ANC) visits varied, with nearly a fifth (19.2%) of women attending four or more times. The majority of women (88.7%) delivered at a health facility. Encouragingly, a large majority (81.9%) reported attending postnatal care (PNC) services, though attendance frequency varied with one-third attending only once (34.4%). Three-quarters (74.3%) of children had complete or up-to-date immunizations (Table 3). Overall, the prevalence of the maternal and child health (MCH) continuum of care in Gode district, 2022 was 13.5% (10.7-17.0%) (Fig. 1).
Factors associated with maternal and child health continuum of care
Sociodemographic characteristics with MCHCC
Crude analysis of socio-demographic characteristics through bivariate logistic regression showed that age of women 25–34 years (COR = 2.4, 95% CI = 0.96–5.96, p-value = 0.06), (COR = 2.3, 95% CI = 0.9–5.9, p-value = 0.08), Ethnicity(Somali) (COR = 0.1,95%CI = 0.02–0.6, p value = 0.0012), Religion (Muslim) (COR = 0.3, 95% CI = 0.03–3.5, p-value = 0.340), marital status(married) (COR = 0.6, 95%CI = 0.2–1.8, p-value = 0.383), Educational status(Primary education 1–8 grade) (COR = 2.0, 95%CI = 1.1–3.5, p-value = 0.017), Maternal occupation Government employee (COR = 1.6, 95%CI = 0.9–2.9, p-value = 0.096), Husband occupation(Government employee (COR = 1.7, 95% CI = 0.99–2.96, p-value = 0.053), head of the house hold (husband) (COR = 0.96, 95% CI = 0.36–2.59, p-value = 0.944), Bread winner wife (COR = 2.0, 95% CI = 0.8–4.9, p-value = 0.128) & both (COR = 2.4, 95% CI = 1.3–4.3, p-value = 0.004), Family size(6-100) (CI = 1.5, 95% CI = 0.9–2.6, p-value = 0.154), Under five children (3) (CI = 2.7, 95% CI = 1.2-6.0, p-value = 0.154) and family income in birr (5000–10,000) (CI = 1.7, 95% CI = 0.8–3.3, p-value = 0.140) are candidate variable for multivariate analysis with P value < 0.2 (Table 4).
Pregnancy related characteristics with MCHCC
Crude analysis of socio-demographic characteristics through bivariate logistic regression showed that types of pregnancy (Planned) (COR = 1.9,95% CI = 1.0–4.0, p-value = 0.067) is a candidate variable to multivariate analysis with p value < 0.2 (Table 5).
Community related factors with MCHCC
Crude analysis of community related factors through bivariate logistic regression showed that residence (rural) (COR = 2.1,95% CI = 1.0–3.0, p-value = 0.039) and perceived time to reach health facility (< 30 min) (COR = 2.8,95% CI = 1.2–6.3, p-value = 0.014) is a candidate variable to multivariate analysis with p value < 0.2 (Table 6).
Institutional related factors with MCHCC
Crude analysis of institutional related factors through bivariate logistic regression showed that health professional behavior (good) (COR = 0.6,95% CI = 0.3-1.0, p-value = 0.06), Drug and medical equipment access(no) (COR = 2.0,95% CI = 1.2–3.5, p-value = 0.012) and Maternity waiting room in nearby health facility (COR = 1.5,95% CI = 0.9–2.7, p-value = 0.129) are a candidate variable to multivariate analysis with p value < 0.2 (Table 7).
Multivariate logistic regression
Multivariable logistic regression was performed to control the confounding effect of variables. Accordingly, Husband occupation (Government employee) [AOR = 2.3, 95%CI: (1.2–4.7)] and perceived time to reach health facility (less than 30 min) [AOR = 2.96, 95%CI: (1.2–7.5)] were factors showing significant association with maternal and child health continuum of care among mothers in Gode district, Somali regional State;2022 at P-value ≤ 0.05. The odds of maternal and child health continuum of care among mothers had husband employed in government organization 2.3 times [AOR = 2.3, 95%CI: (1.2–4.7)] higher than others. The odds of maternal and child health continuum of care among mothers perceived that distance to reach health facility less than 30 min 2.96 times [AOR = 2.96, 95%CI: (1.2–7.5)] higher than those perceived as greater than 30 min (Table 8).
Disscusion
This study conducted in Gode district, Ethiopia, yielded mixed findings regarding maternal healthcare utilization. While a high proportion of participants (90.9%) reported attending at least one antenatal care (ANC) visit during a prior pregnancy, suggesting some awareness of its significance, only 19.2% received the recommended minimum of four visits. This falls short of both the national average of 44% reported in the latest Ethiopian Demographic and Health Survey (EDHS) and the considerably higher rates observed in urban centers like Addis Ababa (84%). Notably, even within the Somali region, Gode exhibits the lowest recorded rate (19.2% compared to the regional average of 23.9%) [9]. This disparity underscores the persistent challenges in achieving equitable access to high-quality maternal healthcare services in rural Ethiopia. Geographical barriers likely play a significant role in Gode, with limited healthcare facilities and substantial travel distances for expecting mothers. These geographical constraints can be further compounded by cultural factors and economic limitations that restrict women’s ability to access adequate ANC care. Additionally, a potential knowledge gap regarding the benefits of ANC, particularly among first-time mothers, could further hinder utilization.
However, the study found positive trends in facility deliveries (86.7%) and postnatal care utilization (81.9%). This suggests a potential government effort in expanding access to delivery care and the value of institutional deliveries. Similarly, postnatal care utilization (75.4% within two days) was higher than national averages (33.8% within 48 h) [29]. This might be due to Ethiopian government initiatives promoting postnatal care services.
This study finding showed that the prevalence of MCH continuum of care was 13.5% (10.7-17.0%). This finding is lower than a study finding in different part of Ethiopia such as, Wayu district 16.1% and Debrebrhan town 37.2% North west Ethiopia 21.60% [30,31,32]. However, this finding is higher than a study finding in Ethiopia (2%) [33].It is also higher than findings of different part of the world Cambodia and Korea, which were 5.0% [34] and 6.8% [35] respectively. The probable reason for such variation could be different access to health care services, economic status, and education.
The odds of maternal and child health continuum of care among mothers had husband employed in government organization 2.3 times higher than others. Occupational status being other than a farmer, clinical/sales employed and not involved in agricultural activities are more likely to get the maternal, newborn and child health continuum of care respectively compared to their counterparts in Studies finding in Lao PDR in rural Khammouane, Nigeria, and Ethiopia [19, 36, 37]. But in Pakistan, occupational status was not a significant factor [17]. A husband’s occupation can have a significant impact on the maternal and child health continuum of care. Spousal employment in the government sector, characterized by typically stable salaries and comprehensive benefit packages, might be associated with a higher likelihood of women accessing prenatal care, delivering at healthcare facilities, and ensuring their children’s complete vaccination schedules.
The odds of maternal and child health continuum of care among mothers perceived that distance to reach health facility less than 30 min 3.0 times higher than those perceived as greater than 30 min. It is similar with study finding on Wayu district and northwest Ethiopia [32, 38]. Long distances to health facilities can translate to significant travel times, especially in rural areas with limited public transportation options. This can be a major deterrent, particularly for pregnant women or those with young children.
Strength and limitation
This investigation assesses service utilization within the maternal and child health continuum in a pastoral setting. However, the generalizability of these findings to the entire nation may be limited due to the study being confined to a single district. It is important to acknowledge that recall bias could be a potential limitation.
Conclusion
This study in Gode district, Somali Region, Ethiopia (2022) identified a relatively low prevalence of complete utilization of the maternal and child health (MCH) continuum of care. Despite a high proportion of participants having at least one antenatal care (ANC) visit during a previous pregnancy, only less than one fifth received the recommended four or more ANC visits. However, facility deliveries and postnatal care utilization were encouraging.
A study suggests that husband occupation (government employment) and perceived time to reach health facility (less than 30 min) appears to be a crucial factor influencing MCH service utilization.
Recommendation
Invest in healthcare infrastructure, especially in remote areas, to make services more accessible. Strengthen existing programs and facilities to keep delivery and postnatal care utilization rates high. Explore possibilities of integrating ANC visits with delivery and postnatal care services to create a more cohesive MCH experience.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Notes
NGO.
Amhara and Oromo
Orthodox and protestant
Widowed & divorced
Farmer, Marchant & Housewife
Abbreviations
- ANC:
-
Antenatal Care
- AOR:
-
Adjusted Odd Ratio
- BPCR:
-
Birth Preparedness and Complication Readiness
- CoC:
-
Continuum of Care
- COR:
-
Crude Odd Ratio
- CSA:
-
Central Statistics Agency
- FP:
-
Family Planning
- HIV:
-
Human Immunodeficiency Virus
- MNCH:
-
Maternal Neonatal and Child Health
- MCH:
-
Maternal and Child Health
- PNC:
-
Post Natal Care
- SBA:
-
Skilled Birth Attendance
- SPSS:
-
Statistical Package for Social Sciences
- WHO:
-
World Health Organization
References
World Health O. September. Reproductive, maternal, newborn and child health. https://www.whoint/pmnch/about/continuum_of_care/en/. 2011;1.
Organization WH, UNICEF, UNFPA, World Bank Group. Trends in maternal mortality: 1990–2015: estimates from WHO. and the United Nations Population Division: World Health Organization; 2015.
Organization WH. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA. World Bank Group and the United Nations Population Division; 2019.
Shibanuma A, Yeji F, Okawa S, Mahama E, Kikuchi K, Narh C et al. The coverage of continuum of care in maternal, newborn and child health: a cross-sectional study of woman-child pairs in Ghana. BMJ Global Health. 2018;3(4).
Ethiopia MoH. Reproductive, Maternal, Neonatal and Child Health Program Overview and Pharmaceuticals Management Training for Pharmacy Professionals,Participant Manual. 2018.
Tinker A, ten Hoope-Bender P, Azfar S, Bustreo F, Bell R. A continuum of care to save newborn lives. Lancet. 2005;365(9462):822–5.
Kerber K, De Graft–Johnson JE, Bhutta ZA, Okong P, Starrs A, Lawn JE. Continuum of care for maternal, newborn, and child health: from slogan to services delivery Lancent. 2007;370(9595):1358–69.
World Health O. World health statistics 2020: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization; 2020 2020.
Yemane GD. The factors associated with antenatal care utilization in Ethiopia. Ann Med Surg (Lond). 2022;79:104092.
World Health O. World health statistics 2017: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization; 2017 2017.
de Graft-Johnson J, Kerber K, Tinker A, Otchere S, Narayanan I, Shoo R et al. The maternal, newborn and child health continuum of care. Opportunities for Africa’s newborns. 2006:23–36.
UNICEF: UNICEF Global database. 2019, monitoring the situation of children and women [Internet]. 2019. https://data.unicef.org/topic/maternal-health/deliverycare/accessed date 1/14/2020.
Organization WH. World health statistics overview 2019: monitoring health for the SDGs, sustainable development goals. World Health Organization; 2019.
Csa I. Central statistical agency (CSA)[Ethiopia] and ICF. Ethiopia demographic and health survey, Addis Ababa, Ethiopia and Calverton, Maryland, USA. 2016.
ICF EPHiEa. ethiopian mini demogeraphic health survey 2019. 2019.
Ganchimeg T, Ota E, Morisaki N, Laopaiboon M, Lumbiganon P, Zhang J, et al. Pregnancy and childbirth outcomes among adolescent mothers: a w orld H ealth O rganization multicountry study. BJOG: Int J Obstet Gynecol. 2014;121:40–8.
Iqbal S, Maqsood S, Zakar R, Zakar MZ, Fischer F. Continuum of care in maternal, newborn and child health in Pakistan: analysis of trends and determinants from 2006 to 2012. BMC Health Serv Res. 2017;17(1):189.
Wang W, Hong R. Levels and determinants of continuum of care for maternal and newborn health in Cambodia-evidence from a population-based survey. BMC Pregnancy Childbirth. 2015;15(1):62.
Akinyemi JO, Afolabi RF, Awolude OA. Patterns and determinants of dropout from maternity care continuum in Nigeria. BMC Pregnancy Childbirth. 2016;16(1):282.
Chaka EE, Parsaeian M, Majdzadeh R. Factors associated with the completion of the continuum of care for maternal, newborn, and child health services in Ethiopia. Multilevel model analysis. Int J Prev Med. 2019;10.
Otindu B. Factors Associated with Continuum of Maternal Health Care in Kenya. University of Nairobi; 2019.
Abebe GF, Belachew DZ, Girma D, Aydiko A, Negesse Y. Multilevel analysis of the predictors of completion of the continuum of maternity care in Ethiopia; using the recent 2019 Ethiopia mini demographic and health survey. BMC Pregnancy Childbirth. 2022;22(1):691.
Emiru AA, Alene GD, Debelew GT. Women’s retention on the continuum of maternal care pathway in west Gojjam Zone, Ethiopia: multilevel analysis. BMC Pregnancy Childbirth. 2020;20:1–14.
Amare NS, Araya BM, Asaye MM. The proportion of dropouts from the maternity continuum of care and its predictors among antenatal booked women who gave birth in the last 12 months in Northwest Ethiopian women: a community-based cross-sectional study. Pan Afr Med J. 2022;41:312.
Khorshed MS, Lindsay D, McAuliffe M, West C, Wild K. Factors affecting quality of Care in Maternal and Child Health in Timor-Leste: a scoping review. Health Serv Insights. 2022;15:11786329221110052.
Atnafu A, Kebede A, Misganaw B, Teshome DF, Biks GA, Demissie GD et al. Determinants of the Continuum of Maternal Healthcare Services in Northwest Ethiopia: Findings from the Primary Health Care Project. Journal of Pregnancy. 2020;2020.
Bahl R, Qazi S, Darmstadt GL, Martines J. Why is continuum of Care from Home to Health facilities essential to improve Perinatal Survival? Seminars in Perinatology. 2010;34(6):477–85.
World Health Organization. Immunization, vaccines, and biological: implementation research in immunization. 2017.
Indicators K. Mini demographic and health survey. EPHI and ICF. 2019.
Atnafu A, Kebede A, Misganaw B, Teshome DF, Biks GA, Demissie GD, et al. Determinants of the Continuum of Maternal Healthcare Services in Northwest Ethiopia: findings from the Primary Health Care Project. J Pregnancy. 2020;2020:4318197.
Tizazu MA, Sharew NT, Mamo T, Zeru AB, Asefa EY, Amare NS. Completing the continuum of maternity care and associated factors in Debre Berhan town, Amhara, Ethiopia, 2020. J Multidisciplinary Healthc. 2021:21–32.
Sertsewold SG, Debie A, Geberu DM. Continuum of maternal healthcare services utilisation and associated factors among women who gave birth in Siyadebirena Wayu district, Ethiopia: community-based cross-sectional study. BMJ open. 2021;11(11):e051148.
Gebremedhin AF, Dawson A, Hayen A. Determinants of continuum of care for maternal, newborn, and child health services in Ethiopia: analysis of the modified composite coverage index using a quantile regression approach. PLoS ONE. 2023;18(1):e0280629.
Kikuchi K, Yasuoka J, Nanishi K, Ahmed A, Nohara Y, Nishikitani M, et al. Postnatal care could be the key to improving the continuum of care in maternal and child health in Ratanakiri, Cambodia. PLoS ONE. 2018;13(6):e0198829.
Sakuma S, Yasuoka J, Phongluxa K, Jimba M. Determinants of continuum of care for maternal, newborn, and child health services in rural Khammouane, Lao PDR. PLoS ONE. 2019;14(4):e0215635.
Amare NS, Araya BM, Asaye MM. Dropout from maternity continuum of care and associated factors among women in Debre Markos town, Northwest Ethiopia. bioRxiv. 2019:620120.
Haile D, Kondale M, Andarge E, Tunje A, Fikadu T, Boti N. Level of completion along continuum of care for maternal and newborn health services and factors associated with it among women in Arba Minch Zuria Woreda, Gamo Zone, Southern Ethiopia: a community based cross-sectional study. PLoS ONE. 2020;15(6):e0221670.
Asratie MH, Muche AA, Geremew AB. Completion of maternity continuum of care among women in the post-partum period: magnitude and associated factors in the northwest, Ethiopia. PLoS ONE. 2020;15(8):e0237980.
Acknowledgements
Authors would like to thank Jigjiga University for supporting this research. We forward appreciation to Somali regional health office for their provision of information related to our research topic. Our gratitude also goes to our colleagues for their encouragement and meticulous support while conducting this research. Finally, we would like to thank the data collectors, supervisors and all research participants who took part in the study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
LM designed the research, analyzed the data, interpreted the findings, and drafted the manuscript. SH, ZS & MT are also involved in all the processes of this research. All authors read and approved the final manuscript for publication.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ayehubizu, L.M., Yohannes, S.H., Yadeta, Z.S. et al. Completion of maternal and child health continuum of care and associated factors among women in Gode district, Shebele Zone, Eastern Ethiopia, 2022. BMC Pregnancy Childbirth 24, 441 (2024). https://doi.org/10.1186/s12884-024-06639-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06639-0