Abstract
Background
Pregnancy and early infancy are increased risk periods for severe adverse effects of respiratory infections. Aboriginal and/or Torres Strait Islander (respectfully referred to as First Nations) women and children in Australia bear a disproportionately higher burden of respiratory diseases compared to non-Indigenous women and infants. Influenza vaccines and whooping cough (pertussis) vaccines are recommended and free in every Australian pregnancy to combat these infections. We aimed to assess the equity of influenza and/or pertussis vaccination in pregnancy for three priority groups in Australia: First Nations women; women from culturally and linguistically diverse (CALD) backgrounds; and women living in remote areas or socio-economic disadvantage.
Methods
We conducted individual record linkage of Perinatal Data Collections with immunisation registers/databases between 2012 and 2017. Analysis included generalised linear mixed model, log-binomial regression with a random intercept for the unique maternal identifier to account for clustering, presented as prevalence ratios (PR) and 95% compatibility intervals (95%CI).
Results
There were 445,590 individual women in the final cohort. Compared with other Australian women (n = 322,848), First Nations women (n = 29,181) were less likely to have received both recommended antenatal vaccines (PR 0.69, 95% CI 0.67–0.71) whereas women from CALD backgrounds (n = 93,561) were more likely to have (PR 1.16, 95% CI 1.10–1.13). Women living in remote areas were less likely to have received both vaccines (PR 0.75, 95% CI 0.72–0.78), and women living in the highest areas of advantage were more likely to have received both vaccines (PR 1.44, 95% CI 1.40–1.48).
Conclusions
Compared to other groups, First Nations Australian families, those living in remote areas and/or families from lower socio-economic backgrounds did not receive recommended vaccinations during pregnancy that are the benchmark of equitable healthcare. Addressing these barriers must remain a core priority for Australian health care systems and vaccine providers. An extension of this cohort is necessary to reassess these study findings.
Similar content being viewed by others
Introduction
Pregnancy and early infancy are increased risk periods for severe adverse effects of respiratory infections [1, 2]. A decrease in immunity from physiological effects of pregnancy, [3] and age-associated immune immaturity in infants, exacerbated in infants born preterm, are among the reasons for these heightened infection risks [2]. Other risk factors include co-morbidities, living in remote regions, lower socio-economic status, inadequate housing, decreasing rates of exclusive breastfeeding, and limited access to culturally safe and appropriate, affordable health care [4]. To combat respiratory infections among these groups, inactivated influenza vaccines (IIV) and pertussis-antigen containing vaccines (dTpa) are recommended during pregnancy and provided free to all Australian women, [5] however data to inform the equity of antenatal vaccination coverage are scarce.
Internationally, antenatal IIV and dTpa vaccination studies have reported a lower uptake of both vaccines among their Indigenous populations compared to uptake in Asian/European ethnicities [6,7,8]. Aboriginal and/or Torres Strait Islander (herein respectfully referred to as “First Nations”) women and children in Australia bear a disproportionately high burden of respiratory diseases compared to non-Indigenous women and infants [9]. As such, First Nations women are a priority for antenatal vaccination. Several Australian studies incorporating First Nations women have suggested the coverage of IIV in pregnancy is low (range < 3–49%), however small samples sizes and biases [10,11,12,13] precluded reliable estimates of coverage. We previously reported lower and declining proportions of IIV and dTpa vaccination coverage among First Nations pregnant women compared to non-Indigenous pregnant women [14]. Also, although over 30% of Australian women are born overseas, [15] data describing antenatal IIV and dTpa vaccination coverage in women from culturally and linguistically diverse populations (CALD) are scarce. One Australian survey conducted over a three-month period examined IIV and dTpa vaccination coverage in pregnant women from CALD backgrounds in Victoria [16]. Although these results are important, the small sample size (n = 370) and restricted location preclude generalisable estimates of vaccine coverage in CALD women from other Australian jurisdictions and do not allow evaluation of temporal trends. A population-based study using data from Western Australia (WA) and New South Wales examined childhood vaccination coverage and showed pockets of lower vaccine coverage in children born from CALD mothers [17]. It is not known whether these pockets of low vaccine coverage extends to antenatal vaccination.
To our knowledge, no other Australian study has examined the influence of living in a remote area, or the level of socio-economic variation upon IIV and dTpa vaccine coverage in First Nations, non-Indigenous and non-CALD (hereafter referred to as ‘other Australian’), and CALD pregnant women.
The primary aim of this study was to provide robust estimates of antenatal IIV and/or dTpa vaccine coverage across three Australian jurisdictions over six years, among (1) women who identified as First Nations, who were from CALD backgrounds, or other Australians, and (2) among women from different levels of socio-economic advantage/disadvantage and remoteness of living. These data together are essential to indicate the equity of the Australian National Immunisation Program (NIP) and guide future antenatal vaccination policy.
Methods
Study design and population
Links2HealthierBubs (Links2HB) is a retrospective observational cohort study of mother-infants pairs [18]. The eligible cohort comprised mothers with a pregnancy ≥ 20 weeks gestation, between 01 Jan 2012-31 and Dec 2017 inclusive, in the Northern Territory (NT), Queensland (Qld), and WA. Collectively these jurisdictions encompass 5.92 million km2 of land, incorporating the largest geographic land mass and diverse climatic variations in Australia, [19] with ~ 95,000 births annually, (~ 32% of Australia’s total number of births) [20].
Inclusions/exclusions
Women were excluded from the study if: they recorded a birth before 20 weeks gestation; had missing data related to gestation at birth; or birthed outside the study period.
Data collection methods and sources
The cohort was created through the linkage of Perinatal Data Collections (PDCs) and immunisation registers and databases. These data sources are described in Supplementary box 1. A combination of deterministic and probabilistic record linkage was used to identify individual women and their pregnancies. Analysis of antenatal IIV coverage involved the whole study period (2012–2017) whereas dTpa was analysed from 2015 onwards following implementation of funded vaccination programs [21].
The key variables used to estimate vaccination coverage were; infant date of birth, gestation in weeks at the time of infant birth, gestation in weeks at the time of vaccination, and trimester of pregnancy in which maternal vaccination occurred. Vaccination in pregnancy (antenatal vaccination) was defined by documented receipt of an IIV and/or dTpa vaccine between the date of conception and the date of infant birth. Participants with no IIV and/or dTpa vaccination data during a pregnancy were considered ‘unvaccinated in pregnancy’.
First Nations status, ethnicity, socio-economic advantage and geographic variation
First Nations status was determined from identifiers located in PDCs and hospital admissions data. In WA, the data linkage branch also identifies Indigeneity through a validated algorithm implemented by the WA Department of Health, for any individual with at least one record in a government administrative dataset [22].
Ethnicity and mother’s country of birth variables recorded in the PDCs were used to categorise women from CALD backgrounds. Country of birth classifications were from Standard Australian Classification of Countries (SACC), 2016 Australian Bureau of Statistics [23]. A composite variable was created to classify women as (a) ‘First Nations’ if they identified as ‘Indigenous’ AND were classified as ‘Aboriginal and/or Torres Strait Islander’ in the ethnicity variable; (b) CALD if they did not identify as First Nations AND were not born in Australia AND were not classified as Caucasian in the ethnicity variable; and (c) ‘Other Australian’ if they were Australian born and did not identify as First Nations AND were classified as ‘Caucasian’ in the ethnicity variable (Supplementary box 2).
The Index of Relative Socio-economic Advantage and Disadvantage (IRSAD); derived from the Socio-Economic Indexes for Australia (SEIFA; Australian Bureau of Statistics 2016) index, [24] was used to define socio-economic advantage and disadvantage. The score includes measures of economic, educational and social domains and is ranked on a scale from 1 to 10, with one being the most disadvantaged and 9 and 10 being the most advantaged. The Accessibility Remoteness Index of Australia [25, 26] was used to identify remote and non-remote living participants, and hence their accessibility to health care services. Remote and very remote categories were combined to enhance statistical power. The mother’s recorded postcode of residence at the time of infant birth was used to establish their SEIFA and ARIA indexes.
Data analysis
The number of pregnancies, proportion of women who were administered antenatal vaccinations, and socio-economic and geographic characteristics were calculated for First Nations, Other Australian and CALD participants. A binomial generalized linear mixed model (GLMM) with a random intercept for the mother’s ID was used to account for clustering of participants who were in the cohort more than once over the study period. To determine the relative influence of (a) living remotely [25] and (b) socio-economic disadvantage (IRSAD/SEIFA) on antenatal IIV and dTpa vaccine coverage, we then calculated unadjusted prevalence risks (PR) and 95% compatibility intervals (95% CIs) [27]. All potential confounding variables statistically (5% significance level in univariable analysis) or speculatively associated with maternal vaccination coverage were then included in a multivariable GLMM and reported as adjusted prevalence ratios (aPR) with 95% CIs. Not living remotely and SEIFA 1 were used as the reference groups. All data analyses were conducted using Stata statistical software v.17.1 (StataCorp, College Station, Texas).
Missing data
Data for the main variables of interest ‘First Nations’ and ‘Ethnicity’ were > 99% complete. Denominators and accompanying proportions for other variables with missing data are presented in tables.
Ethics and governance
Multi-jurisdictional ethics committee approvals were gained from WA Department of Health (HREC 2016/56), Curtin University (HRE2017-0808), Menzies School of Health Research (HREC 2018–3199), Queensland Health and Royal Brisbane and Women’s Hospital (HREC/2018/QRBW/47,660), and WA Aboriginal Health Ethics Committees (HREC 889) [18].
Results
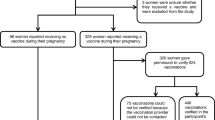
In the final Links2HB cohort (Fig. 1), there were 445,590 individual women out of 591,867 unique pregnancies; comprising 29,181 First Nations, 322,848 Other Australian and 93,561 women from CALD backgrounds.
Participant flow diagram of unique Links2HealthierBubs study participants by ethnicity and jurisdiction, Australia, 2012–2017
† Participants within the cohort more than once were identified
* Australian born women, who did not identify as First Nations and were classified as ‘Caucasian’ in the variable ‘Ethnicity’
Overall, 69,670 (16%) received an IIV during pregnancy, 125,023 (43%) received dTpa and 53,861 (18%) received both vaccines during pregnancy. Respective coverage of IIV among First Nations, Other Australian and CALD women was 14%,15% and 19%; for dTpa this was 31%, 44% and 43%; and for both vaccines, 13%, 18% and 21% (Supplementary Table 1). Compared to other Australians, First Nations women were less likely to have received any of the recommended vaccines during pregnancy: dTpa; PR 0.70, 95%CI 0.69–0.71) and both vaccines; PR 0.69, 95%CI 0.67–0.71, and women from CALD backgrounds were more likely to have received IIV (PR 1.24, 95%CI 1.22–1.25) and both vaccines (PR 1.16, 95%CI 1.10–1.13) seen in Table 2.
All potential confounding variables included in the GLMM analysis are shown in Table 2. Factors that positively predicted antenatal vaccine coverage for the overall cohort were; increasing maternal age at birth, birthing in a private hospital, parity, attending antenatal care during the first trimester, and increasing socio-economic advantage (SEIFA) (Table 2). Factors positively associated with vaccine coverage within the population groups were similar to those overall, apart from increasing maternal age among First Nations women (PR 0.82, 95%CI 0.71–0.93), and relative to the other jurisdictions, antenatal vaccine coverage in the NT was consistently lower (Supplementary Table 2).
Remoteness and socio-economic influence
Coverage of antenatal IIV was similar (13–19%) between population groups regardless of remoteness of living, however coverage of dTpa and both vaccines were 10–20% lower among First Nations women, particularly for those living remotely (Supplementary Fig. 1). This trend was consistent across each jurisdiction (Supplementary Fig. 2). Univariable and multivariable models confirmed statistically that overall, living remotely detracted from antenatal vaccination coverage: IIV PR 0.88 (95% CI 0.85–0.90); dTpa PR 0.75 (95% CI 0.73–0.76); and both vaccines PR 0.75 (95% CI 0.72–0.78) (Table 1). This trend remained consistent among all groups (Supplementary Table 2).
Antenatal vaccine coverage increased with socio-economic advantage. The highest proportions of vaccine coverage were in the SEIFA 10 decile compared to women from areas of highest disadvantage (SEIFA deciles 1 and 2) shown in Fig. 2.
This positive association was most notable for coverage of dTpa, and both IIV and dTpa vaccines among First Nations women in SEIFA 9 decile: IIV (PR 1.28, 95%CI 1.05–1.57); dTpa, (PR 1.33, 95%CI 1.20–1.47); and both IIV and dTpa; (PR 1.36, 95%CI 1.14–1.62). The trends were consistent across each group (Supplementary Table 2), and each jurisdiction (supplementary Fig. 3a-c).
Discussion
We identified overarching inequity in coverage of antenatal vaccinations among First Nations women, and in women who lived in remote areas, and women who lived in areas of higher socio-economic disadvantage. Other Australian women and CALD women living in major cities were more likely to have received the recommended and funded vaccines in pregnancy, and women from lower socio-economic backgrounds were less likely to have received vaccines. We also confirmed that younger women who birthed in public hospitals and who attended antenatal care later during pregnancy were less likely to have received antenatal vaccines. These geographic, social and financial access issues demonstrate shortcomings in our current health systems and NIP, and highlight the need for more dedicated resources and training to address the inequity.
As with other studies, we saw vaccination coverage improve over the years of the study, [28] particularly following the implementation of the antenatal dTpa program, but despite surveys indicating a high willingness of First Nations women to be vaccinated in pregnancy if offered, [10, 29] coverage of antenatal IIV and dTpa vaccination remained low. The gap between willingness and coverage is a potential physical and financial health systems access issue. Designing antenatal services specifically for younger mothers and promoting young parent programmes similar to some existing models may be one way to increase antenatal vaccination coverage among both younger and First Nations mothers [30]. Midwifery group practices co-designed with First Nations peoples for First Nations families, and antenatal care provided by First Nations health workers and midwives have demonstrated improved antenatal care attendance and equitable or better outcomes among First Nations mothers and infants compared to other Australians in mainstream care [31, 32]. However, this has not translated into practice for antenatal vaccination coverage in all jurisdictions as yet. Although our data relate to the years 2012–2017, data from a 2021 clinical audit within a major Qld public hospital showed both antenatal IIV and dTpa coverage remained considerably low among First Nations mothers (~ 17% for IIV and 26% for dTpa) compared to non-Indigenous mothers (39% for IIV and ~ 61% for dTpa) [33]. Other jurisdictions have also reported ongoing sub-optimal coverage of IIV after this time period (in 2017), with overall uptake ~ 48% in South Australia and Victoria, higher for dTpa (~ 79–83%), [34, 35] however, our data are the most comprehensive and contemporary for comparison thus far. An updated analysis of national data are warranted, particularly now that COVID-19 vaccination in pregnancy has been recommended since 2021 [36]. This recommendation may have influenced the priority of antenatal COVID-19 vaccination over antenatal IIV and dTpa administration during this time period, or pandemic restrictions may have affected access to antenatal IIV and dTpa.
Where First Nations or CALD focused midwifery models of care are not in place, more attention should be given to developing culturally safe clinical practice, and improving vaccine education and service delivery to avoid systemic barriers to equity such as racism and discrimination [37]. Strategies to increase antenatal vaccination coverage could include the use of appropriate language and interpreters in healthcare provider service settings.
Strengths and limitations
Our data include the largest linked cohort of First Nations mother-infant pairs across three Australian jurisdictions, and includes urban, rural and remote-living representation. The WA validated algorithm used to identify maternal First Nations status across multiple datasets strengthens the accuracy of these data. Our data are also the first to describe antenatal vaccination status by areas of accessibility to services and socio-economic advantage and disadvantage based on individual postcode level data. Our antenatal vaccination coverage results are consistent with international studies conducted during similar time periods, with similar Indigenous and ethnic population proportions [6,7,8]. These studies have also suggested that sub-optimal antenatal IIV and dTpa vaccination will persist if strategies to address ongoing inequity are not met.
Our data did not include First Nations status or ethnicity of infants. We acknowledge that including Indigeneity only of the mother underrepresents First Nations infants of First Nations fathers, and that the mother may choose to not identify as First Nations due to risks of receiving poorer care [37]. Our large sample size of First Nations mothers however, affords good generalisability for the three jurisdictions included in our study. We also acknowledge potential limitations around using the variables ‘country of birth’ and ‘ethnicity’ as an imperfect way of assessing English language capacity and health literacy. We also acknowledge potential unknown errors of vaccine reporting.
Conclusions
Our data demonstrated significant inequity in antenatal vaccination among First Nations Australian families, and families who live remotely and/or from lower socio-economic backgrounds. Given that the known increased risk factors for acquiring influenza or pertussis infections are living in remote regions, lower socio-economic status, inadequate housing, and limited access to culturally safe and appropriate, affordable health care, vaccination against these infections remains a key public health strategy in preventing severe disease in pregnancy and early infancy. Systematically monitoring vaccine coverage, and strategies that ensure vaccines are offered and provided to women equitably alongside other quality healthcare during pregnancy are required. This is a core responsibility of Australian health care systems and vaccine providers.
Data Availability
The datasets generated and/or analysed during the current study are not publicly available and are only made available to researchers through an application process. State and Territory Departments of Health and Data Custodians stipulate the non-sharing of these data, however analytic code used in this study can be made available upon request to the corresponding author.
Abbreviations
- IIV:
-
inactivated influenza vaccines
- dTpa:
-
diptheria-tetanus-acellular pertussis vaccine
- CALD:
-
culturally and linguistically diverse
- WA:
-
Western Australia
- NIP:
-
National Immunisation Program
- Links2HB:
-
Links2HealthierBubs
- NT:
-
Northern Territory
- Qld:
-
Queensland
- PDC:
-
Perinatal Data Collections
- IRSAD:
-
Index of Relative Socio-economic Advantage and Disadvantage
- SEIFA:
-
Socio-Economic Indexes for Australia
- ARIA:
-
Accessibility Remoteness Index of Australia
- GLMM:
-
generalized linear mixed model
- PR:
-
prevalence risk
- 95% CIs:
-
95% compatibility intervals
- aPR:
-
adjusted prevalence ratios
References
Wood N, Quinn H, McIntyre P, Elliott E. Pertussis in infants: preventing deaths and hospitalisations in the very young. J Paediatr Child Health. 2008;44(4):161–5.
Rasmussen SA, Jamieson DJ, Bresee JS, Englund JA, Uyeki TM. Effects of influenza on pregnant women and infants. Am J Obstet Gynecol. 2012;207(3 Suppl):3–8.
Memoli MJ, Harvey H, Morens DM, Taubenberger JK. Influenza in pregnancy. Influenza Other Respir Viruses. 2013;7(6):1033–9.
Kildea SV, Gao Y, Rolf M, Boyle J, Tracy S, Barclay LM. Risk factors for preterm, low birthweight and small for gestational age births among Aboriginal women from remote communities in Northern Australia. Women and Birth. 2017(16):30225–6.
Australian Government. Australian Technical Advisory Group on Immunisation (ATAGI) National Health and Medical Research Council. The Australian Immunisation Handbook: Department of Health and Ageing: Canberra, 10th ed, 2013.
Pointon L, Howe AS, Hobbs M, Paynter J, Gauld N, Turner N, et al. Evidence of suboptimal maternal vaccination coverage in pregnant New Zealand women and increasing inequity over time: a nationwide retrospective cohort study. Vaccine. 2022;40(14):2150–60.
Barber A, Halstead Muscoplat M, Fedorowicz A. Coverage with Tetanus, Diphtheria, and Acellular Pertussis Vaccine and Influenza Vaccine among pregnant women — Minnesota, March 2013–December 2014. MMWR Morb Mortal Wkly Rep. 2017;66(2):56–9.
Ding H, Black CL, Ball S, Donahue S, Fink RV, Williams WW, et al. Influenza vaccination coverage among pregnant women – United States, 2014-15 influenza season. MMWR Morb Mortal Wkly Rep. 2015;64(36):1000–5.
McHugh L, Andrews RM, Leckning B, Snelling T, Binks MJ. Baseline incidence of adverse birth outcomes, and infant influenza and pertussis hospitalisations prior to the introduction of influenza and pertussis vaccination in pregnancy: a data linkage study of 78,382 mother-infant pairs, Northern Territory, Australia, 1994–2015. Epidemiol Infect. 2019;147:e233. pp. 1–11.
O’Grady KF, Dunbar M, Medlin LG, Hall KK, Toombs M, Meiklejohn J et al. Uptake of influenza vaccination in pregnancy amongst Australian Aboriginal and Torres Strait Islander women: a mixed-methods pilot study.BMC. 2015;8(169):1–8.
Lotter K, Regan AK, Thomas T, Effler P, Mak DB. Antenatal influenza and pertussis vaccine uptake among Aboriginal mothers in western Australia. Aust N Z J Obstet Gynaecol. 2017;58(online):417–24.
Overton K, Webby R, Markey P, Krause V. Influenza and pertussis vaccination coverage in pregnant women in the Northern Territory in 2015 – new recommendations to be assessed. Darwin: The Northern Territory Disease Control Bulletin; 2016. pp. 1–8.
Krishnaswamy S, Thalpawila S, Halliday M, Wallace EM, Buttery J, Giles M. Uptake of maternal vaccinations by indigenous women in Central Australia. Aust N Z J Public Health. 2018;42(3):321.
McHugh L, Van Buynder P, Sarna M, Andrews RM, Moore HC, Binks MJ et al. Timing and temporal trends of influenza and pertussis vaccinations during pregnancy in three Australian jurisdictions: The Links2HealthierBubs populationbased linked cohort study, 2012–17.Aust N Z J Obstet Gynaecol. 2022;63(1):1–7.
Australian Bureau of Statistics. Census of Population and Housing: Reflecting Australia - Stories from the Census., 2016 Canberra; 2016.
Krishnaswamy S, Cheng AC, Wallace EM, Buttery J, Giles ML. Understanding the barriers to uptake of antenatal vaccination by women from culturally and linguistically diverse backgrounds: a cross-sectional study. Hum Vaccin Immunother. 2018;14(7):1591–8.
Abdi I, Gidding H, Leong RN, Moore HC, Seale H, Menzies R. Vaccine coverage in children born to migrant mothers in Australia: a population-based cohort study. Vaccine. 2021;39(6):984–93.
Sarna M, Andrews RM, Moore H, Binks MJ, McHugh L, Pereira GF et al. ‘Links2HealthierBubs’ cohort study: protocol for a record linkage study on the safety, uptake and effectiveness of influenza and pertussis vaccines among pregnant Australian women. BMJ Open. 2019;9(e030277):1–9.
Australian Government Geoscience Australia. National Location Information 2021 [Land areas of States and Territories]. Available from: https://www.ga.gov.au/scientific-topics/national-location-information/dimensions/area-of-australia-states-and-territories.
Australian Institute of Health and Welfare. Mothers and babies overview. Canberra: Department of Health; 2021.
Beard F. Pertussis immunisation in pregnancy: a summary of funded australian state and territory programs. Commun Dis Intell short Rep. 2015;39(3):E329–36.
Western Australian Government. Getting our stories right algorithm: Derived Aboriginal and Torres Strait Islander status flag. Department of Health. Data Linkage Branch Services; 2021.
Australian Bureau of Statistics. Standard australian classification of Countries. SACC) Canberra; 2016.
Australian Bureau of Statistics. Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2016. Available from: https://www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001.
Donahue JG, Kieke BA, King JP, DeStefano F, Mascola MA, Irving SA, et al. Association of spontaneous abortion with receipt of inactivated influenza vaccine containing H1N1pdm09 in 2010–11 and 2011–12. Vaccine. 2017;35(40):5314–22.
Australian Bureau of Statistics. Australian Standard Geographical Classification (ASGC) census 2011 [Remoteness Structure]. Available from: http://stat.abs.gov.au/itt/r.jsp?ABSMaps.
Gelman A, Greenland S. Are confidence intervals better termed “uncertainty intervals”? BMJ. 2019;366:l5381.
McHugh L, O’Grady KA, Nolan T, Richmond PC, Wood N, Marshall HS, et al. National predictors of influenza vaccine uptake in pregnancy: the FluMum prospective cohort study, Australia, 2012–2015. Aust NZ J Public Health. 2021;45(5):455–61.
Wiley KE, Massey PD, Cooper SC, Wood N, Quinn HE, Leask J. Pregnant women’s intention to take up a post-partum pertussis vaccine, and their willingness to take up the vaccine while pregnant: a cross sectional survey. Vaccine. 2013;31(37):3972–8.
Australian Institute of Health and Welfare. Maternity care in Australia: first national report on models of care, 2021. Australian Government. Canberra; 2021.
Kildea S, Gao Y, Hickey S, Nelson C, Kruske S, Carson A, et al. Effect of a birthing on Country service redesign on maternal and neonatal health outcomes for First Nations Australians: a prospective, non-randomised, interventional trial. The Lancet Global Health. 2021;9(5):E651–E9.
Ireland S, Lawurrpa Maypilama E, Roe Y, Lowell A, Kildea S. Caring for Mum on Country: exploring the transferability of the Birthing on Country RISE framework in a remote multilingual northern australian context. Women Birth. 2021;34(5):487–92.
Royal Brisbane and Women’s Hospital. Women’s and Newborn Services. Metro North Hospital and Health Service. Influenza and pertussis vaccination rates: OBSDATA; 2022.
Mohammed H, Clarke M, Koehler A, Watson M, Marshall HS. Factors associated with uptake of influenza and pertussis vaccines among pregnant women in South Australia. PLoS ONE. 2018;13(6):e0197867.
Moir D, Gunter K, Lynch L, Said SV. Antenatal vaccine uptake: a cross-sectional study investigating factors influencing women’s choices in pregnancy. Aust N Z J Obstet Gynaecol. 2020;60(5):729–37.
Australian Government. Pregnancy, breastfeeding and COVID-19 vaccines. Department of Health and Aged Care. Canberra; 2023.
Smylie J, W P-B. Truth, respect and recognition: addressing barriers to Indigenous maternity care. CMAJ. 2019;191(8):E207–E8.
PFIZER-BIONTECH COVID-19 VACCINE (BNT162, PF-07302048). Vaccines and related biological products advisory committee. Briefing document, 10 December 2020. Pages 1–92.
Australian Institute of Health and Welfare. 2010. Australia’s health 2010. The twelfth biennial health report of the Australian Institute of Health and Welfare. Canberra: AIHW; 2010.
Steinhoff MC, Katz J, Englund JA, Khatry SK, Shrestha L, Kuypers J, et al. Year-round influenza immunisation during pregnancy in Nepal: a phase 4, randomised, placebo-controlled trial. Lancet Infect Dis. Sep; 2017;17(9):981–9.
Acknowledgements
We would like to acknowledge Associate Investigator Heather D’Antoine for her guidance and governance for the First Nations data. In Queensland, we would like to thank the Linkages Services Branch at Queensland Health and Data Custodians for the Perinatal and Immunisation Data collections, and thank the Data Management team from the Royal Brisbane Women’s and Newborn Service for providing antenatal vaccination clinical audit data. In Western Australia, we would like to thank staff at the Linkage and Client Services Teams at the Data Linkage Branch, Department of Health Western Australia, as well as the Data Custodians for the Birth Registrations, Midwives Notification System, and WA Antenatal Vaccination Database. In the Northern Territory, we would like to thank Nicky O’Brien at SA-NT DataLink, Peter Markey, Heather Cook, and Vicki Krause at the NT Centre for Disease Control, and the Data Custodians for the NT Perinatal Trends and Immunisation Databases.
Funding
This project was supported by a National Health and Medical Research Council (NHMRC) Project Grant (GNT1141510) and operational funds provided by the Department of Health Western Australia. LMc was funded through a University of Queensland Early Career Research Fellowship. AKR was supported by an NHMRC Early Career Fellowship (GNT1138425). HCM was supported by a Stan Perron Charitable Foundation People Fellowship. CCB was supported by an NHMRC Career Development Fellowship (GNT1111596) and NHMRC Investigator award (APP1173163). MJB was supported by an NHMRC Early Career Fellowship (GNT1088733) and NHMRC funded Hot North - Improving Health Outcomes in the Tropical North – Fellowship (1131932). GP was supported with funding from NHMRC Project and Investigator Grants (GNT1099655 and GNT1173991), and the Research Council of Norway through its Centres of Excellence funding scheme (GNT262700).
Author information
Authors and Affiliations
Contributions
All authors have met the ICMJE criteria for authorship. All authors have read and approved the final manuscript. All authors contributed to all drafts of the manuscript. Other contributions involved: LMc was responsible for Qld ethics approvals and data acquisition, performed data cleaning and all data analyses, wrote the original and all draft manuscripts. AR provided expert content on immunisation in pregnancy and interpretation of findings for WA. MS conducted ethics approvals and data acquisition for WA, data cleaning and project management. HM provided expert content on immunisation in pregnancy and interpretation of findings for WA. PVB provided expert content on immunisation in pregnancy, government policy and recommendations. GP provided expert biostatistical analysis methods and interpretation of findings. CCB provided expert content on immunisation in pregnancy, government policy and recommendations. KL provided expert content on immunisation in pregnancy and clinical findings from an obstetric standpoint. RMA provided expert content on immunisation in pregnancy, government policy and recommendations, data analyses and interpretation of findings. KC and PM provided expert content on First Nations perspectives and data governance. MJB oversaw the project and provided expert content on immunisation in pregnancy, facilitated ethics approvals and data acquisition for the NT and interpretation of findings. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations, and protocols were approved by ethics committees. Due to the study design and sample size of this study, a waiver of informed consent was sought and granted by the following ethics committees: WA Department of Health (HREC 2016/56), Curtin University (HRE2017-0808), Menzies School of Health Research (HREC 2018–3199), Queensland Health and Royal Brisbane and Women’s Hospital (HREC/2018/QRBW/47660), and WA Aboriginal Health Ethics Committees (HREC 889). Overarching ethics approvals were gained from each of the abovenamed committees.
Consent for publication
Not applicable.
Competing interests
LMc, AKR, MS, PVB, GP, CCB, KL, RMA, KC, PM, MJB - no relevant disclosures. HCM- has received grants and honorarium from Merck Sharpe and Dohme for work not related to results presented in this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional file 1: Supplementary box 1.
Vaccination sources by jurisdiction and year
Additional file 2: Supplementary box 2.
Country of birth, Indigeneity and ethnicity of individual participants
Additional file 3: Supplementary Table 1.
Indigeneity, ethnicity, remoteness and socio-economic advantage on antenatal vaccine coverage in Links2HealthierBubs cohort, 2012-2017
Additional file 4: Supplementary Table 2.
Prevalence ratios of antenatal vaccine coverage among diverse population groups in the Links2HealthierBubs cohort, 2012-2017
Additional file 5: Supplementary figure 1.
Vaccination status in pregnancy by Indigenous status and remoteness
Additional file 6: Supplementary figure 2.
Vaccination status in pregnancy by Indigenous status and remoteness by jurisdiction
Additional file 7: Supplementary Figure 3. a
Antenatal vaccination by Indigenous status, ethnicity, and socio-economic variation in NT. b Antenatal vaccination by Indigenous status, ethnicity, and socio-economic variation in Qld. c Antenatal vaccination by Indigenous status, ethnicity, and socio-economic variation in WA
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
McHugh, L., Regan, A.K., Sarna, M. et al. Inequity of antenatal influenza and pertussis vaccine coverage in Australia: the Links2HealthierBubs record linkage cohort study, 2012–2017. BMC Pregnancy Childbirth 23, 314 (2023). https://doi.org/10.1186/s12884-023-05574-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-05574-w