Abstract
Background
Sub-Saharan Africa (SSA) has seen an increase in facility-based births over the years. However, the region has the world’s highest newborn mortality rate (42% in 2019). Quality care around the time of birth can avert these deaths. This study examined the newborn care interventions given to women who gave birth in health facilities in 17 countries in SSA.
Methods
A cross-sectional population-based study was conducted. We used data from the most recent Demographic and Health Surveys (DHS) conducted in 17 sub-Saharan African countries. We analysed a weighted sample of 226,706 women aged 15–49 years who gave birth in the five years preceding the surveys. We described the coverage of nine newborn care services, namely weighing at birth, breastfeeding initiation within 1 h after birth, skin-to-skin contact, temperature measurement, cord examination, counselling on newborn danger signs, counselling on breastfeeding, breastfeeding observation, and child health assessment before discharge.
Results
Overall, 72.0% (95% CI: 71.1, 72.8) of births occurred in health facilities, ranging from 40.0% (95% CI: 38.0, 42.1) in Nigeria to 96.3% (95% CI: 95.4, 97.1) in South Africa. Weighing at birth was the most common intervention (91.4%), followed by health checks before discharge (81%). The other interventions, including those given immediately at birth (breastfeeding and skin-to-skin contact), had suboptimal coverage. For instance, 66% of newborns were breastfed within 1 h after birth, and 56% had immediate skin-to-skin contact. Service coverage varied considerably by country and healthcare provider type.
Conclusions
The majority of the examined services, namely early breastfeeding, skin-to-skin contact, cord examination, temperature measurement, counselling on newborn danger signs, breastfeeding observation, and counselling on breastfeeding, were found to have suboptimal coverage. Even though many pregnant women in SSA give birth in healthcare facilities, some newborns do not always get the care they need to be healthy and live. This is a missed chance to improve newborn health and survival around the time of birth.
Similar content being viewed by others
Background
Newborn survival has improved. From 37 deaths per 1,000 live births in 1990 to 17 deaths per 1,000 live births in 2019, the global neonatal mortality rate went down by 52%, though it went down more slowly than deaths among children 1–59 months old [1]. In 2019, an estimated 2.4 million children died in their first month of life, with more than half of neonatal deaths occurring in the first 3 days of life and about two-thirds of these deaths occurring on the first day alone [1, 2]. Most of these deaths are preventable and occur in low- and middle-income countries (LMICs). Sub-Saharan Africa (SSA) alone accounted for 42% of all newborn deaths in 2019, the highest globally [1].
Preterm delivery complications, intrapartum events like birth asphyxia, or infections like sepsis or pneumonia account for almost 80% of newborn mortality [3].The Every Newborn Action Plan (ENAP) was adopted in June 2014 in response to the increasing focus on newborn mortality. The ENAP emphasised the strategic importance of focusing on quality care around the time of delivery. This includes ensuring that all pregnant women have access to the skilled quality care required for a healthy pregnancy, newborn protection, and care for small and sick babies [4]. This also aligns with the World Health Organization’s (WHO) recommendation on having a skilled attendant at birth to reduce mortality. However, the benefits of a skilled attendant at birth in reducing neonatal mortality are most clearly seen in the services provided during labour and delivery to prevent deaths and improve survival [5]. Therefore, concentrating on the period just before birth with crucial interventions that have been demonstrated to have a significant impact and providing good care for infants who are small or ill could prevent up to 80% of newborn deaths [3]. Essential newborn care includes care right after the baby is born and care throughout the first few weeks of life, such as delaying cord clamping, drying the baby well, checking the baby’s breathing, skin-to-skin contact, and breastfeeding as soon as possible [6, 7].
A significant portion of the extant scholarly works in Sub-Saharan Africa (SSA) have been dedicated to the investigation of antenatal care (ANC), comprising its scope of coverage, frequency of utilization, and the factors influencing its use [8,9,10,11]. Similarly, considerable attention has been paid to the locale of childbirth, particularly its extent of coverage, and the determinants of facility-based delivery [11,12,13,14]. We also found studies that examined services provided during the postpartum period, but their scope was limited. Benova and company, for instance, examined postnatal checks for women who gave birth in health facilities in SSA [15]. The focus of their study was whether the mother received a check-up by a health provider while in the facility and before discharge. Tessema and colleagues also investigated the determinants of postnatal care check up by health professionals within 42 days after birth among women in SSA [16]. As a result, there is still a lack of information about the coverage of essential services given to mothers and their newborns in health facilities after delivery to improve the health of newborns.
The current study used data from the most recent Demographic and Health Surveys (DHS) from 17 countries in SSA to examine the extent of coverage of certain newborn care interventions for women who gave birth at health facilities during the postpartum period. More specifically, the investigation focused on determining the percentage of postpartum women and their newborns who received essential services, including timely initiation of breastfeeding, skin-to-skin contact, examination of the umbilical cord, and measurement of body temperature, at the healthcare establishments where delivery occurred.
Methods
Study design, setting, and source of data
We used the most recent DHS, which was conducted in 17 SSA countries. These countries collected data on all the examined interventions, making them suitable for the present study. The DHS, funded by the United States Agency for International Development (USAID), collects information on a wide range of health indicators for the population, with a strong focus on the health of women and children. So far, the DHS is the primary source of information on the population-level coverage of health interventions for newborns. Standardized questionnaires are used in these surveys, ensuring that the information collected can be compared across countries. Strategies and methods for sampling have been explained previously [17].
Participants
Our target population consisted of all women of reproductive age (15–49 years) who had given birth in the past 5 years preceding the surveys. After appending, the dataset contained 230,127 observations. However, we included 226,706 women who gave birth vaginally or via caesarean section; that is, 3421 observations were excluded because the place of delivery could not be reliably identified. The sample was weighted for the final analysis. The survey data ranged from 2011 to 2020.
Interventions examined
In the DHS, women who gave birth were asked about the postpartum care they received while at the delivery facility. We incorporated nine interventions: (1) weighing of the newborn at birth; (2) immediate skin-to-skin contact; (3) timing of breastfeeding initiation; (4) examination of the newborn’s umbilical cord; (5) measurement of the newborn’s temperature; (6) counselling of the mother on danger signs for newborns; (7) counselling of the mother on breastfeeding; (8) observing the newborn breastfeeding; and (9) checking the baby’s health before discharge. We acknowledge that essential newborn care services encompass a broad range of services, including but not limited to delayed cord clamping, infection prevention, thorough drying, nurturing care, and timely and safe referral when needed, among others [6, 7]. However, we chose services that were measured in most (17 countries) of the countries in SSA.
Statistical analysis
In the current study, descriptive statistics were used. In each country, the percentage of women who delivered their most recent baby in a health facility was calculated. Home deliveries, including those performed by traditional birth attendants (TBAs), are births that took place outside of healthcare institutions. Then we used a design-based Chi-square analysis on only the pooled data to compare the characteristics of women who delivered in healthcare facilities against those who delivered at home or with TBAs. We estimated the coverage of each newborn care intervention as the percentage of mothers who reported that the intervention was provided at the delivery healthcare facility. This analysis was restricted to only women who reported giving birth in healthcare facilities (N = 163, 185). All the analyses were carried out using STATA/IC 15.0 for Windows (StataCorp LLC, College Station, TX 77,845, USA). A probability value (p-value) of less than 0.05 was considered statistically significant. We used weighting factors to account for the DHS’s non-proportional sampling methods in its surveys [17]. In the analysis, the “svset” and “svy” commands were used to apply the complex survey design in our estimations.
Ethical considerations
The current study analysed de-identified secondary data from the DHS. Therefore, no approval from an Institutional Review Board (IRB) was required. However, the DHS programme received ethical approval from both the Inner City Fund IRB and the IRB of the host nation. The surveys are conducted in accordance with the principles and ethics of health research involving human subjects. You can find the rules for protecting the privacy of survey respondents and household members in all DHS surveys 0n the DHS website (https://dhsprogram.com/Methodology/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm). We had access to the raw datasets used in the current study after obtaining written approval from the DHS program through the ICF.
Results
Prevalence of health facility delivery in the 17 sub-Saharan African countries
A weighted sample of 226,706 women aged 15–49 years who delivered vaginally or by caesarean section was analyzed. According to the results, the percentage of women who delivered in health facilities varied by country. Health facility delivery ranged from 40.0% (95% CI: 38.0, 42.1) in Nigeria to 96.3% (95% CI: 95.4, 97.1) in South Africa. The pooled results indicated that 72.0% (95% CI: 71.1, 72.8) of the deliveries occurred in health institutions. In six (35.3%) of the seventeen countries, that is Angola, Congo, Guinea, Mali, Nigeria, and Tanzania, health facility delivery was below the average of 72.0% (Table 1).
Comparison of the characteristics of women who delivered in healthcare facilities in the 17 sub-Saharan African countries
Our pooled analysis revealed that women who delivered in health facilities in the 17 SSA countries differed significantly from those who delivered at home in terms of sociodemographic, economic, and obstetrical characteristics. Compared to their counterparts, a greater percentage of women aged 15–24 (73.3%) delivered in healthcare facilities compared to women in the age groups of 25–34 (72.6%) and 35–49 (69.1%). A higher percentage of women with at least secondary education (87.1%) and women who have never been in a union (84.3%) delivered in healthcare facilities compared to their counterparts. Regarding ANC use, 75.4% of women who used ANC at least once during their recent pregnancy delivered in healthcare facilities, compared to 17.8% of women who did not use ANC. A significantly higher percentage of women who resided in urban areas (84.0%) delivered in healthcare facilities compared to 65.6% of women in rural settings. A higher percentage of women from the richest households (93.4%) gave birth in healthcare facilities compared to women from households in the other wealth groups (Table 2).
Coverage of essential newborn care services among women who delivered in health facilities in the 17 sub-Saharan African countries.
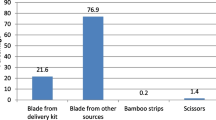
There were disparities in the coverage of newborn care services among women who gave birth in health facilities in the 17 SSA countries. Among the examined services, weighing at birth was commonly reported by 91.4% of the sample (ranging from 60% in Liberia to 99.1% in Rwanda and Zimbabwe), followed by checking a child’s health before discharge (80.7%). Counselling on newborn danger signs had the lowest coverage of 53.0% (ranging from 31.5% in Mali to 82.4% in Sierra Leone). The coverage rates for breastfeeding initiation within 1 h of birth and immediate skin-to-skin contact were 66.2% (ranging from 37.6% in Gambia to 86.8% in Rwanda) and 55.8% (ranging from 12.7% in Burundi to 86.7% in Benin), respectively (Fig. 1 and Additional file 1: Table S1). When the analysis excluded women who delivered through caesarean section (see Additional file 1: Table S1), we observed that early breastfeeding initiation was 68.8% (ranging from 38.8% in Gambia to 91.6% in Rwanda), while immediate skin-to-skin was 57.5% (ranging from 13.1% in Burundi to 89.1% in Benin).
Coverage of essential newborn care services by healthcare provider type
We also analysed newborn service coverage by type of health care provider. According to the data (Table 3), the coverage of the following services was comparable between public and private health facilities: weight taking at birth, counselling on newborn danger signs, counselling on breastfeeding, and observation of breastfeeding. The coverage of services, such as breastfeeding initiation within 1 h after birth, skin-to-skin contact, cord examination, and temperature measurement, varied considerably between public and private health institutions. A greater percentage of newborns in private facilities than in public facilities have their cords examined, their temperatures taken, and their health checked before discharge. In private facilities, the rate of cord examination is 62.7%, compared to 59.6% in public facilities. Similarly, private health facilities measure newborn temperatures at a rate of 62.1%, compared to 57.4% in public health facilities. Also, the percentage of children’s health checked before discharge at private health facilities was 83.5% compared to 80.2% in public health facilities. In contrast, public health facilities had higher rates of early breastfeeding initiation within 1 h after birth and skin-to-skin contact coverage than private ones. For instance, initiation of breastfeeding within 1 h of birth was more prevalent (67.0%) in public health facilities than in private health facilities (60.97%). Similarly, the rate of immediate skin-to-skin contact was 56.5% in public health facilities and 51.1% in private health facilities (Table 3).
Discussion
The purpose of this descriptive study was to examine the coverage of nine newborn care interventions among women who delivered in healthcare facilities in seventeen countries in SSA. We discovered that more than two-thirds of deliveries took place in healthcare facilities, with Nigeria having the lowest rate and South Africa having the highest. The documented rate of health facility delivery in the current study is greater than the 66% reported by Adde et al. in their analysis of 28 countries in SSA [12]. The estimate of health facility delivery is based on a pooled analysis and may be influenced by country-level coverages. As a result, we suspect that the lower estimate reported by Adde et al.’s study, which rather included a relatively higher number of countries, was influenced by low prevalence rates observed in more than half of the included countries, which probably obscured the high coverages in the remaining few countries. However, similar to the current study’s findings, there were substantial variations in prevalence rates between countries. Based on their findings, the percentage of births that occurred in health facilities ranged from 23% in Chad to 94% in Gabon.
In the first 3 days after birth, more than half of neonatal deaths occur [2]. Reducing mortality during this period would require evidenced-based interventions such as postnatal care and care for small babies and sick newborns. Immediate care at birth, specifically early breastfeeding initiation within 1 h after birth and immediate skin-to-skin contact, improves newborn health and survival. Early breastfeeding initiation reduces the risk of neonatal morbidity and mortality [18,19,20]. Immediate skin-to-skin contact reduces neonatal hypothermia and maintains optimal body temperature [21]. Skin-to-skin newborns were more likely to be breastfed early than those who were not [21,22,23]. Feldman et al. also found that children who were put in skin-to-skin contact with their mothers had better autonomic functioning and cognitive control in their first 10 years of life [24]. The act of weighing neonates at birth could aid in the identification of infants with distinct healthcare requirements, notably those who are born with a low birthweight, warranting specific attention and interventions to improve their chances of survival. According to survey data from 20 SSA countries, babies weighed at birth are less likely to die within the first 27 days of life [20]. Despite these obvious benefits, the current study revealed that coverage of most essential newborn interventions, including those classified under “immediate care at birth” (initiation of breastfeeding within 1 h and skin-to-skin contact) by the WHO, is less than optimal across countries. Only weight taking at birth and assessing the child’s health at discharge had higher coverage rates among the interventions. It is important to note, however, that the current study’s coverage of early breastfeeding initiation and immediate skin-to-skin contact is higher than previously reported [25, 26]. We also found that coverage of five interventions: early breastfeeding initiation within 1 h after birth, immediate skin-to-skin contact, cord examination, temperature taking, and checking the child’s health before discharge differed substantially by provider type. Private facilities outperformed public health in providing quality primary health care according to a previous study conducted in the current study’s setting [27]. In the current study, private facilities had higher coverage in three of the five interventions that differed by provider type, thus outperforming public ones. However, newborns were more likely to receive early breastfeeding and skin-to-skin contact in public health facilities than in private facilities. This finding confirms earlier research indicating that babies in Uganda were more likely to receive thermal care practises in public facilities than in private ones [28].
The current study’s design prevented us from investigating the factors underlying the observed coverages. Furthermore, we believe that because women gave birth in healthcare facilities, any differences in services received may be related to the healthcare system in question. However, aside from the type of provider, the datasets used for the current analysis did not contain information about the healthcare system that we could investigate further. Nonetheless, existing literature suggests that a variety of factors, including service readiness, may influence the variation in service coverage between countries. An assessment of the health service environment revealed that newborns in areas with high service readiness are more likely to receive essential newborn care [29]. Major deficiencies in essential newborn care supplies and equipment, health care worker density, as well as in health worker knowledge and performance of key routine newborn care practices, especially for immediate skin-to-skin contact and breastfeeding initiation, were also identified in a cross-section of health facilities across six eastern SSA nations: Ethiopia, Kenya, Madagascar, Mozambique, Rwanda, and Tanzania [30].
The facility’s delivery of newborn services can be impacted by several factors, including the mode of delivery and other newborn outcomes, such as birth weight and Apgar score. Notably, cesarean deliveries were found to exhibit a decreased likelihood of early breastfeeding within the first hour after birth and immediate skin-to-skin contact, in comparison to spontaneous vaginal deliveries [22, 23, 31, 32]. Similarly, it was observed that women exhibited decreased likelihood to commence skin-to-skin contact and initiate early breastfeeding when their neonates presented with an Apgar score of less than seven at one minute post-delivery [33]. Low birthweight infants, on the other hand, were more likely to engage in immediate skin-to-skin contact with their mothers than babies born with a normal birthweight [25]. Furthermore, it was observed that singleton births were associated with a higher likelihood of initiating early breastfeeding compared to multiple births or twin deliveries [34]. As shown in the current study, coverages of early breastfeeding and immediate skin-to-skin contact increased when caesarean births were excluded in the analyses. Unfortunately, our analysis was unable to assess the potential influence of Apgar score at birth and birth type on these interventions.
Heterogeneity between the countries also explains the observed variations in the coverage of newborn services. In assessing the quality of primary health care services in seven countries across eastern, western, and southern Africa, Kruk and her colleagues found that differences between countries were more important than all other factors in explaining differences in care quality [27]. The quality of maternal and newborn care services in SSA differs by country due to a range of factors, including variations in health system infrastructure, health workforce availability and capacity, financing mechanisms, and political will. In countries where there is insufficient or weak health infrastructure, inadequate health workforce, limited health expenditure, and weak political commitment, the quality of healthcare services is often suboptimal [35].
Interpretation
This study’s findings have implications for stakeholders and policymakers who are involved in neonatal and child health. First, the findings confirm that there is a gap in the quality of care during the critical period of a newborn’s life in some SSA countries. In particular, even though a substantial proportion of pregnant women in nearly half of countries in SSA utilize the health system to deliver, the essential interventions required to promote optimal health and survival of the newborn after birth are not always available, and even when they are, they are not always provided.
Second, there is an urgent need to increase the proportion of newborns receiving essential newborn care interventions in healthcare facilities during the critical period of life. SSA is particularly important given the high mortality across all age groups and the continuous population growth. The region is estimated to realise 446 million births by 2030 [36]. The rapid increase in the number of births and population necessitates increased investment in newborn and child survival interventions as well as strengthening the health systems that provide them, otherwise neonatal mortality in the region may stagnate or worsen. There are a variety of strategies to improve the coverage of newborn care interventions at the facility level in LMICs, including training for key staff, implementation of checklists or job aids, and task shifting [7]. Nonetheless, to be effective, these interventions need to be well-described and accompanied by systems for monitoring and reporting implementation outcomes.
Study strengths and limitations
This study used nationally representative data from 17 SSA countries to investigate the coverage of essential newborn care services provided to women who deliver at health facilities during the postpartum period. This study adds to the literature on the quality gap during the postpartum period in these countries. However, although the current study provides useful information that could potentially, aid in the improvement of newborn care services in LMICs, some weaknesses have to be acknowledged. The current study has a descriptive design. As a result, we could only provide information on the coverage of the interventions examined; we were unable to examine the specific reasons for these coverages through analysis. Also, there are several newborn care services available. However, we only examined nine interventions because information on them was available for only 17 countries. It is imperative to acknowledge that these interventions must not supersede other measures such as infection control and neonatal resuscitation. It is unfortunate that the surveys conducted by DHS do not capture data on these interventions. We used secondary data from surveys of women who had their most recent baby within the previous five years. Women’s deliveries could have occurred up to three or four years before the survey, and they may not remember whether or not a certain service was provided. As a result, the possibility of recall errors cannot be ruled out. However, a study demonstrated that women could accurately recall maternal and newborn interventions received in the postnatal period [37]. Furthermore, we encountered a challenge in discerning between preterm and asphyxiated infants from healthy newborns using the dataset. Another limitation is that the DHSs are conducted on an ongoing basis, and the data from the participating countries in the current study were not collected at the same time, limiting contemporaneous cross-country comparisons by time. Nonetheless, we used data from the most recent surveys, which allowed us to learn about the most recent trends within these countries.
Conclusion
The study found that, among the majority of the services examined, namely early breastfeeding, skin-to-skin contact, cord examination, temperature measurement, counselling on newborn danger signs, breastfeeding observation, and counselling on breastfeeding, coverage was found to be less than optimal. From the study, although a significant percentage of pregnant women in SSA give birth in health facilities, the essential interventions that are needed to promote newborn health and survival are sometimes not provided. The findings demonstrate a missed opportunity around the time of birth to promote newborn survival in many SSA countries.
Data Availability
The data underlining the conclusions drawn in this study are contained within the manuscript. The dataset, however, can be obtained freely from the DHS website (https://dhsprogram.com/data/dataset_admin/index.cfm) with permission from the DHS program. The authors do not have the right to share the dataset with other researchers without approval from the DHS program.
Abbreviations
- ANC:
-
Antenatal care
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- DHS:
-
Demographic and Health Survey
- ENAP:
-
Every Newborn Action Plan
- IRB:
-
Institutional Review Board
- LMICs:
-
low-and-middle income countries
- SSA:
-
sub-Saharan Africa
- TBAs:
-
Traditional Birth Attendants
- USAID:
-
United State Agency for International Development
- WHO:
-
World Health Organization
References
United Nations Inter-agency Group for Child Mortality Estimation (UN IGME). Levels & Trends in Child Mortality: Report 2020, Estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation. New York. : 2020. https://cdn.who.int/media/docs/default-source/mca-documents/child/levels-and-trends-in-child-mortality-igme-english_2020_.pdf (accessed 13 Sep 2021).
Sankar MJ, Natarajan CK, Das RR, et al. When do newborns die? A systematic review of timing of overall and cause-specific neonatal deaths in developing countries. J Perinatol. 2016;36:1–11. https://doi.org/10.1038/jp.2016.27.
Ahmed I, Ali SM, Amenga-Etego S, et al. Population-based rates, timing, and causes of maternal deaths, stillbirths, and neonatal deaths in south Asia and sub-saharan Africa: a multi-country prospective cohort study. Lancet Glob Heal. 2018;6:e1297–308. https://doi.org/10.1016/S2214-109X(18)30385-1.
World Health Organization. Every newborn: An action plan to end Preventable deaths: Executive summary Geneva: World Health Organization. Geneva. : 2014. https://www.who.int/initiatives/every-newborn-action-plan (accessed 10 Jan 2022).
Bhutta ZA, Das JK, Bahl R, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet. 2014;384:347–70. https://doi.org/10.1016/S0140-6736(14)60792-3.
Madaj B, Smith H, Mathai M, et al. Developing global indicators for quality of maternal and newborn care: a feasibility assessment. Bull World Health Organ. 2017;95:445–452I. https://doi.org/10.2471/BLT.16.179531.
Peven K, Bick D, Purssell E, et al. Evaluating implementation strategies for essential newborn care interventions in low- and low middle-income countries: a systematic review. Health Policy Plan. 2020;35:ii47–65. https://doi.org/10.1093/heapol/czaa122.
Adedokun ST, Yaya S. Correlates of antenatal care utilization among women of reproductive age in sub-saharan Africa: evidence from multinomial analysis of demographic and health surveys (2010–2018) from 31 countries. Arch Public Heal. 2020;78:134. https://doi.org/10.1186/s13690-020-00516-w.
Okedo-Alex IN, Akamike IC, Ezeanosike OB, et al. Determinants of antenatal care utilisation in sub-saharan Africa: a systematic review. BMJ Open. 2019;9:e031890. https://doi.org/10.1136/bmjopen-2019-031890.
Tessema ZT, Teshale AB, Tesema GA, et al. Determinants of completing recommended antenatal care utilization in sub-saharan from 2006 to 2018: evidence from 36 countries using demographic and health surveys. BMC Pregnancy Childbirth. 2021;21:192. https://doi.org/10.1186/s12884-021-03669-w.
Woldegiorgis MA, Hiller J, Mekonnen W, et al. Determinants of antenatal care and skilled birth attendance in sub-saharan Africa: a multilevel analysis. Health Serv Res. 2019;54:1110–8. https://doi.org/10.1111/1475-6773.13163.
Adde KS, Dickson KS, Amu H. Prevalence and determinants of the place of delivery among reproductive age women in sub–Saharan Africa. PLoS ONE. 2020;15:e0244875. https://doi.org/10.1371/journal.pone.0244875.
Doctor HV, Nkhana-Salimu S, Abdulsalam-Anibilowo M. Health facility delivery in sub-saharan Africa: successes, challenges, and implications for the 2030 development agenda. BMC Public Health. 2018;18:765. https://doi.org/10.1186/s12889-018-5695-z.
Gebremichael SG, Fenta SM. Determinants of institutional delivery in Sub-Saharan Africa: findings from demographic and Health Survey (2013–2017) from nine countries. Trop Med Health. 2021;49:45. https://doi.org/10.1186/s41182-021-00335-x.
Benova L, Owolabi O, Radovich E, et al. Provision of postpartum care to women giving birth in health facilities in sub-saharan Africa: a cross-sectional study using demographic and Health Survey data from 33 countries. PLOS Med. 2019;16:e1002943. https://doi.org/10.1371/journal.pmed.1002943.
Tessema ZT, Yazachew L, Tesema GA, et al. Determinants of postnatal care utilization in sub-saharan Africa: a meta and multilevel analysis of data from 36 sub-saharan countries. Ital J Pediatr. 2020;46:175. https://doi.org/10.1186/s13052-020-00944-y.
Croft TN, Aileen MMJ, Courtney AK. Guide to DHS Statistics. 2018.https://dhsprogram.com/data/Guide-to-DHS-Statistics/index.cfm
Debes AK, Kohli A, Walker N, et al. Time to initiation of breastfeeding and neonatal mortality and morbidity : a systematic review. BMC Public Health. 2013;13:19.
Smith ER, Hurt L, Chowdhury R, et al. Delayed breastfeeding initiation and infant survival: a systematic review and meta-analysis. PLoS ONE. 2017;12:e0180722. https://doi.org/10.1371/journal.pone.0180722.
Amouzou A, Ziqi M, Carvajal–Aguirre L, et al. Skilled attendant at birth and newborn survival in Sub–Saharan Africa. J Glob Health. 2017;7. https://doi.org/10.7189/jogh.07.020504.
Safari K, Saeed AA, Hasan SS, et al. The effect of mother and newborn early skin-to-skin contact on initiation of breastfeeding, newborn temperature and duration of third stage of labor. Int Breastfeed J. 2018;13:32. https://doi.org/10.1186/s13006-018-0174-9.
Seidu A, Ahinkorah BO, Agbaglo E, et al. Determinants of early initiation of breastfeeding in Papua New Guinea: a population-based study using the 2016–2018 demographic and health survey data. Arch Public Heal. 2020;78:124. https://doi.org/10.1186/s13690-020-00506-y.
Singh K, Khan SM, Carvajal–Aguirre L, et al. The importance of skin–to–skin contact for early initiation of breastfeeding in Nigeria and Bangladesh. J Glob Health. 2017;7:1–9. https://doi.org/10.7189/jogh.07.020505.
Feldman R, Rosenthal Z, Eidelman AI. Maternal-preterm skin-to-skin contact enhances child physiologic organization and cognitive control across the first 10 years of life. Biol Psychiatry. 2014;75:56–64. https://doi.org/10.1016/j.biopsych.2013.08.012.
Aboagye RG, Boah M, Okyere J, et al. Mother and newborn skin-to-skin contact in sub-saharan Africa: prevalence and predictors. BMJ Glob Heal. 2022;7:e007731. https://doi.org/10.1136/bmjgh-2021-007731.
Appiah F, Ahinkorah BO, Budu E, et al. Maternal and child factors associated with timely initiation of breastfeeding in sub-saharan Africa. Int Breastfeed J. 2021;16:55. https://doi.org/10.1186/s13006-021-00402-3.
Kruk ME, Chukwuma A, Mbaruku G, et al. Variation in quality of primary-care services in Kenya, Malawi, Namibia, Rwanda, Senegal, Uganda and the United Republic of Tanzania. Bull World Health Organ. 2017;95:408–18. https://doi.org/10.2471/BLT.16.175869.
Waiswa P, Akuze J, Peterson S, et al. Differences in essential newborn care at birth between private and public health facilities in eastern Uganda. Glob Health Action. 2015;8:24251. https://doi.org/10.3402/gha.v8.24251.
Carvajal–Aguirre L, Mehra V, Amouzou A, et al. Does health facility service environment matter for the receipt of essential newborn care? Linking health facility and household survey data in Malawi. J Glob Health. 2017;7. https://doi.org/10.7189/jogh.07.020508.
de Graft-Johnson J, Vesel L, Rosen HE, et al. Cross-sectional observational assessment of quality of newborn care immediately after birth in health facilities across six sub-saharan african countries. BMJ Open. 2017;7:e014680. https://doi.org/10.1136/bmjopen-2016-014680.
Exavery A, Kanté AM, Hingora A, et al. Determinants of early initiation of breastfeeding in rural Tanzania. Int Breastfeed J. 2015;10:27. https://doi.org/10.1186/s13006-015-0052-7.
Liben ML, Yesuf EM. Determinants of early initiation of breastfeeding in Amibara district, northeastern Ethiopia: a community based cross-sectional study. Int Breastfeed J. 2016;11:7. https://doi.org/10.1186/s13006-016-0067-8.
Lau Y, Tha PH, Ho-Lim SST, et al. An analysis of the effects of intrapartum factors, neonatal characteristics, and skin-to-skin contact on early breastfeeding initiation. Matern Child Nutr. 2018;14:e12492. https://doi.org/10.1111/mcn.12492.
Nkoka O, Ntenda PAM, Kanje V, et al. Determinants of timely initiation of breast milk and exclusive breastfeeding in Malawi: a population-based cross-sectional study. Int Breastfeed J. 2019;14:37. https://doi.org/10.1186/s13006-019-0232-y.
Kruk ME, Gage AD, Arsenault C, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob Heal. 2018;6:e1196–252. https://doi.org/10.1016/S2214-109X(18)30386-3.
United Nations Department of Economics and Social Affiairs Population Division. World Population Prospects 2019: Highlights. 2019. https://population.un.org/wpp/publications/files/wpp2019_highlights.pdf (accessed 6 Jul 2022).
McCarthy KJ, Blanc AK, Warren CE, et al. Women’s recall of maternal and newborn interventions received in the postnatal period: a validity study in Kenya and Swaziland. J Glob Health. 2018;8. https://doi.org/10.7189/jogh.08.010605.
Acknowledgements
Not Applicable.
Funding
The study did not receive any funding from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
SW, BJ, MRK, ANI, DY, JA, and MB conceived and designed the study. SW, DY, and MB conducted the data analysis. MRK, ANI, and JA interpreted the results for intellectual content and wrote the draft manuscript. SW, BJ, DY, and MB revised the draft manuscript. All authors read and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The current study analysed de-identified secondary data from the DHS. Therefore, no approval from an Institutional Review Board (IRB) was required. However, the DHS programme received ethical approval from both the Inner City Fund IRB and the IRB of the host nation. The surveys are conducted in accordance with the principles and ethics of health research involving human subjects. You can find the rules for protecting the privacy of survey respondents and household members in all DHS surveys 0n the DHS website (https://dhsprogram.com/Methodology/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm). We had access to the raw datasets used in the current study after obtaining written approval from the DHS program through the ICF.
Competing interests
The authors have not competing interests to declare.
Consent for publication
Not Applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional file 1:
Table S1
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wan, S., Jin, B., Kpordoxah, M.R. et al. A descriptive analysis of the coverage of newborn care services among women who delivered in health facilities in 17 sub-Saharan African countries. BMC Pregnancy Childbirth 23, 256 (2023). https://doi.org/10.1186/s12884-023-05592-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-05592-8