Abstract
Aim
To evaluate placental pathology in term and post-term births, investigate differences in clinical characteristics, and assess the risk of adverse neonatal outcome.
Methods
This prospective observational study included 315 singleton births with gestational age (GA) > 36 weeks + 6 days meeting the local criteria for referral to placental histopathologic examination. We applied the Amsterdam criteria to classify the placentas. Births were categorized according to GA; early-term (37 weeks + 0 days to 38 weeks + 6 days), term (39 weeks + 0 days to 40 weeks + 6 days), late-term (41 weeks + 0 days to 41 weeks + 6 days), and post-term births (≥ 42 weeks + 0 days). The groups were compared regarding placental pathology findings and clinical characteristics. Adverse neonatal outcomes were defined as 5-minute Apgar score < 7, umbilical cord artery pH < 7.0, admission to the neonatal intensive care unit or intrauterine death. A composite adverse outcome included one or more adverse outcomes. The associations between placental pathology, adverse neonatal outcomes, maternal and pregnancy characteristics were evaluated by logistic regression analysis.
Results
Late-term and post-term births exhibited significantly higher rates of histologic chorioamnionitis (HCA), fetal inflammatory response, clinical chorioamnionitis (CCA) and transfer to neonatal intensive care unit (NICU) compared to early-term and term births. HCA and maternal smoking in pregnancy were associated with adverse outcomes in an adjusted analysis. Nulliparity, CCA, emergency section and increasing GA were all significantly associated with HCA.
Conclusions
HCA was more prevalent in late and post-term births and was the only factor, along with maternal smoking, that was associated with adverse neonatal outcomes. Since nulliparity, CCA and GA beyond term are associated with HCA, this should alert the clinician and elicit continuous intrapartum monitoring for timely intervention.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Pregnancy complications and adverse neonatal outcomes, such as stillbirth and neonatal death, become increasingly prevalent after 40 weeks’ gestation [1, 2]. To address the increased risk, a Swedish multicentre randomised trial concluded that induction of labour instead of expectant management should be recommended at 41 weeks, [3] and this was supported by another study in the Netherlands [4]. However, this study also demonstrated that induction of labour after 41 weeks increased the rates of adverse neonatal outcomes such as 5-minute Apgar score < 7, admission to the neonatal intensive care unit (NICU), and emergency caesarean section. With up to one in four pregnant women in the developed world having their labour induced [5], the high cost to health services and the impact on women and their families, there is an imperative need to better understand the factors that can identify high-risk pregnancies or women who would benefit from labour induction. Despite the acknowledged link between placental dysfunction and increased risk of chronic diseases later in life, [6] few studies have explored the connection between neonatal morbidity and underlying placental pathology. A recent paper by Nikkels et al. [7] compared placental findings in uneventful term deliveries with cases of NICU admission or perinatal death. They found more placental pathology in neonates with severe perinatal morbidity and mortality, which is in accordance with studies including placentas from births with adverse outcome only [8,9,10]. Throughout pregnancy, the placenta matures to meet the increased needs of the fetus for oxygen and nutrients, but the process of placental ageing and decreasing functional capacity beyond term is not well understood. Research has focused on biological markers, gene expression and ancillary techniques that can assess or measure placental function. Nonetheless, with the exception of markers for preeclampsia, no marker has been found useful in a clinical setting [11, 12]. Consequently, the primary aim of this study was to assess placental pathology according to gestational age (GA) at birth; early-term/term and late-term/post-term births that align with the local criteria for placental examination. A secondary aim was to explore potential differences between these groups in terms of clinical characteristics and the risk of adverse neonatal outcomes. We hypothesised that placental pathology and related neonatal morbidity would differ according to GA at birth.
Materials and methods
Participants and study design
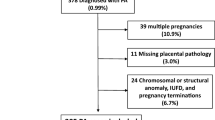
Women who delivered at Haukeland University Hospital and had a histological placental examination carried out according to local clinical routines (Supplementary S1) between January 2013 and May 2015 (n = 1143) were asked to enrol in our placental pathology database. The study required written informed consent, and eligible women were invited to participate. Of these, 492 (43.0%) did not complete the consent form, nine (0.8%) declined to participate, and 30 (2.6%) had emigrated from Norway (n = 29) or died (n = 1). Thus, a total of 612 (53.5%) placentas were included in the database. The present study includes births with GA > 36 week + 6 days without congenital malformations or syndromes, a total of 315 (Fig. 1).
The Regional Committees for Medical and Health Research Ethics approved the study (REK ID 2014/1926).
Classification of placental histological findings
The placentas with the cord and membranes attached were grossly examined by the midwife attending the birth, rinsed in water, and fixated in a bucket with formalin. In the Pathology Department the placentas were measured in three dimensions and weighed without cord and membranes. Our department followed a standardised protocol, which included sampling of full-thickness sections from visually normal parenchyma at the inner two-thirds, sections from the cord insertion site, as well as two sections from the umbilical cord and membrane rolls, in agreement with the recommended guidelines [13]. Additionally, samples from macroscopically abnormal parenchyma were submitted. The histological evaluation was performed by a team (N = 5) of pathologists trained in perinatal pathology. Subsequently, two of those (EBB and KC) independently re-examined the slides to ensure consistency and accuracy of the findings.
Histologic chorioamnionitis (HCA) was defined as the presence of neutrophils in the chorionic plate or extraplacental membranes. Notably, a mild acute placental inflammation at term is considered to be part of the physiological process leading to parturition rather than an acute infection [10, 14,15,16]. Therefore, we dichotomised the maternal inflammatory response into two categories: No inflammation/neutrophils in the subchorionic fibrin (stage 0 or 1) versus Neutrophils in the chorioamnion (stage 2 or 3). Thus, only stage 2 or 3 were defined as presence of maternal inflammatory response.
A fetal inflammatory response (FIR) was defined as the presence of neutrophils in the wall of the chorionic vessels, the umbilical vein or arteries. This response was also divided into two groups of FIR: No and Yes.
Maternal vascular malperfusion (MVM) included a constellation of findings based on placental weight (weight < 10th centile), presence of villous infarctions or intervillous thrombi, and histological findings such as distal villous hypoplasia, accelerated villous maturation or decidual arteriopathy.
Fetal vascular malperfusion (FVM) was defined as thrombi (occlusive or non-occlusive) in large fetal vessels of the placenta, including umbilical, chorionic plate, and stem villous vessels or foci of avascular villi.
Delayed villous maturation (DVM) was defined as the presence of immature-appearing villi with poor vasculosyncytial membrane formation and centrally placed capillaries. To be classified as DVM, this abnormality had to be observed in at least 30% of a full thickness section.
Villitis was defined as a lymphohistiocytic infiltrate involving the chorionic villi and intervillositis as a diffuse infiltration of the intervillous space by monocyte-macrophages. These findings were not graded and were combined in the analyses due to the small number of cases.
The variables MVM, FVM, DVM and villitis/intervillositis were dichotomised into two groups: No (absence of the finding) or Yes (presence of the specific finding).
Clinical variables
According to guidelines, [17] preeclampsia was defined as newly onset hypertension after gestation week 20 (blood pressure ≥ 140 mmHg systolic and/or ≥ 90 mmHg diastolic) combined with proteinuria or other signs of organ dysfunction.
Clinical chorioamnionitis (CCA) was diagnosed in the presence of maternal fever (rectal temperature ≥ 38 °C) accompanied by at least two of the following: maternal tachycardia (> 100 beats/minute), fetal tachycardia (> 160 beats/minute in at least 10 min), maternal leukocytosis (> 15 × 109/L), uterine tenderness, or malodourous amniotic fluid.
GA was estimated based on ultrasound biometry in 1st trimester or at 17–19 weeks of gestation (92.8%) or according to in vitro fertilization data (7.0%). We divided the participants into four groups according to GA at delivery: early-term (37 weeks + 0 days to 38 weeks + 6 days), term (39 weeks + 0 days to 40 weeks + 6 days), late-term (41 weeks + 0 days to 41 weeks + 6 days) and post-term birth (42 weeks + 0 days to 42 weeks + 2 days).
Delivery outcomes as GA at birth, birthweight, information about the delivery, Apgar score, pH in umbilical cord artery, and admission to NICU were collected from the clinical files. A 5-min Apgar score < 7, umbilical cord artery pH < 7.0, NICU admission, or perinatal death were considered as adverse neonatal outcomes. The composite adverse neonatal outcome variable was none vs. at least one adverse outcome.
Statistics
The chi-square or Fisher’s exact test was used for comparison of categorical variables, presented as proportions. For continuous variables, Student’s T-test or Mann-Whitney’s.
U-test was used, as appropriate, and presented as means with standard deviations. The adverse outcome measures were binary; therefore, a logistic regression model was used to estimate the odds ratio (OR) and 95% confidence intervals (CIs). Independent variables were included in the multivariate analysis if p < 0.2 in the unadjusted analysis, and only significant variables were included in the final model. P-values ≤ 0.05 were considered significant. The same procedure was used to explore associations between HCA and maternal and pregnancy characteristics. All analyses were performed using SPSS Statistics for Windows, version 26.0 (IBM Corp, New York, USA).
Results
A total of 315 individual cases were included in the study (Fig. 1), among these 13 (4.1%) stillbirths. Table 1 presents the characteristics of the mothers, newborns, and placentas according to GA at birth. Delivery by emergency caesarean occurred more often in the late-term and post-term group compared to the early-term and term group (p = 0.0047). In addition, in late-term/post-term births, HCA and FIR were more common compared to early-term/term births (p = 0.004 and p = 0.001, respectively). This was accompanied by a higher rate of CCA (p = 0.023) and NICU transfer (p = 0.037). In contrast, MVM and preeclampsia were more common in early-term/term births, but the difference was not significant. A higher rate of small for gestational age neonates was also seen in the early-term/term group.
When the cases were stratified based on the presence of adverse neonatal outcome, HCA (including both the maternal and fetal inflammatory response) was more common in the adverse outcome group (22.2% vs. 11.6%, and 24.4% vs. 15.1%, respectively, Table 2). Additionally, the rate of smoking was higher in the adverse outcome group (8.9% versus 1.8%).
When exploring the association between adverse neonatal outcome and selected clinical and histological characteristics, we found that maternal smoking and HCA were associated with adverse neonatal outcome in the unadjusted logistic regression analyses (Table 3). This association persisted in the adjusted analysis (Table 3). We then explored the relationship between maternal and pregnancy characteristics and HCA. In the adjusted regression analysis, four factors were identified to influence the risk of HCA (Table 4). Nulliparous women had twice the risk of developing HCA (OR: 2.22, 95% CI: 1.01 to 4.86). The presence of CCA was associated with an almost sixfold increased risk of HCA (OR: 5.97, 95% CI: 1.99 to 17.91). There was also an association between HCA and emergency caesarean section and advanced gestational age (OR: 2.05, 95% CI: 1.01 to 4.15 and OR: 1.45, 95% CI: 1.13 to 1.87, respectively).
Discussion
In this study of births from the early-term to the post-term period, we found that HCA was the most important factor associated with adverse neonatal outcome. Nulliparity, CCA and increasing GA all carried an increased risk of HCA.
Although there is agreement in guidelines to recommend induction of labour in post-term pregnancies, some argue for routine induction during the late-term or term period [18]. However, a large, randomised, multicentre trial (ARRIVE) on low-risk nulliparous women found that induction of labour at 39 weeks reduced the incidence of caesarean section but did not significantly lower the frequency of a composite adverse perinatal outcome [19]. A systematic review found that inducing labour at 39 weeks was associated with improved neonatal outcomes in both in nulliparous and primiparous women. However, in nulliparous women, induction of labour was associated with shoulder dystocia [20]. The external validity of these studies [19, 20] for the Norwegian practice is questionable since intervention rates during spontaneous and induced labour are substantially lower [21, 22]. There is some evidence that induction of labour may reduce perinatal death and morbidity [23]. This could explain the change in clinical practice with increased rates of inductions, but there is a trade-off against adverse outcomes due to interventions [24]. Therefore, it is important to identify risk factors of adverse outcome in order to differentiate care. Likewise, identifying predictors of induction success is important, and obstetric background factors such as maternal age and weight, insulin-dependent diabetes and obstetric history are considered. In a nationwide study from Denmark, maternal fever was significantly more common in the late-term group (GA 41 weeks + 4 days to 42 weeks + 0 days) than in the term group (GA 41 weeks + 0 days to 41 weeks + 3 days), which was also associated with an increased risk of neonatal morbidity [25]. Less attention has been paid to the placenta, although placental function is a major determinant for acute and unexpected adverse outcomes [26]. Placental function changes during pregnancy and may adapt according to fetal and maternal factors such as obesity, [27] maternal glucose metabolism and cardiovascular function [28]. It has taken a long time to reach consensus on the nomenclature of placental findings due to a shortage of pathologists with the necessary training and a lack of understanding of placental pathophysiology among clinicians [26]. As a result, placental reports are often delayed, which may have contributed to a lack of interest in placentas role in determining the optimal timing of induction in the next pregnancy [29]. Rather than finding associations between placental pathology and maternal and fetal factors, the focus has been on biological markers and ancillary techniques that can assess or measure placental function before labour. Although term HCA is considered a heterogeneous condition and often does not correspond to a clinical presentation, it is associated with adverse neonatal outcomes [30]. HCA has been found common in perinatal stroke [31] and associated with early onset sepsis in term births [32]. Interestingly, in a study by Roberts et al. that included only low-risk pregnancies, almost all HCA at term were non-infectious [33]. Milder inflammatory lesions are often seen in placentas with normal outcomes at term, and awareness should be raised when comparing low- and high-risk pregnancies if grading has not been taken into account [10].
In a study by Stormdal Bring et al. [34] umbilical cord complications and infections (defined as HCA) were more frequent in term (GA 37 weeks + 0 days to 40 weeks + 6 days) and post-term (GA ≥ 41 weeks + 0 days) stillbirths than in preterm stillbirths (GA ≤ 37 weeks + 0 days), corroborating our findings. The study by Nikkels et al. [7] confirmed that HCA was more frequent in stillbirths (antepartum and intrapartum) and neonatal deaths and in those admitted to NICU. In line with their findings, we also found that less frequent placental abnormalities such as fetal vascular malperfusion, delayed villous maturation and villitis of unknown etiology were more common in the adverse neonatal outcome group, but the number of events in our study was too small to examine this. Unlike their study, [7] which compared the outcome of uncomplicated pregnancies and births with groups of stillbirths, neonatal deaths and NICU survivors, we only included cases that met local clinical guidelines for histologic examination of the placenta. Therefore, we do not know the incidence of HCA in uncomplicated pregnancies and births in our region. On the other hand, in clinical practice it is not appropriate to send all placentas for histopathological examination, as most placentas from low-risk births have mild inflammatory or vascular lesions only and rarely provide additional significant information [10, 35].
Our study showed that HCA was inversely related to parity. This is in agreement with other reports [36]. Early HCA may represent the inflammatory process of labour itself and does not necessarily have an infectious etiology [15, 37]. As nulliparity is associated with longer duration of labour, the finding of early HCA in this group has been suggested to be a subclinical process [10]. We found that the subgroup with FIR, which is considered a higher burden lesion, was also more common in nulliparas (data not shown). Regardless of the cause of HCA, our results indicate that nulliparity should be considered as a risk factor for both HCA and FIR in term births.
Our results are further in line with previous studies that have found smoking to be a significant maternal factor associated with adverse neonatal outcomes [38, 39]. However, this association may be due to the confounding effect of smoking with other known causes of adverse outcomes, such as socioeconomic status and psychosocial stress [40]. On the other hand, the adverse effects of nicotine exposure on placental development are well known [41,42,43]. A recent study suggests that placental injury may induce a sterile inflammation through a shift in the pro- versus anti-inflammatory balance mediated by damage associated molecular patterns (DAMP) [44]. This is consistent with several other reports concluding that intrauterine inflammation can be triggered by many factors and supports theories about the complex relationship between intrauterine inflammation and infection [45].
One of the major challenges for obstetricians is to identify the group of term pregnancies that would benefit from induction of labour rather than expectant management at around 41 weeks. We found that neither preeclampsia nor MVM had an effect on neonatal outcome compared to other high-risk conditions. This may be explained by the fact that preeclamptic mothers are often induced earlier (37- and 38-weeks’ gestation). In a report by Lisonkova et al. [46] early-onset preeclampsia, but not late-onset preeclampsia, was associated with a high risk of fetal death. However, they also found that the rate of severe neonatal morbidity and death was higher in the group with late-onset preeclampsia compared with those without preeclampsia. Our findings are consistent with a report that concluded that late-onset preeclampsia (after 34 weeks’ GA) does not have a serious impact on neonatal complications, [47] although this was a small study involving only 77 newborns. Our results are further in line with a report by Levy et al., including placentas from preeclampsia cases routinely sent for assessment, that advanced GA and HCA were independently associated with adverse outcomes [48].
A strength of this study is that it is population-based and includes detailed maternal and neonatal characteristics. The placentas were investigated by perinatal pathologists according to international consensus criteria, and the diagnosis further strengthened by a second look. Similar to other perinatal studies, a composite variable was used to predict adverse outcomes. However, the use of a composite variable has its limitations as it often combines neonatal transition problems related to both the condition (such as placental insufficiency) and its treatment (such as relatively premature delivery) [49]. Additionally, there is a lack of information regarding the time needed to induce labour and the methods used. The pre-requisite of a clinical indication for placental investigation, and thus recruitment to the study, introduces a selection bias towards a high-risk cohort, which limits comparison and prediction statistics to be performed within this cohort of different maternal and fetal high-risk conditions. Comparison with a control group of uncomplicated pregnancies and births may have identified additional placental pathology associated with adverse outcomes.
Conclusion
We found that in a cohort of term and late-term neonates, HCA and smoking during pregnancy were risk factors associated with adverse neonatal outcome. HCA was more common in the late-term group and was associated with nulliparity, CCA and advanced GA, which should increase awareness and surveillance during labour and delivery.
Data availability
The data that support the findings of this study are not available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are in controlled access data storage at Haukeland University Hospital.
Abbreviations
- GA:
-
gestational age
- HCA:
-
histologic chorioamnionitis
- CCA:
-
clinical chorioamnionitis
- NICU:
-
neonatal intensive care unit
- FIR:
-
fetal inflammatory response
- MVM:
-
maternal vascular malperfusion
- FVM:
-
fetal vascular malperfusion
- DVM:
-
delayed villous maturation
References
Heimstad R, Romundstad PR, Eik-Nes SH, Salvesen KA. Outcomes of pregnancy beyond 37 weeks of gestation. Obstet Gynecol. 2006;108(3 Pt 1):500–8.
Linder N, Hiersch L, Fridman E, et al. Post-term pregnancy is an independent risk factor for neonatal morbidity even in low-risk singleton pregnancies. Archives Disease Child Fetal Neonatal Ed. 2017;102(4):F286–90.
Wennerholm UB, Saltvedt S, Wessberg A, et al. Induction of labour at 41 weeks versus expectant management and induction of labour at 42 weeks (SWEdish post-term induction study, SWEPIS): multicentre, open label, randomised, superiority trial. BMJ. 2019;367:l6131.
Ravelli ACJ, van der Post JAM, de Groot CJM, et al. Does induction of labor at 41 weeks (early, mid or late) improve birth outcomes in low-risk pregnancy? A nationwide propensity score-matched study. Acta Obstet Gynecol Scand. 2023;102(5):612–25.
Marconi AM. Recent advances in the induction of labor. F1000Res 2019;8.
Thornburg KL, Kolahi K, Pierce M, et al. Biological features of placental programming. Placenta. 2016;48(Suppl 1):S47–53.
Nikkels PG, Evers AC, Schuit E, et al. Placenta Pathology from term born neonates with normal or adverse outcome. Pediatric and developmental pathology: the official journal of the Society for Pediatric Pathology and the Paediatric. Pathol Soc. 2021;24(2):121–30.
Korteweg FJ, Erwich J, Holm JP, et al. Diverse placental pathologies as the main causes of fetal death. Obstet Gynecol. 2009;114(4):809–17.
Man J, Hutchinson JC, Heazell AE, et al. Stillbirth and intrauterine fetal death: role of routine histopathological placental findings to determine cause of death. Ultrasound Obstet Gynecol. 2016;48(5):579–84.
Romero R, Kim YM, Pacora P, et al. The frequency and type of placental histologic lesions in term pregnancies with normal outcome. J Perinat Med. 2018;46(6):613–30.
Tossetta G. Physiology and pathophysiology of the Placenta. Int J Mol Sci 2023;24(10).
Manokhina I, Del Gobbo GF, Konwar C, et al. Review: placental biomarkers for assessing fetal health. Hum Mol Genet. 2017;26(R2):R237–45.
Khong TY, Mooney EE, Ariel I, et al. Sampling and definitions of placental lesions: Amsterdam Placental Workshop Group Consensus Statement. Arch Pathol Lab Med. 2016;140(7):698–713.
Lee SM, Lee KA, Kim SM, et al. The risk of intra-amniotic infection, inflammation and histologic chorioamnionitis in term pregnant women with intact membranes and labor. Placenta. 2011;32(7):516–21.
Park HS, Romero R, Lee SM, et al. Histologic chorioamnionitis is more common after spontaneous labor than after induced labor at term. Placenta. 2010;31(9):792–5.
Ganer Herman H, Schreiber L, Miremberg H, et al. Histological chorioamnionitis at term according to labor onset: a prospective controlled study. J Perinatology: Official J Calif Perinat Association. 2019;39(4):581–7.
Staff A, Kvie A, Langesæter E et al. Hypertensive svangerskapskomplikasjoner og eklampsi.; https://www.legeforeningen.no/foreningsledd/fagmed/norsk-gynekologisk-forening/veiledere/veileder-i-fodselshjelp/hypertensive-svangerskapskomplikasjoner-og-eklampsi/. Accessed 10/10/23.
Jeer B, Haberfeld E, Khalil A, et al. Perinatal and maternal outcomes according to timing of induction of labour: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2023;288:175–82.
Grobman WA, Rice MM, Reddy UM, et al. Labor Induction versus Expectant Management in Low-Risk Nulliparous women. N Engl J Med. 2018;379(6):513–23.
Hong J, Atkinson J, Roddy Mitchell A, et al. Comparison of Maternal Labor-Related Complications and Neonatal Outcomes Following Elective Induction of Labor at 39 weeks of Gestation vs Expectant Management: a systematic review and Meta-analysis. JAMA Netw Open. 2023;6(5):e2313162.
Sørbye IK, Oppegaard KS, Weeks A, et al. Induction of labor and nulliparity: a nationwide clinical practice pilot evaluation. Acta Obstet Gynecol Scand. 2020;99(12):1700–9.
Haavaldsen C, Morken NH, Saugstad OD, Eskild A. Is the increasing prevalence of labor induction accompanied by changes in pregnancy outcomes? An observational study of all singleton births at gestational weeks 37–42 in Norway during 1999–2019. Acta Obstet Gynecol Scand. 2023;102(2):158–73.
Gibson KS, Waters TP, Bailit JL. Maternal and neonatal outcomes in electively induced low-risk term pregnancies. American journal of obstetrics and gynecology. 2014;211(3):249.e241-249.e216.
Souter V, Painter I, Sitcov K, Caughey AB. Maternal and newborn outcomes with elective induction of labor at term. Am J Obstet Gynecol. 2019;220(3):e273271–273211.
Andersson CB, Petersen JP, Johnsen SP, et al. Risk of complications in the late vs early days of the 42nd week of pregnancy: a nationwide cohort study. Acta Obstet Gynecol Scand. 2022;101(2):200–11.
Redline RW, Roberts DJ, Parast MM, et al. Placental pathology is necessary to understand common pregnancy complications and achieve an improved taxonomy of obstetrical disease. Am J Obstet Gynecol. 2023;228(2):187–202.
Santos ED, Hernández MH, Sérazin V et al. Human placental adaptive changes in response to maternal obesity: sex specificities. Int J Mol Sci 2023;24(11).
Gyselaers W, Thilaganathan B. Preeclampsia: a gestational cardiorenal syndrome. J Physiol. 2019;597(18):4695–714.
Khong TY, Ting M, Gordijn SJ. Placental pathology and clinical trials: histopathology data from prior and study pregnancies may improve analysis. Placenta. 2017;52:58–61.
Conti N, Torricelli M, Voltolini C, et al. Term histologic chorioamnionitis: a heterogeneous condition. Eur J Obstet Gynecol Reprod Biol. 2015;188:34–8.
Leon RL, Kalvacherla V, Andrews MM, et al. Placental pathologic lesions associated with stroke in term neonates. Front Endocrinol (Lausanne). 2022;13:920680.
Cuna A, Hakima L, Tseng YA, et al. Clinical dilemma of positive histologic chorioamnionitis in term newborn. Front Pediatr. 2014;2:27.
Roberts DJ, Celi AC, Riley LE, et al. Acute histologic chorioamnionitis at term: nearly always noninfectious. PLoS ONE. 2012;7(3):e31819.
Stormdal Bring H, Hulthén Varli IA, Kublickas M, et al. Causes of stillbirth at different gestational ages in singleton pregnancies. Acta Obstet Gynecol Scand. 2014;93(1):86–92.
Zhou YY, Ravishankar S, Luo G, Redline RW. Predictors of high Grade and other clinically significant placental findings by indication for submission in Singleton Placentas from term births. Pediatric and developmental pathology: the official journal of the Society for Pediatric Pathology and the Paediatric. Pathol Soc. 2020;23(4):274–84.
Mi Lee S, Romero R, Lee KA, et al. The frequency and risk factors of funisitis and histologic chorioamnionitis in pregnant women at term who delivered after the spontaneous onset of labor. The journal of maternal-fetal & neonatal medicine: the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies. Int Soc Perinat Obstet. 2011;24(1):37–42.
Kim CJ, Romero R, Chaemsaithong P, et al. Acute chorioamnionitis and funisitis: definition, pathologic features, and clinical significance. Am J Obstet Gynecol. 2015;213(4 Suppl):S29–52.
Castles A, Adams EK, Melvin CL, et al. Effects of smoking during pregnancy. Five meta-analyses. Am J Prev Med. 1999;16(3):208–15.
Dietz PM, England LJ, Shapiro-Mendoza CK, et al. Infant morbidity and mortality attributable to prenatal smoking in the U.S. Am J Prev Med. 2010;39(1):45–52.
Blumenshine P, Egerter S, Barclay CJ, et al. Socioeconomic disparities in adverse birth outcomes: a systematic review. Am J Prev Med. 2010;39(3):263–72.
Bjørnholt SM, Leite M, Albieri V, et al. Maternal smoking during pregnancy and risk of stillbirth: results from a nationwide Danish register-based cohort study. Acta Obstet Gynecol Scand. 2016;95(11):1305–12.
Suter MA, Aagaard KM. The impact of tobacco chemicals and nicotine on placental development. Prenat Diagn. 2020;40(9):1193–200.
Ernst LM. Maternal vascular malperfusion of the placental bed. APMIS: Acta Pathologica Microbiol et Immunol Scand. 2018;126(7):551–60.
Baker BC, Heazell AEP, Sibley C, et al. Hypoxia and oxidative stress induce sterile placental inflammation in vitro. Sci Rep. 2021;11(1):7281.
Peng CC, Chang JH, Lin HY, et al. Intrauterine inflammation, infection, or both (Triple I): a new concept for chorioamnionitis. Pediatr Neonatol. 2018;59(3):231–7.
Lisonkova S, Joseph KS. Incidence of preeclampsia: risk factors and outcomes associated with early- versus late-onset disease. American journal of obstetrics and gynecology. 2013;209(6):544.e541-544.e512.
Tousty P, Fraszczyk-Tousty M, Ksel-Hryciów J et al. Adverse Neonatal Outcome Pregnancies Complicated Preeclampsia Biomedicines 2022;10(8).
Levy M, Mor L, Kovo M, et al. Histologic Chorioamnionitis in pregnancies complicated by Preeclampsia and the Effect on neonatal outcomes. Reproductive sciences (Thousand Oaks. Calif). 2021;28(7):2029–35.
Gordijn SJ, Ganzevoort W. Search for the best prediction model, definition and growth charts for fetal growth restriction using a composite of adverse perinatal outcomes: a catch-22? Ultrasound Obstet Gynecol. 2022;60(3):305–6.
Acknowledgements
We are grateful to the Norwegian SIDS and Stillbirth Society (Landsforeningen uventet barnedød - LUB) for financial support for technical assistance and distribution of the consent forms, which were sent by post. We are also grateful to Bjørg Sandvik for excellent technical support.
Funding
Grant no. 912123 Helse Vest.
Open access funding provided by University of Bergen.
Author information
Authors and Affiliations
Contributions
EBB and KC wrote the initial main manuscript. CE and JK contributed with important clinical information, ideas, views and perspective to the article. JK also contributes with clinical data. GEE quality assured the statistical analyses and tables. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki.
It was approved by the regional committee for Medical Research Ethics Western Norway, Bergen University Hospital (REK ID 2014/1926).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Budal, E.B., Kessler, J., Eide, G.E. et al. Placental pathology and neonatal morbidity: exploring the impact of gestational age at birth. BMC Pregnancy Childbirth 24, 201 (2024). https://doi.org/10.1186/s12884-024-06392-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06392-4