Abstract
Background
Pregnancy registration is one of the most critical components of women’s reproductive health because it is the gateway to entering the continuum of care services such as antenatal care, institutional delivery, and postnatal care. There is a lack of studies exploring the relationship between pregnancy intention and pregnancy registration, especially in the Indian context.
Method
This study used the National Family Health Survey-5 (2019-21) data to explore the relationship between birth intention and failure of pregnancy registration. The bivariate and multivariate (binary logistic regression) analysis was carried out.
Results
Adjusting the effects of socio-demographic and economic characteristics, compared with women with an intended pregnancy, the odds of failure of pregnancy registration were significantly high among women with a mistimed pregnancy (OR = 1.60, 95% CI = 1.47–1.73) and unwanted pregnancy (OR = 1.38, 95% CI = 1.26–1.52). The study found pregnancy intention as a significant predictor of pregnancy registration.
Conclusions
Results suggest strengthening the interaction of grassroots-level health workers with women, especially those with possibly lower healthcare autonomy and unintended pregnancy. Higher and earlier pregnancy registration will enhance maternal healthcare utilization and reduce adverse health consequences to mothers and children, thus ensuring better maternal and child health.
Similar content being viewed by others
Introduction
Maternal mortality continues to be high in India, although remarkable improvements have recently been noticed [1]. With a prevalence of 120 per 1000 live births, severe maternal morbidities indicate the equally bad maternal health status of Indian women [2]. Antenatal care (ANC), institutional delivery, and appropriate postnatal care (PNC) are the deterrent factors of maternal morbidity and mortality [3, 4]. An early ANC visit allows for the most effective screening and tests, including correct gestational age determination for proper preterm labor treatment, genetic and congenital diseases screening, folic acid supplementation to lower iron deficiency anemia, and sexually transmitted infections screening and treatment [5]. It is thus critical to identify and register women early in their pregnancies to ensure the utilization of suggested ANC services [6]. Early pregnancy registration is the starting point of Indian government’s maternal healthcare delivery system [7]. Delays in pregnancy registration influence obtaining appropriate treatment, immunization, and vitamin supplementation, all critical in reducing pregnancy-related problems. Policy initiatives to increase pregnancy registration are well in place universally in India. Pregnant women are given Mother and Child Protection (MCP) Cards and safe motherhood booklets [7], and some states have added initiatives along with this MCP card to increase pregnancy registration. For example, Karnataka has introduced the Thayi card and the mother and child tracking systems (MCTS). Pregnant women get the Thayi card with a unique identification number when registered with a female health assistant in their area, enabling socioeconomically disadvantaged women to avail of ANC and delivery services from registered private hospitals free of cost [8]. Similarly, Tamil Nadu has a Pregnancy and Infant Cohort Monitoring and Evaluation System (PICME) both in urban and rural areas [9].
Women in low-and-middle-income countries disguise their pregnancy during the first few months due to various socio-cultural behaviors and attitudes that make early pregnancy registration difficult [10, 11]. According to a study in Maharashtra, fear of losing the baby owing to black magic and the casting of evil eyes by jealous neighbors and those with malicious intentions are the causes of delayed disclosure and registration of pregnancy [12]. Women are again reluctant to inform the grassroot level health workers i.e., Accredited Social Health Activist (ASHA) and Anganwadi Worker (AWW) about their pregnancy at an early stage, as it would require them to attend the village health facility and thus, make their pregnancy evident to everyone, which they did not want [12]. ASHA, a selected trained female member from the community, works as an interface between the community and the public health system. AWW, also known as Integrated Child Development Services (ICDS) workers, are grassroots workers within the Integrated Child Development Services scheme, which aims to meet the essential health and nutritional needs of children, adolescent girls, and lactating mothers. The ASHA and AWW are the first contact points for health care seeking, mainly for women living in rural areas. Impolite health staff who do not respect confidentiality are barriers to early ANC utilization [10]. Literature reveals that women’s education is critical in obtaining early pregnancy registration [13, 14]. The average gestational age at registration and first-trimester appointment is closely connected for women with lower parity and those that have previously experienced stillbirths [13]. However, some studies show no link between a previous unfavorable obstetric history and the length of pregnancy at registration [15]. Morbidity in the index pregnancy and nulliparity favor early appointment considerably [15]. Despite considering pregnancy registration in the first trimester important, many women do not practice it, especially with increasing parity [16]. A 2009 study found that women with unplanned or mistimed pregnancies were more likely to delay starting prenatal care until after the first trimester than planned pregnancies [17]. The role of the husband behind the failure of pregnancy registration also become crucial as women are often dependent on their husband’s decisions [12]. A recent study found that socially marginalized groups, i.e., Scheduled Caste (SC), Scheduled Tribe (ST), and Other Backward Classes (OBC) have taken a longer time and late initiated the first ANC check-up (registration of pregnancy) than Non-SC/ST/OBC [18]. Most tribal women from East Khasi Hills failed to receive full ANC because they did not register early enough [19]. This late enrollment in the first ANC services among the lower caste groups might result in high infant and maternal morbidity and mortality [20]. One of the main causes of India’s unequal access to healthcare, low utilization of health services, and poor health outcomes are caste-based exclusion and discrimination [21, 22].
Early pregnancy registration contributes to improved maternal and child health. However, to our knowledge, no empirical study using nationally representative data has explored the correlates of pregnancy registration in India. Moreover, the relationship between pregnancy intention of last birth and pregnancy registration is inadequately explored. This study assesses the determinants of pregnancy registration, especially the role of the intention of the last birth in the country.
Materials and methods
Data
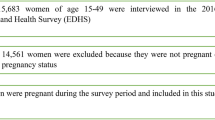
The present study used data from the nationally representative fifth round of the National Family Health Survey (NFHS) conducted in 2019-21. The NFHS-5 provides state and district-level estimates on various indicators such as maternal and child health, fertility, mortality, nutrition, family planning, domestic violence, and women empowerment. The survey used a two-stage stratified sampling technique in all states and union territories, covering 636,699 households, 724,115 women aged 15–49, and 101,839 men aged 15–54. The response rates of women, men, and households in NFHS-5 were 97%, 92%, and 98%, respectively. An informed consent procedure was followed, and only those who voluntarily consented were interviewed. The survey report contains the survey protocol, sampling, data collection tools, and quality control measures [23]. The survey has collected the pregnancy registration information for the most recent live birth to women during the five years preceding the survey. Specifically, the sample of women for whom the pregnancy registration status (N = 176,843) was available was analyzed for this study (Fig. 1).
Outcome variable
The outcome variable used in this analysis was ‘failure of pregnancy registration.‘ In the survey, for the last birth child, mothers were asked, ‘Was this pregnancy registered?’. Based on the response from mothers, the variable was coded in 0 as “no” and 1 as “yes.“
Exposure variables
This study included relevant exposure variables suggested by existing literature [15, 17]. Pregnancy intention of last birth was our main exposure variable, categorized into wanted, mistimed, and unwanted pregnancy. Additionally, the other key variables included in the analysis were the age of women (15–19, 20–24, 25–29, 30–34, 35–39 y, 40–49), years of schooling of the women (no schooling, 1–5 years, 6–10 years, 10 + years), parity (1, 2–3, 4+), history of obstetric complications (no, yes), interaction with ASHA)/AWW in last three months (no, yes), mass media exposure (exposed, not exposed), religion (Hindu, Muslim, others), social group (SC, ST, OBC, others), wealth index of the household (poorer, poor, middle, richer, richest), place of residence (rural, urban) and geographical region (north, central, east, northeast, west, south). Women exposed to television, radio, newspapers, and cinema were considered mass media exposure.
Statistical methods
We used bivariate and multivariable analysis to analyze the data. We used a logistic regression model to examine the association between exposure and outcome variables which were dichotomous.
Where \({b}_{0}, {b}_{1}, {b}_{2},.,{b}_{n}\)are coefficients of each exposure variable and ‘e’ denotes the error term. Binary logistic regression was conducted to examine the adjusted effect of socio-economic and demographic predictors of pregnancy registration and registration in the first trimester. The predictor variables included in the regression analysis were finalized after assessing their independent association with the outcome variable (pregnancy registration) and checking collinearity among the predictor variables. Multicollinearity was assessed through the Variance Inflation Factor (VIF) method. National individual sample weight was used in the analysis. The analysis was done in Stata (Version 16) with a 5% significance level.
Results
Table 1 shows the prevalence of failure of pregnancy registration by women’s socio-economic, demographic, and health-related characteristics. In 2019-21, 6% of the women did not register their last pregnancy. Women with mistimed pregnancies (12.6%) had the maximum registration failure, followed by unwanted pregnancies (8.2%). Failure of pregnancy registration had increased with the age of women. The highest proportion of failure of pregnancy registration was among women aged 40–49 years (11.2%). 8% of Muslim women failed to register their pregnancy compared to women who belong to other religions (6.6%) and Hindu women (5.8%). Women with no education and belonging to the lowest wealth quintile had the highest prevalence of failure of pregnancy registration (10.6% and 9.4%, respectively). The failure of pregnancy registration among women with four and above parity was twice as much as for women with one parity. Women who had consulted the ASHA/AWW in the last three months had the lowest prevalence (2.9%). Similarly, women exposed to any media had the lowest prevalence (4.9%). Failure in pregnancy registration also showed regional variation, southern India had the lowest, and the eastern part had the highest prevalence of failure of pregnancy registration. By looking at states/union territories, Nagaland (32%) had the highest percentage of failure to register pregnancy, followed by Bihar (16%), Manipur (15%), and Arunachal Pradesh (14%). The lowest percentage of failure to register pregnancy was found in Odisha, Karnataka, and Tamil Nadu, and all of these states had a 2% failure in pregnancy registration (Fig. 2).
Table 2 presents the result of the logistic regression of factors affecting the pregnancy registration. Model 1 shows the unadjusted odds ratio (OR). Women with mistimed pregnancies (OR = 2.26, 95% CI = 2.09–2.44), and unwanted pregnancies (OR = 1.42, 95% CI = 1.30–1.55) had higher odds of not registering their pregnancy as compared to women with wanted pregnancies. This association remained significant after adjusting the effects of other socio-economic and demographic characteristics used in Model 2. Mistimed and unwanted pregnancies had 60% (OR = 1.60, 95% CI = 1.47–1.73) and 38% (OR = 1.38, 95% CI = 1.26–1.52) higher likelihood of non-registration. Age had no statistically significant association with the failure of pregnancy registration. Women with higher education and wealth status were less likely to fail in registering their pregnancy than those with no schooling and the poorest wealth status. Women belonging to SC and OBC had a weak association with pregnancy registration. As compared to Hindu women, Muslim women (OR = 1.10; 95% CI = 1.04–1.16) and women who follow other religions (OR = 1.44; 95% CI = 1.30-1. 59) had a higher likelihood of failing in pregnancy registration. The parity of the women was directly proportional to the failure of pregnancy registration. Higher the parity of women, the higher the odds of failure of pregnancy registration. Women who consulted the ASHA/AWW in the last three months had a 79% (OR = 0.21; 95% CI = 0.20–0.22) lower chance of failure of pregnancy registration. Likewise, women exposed to mass media had lower odds of failure in pregnancy registration. Considering the regional variation, women of central (OR = 1.94; 95% CI = 1.79–2.11), eastern (OR = 2.24; 95% CI = 2.06–2.44), and north-eastern (OR = 1.26;95% CI = 1.10–1.44) part of the country had a significantly higher likelihood of failure of pregnancy registration compared to women of the southern region.
Discussion
The study found that pregnancy registration is not universal in India. The determinants of pregnancy registration varied considerably by socio-economic and demographic characteristics plus pregnancy intention of the last birth. The pregnancy intention of the last birth had a robust association with the pregnancy registration. Maternal education, parity, mass-media exposure, interaction with health workers, household wealth index, social group, religion, and region were other significant determinants of pregnancy registration.
The pregnancy intention of the last child is a significant determinant of the pregnancy registration. The failure of pregnancy registration was higher among women with either a mistimed or an unwanted last child. This result is in line with the previous studies, which found that unplanned birth had less chance of pregnancy registration and other negative implications on women’s reproductive and mental health [17, 24]. Non-registered pregnancies are again less likely to receive appropriate ANC, thus putting women at higher risk of maternal complications. Earlier studies reveal that women with inadequate ANC had higher maternal morbidities and mortality [25]. There is also low institutional delivery for those unintended births [26]. Additionally, inadequate ANC and non-institutionalized births for unintended pregnancies are detrimental to child health [27]. Early pregnancy registration would ensure appropriate ANC, vaccination, supplementary foods from ICDS, institutional delivery, and PNC, thus improving maternal and child health.
Maternal education positively influences the utilization of various maternal healthcare services [28]. Our study also found that educated women are more likely to register their pregnancies. As evidenced in a past study [15], this study also found an inverse association between failure to register pregnancy and parity. An African study revealed that women with earlier births cited their experience identifying maternal complications and frequent travel for ANC as the reason for delayed or no registration. We found that women with a history of pregnancy complications are less likely to fail to register their pregnancy. This conforms with earlier studies in India [14] and Africa [15]. The study found that interaction with the ASHA/AWW is beneficial for pregnancy registration. An earlier study [29] also documented the beneficial role of ASHA/AWW in enhancing the utilization of maternal healthcare services, including pregnancy registration. Nevertheless, some past studies suggest that due to impolite behavior and lack of confidentiality, women do not want to inform the ASHA and AWW about their pregnancy at an early stage, which lead to non-registration of pregnancy [10, 12]. Mass media exposure was found beneficial so far as pregnancy registration is concerned. This result conforms with a past study that reveals its contribution to the utilization of maternal healthcare services [30]. As compared to Hindu women, Muslim women and women who follow other religions are less likely to register their pregnancy. A previous study confirms the critical role of religion as a key determinant of women’s reproductive health-seeking behavior, as different religions follow different beliefs [31]. Past studies found wealth status of the household positively influences health-seeking behavior [20, 32]. Our study also reveals that failure of pregnancy registration decreases with the increasing economic condition of the household. Higher chances of pregnancy registration in rural areas may be credited to the outreach of the grass-root level health workers like ASHA/AWW. There is enough literature to prove the significant contribution of ASHA/AWW to improved maternal health [29, 33]. This study found a wide regional disparity in the registration of pregnancy. The lower likelihood of pregnancy registration in the country’s central and eastern regions, which comprise a sizable proportion of the country’s reproductive-age women, is a cause of concern.
Results suggest provision of context-specific, and culturally sensitive awareness programs regarding the benefits of early pregnancy registration to all eligible couples preferably by local grassroots-level health workers (ASHAs and AWWs). The risks of late pregnancy registration and the benefits of early pregnancy registration can also be advocated through several public interaction initiatives, i.e., awareness campaigns, street play, quizzes, lectures by local administrative authorities, such as Panchayati Raj Institutions (PRI), local educational institutions, and non-government organizations (NGO). Some previous studies have also advocated this [12, 14].
Strengths and limitations of the study
There are several strengths and limitations of this study. The findings are based on a large nationally representative sample of women covered in the NFHS-5 with a robust sampling design, which makes the findings relevant for policy and program. Secondly, to our knowledge, this is the first study to investigate several socio-economic and demographic determinants of pregnancy registration at a national level. However, the survey’s cross-sectional design limits pregnancy registration’s causal association with factors drawn from this analysis. Additionally, other socio-cultural factors could influence pregnancy registration, which could not be included in this analysis due to their unavailability in NFHS data. Despite this, the study’s findings would help strengthen the existing service delivery mechanism to increase early and overall pregnancy registration, thus ensuring better maternal and child health in the country.
Conclusion
Pregnancy intention is significantly associated with pregnancy registration in India. The grassroots-level health workers may strengthen their efforts to highlight the benefits of pregnancy registration, especially among women with possibly lower healthcare autonomy and unintended pregnancy. Pregnancy registration will enhance maternal healthcare utilization and reduce adverse health consequences for mothers and children, thus ensuring better health.
Data Availability
The datasets generated and/or analysed during the current study are available in the [Demographic and Health Surveys Repository] repository, [https://dhsprogram.com].
References
Bhatia M, Dwivedi LK, Banerjee K, Bansal A, Ranjan M, Dixit P. Pro-poor policies and improvements in maternal health outcomes in India. BMC Pregnancy Childbirth. 2021;21:389.
Pandey A, Das V, Agarwal A, Agrawal S, Misra D, Jaiswal N. Evaluation of obstetric near miss and maternal deaths in a tertiary care hospital in north India: shifting focus from mortality to morbidity. J Obstet Gynecol India. 2014;64:394–9.
Berhan Y, Berhan A. Antenatal care as a means of increasing birth in the health facility and reducing maternal mortality: a systematic review. Ethiop J Health Sci. 2014;24:93–104.
Darroch J, Singh S. Adding It Up: The Costs and Benefits of Investing In Family Planning and Maternal and Newborn Health Estimation Methodology. 2009.
Committee ES. The public health importance of antenatal care. Facts Views & Vision in ObGyn. 2015;7:5–6.
Kumar G, Choudhary TS, Srivastava A, Upadhyay RP, Taneja S, Bahl R, Martines J, Bhan MK, Bhandari N, Mazumder S. Utilisation, equity and determinants of full antenatal care in India: analysis from the National Family Health Survey 4. BMC Pregnancy Childbirth. 2019;19(1):327.
PRADHAN MANTRI SURAKSHIT MATRITVA ABHIYAN. [https://pmsma.mohfw.gov.in/about-scheme/.
Sadhana SM, STRENGTHENING THE MOTHER AND CHILD TRACKING SYSTEM THROUGH AN ENHANCED REVIEW MECHANISM USING A SIMPLE TOOL. BMJ Global Health. 2016;1(Suppl 1):A33.
Gaitonde R. Registration and monitoring of pregnant women in Tamil Nadu, India: a critique. Reprod Health Matters. 2012;20:118–24.
Chimatiro C, Hajison P, Chipeta E, Muula A. Understanding barriers preventing pregnant women from starting antenatal clinic in the first trimester of pregnancy in Ntcheu District-Malawi. Reproductive Health 2018, 15.
Finlayson K, Downe S. Why do women not use Antenatal Services in low- and Middle-Income Countries? A Meta-synthesis of qualitative studies. PLoS Med. 2013;10:e1001373.
Khan SS, Tawale NK, Patel A, Dibley MJ, Alam A. My husband is my family. The culture of pregnancy disclosure and its implications on early pregnancy registration in a child nutrition intervention in rural Maharashtra, India. Midwifery. 2021;103:103141.
Oladokun A, Oladokun RE, Morhason-Bello I, Bello AF, Adedokun B. Proximate predictors of early antenatal registration among nigerian pregnant women. Ann Afr Med. 2010;9:222–5.
Patel PB, Rupani MP, Patel SS. Antenatal care registration and predicting factors of late registration among pregnant women. Trop Doct. 2013;43:9–12.
Okunlola MA, Ayinde OA, Owonikoko KM, Omigbodun AO. Factors influencing gestational age at antenatal booking at the University College Hospital, Ibadan, Nigeria. J Obstet Gynaecology: J Inst Obstet Gynecol. 2006;26:195–7.
Kisuule I, Kaye DK, Najjuka F, Ssematimba SK, Arinda A, Nakitende G, Otim L. Timing and reasons for coming late for the first antenatal care visit by pregnant women at Mulago hospital, Kampala Uganda. BMC Pregnancy Childbirth. 2013;13:121.
Cheng D, Schwarz EB, Douglas E, Horon I. Unintended pregnancy and associated maternal preconception, prenatal and postpartum behaviors. Contraception. 2009;79:194–8.
Tripathy A, Mishra PS. Inequality in time to first antenatal care visits and its predictors among pregnant women in India: an evidence from national family health survey. Sci Rep. 2023;13(1):4706.
Deb R. Utilization of services related to safe motherhood among the Tribal Population of East Khasi Hills (Meghalaya): an overview. Ethno-Med 2007, 2.
Hamal M, Dieleman M, De Brouwere V, de Cock Buning T. Social determinants of maternal health: a scoping review of factors influencing maternal mortality and maternal health service use in India. Public Health Rev. 2020;41:13.
Borooah V. Inequality in Health Outcomes in India: the role of Caste and Religion. Blocked by Caste: economic discrimination in modern India. edn.: Oxford University Press; 2010: 179–207.
Srinivasan K, Mohanty SK. Deprivation of Basic amenities by Caste and Religion: empirical study using NFHS Data. Economic and Political Weekly. 2004;39(7):728–35.
International Institute for Population Sciences (IIPS), ICF. National Family Health Survey NFHS-5 2019-21. Mumbai, India: IIPS and ICF; 2022.
Goossens J, Van Den Branden Y, Van der Sluys L, Delbaere I, Van Hecke A, Verhaeghe S, Beeckman D. The prevalence of unplanned pregnancy ending in birth, associated factors, and health outcomes. Hum Reprod (Oxford England). 2016;31:2821–33.
Linard M, Blondel B, Estellat C, Deneux-Tharaux C, Luton D, Oury JF, Schmitz T, Mandelbrot L, Azria E. Group tPs: Association between inadequate antenatal care utilisation and severe perinatal and maternal morbidity: an analysis in the PreCARE cohort. BJOG: An International Journal of Obstetrics & Gynaecology. 2018;125:587–95.
Wado YD, Afework MF, Hindin MJ. Unintended pregnancies and the use of maternal health services in Southwestern Ethiopia. BMC Int Health Hum Rights. 2013;13:36.
Kuhnt J, Vollmer S. Antenatal care services and its implications for vital and health outcomes of children: evidence from 193 surveys in 69 low-income and middle-income countries. BMJ Open. 2017;7:e017122.
Barman B, Saha J, Chouhan P. Impact of education on the utilization of maternal health care services: an investigation from National Family Health Survey (2015–16) in India. Child Youth Serv Rev. 2020;108:104642.
Agarwal S, Curtis S, Angeles G, Speizer I, Singh K, Thomas J. The impact of India’s accredited social health activist (ASHA) program on the utilization of maternity services: a nationally representative longitudinal modelling study. Hum Resour Health 2019, 17.
Fatema K, Lariscy JT. Mass media exposure and maternal healthcare utilization in South Asia. SSM - population Health. 2020;11:100614.
Kachoria AG, Mubarak MY, Singh AK, Somers R, Shah S, Wagner AL. The association of religion with maternal and child health outcomes in south asian countries. PLoS ONE. 2022;17(7):e0271165.
Yadav AK, Sahni B, Jena PK, Kumar D, Bala K. Trends, Differentials, and social determinants of maternal Health Care Services utilization in rural India: an analysis from Pooled Data. Women’s Health Reports. 2020;1:179–89.
Nadella P, Subramanian SV, Roman-Urrestarazu A. The impact of community health workers on antenatal and infant health in India: a cross-sectional study. SSM - Population Health. 2021;15:100872.
Acknowledgements
Not Applicable.
Funding
The authors received no financial support from any funding agency, commercial entity, or not-for-profit organization for the research, authorship and/or publication of this article.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript. SM: Methodology, Literature review, editing and final approval; AA: Methodology, data analysis, editing and final approval; NA: Methodology, Literature review, editing and final approval; BS: Methodology, data analysis, editing and final approval; MRP: Conceptualization, methodology, writing first draft, editing and final approval.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study is based on the publicly available data source, and survey agencies that conducted the field survey for the data collection have also collected a prior consent from the respondent. The NFHS-5 was approved by the Institutional Review Board of the Institutions involved, and the datasets are available at https://www.dhsprogram.com for broader use in social research. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. They ruled that no formal ethical consent was required to conduct research from this data source.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mondal, S., Anand, A., Awasthi, N. et al. Factors affecting pregnancy registration in India: does the pregnancy intention matter?. BMC Pregnancy Childbirth 23, 674 (2023). https://doi.org/10.1186/s12884-023-06002-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-06002-9