Abstract
Background
The emerging postpartum rehabilitation (PPR) program in Chinese hospitals characterized by applying ongoing medical care through traditional cultural practices shows a protective effect in early puerperium in China. This study explores the benefit of PPR program practices to postpartum depression (PPD) and the influencing factors for PPD among Chinese women during the first postnatal six weeks.
Methods
The cross-sectional study included 403 participants and was conducted in a Secondary Municipal Hospital in Qingdao, China, from 01 to 2018 to 31 December 2021. Information on this PPR program was collected during the six-weeks postpartum consultation, including the Edinburgh postnatal depression scale (EPDS) scores, the measurement results for diastasis recti abdominis, and the international physical activity questionnaire (long form) (IPAQ-L) scores. Logistic regression models were used to examine the effect of the PPR program on PPD among the local population. The secondary aim of this study was to investigate possible influencing factors for PPD, such as coronavirus disease 2019 (COVID-19), physical exercises, etc.
Results
PPR program has shown a positive effect in preventing PPD (p < 0.001) and diastasis recti prevalence (p < 0.001) during the six-weeks postnatal control in Qingdao, China. Better post-pregnancy weight reduction (p = 0.04) and higher metabolic equivalent of task (MET) value (p < 0.001) were noticed in the non-PPR group. Furthermore, lower PPD risk was associated with factors such as longer relationship duration years (2–5 years) (p = 0.04) and exercising one to three times a week (p = 0.01). A higher PPD risk was related to factors such as urinary incontinence during the postpartum period (p = 0.04) and subjective insomnia (p < 0.001). No significant effect was shown between COVID-19 and the EPDS score in this study (p = 0.50).
Conclusion
Our results suggested that the PPR program provided protection against PPD and diastasis recti during the first six weeks after delivery. Urinary incontinence and subjective insomnia were the main risk factors for PPD, while longer relationship duration years and exercising one to three times a week gave protective effects to PPD. This study emphasized that a comprehensive ongoing medical care program, such as the PPR program, effectively improves women’s mental and physical health in the early postpartum in China.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
The Chinese traditional confinement ‘doing the month’ or ‘zuo yue zi’ [1, 2], refers to a number of cultural practices and health beliefs that influence some Chinese women and east Asian women. These practices include strict prescriptions and proscriptions, food taboos, the use of traditional herbs, avoiding outdoor activities, refraining from washing, etc. [1, 3]. According to some women who advocate these traditions, following these rituals is important for recovering and preventing future illness, regardless of whether these rituals are supported by scientific evidence or not [4]. Conceptually, the majority of Chinese women still adhere to these traditional beliefs and practices [4, 5].Furthermore, due to the quality of life improvements, more and more maternal care centers have emerged in the recent decade, mostly in first-tier cities in China [6]. These are professional maternal health care facilities operated by registered companies or hospitals for taking care of both mothers and their babies, enabling the practice of ‘doing the month’ to be carried out [7]. Women who decide to stay in such care centers pay more attention to their postpartum recovery quality [8]. Studies have shown that an extended postpartum hospital stay assists women to recuperate better, both physically and emotionally [9, 10]. In order to improve the quality of postnatal care for these mothers, medical professionals need to be more aware of how to modify the postpartum care to fit the unique culture of ‘doing the month’ [4].
Recently, a novel service model has been established in certain Chinese hospitals for individuals who want to adhere to the tradition of ‘doing the month’ while simultaneously receiving professional postpartum care [11]. Multi-disciplinary health professionals like family physicians, pediatricians, obstetricians, traditional Chinese medical doctors, nutritionists, midwifes, breastfeeding instructors, nurses, physical therapists, patient servicers, and other co-workers collaborated in this specially designed postpartum care program to provide comprehensive medical care to help both mothers and babies. Necessary physical therapies, routine ward rounding by physicians with different specialties, nursing cares, and other services such as various exercise classes are provided during the hospital stay (see supplementary file 1). The purpose of this postpartum rehabilitation program (PPR) is to manage the delivered women’s health in a more evidence-based manner during ‘doing the month’ period. However, little information is available in the literature to determine whether these maternal centers would benefit the health of women after delivery [8, 12]. Some studies have shown that a high-quality ‘doing the month’ experience positively impacted maternal parenting quality [4, 13,15,16,16] and exercises can be effective in reducing the symptoms of postpartum depression [14, 17], while some restrictions of ‘doing the month’ practices might negatively impact the mental health of postpartum women [18, 19]. We hypothesized that women who joined such PPR program would have a lower postpartum depression (PPD) risk on week six after delivery. The main aim of this study was to examine the effect of the new PPR program to PPD among the local Chinese women. Additionally, limited studies have shown a negative effect of the coronavirus disease 2019 (COVID-19) to PPD [20, 21] and a beneficial effect from undertaking physical activities during the puerperium [22]. A secondary aim of this study was to investigate whether the PPD risk correlates with COVID-19, physical exercises, and other complications.
Methods
Study design and sample
This cross-sectional study was conducted at United Family Hospital (UFH) in Qingdao, China using consecutive sampling, between December 2018 and December 2021. The researchers consecutively invited all patients who attended their six-week postpartum follow-up consultations at Qingdao UFH on a fix pre-scheduled workday every week to participate in the study. After obtaining written informed consent, the participant was asked to complete questionnaires with the assistance of the interviewer. The inclusion criteria for the participants were as follows: (1) patients aged 18 and older (2) Ambulatory outpatients who were able to visit the clinic unassisted (3) Patients coming for their six-week postpartum visit (4) Patients from whom written informed consent was obtained (5) Patients were prepared to complete a self-reported complications questionnaire and receive predefined physical examinations (6) Ability to understand Chinese or English language. Women with a history of mental health disorders, chronic pain, severe diseases that make it difficult to come for the additional ambulatory follow up visits, severe pregnancy complications (preeclampsia/eclampsia, placenta previa, placental abruption, major birth defects, low birth weight (< 1500 gram [23]), still birth, handicap, and women who do not understand Chinese or English were excluded. All participants were guided by trained researchers to complete the questionnaires after a planned consultation in the obstetric department. The power calculation was conducted using online open software OpenEpi [24]. Our sample size was calculated based on the mean and standard deviation of the EPDS score as reported in a previous study as well as the estimates obtained in our pretest stage [25]. The estimated sample size was 129 subjects in each group (total 258 participants), with 80% power and 95% confidence interval.
As the trained researchers were full-time medical staff members who volunteered their spare time to assist with this study, and as a result of covid regulations, we attempted to collect the participants’ information on a set workday during the week. Additional survey questions concerning postpartum practices, demographic status, and complications were reviewed by experts and pretested prior to being collected.
Data collection
Participants were recruited from 01 to 2018 to 31 December 2021 during their six-week postpartum checkup in the Qingdao UFH PPR center by using consecutive sampling method. Participants were introduced to a research doctor after getting their verbal permission when their planned routine check-up appointment was complete. After introduction to the trained co-worker, an information sheet and written informed consent form were given to the patient. After the participant signed the informed consent, interviews, physical examinations, and questionnaires were completed through a face-to-face interview with the patient by trained researcher in a physically separated room. Specifically, the patient completed demographic information, a post-partum depression questionnaire, a physical activity questionnaire and was examined for diastasis recti. Participants were divided into two groups based on whether they have ever participated in the PPR program during their first month following delivery. It is intended that the information of this study was not shared with participants at the moment of delivery, so that they could make their own decision regarding whether to enroll in the PPR program or not. The final outcomes (results of the questionnaires and patient’s personal information data) were not shared with the treating physician or any other medical staff in the hospital. The signed consent form and patient’s identification information were both kept confidentially by the main researcher (ZXQ) with one hard copy to ensure the patient’s privacy.
Socio-demographic and clinical measures
Participants were asked to provide their age, height, delivery method, educational level, family income, marital or relationship duration, occupation status, newborn gender, the expectation of the newborn gender, parity numbers, and information regarding planned or unplanned pregnancy.
Assessment of postpartum depression symptoms
Postpartum depression was measured with the validated Chinese version of the Edinburgh postnatal depression scale (EPDS) [27,28,28], aimed to indicate increasing symptoms, explored mood, pleasure, guilt, anxiety, fear, ability to cope, insomnia, sadness, and self-injury [29]. Each question on the EPDS is graded on a 4-point scale (range 0–3), resulting in a total score that ranges from 0 to 30, with scores of 10 or more suggesting potential PPD. The cutoff 9/10 was chosen instead of the threshold 12/13 in English version [28, 30] to achieve a better sensitivity [26].
Assessment of physical exercises
The physical activity was measured through a validated Chinese version of the International Physical Activity Questionnaire (long form) (IPAQ-L) [32,33,33], and the data from the questionnaire were transformed into energy expenditure estimates as metabolic equivalents (METs) in hours per week of activity. The method to calculate “minutes per week” is shown in the formula as shown below (Table 1). The total physical activity of postpartum women was categorized as low (< 600 MET·min·wk-1), moderate (600 ~ 3000 MET·min·wk-1), or high (> 3000 MET·min·wk-1) physical activity [34], corresponding to less than 150 min per week, 150 ~ 750 min per week, or more than 750 min per week of moderate physical activity. This self-administered, long form of IPAQ contains four domains of physical activity: work-related, transportation, housework or gardening and leisure-time activity. The questionnaire also includes data about time spent sitting as an indicator of sedentary behavior.
Assessment of diastasis recti
Diastasis recti abdominis (DRA) is a medical condition in which the rectus abdominis muscles are separated by an abnormal distance without any fascia defect [35]. DRA could be measured by palpating 4.5 cm above, at, and 4.5 cm below the umbilicus in a standardized supine crook-lying position with both arms crossed over the chest [36]. Patients were asked to perform an abdominal crunch till the shoulder blades were off the bench. DRA will be categorized into five categories as non-DRA (separation < 2 fingerbreadths), mild DRA (from 2 fingerbreadths to less than 3 fingerbreadths), moderate DRA (from 3 fingerbreadths to less than 4 fingerbreadths) and severe DRA ( ≧ 4 fingerbreadths). Observed protrusion along the linea alba was categorized as DRA With Protrusion, even if the palpated distance was less than 2 fingerbreadths [36].
Statistical analysis
The data analyses were conducted with the Statistical Package for the Social Science (SPSS for Windows 14.0, SPSS Inc., Chicago, IL). Potential confounders including socio-demographic variables, primary caregivers, exercise times per week, complications during the postpartum period, etc. were reported (Table 2). In addition, we adjusted for parity, expected gender of the newborn baby, and feeding mode to evaluate the influence of these factors. EPDS values, IPAQ data and diastasis recti value were recorded as means with standard deviations. Univariate analysis followed by a multivariate logistic regression analysis were used to calculate the odds ratio (ORs) for different risk factors. Final significance was set at P < 0.05 and Ors with the 95% confidence intervals (95% CI) were considered significant. There was no missing data.
Ethical approval
The procedures were approved by the Qingdao Affiliated University of Qingdao [37], Qingdao United Family hospital, and agreed by the Medical Ethical Board of the KU Leuven (S62625). All participants completed the written informed consent before the study after verbal briefing by the researcher.
Main findings
Participants
As previously mentioned, participants were assessed on a fixed pre-scheduled workday of the week, due to availability of the researcher and COVID regulations. From December 2018 to December 2021, 410 women were invited to participate in this study. A total of 403 valid questionnaires were collected with an effective participation rate of 98.3% (Seven refusals). The non-PPR group consisted of 146 participants while the PPR group consisted of 257 participants. All of the including participants signed the consent forms and completed the questionnaires fully. The age range was between 20 to 45-year-old. There were no significant differences in the socio-demographic and obstetric characteristics between the PPR and non-PPR groups (Table 2).
Main findings
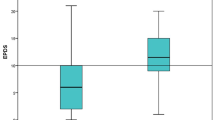
PPR and postpartum depression
Patients who participated in the PPR program had a lower EPDS score (p < 0.001) using logistic regression (Table 3). In total, 66 (16.4%) women were scored as high risk for PPD (≥ 10) on the EPDS, with 35 in non-PPR group and 31 in PPR group. The non-PPR group had a clearly higher average EPDS score than the PPR group (6.25 vs. 4.64, ORu = 2.30, 95% CI = 1.35–3.92) (ORu = univariate odds ratios).
PPR and diastasis recti
A better diastasis recti recovery rate (ORu = 2.91, 95% CI = 1.10–7.68) was also found in the PPR group (Table 3).
PPR and physical exercise
The MET value was significantly higher in the non PPR group, shown in both univariate and multivariate regression models (Table 3).
PPR and other postnatal complications
None of the eight specified complications (urinary incontinence / wound / breasts / pain / sleep / constipation / hemorrhoids / pelvic organ prolapse problems) showed any difference between the two groups (Table 3).
Although a greater post-pregnancy weight reduction was noticed in the non-PPR group on univariate regression analysis, this result was not significant in the multivariate regression model (Table 3).
Other influencing factors for PPD
In addition to the PPR program we analyzed the data for associations between other factors and PPD. The new coronavirus COVID-19 was transmitted between human beings in China since January 2020. This has declared the outbreak as a pandemic in March 2020 (WHO) [38]. Univariate logistic regression analysis was conducted to evaluate factors, such as the COVID-19, physical exercises, and other complications on the postpartum depression risk. No significant correlation was shown in this study between the COVID-19, the MET value itself, and the diastasis recti prevalence rate with the PPD risk. A lower PPD risk was associated with exercising one to three times a week (p = 0.01, ORu = 0.37, 95% CI = 0.17–0.79), and longer marriage or relationship duration years (2–5 years) (p = 0.04, ORu = 0.51, 95% CI = 0.26–0.96) (Table 4). Meanwhile, a higher PPD risk was associated with urinary incontinence during postpartum period (p = 0.04, ORu = 2.33, 95% CI = 1.06–5.14) and subjective insomnia (p < 0.001, ORu = 3.13, 95% CI = 1.77–5.52), but not related with the total sleeping time (Table 4).
Discussion
Main results
The findings of our study provide evidence of a positive impact of a hospital-based postpartum rehabilitation (PPR) program on postpartum depression in the first 6 weeks following delivery.
The proportion of women with a high risk of PPD (EPDS score of ≥ 10) was 12.0% in the PPR group compared with 23.9% in the non-PPR group (p < 0.001). As can be seen in other studies, good environmental factors such as healthier lifestyle-related factors, appropriate social support, and better interpersonal relationships are associated with better postpartum mental health [39, 40]. Interestingly, the PPR program also had a significant positive effect on the reduction of the prevalence of diastasis recti. This is likely due to the fact that the PPR group received extra individual specified physical trainings during the first four weeks after delivery, led by experienced physical therapists. This finding is consistent with previous studies that specified post-partum physical exercises may be effective for reducing the prevalence of diastasis recti [41, 42].
PPR and physical exercise
This study found that both the dose of physical activity (MET value) and the post-pregnancy weight reduction over the six weeks were higher in the non-PPR group. Although the PPR group received extra sport exercises during their month-long stay, other social activities were very limited due to the fact that they were served with daily foods, nanny services and received medical attention on site. The need for outdoor activities therefore became unnecessary for these people. The non-PPR group had more opportunities for outdoor activities, such as buying life supplies and maintaining social contacts. This may explain why the PPR women had fewer daily activities compared with the non-PPR group after discharge. Focusing on encouraging a sport habit rather than giving passive sport lessons during the first month may be more beneficial for new mothers’ weight management and PPD risk control in the future.
Additional influencing factors for postpartum depression
COVID-19
Contrary to other research, although the outdoor activities were very limited to the new mothers, the prevalence of PPD was not significantly higher during the COVID-19 period in this study. We consider the following reasons to explain this phenomenon in our study: First, parents / parents-in-law may use their own experiences and parenting methods to influence the new mothers and the babies in China. When the ideas of parenting are different from both parties, it may cause family conflicts, frustrations, and negative emotions to new mothers [43]. During the COVID period, parents visiting was very limited and even forbidden. This would give the new fathers more chance to take care of the babies and strengthen the relationship between husbands and wives. Secondly, China’s “dynamic zero-COVID” policy has resulted in very few positive cases being reported in Qingdao in the past two years compared to other countries [44, 45]. The negative influence on psychological health by lockdown restrictions during the COVID-19 epidemic to the local residents was not significantly related with the PPD risk in this study.
Physical exercise
In this research endeavour, an investigation was conducted to analyze the relationship between the dose and frequency of physical activity and PPD. Our results indicate that engaging in physical activity one to three times per week was associated with a decreased risk of PPD. However, we found no discernible correlation between PPD and the dose of physical activity, as measured by MET value. Overall, our study findings provide support for the theory that physical activity during the postpartum period could potentially diminish the prevalence of PPD. This outcome may be attributed to the emotional impact of exercise, which can enhance self-confidence and alleviate negative thoughts [46]. Other studies have also illustrated the positive impact of physical activity on the risk of PPD [15]. Further exploration, particularly through subgroup analysis, would be beneficial in determining whether the effects were a consequence of specific dose or frequency levels of physical activity.
Other complications
Relationship duration
The study showed a lower risk of PPD when the marriage or relationship duration of the couples was between 2 and 5 years. These findings indicated that having a baby very shortly (< 2 years) after marriage was a potential risk factor for PPD. This phenomenon might be related with the Chinese social system, which didn’t benefit new mothers for their career promotion path. Having a baby shortly after marriage might create more challenges to the new mother, including complicated family members’ relationships and different socioeconomic status. On the other hand, the risk of PPD increased when the marriage or relationship duration was more than 5 years. Marital satisfaction has strong negative correlation with the prevalence of PPD, which in turn was generally negatively predicted by the duration of marriage [37, 47, 48]. This risk factor for PPD should be studied in the future to improve the mothers’ mental health.
Subjective insomnia
An interesting finding in this study was that the average amount of sleeping hours was not related to PPD, but a subjective experience of insomnia does. While women with an increased risk for PPD may sleep the same number of hours as other delivered mothers, they may feel as if they are not getting enough sleep. The expectation of getting a certain number of sleeping hours or the subjective feeling of sleeplessness may be related with PPD. Breastfeeding mothers need to breastfeed the babies every two to four hours during the first few months causing an interrupted night’s rest. The extra stress created by an interrupted sleep pattern can negatively affect the patient’s mood. How the new mothers cope with this stress might affect their mental state rather than the absolute sleeping hours. More studies on how this experience of insomnia affect the PPD would be useful in the future.
Urinary incontinence
We also found that urinary incontinence had a significant correlation with the PPD. One of the reasons might be that this complication was often perceived as a stigma in traditional Chinese culture. This negative attitudes towards urinary incontinence inhibits patients from seeking care. Additional attention should be spent on these complications by medical staff, actively asking and checking the patient in a comfortable and private environment.
Strength and limitations
This study has investigated the advantage of a pre-existing PPR program in Qingdao, China. It delivered additional information about the risk factors of PPD, partly during the COVID-19 pandemic. The strength of this study is the direct comparison of two groups in a real-world setting. However, several limitations should be considered. First of all, an intervention study comparing two or more randomized comparison groups is more suited to determine the causal relationship than the cross-sectional study design. Yet, such design would not be possible against the background of Chinese customs. Second, our study group was only collected in a secondary municipal hospital in an urban area. This study was conducted in Qingdao, the second biggest city of Shandong province. Our population has a significant higher family income than the average income of other communities. Finally, this study is not double-blinded that the researchers knew the group information of the participants prior to the interviews.
Implications for practice and future research
Our PPR program has more medical input than most PPR programs in China. It would be interesting to investigate other new existing postpartum care programs’ clinical efficacy, including cost-benefit, cost-effectiveness, and cost-utility analysis.
We found associations between duration of the relationship or marriage, urinary incontinence and the feeling of sleeplessness and PPD. These should all be studied further. We also found that despite the patient receiving exercise interventions during the “month”, that this pattern of behavior did not carry through beyond the month. Given the known beneficial effect of exercise [49, 50] this area would benefit from further study.
Finally, we did not see any significant association of the COVID-19 pandemic and PPD. This was different from other studies, possibly due to other factors, such as the environment [21, 51, 52]. Future studies may explore such relationships.
Conclusion
This study has shown a strong association between the PPR program and a reduction in prevalence of PPD symptoms and diastasis recti during the first six weeks after delivery. Urinary incontinence and subjective insomnia were the main risk factors for PPD, while relationship duration between 2 and 5 years and exercising one to three times a week gave protective effects to PPD. Based on the findings of this study, it is evident that a comprehensive program of ongoing care, specifically the PPR program, is crucial for promoting the physical and mental well-being of women during the early postpartum period in China. These results carry significant policy implications for the development and organization of postpartum care services in the country.
Availability of data and materials
The authors are happy to share anonymized data related to this paper upon receiving a specific request, along with the purpose of that request. Interested parties may contact 2187zhang@gmail.com.
Abbreviations
- PPR:
-
Postpartum rehabilitation
- PPD:
-
Postpartum depression
- COVID-19:
-
coronavirus disease 2019
- EPDS:
-
Edinburgh Postnatal Depression Scale
- UFH:
-
United Family Hospital
- IPAQ-L:
-
International Physical Activity Questionnaire – Long Form
- DRA:
-
Diastasis Recti Abdominis
- WHO:
-
World health organization
- MET:
-
Metabolic equivalent of task
- 95% CIs:
-
95% confidence intervals
- SD:
-
Standard deviation
- ORs:
-
Odds ratios
References
Pillsbury BL. “Doing the month”: confinement and convalescence of chinese women after childbirth. Social Sci Med Part B: Med Anthropol. 1978;12:11–22.
Callister LC. Doing the month: chinese postpartum practices. MCN Am. J. Matern. Child Nurs. 2006;31(6):390.
Liu YQ, Petrini M, Maloni JA. “Doing the month”: P ostpartum practices in C hinese women. Nurs Health Sci. 2015;17(1):5–14.
Zheng X, Watts K, Morrell J. “Chinese primiparous women’s experience of the traditional postnatal practice of “doing the month”: a descriptive method study. Japan J Nurs Sci. 2019;16(3):253–62.
Holroyd E, Twinn S, Yim IW. Exploring chinese women’s cultural beliefs and behaviours regarding the practice of “doing the month”. Women Health. 2005;40(3):109–23.
Yan Z. The consumption narratives of postpartum care centers: female body construction from “inter-generational emotional exchange” to “economic consumption identity”. Chinese Youth Studies. 2018;7:13–18.
Dai WY. (2019). Reforming “zuoyuezi”: wrestling among tradition, science and Market. Journal of Guangxi University for Nationalities (Philosophy and Social Science Edition). 41(5):93–100.
Yeh Y-C, John WS, Venturato L. Inside a postpartum nursing center: tradition and change. Asian Nurs Res. 2016;10(2):94–9.
Martin A, et al. Views of women and clinicians on postpartum preparation and recovery. Matern Child Health J. 2014;18(3):707–13.
Kanotra S et al. Challenges faced by new mothers in the early postpartum period: an analysis of comment data from the 2000 Pregnancy Risk Assessment Monitoring System (PRAMS) survey Matern Child Health J. 2007;11(6):549–58
Tao F, et al. Low postnatal care rates in two rural counties in Anhui Province, China: perceptions of key stakeholders. Midwifery. 2011;27(5):707–15.
Yeh YC, St John W, Venturato L. Doing the month in a T aiwanese postpartum nursing center: an ethnographic study. Nurs Health Sci. 2014;16(3):343–51.
Gao Ll, et al. Experiences of postpartum depression among first-time mothers in mainland China. J Adv Nurs. 2010;66(2):303–12.
Poyatos-León R, et al. Effects of exercise‐based interventions on postpartum depression: a meta‐analysis of randomized controlled trials. Birth. 2017;44(3):200–8.
Özkan SA, et al. The effectiveness of an exercise intervention in reducing the severity of postpartum depression: a randomized controlled trial. Perspect Psychiatr Care. 2020;56(4):844–50.
Eustis EH, et al. Innovations in the treatment of perinatal depression: the role of yoga and physical activity interventions during pregnancy and postpartum. Curr Psychiatry Rep. 2019;21:1–9.
Pritchett RV, Daley AJ, Jolly K. Does aerobic exercise reduce postpartum depressive symptoms? A systematic review and meta-analysis. Br J Gen Pract. 2017;67(663):e684–91.
Ho M, et al. The association between behavior restrictions in doing-the-month practice and mental health status among postpartum women. J Altern Complement Med. 2015;21(11):725–31.
Ding G, et al. Doing the month” and postpartum depression among chinese women: a Shanghai prospective cohort study. Women Birth. 2020;33(2):e151–8.
Layton H, et al. Depression, anxiety, and mother-infant bonding in women seeking treatment for postpartum depression before and during the COVID-19 pandemic. J Clin Psychiatry. 2021;82(4):35146.
Mariño-Narvaez C, et al. Giving birth during the COVID‐19 pandemic: the impact on birth satisfaction and postpartum depression. Int J Gynecol Obstet. 2021;153(1):83–8.
Kołomańska-Bogucka D, Mazur-Bialy AI. Physical activity and the occurrence of postnatal depression—a systematic review. Medicina. 2019;55(9):560.
Xie R-h, et al. Fetal gender and postpartum depression in a cohort of chinese women. Soc Sci Med. 2007;65(4):680–4.
Sullivan KM, Dean A, Soe MM. On academics: OpenEpi: a web-based epidemiologic and statistical calculator for public health. Public Health Rep. 2009;124(3):471–474.
Wan EY, et al. Postpartum depression and traditional postpartum care in China: role of zuoyuezi. Int J Gynecol Obstet. 2009;104(3):209–13.
Wang Y, et al. Psychometric evaluation of the mainland chinese version of the Edinburgh postnatal depression scale. Int J Nurs Stud. 2009;46(6):813–23.
Heh SS. Validation of the Chinese version of the Edinburgh Postnatal Depression Scale: detecting postnatal depression in Taiwanese women. Hu Li Yan Jiu. 2001;9(2):105–13.
Lee DT, et al. Detecting postnatal depression in chinese women: validation of the chinese version of the Edinburgh postnatal depression scale. Br J Psychiatry. 1998;172(5):433–7.
Guo P, et al. Adherence to traditional Chinese postpartum practices and postpartum depression: a cross-sectional study in Hunan, China. Front Psychiatry. 2021;12:649972.
Ding G, et al. Therapeutic effects of the traditional “doing the month” practices on postpartum depression in China. Am J Psychiatry. 2018;175(11):1071–2.
Qu N, Li K. Study on the reliability and validity of international physical activity questionnaire (Chinese Vision, IPAQ) Zhonghua liuxingbingxue zazhi, 2004; 25(3):265–268.
Jia Y-J, et al. Reliability and validity regarding the chinese version of the International Physical Activity Questionnaires (long self-administrated format) on women in Chengdu, China Zhonghua liuxingbingxue zazhi, 2008;29(11):1078–82.
Deng HB, et al. Reliability and validity of the IPAQ-Chinese: the Guangzhou Biobank Cohort study. Med Sci Sports Exerc. 2008;40(2):303–7.
Lear SA, et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study The Lancet, 2017; 390(10113):2643–2654.
Reinpold W, et al. Classification of rectus diastasis—a proposal by the German Hernia Society (DHG) and the International Endohernia Society (IEHS). Front Surg. 2019;6:1.
Sperstad JB, et al. Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med. 2016;50(17):1092–6.
Odinka JI, Nwoke M, Chukwuorji JBC, et al. Post-partum depression, anxiety and marital satisfaction: A perspective from Southeastern Nigeria. S Afr J Psychiat. 2018;24:a1109. https://doi.org/10.4102/sajpsychiatry.v24i0.1109
Organization WH. Timeline-COVID-19: Available at: https://www.who.int/news/item/29-06-2020-covidtimeline 2021, Accessed
Ghaedrahmati M, et al. Postpartum depression risk factors: A narrative review. J Educ Health Promot. 2017;6:60.
Hutchens BF, Kearney J. Risk factors for postpartum depression: an umbrella review. J Midwifery Women’s Health. 2020;65(1):96–108.
Berg-Poppe P, et al. Use of Exercise in the management of Postpartum Diastasis Recti: a systematic review. J Women’s Health Phys Therapy. 2022;46(1):35–47.
Laframboise FC, Schlaff RA, Baruth M. Postpartum exercise intervention targeting diastasis recti abdominis. Int J Exerc Sci. 2021;14(3):400.
Guan Z, et al. Postpartum depression and family function in chinese women within 1 year after childbirth: a cross-sectional study. Res Nurs Health. 2021;44(4):633–42.
Chen J-M, Chen Y-Q. China can prepare to end its zero-COVID policy. Nat Med. 2022;28(6):1104–5.
Steele MK, et al. Estimated number of COVID-19 infections, hospitalizations, and deaths prevented among vaccinated persons in the US, December 2020 to September 2021. JAMA Netw Open. 2022;5(7):e2220385–5.
Knapen J, et al. Exercise therapy improves both mental and physical health in patients with major depression. Disabil Rehabil. 2015;37(16):1490–5.
Sorokowski P, et al. Marital satisfaction, sex, age, marriage duration, religion, number of children, economic status, education, and collectivistic values: data from 33 countries. Front Psychol. 2017;8:1199.
Wendorf CA, et al. Marital satisfaction across three cultures: does the number of children have an impact after accounting for other marital demographics? J Cross-Cult Psychol. 2011;42(3):340–54.
DiPietro L, et al. Benefits of physical activity during pregnancy and postpartum: an umbrella review. Med Sci Sports Exerc. 2019;51(6):1292.
Larson-Meyer DE. Effect of postpartum exercise on mothers and their offspring: a review of the literature. Obes Res. 2002;10(8):841–53.
Zanardo V, et al. COVID-19 pandemic: impact on gestational diabetes mellitus prevalence. Diabetes Res Clin Pract. 2022;183:109149.
Zhang CX, et al. Evaluating depression and anxiety throughout pregnancy and after birth: impact of the COVID-19 pandemic. Am J Obstet Gynecol MFM. 2022;4(3):100605.
Acknowledgements
The authors would like to thank the participants who spent their extra time in the study. The authors are also grateful to the staffs of the Qingdao United Family Hospital, Qingdao, China.
Funding
This study was conducted with no specific funding support.
Author information
Authors and Affiliations
Contributions
XQ.Z, C.M designed the review, XQ.Z and XL.Z contributed to the conception and design of the study, data acquisition, and analysis and interpretation of data. XQ.Z participated in writing the first draft of the paper. M.V, B.A, T.L, M.A, and F.B revised critically for important intellectual content and gave final approval of the version to be published. All authors contributed to the intellectual content, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was carried out in accordance with the Declaration of Helsinki. All procedures were approved separately by the affiliated hospital of medical college Qingdao University (QYFY WZ 2018-12-02) and university hospital of KU Leuven (S62625). All participants provided written informed consent prior to participation, and it was clearly explained to all participants that they were free to withdraw from any part of the study at any point in time.
Consent for publication
Not applicable.
Competing Interest
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
† Catharina Matheï started as the main supervisor of this work, but passed away on 13th August 2021 before being able to finalize the work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional file 1: Supplementary File 1.
Services for postpartum women during ‘doing the month’ period in different settings in Qingdao
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, X., Zuo, X., Matheï, C. et al. Impact of a postpartum care rehabilitation program to prevent postpartum depression at a secondary municipal hospital in Qingdao China: a cross-sectional study. BMC Pregnancy Childbirth 23, 239 (2023). https://doi.org/10.1186/s12884-023-05547-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-05547-z