Background
About 1.3 million pregnant women lived with HIV and were eligible to receive antiretroviral therapy (ART) worldwide in 2021. The World Health Organization recommends protease inhibitors (PI)-based regimen as second or third-line during pregnancy. With remaining pregnant women exposed to PIs, there is still an interest to assess whether this treatment affects perinatal outcomes. Adverse perinatal outcomes after prenatal exposure to PI-based ART remain conflicting: some studies report an increased risk of preterm birth (PTB) and low-birth-weight (LBW), while others do not find these results. We assessed adverse perinatal outcomes associated with prenatal exposure to PI-based compared with non-nucleoside reverse transcriptase (NNRTI)-based ART.
Methods
We performed a systematic review searching PubMed, Reprotox, Clinical Trial Registry (clinicaltrials.gov) and abstracts of HIV conferences between 01/01/2002 and 29/10/2021. We used Oxford and Newcastle-Ottawa scales to assess the methodological quality. Studied perinatal outcomes were spontaneous abortion, stillbirth, congenital abnormalities, PTB (< 37 weeks of gestation), very preterm birth (VPTB, < 32 weeks of gestation), LBW (< 2500 grs), very low-birth-weight (VLBW, < 1500 g), small for gestational age (SGA) and very small for gestational age (VSGA). The association between prenatal exposure to PI-based compared to NNRTI-based ART was measured for each adverse perinatal outcome using random-effect meta-analysis to estimate pooled relative risks (RR) and their corresponding 95% confidence intervals (CI). Pre-specified analyses were stratified according to country income and study quality assessment, and summarized when homogeneous.
Results
Out of the 49,171 citations identified, our systematic review included 32 published studies, assessing 45,427 pregnant women. There was no significant association between prenatal exposure to PIs compared to NNRTIs for VPTB, LBW, SGA, stillbirth, and congenital abnormalities. However, it was inconclusive for PTB, and PI-based ART is significantly associated with an increased risk of VSGA (sRR 1.41 [1.08-1.84]; I2 = 0%) compared to NNRTIs.
Conclusions
We did not report any significant association between prenatal exposure to PIs vs NNRTIs-based regimens for most of the adverse perinatal outcomes, except for VSGA significantly increased (+ 41%). The evaluation of antiretroviral exposure on pregnancy outcomes remains crucial to fully assess the benefice-risk balance, when prescribing ART in women of reproductive potential with HIV.
PROSPERO number
CRD42022306896.
Similar content being viewed by others
Background
In 2021, 38 million people lived with HIV worldwide, of whom 1.3 million were pregnant women, and mostly in sub-Saharan Africa [1]. Maternal HIV infection among antiretroviral drug-naïve women is associated with a significantly increased risk of adverse perinatal outcomes, such as prematurity, low-birth-weight, small for gestational age and stillbirth [2]. Antiretroviral therapy (ART) during pregnancy has demonstrated a clear benefit for maternal health, and prevent the risk of HIV mother-to-child-transmission (MTCT) [3]. Since 2015, ART initiation is recommended in all people living with HIV, including pregnant women [4]. As a result, in 2021, 1.05 million pregnant women had access to antiretroviral drug regimen for their own health and prevention of MTCT (PMTCT), with 90% living in sub-Saharan Africa [1, 5]. In 2016, the World Health Organization (WHO) recommended a non-nucleoside-reverse-transcriptase-inhibitor (NNRTI)-based combination as the preferred first-line regimen, while protease inhibitor (PI)-based combinations were recommended as second or third-line regimen mainly due to incomplete information regarding its risk when used during pregnancy [6]. In 2019, the WHO recommended in all adults living with HIV a transition to dolutegravir (DTG)-based ART, despite a slightly higher but significant neural tube defect signal associated with DTG exposure in the pre-conception period compared to other antiretroviral combinations [7]. After all, a DTG-based combination was recommended in all adults, including pregnant women, as the preferred first-line regimen due to improved efficacy, better tolerability and durability compared to all previous ART regimens [3, 8]. Despite the beneficial effects of antiretroviral drugs during pregnancy on both maternal health and PMTCT, their use raises concerns on their potential embryo-foeto-toxicity. It remains crucial to fully assess their associated perinatal outcomes to optimise ART strategies in pregnant women worldwide, but more particularly in sub-Saharan Africa, where both maternal HIV prevalence and rates of adverse perinatal outcomes are high [5]. Several studies have reported an increased risk of adverse perinatal outcomes after prenatal exposure to antiretroviral combinations, depending on the antiretroviral drug classes used [9,10,11,12,13,14,15,16]. PI-regimens still remain an important alternative option for pregnant women in 2022 that still need to be fully understood, due to conflicting results. Indeed, several studies have reported an association between PI-based combinations and preterm birth, while other studies have not found similar results [12, 15,16,17,18]. Therefore, we conducted a systematic review and meta-analysis aimed to assess the risk of adverse perinatal outcomes associated with PI-based combination use during pregnancy compared to NNRTI-based combination.
Methods
Search strategy and selection criteria
We did a systematic review and meta-analysis according to the Preferred Reporting Items for Systematic review and Meta-Analysis (PRISMA) guidelines [19]. The protocol of this review was registered in PROSPERO, the International prospective register of systematic reviews (CRD42022306896). The bibliographic research was based on both published and unpublished studies from 01/01/2002 to 29/10/2021 relative to adverse perinatal outcomes in HIV women who received antiretroviral combination during pregnancy.
Searches were conducted on four electronic scientific literature databases: PubMed, Reprotox, Clinical Trial registry (clinicaltrials.gov) and the abstracts from HIV conferences (Conference on Retroviruses and Opportunists Infections, International AIDS Society, European AIDS Clinical Society, British HIV Association and International Workshop on HIV Pediatrics). We used the keywords and MeSH terms presented in the Table 1.
Inclusion and exclusion criteria
To be eligible, studies must document population (pregnant women with documented perinatal outcomes) and exposure (antiretroviral combination based either on PI or NNRTI, initiated before or during pregnancy). We included all randomised controlled clinical trials, prospective and retrospective cohort studies using a comparative study design. Studies not eligible were those off-topic, not specifying the antiretroviral combination used, those where numbers of adverse perinatal outcomes according to antiretroviral combination were not detailed, those not comparing PI-based versus NNRTI-based antiretroviral combinations, studies with only one type of inhibitor used, and those where integral text was not available. For abstracts, we limited our search to studies in the English or French language. No restriction was applied to geographic area. Study investigators were contacted when the manuscript content was insufficient.
Outcomes
We studied the following adverse perinatal outcomes based on WHO definitions: preterm birth (PTB, < 37 weeks of gestation) [20], very preterm birth (VPTB, < 32 weeks of gestation), low birth weight (LBW, < 2500 g) [21], very low birth weight (VLBW, < 1500 g), small for gestational age (SGA, birthweight < 10th centile for gestational age) [22], very small for gestational age (VSGA, birthweight < 3th percentile for gestational age), stillbirth (foetus born with no sign of life after 28 weeks of gestation) [23], congenital abnormalities (alteration in embryonal development) [24] and spontaneous abortion (< 22 weeks of gestation) [25]. Gestational age was estimated based on the last menstrual period and confirmed by ultrasound when available.
Exposure variable
Pregnant women were considered exposed to antiretroviral combination if they started antiretroviral treatment before or during pregnancy, and continued at least until delivery. Antiretroviral combination was defined by at least three drugs: namely two nucleoside reverse transcriptase inhibitors (NRTI) associated with a PI (lopinavir/ritonavir, atazanavir/ritonavir, darunavir/ritonavir, fosamprenavir, saquinavir and nelfinavir) or a NNRTI (efavirenz or nevirapine). We categorised the exposure into three different periods: pre-conception, early pregnancy (first trimester) and late pregnancy (second and third trimester).
Data extraction and quality analysis
Two investigators, LSL and VL independently reviewed and identified the relevant citations. LSL performed data extraction including description of the studies, their populations, the adverse perinatal outcomes according to antiretroviral combination, and scores of methodological qualities. We used two scales for methodological quality assessment according to study design: the Oxford scale [26] for clinical trials and the Newcastle–Ottawa scale [27] for cohort studies. Methodological quality assessment was conducted by two investigators independently (LSL and JB) and any discordance was resolved by discussion with AS. Studies with an Oxford score lower than three [26] or a Newcastle–Ottawa score lower than four [27] were considered as low methodological quality and were excluded.
Statistical analysis
We first described the characteristics of the studies included. Then, we extracted data from individual studies to generate a relative risk (RR) of prenatal exposure to a PI-based combination compared to those with an NNRTI-based combination for each adverse perinatal outcome. We performed a meta-analysis when more than one study reported the same outcome, using a random effects model to estimate a weighted summary RR and corresponding 95% confidence intervals for each outcome [28, 29]. All pre-specified analyses were stratified according to country income: High-Income Countries (HIC) and Low-to-Middle-Income Countries (LMIC). We investigated between-study heterogeneity by reporting forest plots and using the I2 statistic, with a p-value significance of 0.10 (I² <0.10) [29]. The pooled summarised RR (sRR) was presented only when both LMIC and HIC RRs were consistent (I2 < 0.10). We searched publication bias using funnel-plot and asymmetric Egger tests [28]. We conducted sensitivity analyses excluding outlier studies by graphical research, and then including only studies with high score of methodological quality (Oxford score higher than five [26] and Newcastle–Ottawa score higher than seven [27]). For all analyses, we defined significance at an alpha level of 0.05 (p-value <0.05), except for heterogeneity analyses. Statistical analyses were performed using STATA (14.2).
Results
Study and population characteristics
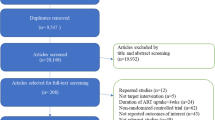
Our search identified 49,171 citations: 1,885 published studies and 47,286 unpublished studies. Initial screening was from title and abstracts of studies in 48,650 records, after exclusion of duplicates. Overall, 208 full-text articles were selected for a complete reading. Finally, after excluding four studies of low methodological quality (two clinical trials [30, 31] and two cohort studies [32, 33]), 32 studies were retained for systematic review and meta-analysis (Fig. 1). These studies were published between 2002 and 2021, and included 45,427 pregnant women from 27 countries. Nineteen (59%) studies were conducted in HIC and thirteen (41%) in LMIC. Only one randomised controlled trial (3.1%) was selected, those remaining being cohort studies. Overall, thirteen studies (40.6%) had a high score of methodological quality (Table 2). Study sample size varied from 75 to 7,009 pregnant women, maternal age from 26 to 33 years and median CD4 + from 154 to 638 cells/mm3 (Table 3).
Out of the 32 studies, gestational age was estimated using ultrasound scan alone, last menstrual period alone or a combination of at least two methods, in 3.2% (1/31), 16.1% (5/31) and 67.7% (21/35) respectively. Information on gestational age estimation methods was not available for five studies (15.6%), reporting only congenital abnormalities [35, 38, 39, 43, 51]. The most common perinatal outcomes reported were PTB (22/32, 68.8%), LBW (13/32, 40.6%) and SGA (13/32, 40.6%) (Table 3).
Preterm birth
PTB was reported in 4,872 cases in twenty-two studies (15.2% [14.8–15.6]) [10, 18, 36, 37, 41, 42, 45,46,47,48,49,50, 52, 53, 55,56,57,58,59,60, 63, 64] (Fig. 2). In both LMIC and HIC separately, prenatal exposure to PI-based combination was not significantly associated with PTB compared to NNRTI-based combination (RR 1.17, 95%CI 0.91–1.49 and RR 1.11, 95%CI 0.97–1.26, respectively), but between-study heterogeneity was significant (I2 67.4% p = 0.002 and 41.6% p = 0.057 respectively). No global summary estimate was provided due to significant heterogeneity. More specifically, in LMIC, heterogeneity was only due to the van der Merwe study [41], the single outlier with opposite results compared to the eight others studies. When excluding this study, the RR became significant (RR 1.26, 95%CI 1.11–1.43) and homogeneous (I2 0%, p = 0.882). When including only studies with high score of methodological quality in LMIC and HIC [36, 42, 45, 55, 56, 59, 60, 64], the results were also homogeneous with a global significant increased risk of PTB after prenatal exposure to PI-based combination, compared to NNRTI-based combination (sRR 1.20 [1.08–1.32], I2 0% p = 0.653).
Very preterm birth
We found a total of 638 VPTB from nine studies (3.9% [3.6–4.1]) [36, 37, 41, 42, 47, 53, 55, 59, 60] (Fig. 3). In LMIC, prenatal exposure to PI-based combination was not significantly associated with VPTB compared to NNRTI-based combination (RR 0.77, 95% CI 0.26–2.27), but with significant between-study heterogeneity (I2 = 81.9%, p = 0.004). No association was either found in HIC (RR 0.96, 95%CI 0.72–1.27, I2 5.3%, p = 0.383). Results were homogeneous when including only studies of high methodological quality [36, 42, 55, 60], reporting a global not significant risk of VPTB (sRR 1.19 [0.89–1.60], I2 15.1% p = 0.318).
Low birth weight
LBW was measured in thirteen studies for 1,902 cases (17.6% [16.9–18.3]) [10, 36, 37, 41, 47, 49, 50, 53, 55,56,57, 63, 64] (Fig. 4). In LMIC, prenatal exposure to PI-based combination was not significantly associated with LBW compared to NNRTI-based combination (RR 1.09, 95% CI 0.75–1.56), but between-study heterogeneity was significant (I2 = 74.5%, p < 10–4). In HIC, the RR was not significant (RR 0.93, 95%CI 0.80–1.08), and homogeneous (I2 16.5%, p = 0.307). Global results were homogeneous when including only studies of high methodological quality [52, 55, 59, 64], reporting a non-significant risk (sRR 1.04 [0.81–1.33], I2 0% p = 0.591).
Very low birth weight
VLBW was reported in 126 cases across seven studies (2.6% [2.2–3.1]) [36, 37, 41, 47, 53, 55, 63] (Fig. 5). Globally, prenatal exposure to PI-based combination was not significantly associated with VLBW compared to NNRTI-based combination (sRR 0.77, 95% CI 0.46–1.29), and without significant between-study heterogeneity (I2 15.4%, p = 0.313). Two studies [36, 55] had a high score of methodological quality and found similar results to those of the main analysis (sRR 0.82 [0.30–2.25], I2 0% p = 0.968).
Small for gestational age
The risk of SGA was reported in thirteen studies for 4615 cases (17.7% [17.3–18.2]) [18, 36, 37, 41, 42, 48, 52, 53, 55, 56, 60, 61, 64] (Fig. 6). In LMIC, prenatal exposure to PI-based combination was not significantly associated with SGA compared to NNRTI-based combination but significantly heterogeneous (RR 1.34, 95% CI 0.92–1.96, I2 77.8%, p = 0.001). In HIC, we found similar results (RR 1.11, 95%CI 0.92–1.34 and I2 54.2%, p = 0.033). When including only studies with high score of quality, we found similar results than those obtained in the main analysis: in LMIC [36, 42, 56, 64] (RR 1.18 [0.80–1.73], I2 56.5% p = 0.075) and HIC [55, 60, 61] (RR 1.35 [0.92–1.99], I2 45.5% p = 0.160).
Very small for gestational age
The risk of VSGA, which was reported in two studies for 508 cases (9.9% [9.0–10.7]) [42, 61] (Fig. 7), was globally significantly increased for prenatal exposure to PI-based compared to NNRTI-based combinations (sRR 1.41, 95% CI 1.08–1.84), and consistent between-studies (I2 = 0%, p = 0.322). Only two studies with a high score of methodological quality contributed to this outcome, which did not allow to evaluate the publication bias.
Stillbirth
Stillbirth was reported in four studies for 269 cases (2.0% [1.7–2.2]) [42, 47, 58, 62]. Globally, prenatal exposure to PI-based combination was not significantly associated with stillbirth risk compared to NNRTI-based combination (sRR 1.06, 95% CI 0.74–1.50) (Fig. 8), and consistent between studies (I2 = 0%, p = 0.953). We found similar results when including only the two studies with high methodological quality [42, 62] (sRR 1.09 [0.75–1.57], I2 = 0%, p = 0.829).
Congenital abnormalities
Congenital abnormalities were reported in nine studies for 279 cases (5.7% [5.0–6.3]) [35, 38,39,40, 43, 44, 46, 51, 63] (Fig. 9). Globally, prenatal exposure to PI-based combination was not significantly associated with congenital abnormalities compared to NNRTI-based combination (sRR 0.94, 95% CI 0.73–1.21). Between-study heterogeneity was not significant (I2 0%, p = 0.473). The three studies [38, 39, 43]] with a high score of methodological quality reported also a non-significant risk (sRR 1.22 [0.84–1.76], I2 0%, p = 0.832).
Spontaneous abortion
Spontaneous abortion was reported in only one study for 50 cases (20.4% [15.4–25.5]) [58]. In this study, prenatal exposure to PI-based combination was not significantly associated with spontaneous abortion compared to NNRTI-based combination (RR 1.26, 95% CI 0.77–2.08). No meta-analysis was conducted.
Exposure period of antiretroviral combination during pregnancy
We were not able to conduct subgroup analyses by exposure pregnancy periods because only one reported numbers of adverse perinatal outcomes according to the pre-conception period [53], and another one according to early/late pregnancy period (before or after 28 weeks of pregnancy) [41].
Discussion
While there is an increasing number of pregnant women living with HIV receiving antiretroviral therapy, especially in sub-Saharan Africa, the risk of adverse perinatal outcomes according to antiretroviral combinations exposure remains critical of fully assess. Our meta-analysis specifically assessed these risks associated with maternal PI-based antiretroviral combination still recommended by WHO as second- or third-line therapy, using a head-to-head comparison to NNRTI-based combination, based on a large sample size of pooled studies and originally stratified according to country income.
By pooling the estimates assessed from 32 studies, our meta-analysis comparing the risk of adverse perinatal outcome after prenatal exposure to PI-based compared to NNRTI-based combinations, in both LMIC and HIC countries, provided the following findings: firstly, we did not report any global significant pooled risk consistently for VLBW, stillbirth and congenital abnormalities. Secondly, despite significant heterogeneity between LMIC and HIC studies, there was no significant risk related to PI-ART exposure reported for VPTB, LBW and SGA. Thirdly, we found a global significant increased pooled risk of PI- based regimen for VSGA (+ 41% [8–84]), in two studies. Fourthly, we cannot formally conclude for the global risk of PTB with inconsistent findings according to sensitivity analysis. Lastly, no meta-analysis was conducted for the risk of spontaneous abortion, reported in only one study.
Three other systematic reviews previously published in 2018, 2020, and 2022 reported the effects of PI-based antiretroviral therapy associated with adverse perinatal outcomes [15, 16, 65]. Saleska et al. reported significant higher risk of LBW when only compared to zidovudine (ZDV) monotherapy, but no significant effect compared to NNRTI-based ART [65]. A network meta-analysis of randomized controlled trials conducted by Tsuivila-Matala, also reports that lopinavir/ritonavir (LPV/r) based regimens were associated with a significant higher risk of LBW compared to ZDV monotherapy, but this was not significant compared to NNRTI-based regimens [16]. In 2022, another meta-analysis reported the PI-ART-related adverse perinatal outcomes risks to be significantly higher for SGA (+ 24%,95% CI 8%-43%), and VSGA (+ 40%; 95% CI 9%-81%), but not with PTB or other perinatal outcomes [15].
Based on our results, prenatal exposure to PI-based ART is significantly associated with a increased risk for VSGA, as also recently reported by Cowdell et al. [15]. Some studies have shown that prenatal exposure to PI-based combination was associated with decreased progesterone levels during pregnancy, resulting in elevated estradiol levels [66,67,68]. Progesterone levels are correlated and estradiol levels are inversely correlated with birth weight. These hormonal changes, induced by prenatal exposure to PI-based combination, may be associated with fetal growth restriction and therefore with a higher VSGA risk [69, 70]. This hypothesis needs to be further investigated to better understand the potential effect of PI-based combination exposure on foetal growth.
In this meta-analysis, some perinatal outcomes (VSGA and spontaneous abortion) are reported in few studies, limiting result interpretation. Spontaneous abortion was investigated in only one study [58], with no meta-analysis conducted for this outcome. For VSGA, one large sample-size study [42] in Botswana, conducted in women who delivered in maternity wards at the national level using a standardized definition of perinatal outcomes, reported an increased risk of VSGA after prenatal exposure to PI-based combination compared to NNRTI-based combination. A standardized definition of gestational age was used in this study, while it is not necessarily the case in others LMIC, providing confidence in pregnancy outcome data quality. Another study [61], in HIC, did not find a significant result of VSGA, but weighed only 3.5% in the overall analysis of this risk. The results obtained for the VSGA risk seem robust thanks to large sample size study and use of standardized definition of perinatal outcomes, but need to be further investigated. Secondly, despite the subgroup analysis stratified between HIC and LMIC, between-study heterogeneity remains significant for most of the perinatal outcomes (PTB, VPTB, LBW and SGA), which may limit the interpretation of our results. This heterogeneity is partly explained by the diversity of methods used to measure perinatal outcomes. We can suppose that estimation of gestational age was more accurate in HIC compared to LMIC, because ultrasound is usually performed at least once during pregnancy in HIC. The heterogeneity for PTB risk can also be explained by one outlier study, excluded in sensitivity analysis in LMIC. The van der Merwe study [41] was conducted in South Africa between 2004 and 2007, and included pregnant women with a median CD4 count of 155 cells/mm3. NNRTI exposure was preferred for women with advanced HIV infection or co-infected with tuberculosis. Tuberculosis can be associated with growth restriction and PTB [71, 72]. It can explain outlier data with high prevalence for NNRTI exposure. Without this study, we found a significant increased risk (+ 26%) for PTB associated to prenatal exposure to PI-based combinations, compared to NNRTI-based combinations. This result was also find in the sensitivity analysis conducted only on studies with high scores of methodological quality (+ 20%). Therefore, the result reported in the main analysis appears not robust and heterogeneous. It must be interpreted cautiously, considering the significant association found in the two sensitivity analyses. Moreover, we cannot conduct sensitivity analyses excluding outlier studies for others perinatal outcomes (VPTB, LBW and SGA) due to conflicting results. Indeed, results in the main analysis were heterogeneous, especially in LMIC. However, we found homogeneous and similar results in the sensitivity analyses including only studies with high scores of methodological qualities (VPTB and LBW), showing the robustness of the main analysis results. Last, despite the sensitive analysis conducted on high quality studies, the result of SGA remained heterogeneous but still not significant. As we found a significant increased risk of VSGA, we supposed that no significant risk was reported due to lack of statistical power in the subgroup analyses. Since these two perinatal outcomes are strongly correlated (SGA and VSGA), we suggest to conduct further investigations on the effect of PI-based combination exposure on overall foetal growth.
Our systematic review has some limitations. We could not disentangle effects of HIV exposure also associated with adverse perinatal outcomes [2] from those associated with antiretroviral exposure. The impact of the timing of ART initiation in pregnancy (before/after conception) on perinatal outcomes remains uncertain, as we were not able to conduct the sensitivity analyses due to the lack of information. In our study, we did not specifically explore the effect of NRTI backbone, but it would be relevant to investigate the potential association between PTB and VPTB risks and exposure to ZDV-3TC-LPV/r. Finally, we were not able to investigate the effects on perinatal outcomes according the different PI-based regimen.
Our systematic review has also strengths. Our search was exhaustive thanks to use of several bibliographical databases, abstracts of HIV conference and clinical trials registry. Studies included all available comparative study designs (randomized clinical trials and cohorts) to guarantee the representativeness. No restriction for geographical area and publication date ensured representative results. The use of an appropriate comparator defined as a NNRTI antiretroviral combination allowed us to estimate relative risks, strong indicators of risk. Methodological quality assessment was also performed by two investigators independently. Standardization of data collection and outcome definition raise many challenges in data quality assessment [73]. Our results were detailed according to country-outcome to consider data quality heterogeneity. We conducted sensitivity analyses including only studies with high methodological quality and results were mostly consistent with those of the main analysis. Most of the results obtained in the subgroup analyses were consistent with those obtained in primary analysis, with robust analysis for most of the outcomes, except for PTB.
Conclusion
Our study did not show a higher risk for most of the adverse perinatal outcomes after prenatal exposure to PI-based combination compared to NNRTI-based combination. However, our review suggests a significant increased risk of VSGA, similarly reported in another recent review [15]. The risk of PTB initially reported is not clearly demonstrated [10, 18, 30, 31, 36, 37, 41, 45, 48, 49, 52, 53, 55,56,57,58,59, 63, 64], with significant between-studies heterogeneity. Therefore, this result should be interpreted with caution. Our results should be considered to inform clinical guidelines, with appropriate messaging regarding the PI benefit-risk balance in pregnant women and those of childbearing potential living with HIV to improve their perinatal outcomes.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartame aminotransferase
- ATHENA:
-
AIDS Therapy Evaluation in the Netherlands
- CI95:
-
Confidence interval 95
- ECS:
-
European Collaborative Study
- HAART:
-
Highly Active Antiretroviral Therapy
- HIV:
-
Human Immunodeficiency Virus
- IPMTCT:
-
Integrated Prevention of Mother To Child Transmission
- EFV:
-
Efavirenz
- EPPICC:
-
European Pregnancy and Paediatric HIV Cohort Collaboration
- LBW:
-
Low birth weight
- LPV/r:
-
Lopinavir/ritonavir
- MTCT:
-
Mother to Child Transmission
- NA:
-
Not available
- NSHPC:
-
National Study of HIV in Pregnancy and Childhood
- ND:
-
Not define
- NISDI:
-
NICHD (National Institute of Child Health & Human Development) International Site Development Initiative
- NNRTI:
-
Non-nucleoside reverse transcriptase inhibitor
- non PI:
-
Considered here like NNRTI
- NVP:
-
Nevirapine
- PI:
-
Protease inhibitor
- PSD:
-
Pediatric Spectrum of HIV Disease
- RR:
-
Relative Risks
- SGA:
-
Small for gestational age
- SMARTT:
-
Surveillance Monitoring of ART Toxicities, the French ANRS (National Research Agency on HIV and hepatitis)
- TS:
-
Trimethoprim-sulfamethoxazole
- VLBW:
-
Very low birth weight
- VPT:
-
Very preterm birth
- VSGA:
-
Very small for gestational age
- WHO:
-
World Health Organisation
References
UNAIDS. Global HIV & AIDS statistics — Fact sheet 2022 n.d. https://www.unaids.org/en/resources/fact-sheet (accessed August 2, 2022).
Wedi COO, Kirtley S, Hopewell S, Corrigan R, Kennedy SH, Hemelaar J. Perinatal outcomes associated with maternal HIV infection: a systematic review and meta-analysis. Lancet HIV. 2016;3:e33-48. https://doi.org/10.1016/S2352-3018(15)00207-6.
WHO | Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: what’s new. WHO n.d. http://www.who.int/hiv/pub/arv/policy-brief-arv-2015/en/ (accessed January 16, 2019).
WHO. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV guidelines 2015. http://apps.who.int/iris/bitstream/10665/186275/1/9789241509565_eng.pdf?ua=1 (accessed June 10, 2018).
WHO. HIV/AIDS - Key facts 2020. https://www.who.int/news-room/fact-sheets/detail/hiv-aids (accessed January 9, 2019).
WHO. Update of recommendations on first- and second-line antiretroviral regimens 2019.
Zash R, Holmes L, Diseko M, Jacobson DL, Brummel S, Mayondi G, et al. Neural-Tube Defects and Antiretroviral Treatment Regimens in Botswana. N Engl J Med. 2019;381:827–40. https://doi.org/10.1056/NEJMoa1905230.
Mofenson LM, Pozniak AL, Wambui J, Raizes E, Ciaranello A, Clayden P, et al. Optimizing responses to drug safety signals in pregnancy: the example of dolutegravir and neural tube defects. J Int AIDS Soc. 2019;22:e25352. https://doi.org/10.1002/jia2.25352.
WHO. Lignes directrices unifiées relatives à l’utilisation de médicaments antirétroviraux pour le traitement et la prévention de l’infection à VIH 2015. http://www.who.int/hiv/pub/arv/policy-brief-arv-2015/fr/ (accessed March 23, 2018).
Schulte J, Dominguez K, Sukalac T, Bohannon B, Fowler MG. for the Pediatric Spectrum of HIV Disease Consortium. Declines in Low Birth Weight and Preterm Birth Among Infants Who Were Born to HIV-Infected Women During an Era of Increased Use of Maternal Antiretroviral Drugs: Pediatric Spectrum of HIV Disease, 1989–2004. PEDIATRICS. 2007;119:e900-6. https://doi.org/10.1542/peds.2006-1123.
Simon A, Warszawski J, Kariyawasam D, Le Chenadec J, Benhammou V, Czernichow P, et al. Association of prenatal and postnatal exposure to lopinavir-ritonavir and adrenal dysfunction among uninfected infants of HIV-infected mothers. JAMA. 2011;306:70–8. https://doi.org/10.1001/jama.2011.915.
Sibiude J, Warszawski J, Tubiana R, Dollfus C, Faye A, Rouzioux C, et al. Premature delivery in HIV-infected women starting protease inhibitor therapy during pregnancy: role of the ritonavir boost? Clin Infect Dis Off Publ Infect Dis Soc Am. 2012;54:1348–60. https://doi.org/10.1093/cid/cis198.
Ørbaek M, Thorsteinsson K, Moseholm Larsen E, Katzenstein TL, Storgaard M, Johansen IS, et al. Risk factors during pregnancy and birth-related complications in HIV-positive versus HIV-negative women in Denmark, 2002–2014. HIV Med. 2020;21:84–95. https://doi.org/10.1111/hiv.12798.
Williams PL, Yildirim C, Chadwick EG, Van Dyke RB, Smith R, Correia K, et al. Association of maternal antiretroviral use with microcephaly in children who are HIV-exposed but uninfected (SMARTT): a prospective cohort study - The Lancet HIV 2019.
Cowdell I, Beck K, Portwood C, Sexton H, Kumarendran M, Brandon Z, et al. Adverse perinatal outcomes associated with protease inhibitor-based antiretroviral therapy in pregnant women living with HIV: A systematic review and meta-analysis. EClinicalMedicine. 2022;46:101368. https://doi.org/10.1016/j.eclinm.2022.101368.
Tshivuila-Matala COO, Honeyman S, Nesbitt C, Kirtley S, Kennedy SH, Hemelaar J. Adverse perinatal outcomes associated with antiretroviral therapy regimens: systematic review and network meta-analysis. AIDS Lond Engl. 2020;34:1643–56. https://doi.org/10.1097/QAD.0000000000002593.
Tookey PA, Thorne C, van Wyk J, Norton M. Maternal and foetal outcomes among 4118 women with HIV infection treated with lopinavir/ritonavir during pregnancy: analysis of population-based surveillance data from the national study of HIV in pregnancy and childhood in the United Kingdom and Ireland. BMC Infect Dis. 2016;16:65. https://doi.org/10.1186/s12879-016-1400-y.
Watts DH, Williams PL, Kacanek D, Griner R, Rich K, Hazra R, et al. Combination Antiretroviral Use and Preterm Birth. J Infect Dis. 2013;207:612–21. https://doi.org/10.1093/infdis/jis728.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009;6:e1000100. https://doi.org/10.1371/journal.pmed.1000100.
WHO. Preterm birth 2018. https://www.who.int/news-room/fact-sheets/detail/preterm-birth (accessed January 9, 2019).
WHO. Newborns with low birth weight. WHO 2006. http://webcache.googleusercontent.com/search?q=cache:-JeHP_u3DZAJ:www.who.int/whosis/whostat2006NewbornsLowBirthWeight.pdf+&cd=6&hl=fr&ct=clnk&gl=fr&client=firefox-b (accessed March 22, 2018).
Sharma D, Shastri S, Sharma P. Intrauterine Growth Restriction: Antenatal and Postnatal Aspects. Clin Med Insights Pediatr. 2016;10:67–83. https://doi.org/10.4137/CMPed.S40070.
WHO. Stillbirths. WHO 2015. http://www.who.int/maternal_child_adolescent/epidemiology/stillbirth/en/ (accessed March 22, 2018).
WHO. Congenital anomalies 2016. https://www.who.int/news-room/fact-sheets/detail/congenital-anomalies (accessed January 9, 2019).
Regan L, Rai R. Epidemiology and the medical causes of miscarriage. Baillieres Best Pract Res Clin Obstet Gynaecol. 2000;14:839–54. https://doi.org/10.1053/beog.2000.0123.
Jadad AR. Assessing the quality of reports of randomized clinical trials: is blinding necessary? n.d.
Wells GA. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses n.d. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed April 24, 2018).
Bias in Meta-analyses (Funnel Plots and Tests) - StatsDirect n.d. https://www.statsdirect.com/help/meta_analysis/bias_detection.htm (accessed June 10, 2018).
Cucherat M. Hétérogénéité et analyses en sous-groupes n.d.
Masaba R, Borkowf CB, Girde S, Zeh C, Ndivo R, Nyang’au I, et al. Adverse fetal and infant outcomes among HIV-infected women who received either nonnucleoside reverse transcriptase inhibitor-based or protease inhibitor-based antiretroviral therapy for prevention of mother-to-child transmission. AIDS Lond Engl. 2018;32:1625–32. https://doi.org/10.1097/QAD.0000000000001816.
Koss CA, Natureeba P, Plenty A, Luwedde F, Mwesigwa J, Ades V, et al. Risk Factors for Preterm Birth Among HIV-Infected Pregnant Ugandan Women Randomized to Lopinavir/Ritonavir- or Efavirenz-Based Antiretroviral Therapy: JAIDS. J Acquir Immune Defic Syndr. 2014;67:128–35. https://doi.org/10.1097/QAI.0000000000000281.
Heather Watts D, Covington DL, Beckerman K, Garcia P, Scheuerle A, Dominguez K, et al. Assessing the risk of birth defects associated with antiretroviral exposure during pregnancy. Am J Obstet Gynecol. 2004;191:985–92. https://doi.org/10.1016/j.ajog.2004.05.061.
Winston J, Kasaro M, Stoner MCD, Mulenga L, Price JT, Stringer E, et al. Prenatal antiretroviral exposure and risk of low birth weight in Lusaka, Zambia, Boston, Massachusetts: 2018.
Delicio AM, Lajos GJ, Amaral E, Cavichiolli F, Polydoro M, Milanez H. Adverse effects in children exposed to maternal HIV and antiretroviral therapy during pregnancy in Brazil: a cohort study. Reprod Health 2018;15. https://doi.org/10.1186/s12978-018-0513-8.
Townsend CL, Tookey PA, Cortina-Borja M, Peckham CS. Antiretroviral Therapy and Congenital Abnormalities in Infants Born to HIV-1-Infected Women in the United Kingdom and Ireland, 1990 to 2003. J Acquir Immune Defic Syndr. 2006;42:91–4. https://doi.org/10.1097/01.qai.0000196667.24239.c2.
Malaba TR, Phillips T, Le Roux S, Brittain K, Zerbe A, Petro G, et al. Antiretroviral therapy use during pregnancy and adverse birth outcomes in South African women. Int J Epidemiol. 2017;46:1678–89. https://doi.org/10.1093/ije/dyx136.
Phiri K, Williams PL, Dugan KB, Fischer MA, Cooper WO, Seage GR, et al. Antiretroviral Therapy Use During Pregnancy and the Risk of Small for Gestational Age Birth in a Medicaid Population. Pediatr Infect Dis J. 2015;34:e169-175. https://doi.org/10.1097/INF.0000000000000712.
Brogly SB, Abzug MJ, Watts DH, Cunningham CK, Williams PL, Oleske J, et al. Birth defects among children born to human immunodeficiency virus-infected women: pediatric AIDS clinical trials protocols 219 and 219C. Pediatr Infect Dis J. 2010;29:721–7. https://doi.org/10.1097/INF.0b013e3181e74a2f.
Prieto LM, González- Tomé MI, Muñoz E, Fernández-Ibieta M, Soto B, Álvarez A, et al. Birth defects in a cohort of infants born to HIV-infected women in Spain, 2000–2009. BMC Infect Dis. 2014;14:700. https://doi.org/10.1186/s12879-014-0700-3.
Floridia M, Mastroiacovo P, Tamburrini E, Tibaldi C, Todros T, Crepaldi A, et al. Birth defects in a national cohort of pregnant women with HIV infection in Italy, 2001–2011. BJOG Int J Obstet Gynaecol. 2013;120:1466–75. https://doi.org/10.1111/1471-0528.12285.
van der Merwe K, Hoffman R, Black V, Chersich M, Coovadia A, Rees H. Birth outcomes in South African women receiving highly active antiretroviral therapy: a retrospective observational study. J Int AIDS Soc. 2011;14:42. https://doi.org/10.1186/1758-2652-14-42.
Zash R, Jacobson DL, Diseko M, Mayondi G, Mmalane M, Essex M, et al. Comparative Safety of Antiretroviral Treatment Regimens in Pregnancy. JAMA Pediatr. 2017;171:e172222. https://doi.org/10.1001/jamapediatrics.2017.2222.
Williams PL, Crain MJ, Yildirim C, Hazra R, Van Dyke RB, Rich K, et al. Congenital anomalies and in utero antiretroviral exposure in human immunodeficiency virus-exposed uninfected infants. JAMA Pediatr. 2015;169:48–55. https://doi.org/10.1001/jamapediatrics.2014.1889.
Patel D, Thorne C, Fiore S, Newell M-L, European Collaborative Study. Does highly active antiretroviral therapy increase the risk of congenital abnormalities in HIV-infected women? J Acquir Immune Defic Syndr 1999 2005;40:116–8.
Hu F, Liang JJ, Lu JJ, Hu YF, Hu Y, Yu J, et al. Effects of Antiretroviral Therapy and HIV Exposure in Utero on Adverse Pregnancy and Infant Outcomes: A Prospective Cohort Study in Guangzhou. China Biomed Environ Sci BES. 2019;32:719–29. https://doi.org/10.3967/bes2019.092.
Grosch-Woerner I, Puch K, Maier R, Niehues T, Notheis G, Patel D, et al. Increased rate of prematurity associated with antenatal antiretroviral therapy in a German/Austrian cohort of HIV-1-infected women: Antiretroviral therapy during pregnancy. HIV Med. 2008;9:6–13. https://doi.org/10.1111/j.1468-1293.2008.00520.x.
Cotter AM, Garcia AG, Duthely ML, Luke B, O’Sullivan MJ. Is Antiretroviral Therapy during Pregnancy Associated with an Increased Risk of Preterm Delivery, Low Birth Weight, or Stillbirth? J Infect Dis. 2006;193:1195–201. https://doi.org/10.1086/503045.
Carceller A, Ferreira E, Alloul S, Lapointe N. Lack of Effect on Prematurity, Birth Weight, and Infant Growth from Exposure to Protease Inhibitors In Utero and After Birth. Pharmacotherapy. 2009;29:1289–96. https://doi.org/10.1592/phco.29.11.1289.
Natureeba P, Ades V, Luwedde F, Mwesigwa J, Plenty A, Okong P, et al. Lopinavir/ritonavir-based antiretroviral treatment (ART) versus efavirenz-based ART for the prevention of malaria among HIV-infected pregnant women. J Infect Dis. 2014;210:1938–45. https://doi.org/10.1093/infdis/jiu346.
Szyld EG, Warley EM, Freimanis L, Gonin R, Cahn PE, Calvet GA, et al. Maternal antiretroviral drugs during pregnancy and infant low birth weight and preterm birth. AIDS. 2006;20:2345–53. https://doi.org/10.1097/01.aids.0000253362.01696.9d.
Joao EC, Calvet GA, Krauss MR, Freimanis Hance L, Ortiz J, Ivalo SA, et al. Maternal Antiretroviral Use During Pregnancy and Infant Congenital Anomalies: The NISDI Perinatal Study: JAIDS. J Acquir Immune Defic Syndr. 2010;53:176–85. https://doi.org/10.1097/QAI.0b013e3181c5c81f.
European Pregnancy and Paediatric HIV Cohort Collaboration (EPPICC) Study Group. Nucleoside reverse transcriptase inhibitor backbones and pregnancy outcomes. AIDS Lond Engl 2019;33:295–304. https://doi.org/10.1097/QAD.0000000000002039.
Snijdewind IJM, Smit C, Godfried MH, Bakker R, Nellen JFJB, Jaddoe VWV, et al. Preconception use of cART by HIV-positive pregnant women increases the risk of infants being born small for gestational age. PLoS ONE. 2018;13:e0191389. https://doi.org/10.1371/journal.pone.0191389.
Kreitchmann R, Li S, Melo V, Fernandes Coelho D, Watts D, Joao E, et al. Predictors of adverse pregnancy outcomes in women infected with HIV in Latin America and the Caribbean: a cohort study. BJOG Int J Obstet Gynaecol. 2014;121:1501–8. https://doi.org/10.1111/1471-0528.12680.
Floridia M, Dalzero S, Giacomet V, Tamburrini E, Masuelli G, Savasi V, et al. Pregnancy and neonatal outcomes in women with HIV-1 exposed to integrase inhibitors, protease inhibitors and non-nucleoside reverse transcriptase inhibitors: an observational study. Infection. 2020;48:249–58. https://doi.org/10.1007/s15010-019-01384-5.
Ejigu Y, Magnus JH, Sundby J, Magnus MC. Pregnancy outcome among HIV-infected women on different antiretroviral therapies in Ethiopia: a cohort study. BMJ Open. 2019;9:e027344. https://doi.org/10.1136/bmjopen-2018-027344.
Machado ES, Hofer CB, Costa TT, Nogueira SA, Oliveira RH, Abreu TF, et al. Pregnancy outcome in women infected with HIV-1 receiving combination antiretroviral therapy before versus after conception. Sex Transm Infect. 2008;85:82–7. https://doi.org/10.1136/sti.2008.032300.
Stringer EM, Kendall MA, Lockman S, Campbell TB, Nielsen-Saines K, Sawe F, et al. Pregnancy outcomes among HIV-infected women who conceived on antiretroviral therapy. PLoS ONE. 2018;13:e0199555. https://doi.org/10.1371/journal.pone.0199555.
Patel K, Shapiro DE, Brogly SB, Livingston EG, Stek AM, Bardeguez AD, et al. Prenatal Protease Inhibitor Use and Risk of Preterm Birth among HIV-Infected Women Initiating Antiretroviral Drugs during Pregnancy on JSTOR. J Infect Dis n.d.;Vol. 201:1035–44.
Favarato G, Townsend CL, Bailey H, Peters H, Tookey PA, Taylor GP, et al. Protease inhibitors and preterm delivery: another piece in the puzzle. AIDS Lond Engl. 2018;32:243–52. https://doi.org/10.1097/QAD.0000000000001694.
Aaron E, Bonacquisti A, Mathew L, Alleyne G, Bamford LP, Culhane JF. Small-for-gestational-age births in pregnant women with HIV, due to severity of HIV disease, not antiretroviral therapy. Infect Dis Obstet Gynecol. 2012;2012:135030. https://doi.org/10.1155/2012/135030.
Favarato G, Townsend CL, Peters H, Sconza R, Bailey H, Cortina-Borja M, et al. Stillbirth in Women Living With HIV Delivering in the United Kingdom and Ireland: 2007–2015. J Acquir Immune Defic Syndr. 1999;2019(82):9–16. https://doi.org/10.1097/QAI.0000000000002087.
Bellón Cano JM, Sánchez-Ramón S, Ciria L, León JA, Gurbindo D, Fortuny C, et al. The effects on infants of potent antiretroviral therapy during pregnancy: a report from Spain. Med Sci Monit Int Med J Exp Clin Res. 2004;10:CR179-184.
Delicio AM, Lajos GJ, Amaral E, Cavichiolli F, Polydoro M, Milanez H. Adverse effects in children exposed to maternal HIV and antiretroviral therapy during pregnancy in Brazil: a cohort study. Reprod Health. 2018;15:76. https://doi.org/10.1186/s12978-018-0513-8.
Saleska JL, Turner AN, Maierhofer C, Clark J, Kwiek JJ. Use of Antiretroviral Therapy During Pregnancy and Adverse Birth Outcomes Among Women Living With HIV-1 in Low- and Middle-Income Countries: A Syst... - PubMed - NCBI. JAIDS. 2018;79:1–9. https://doi.org/10.1097/QAI.0000000000001770.
Papp E, Mohammadi H, Loutfy MR, Yudin MH, Murphy KE, Walmsley SL, et al. HIV protease inhibitor use during pregnancy is associated with decreased progesterone levels, suggesting a potential mechanism contributing to fetal growth restriction. J Infect Dis. 2015;211:10–8. https://doi.org/10.1093/infdis/jiu393.
Papp E, Balogun K, Banko N, Mohammadi H, Loutfy M, Yudin MH, et al. Low Prolactin and High 20-α-Hydroxysteroid Dehydrogenase Levels Contribute to Lower Progesterone Levels in HIV-Infected Pregnant Women Exposed to Protease Inhibitor-Based Combination Antiretroviral Therapy. J Infect Dis. 2016;213:1532–40. https://doi.org/10.1093/infdis/jiw004.
Balogun KA, Guzman Lenis MS, Papp E, Loutfy M, Yudin MH, MacGillivray J, et al. Elevated Levels of Estradiol in Human Immunodeficiency Virus-Infected Pregnant Women on Protease Inhibitor-Based Regimens. Clin Infect Dis Off Publ Infect Dis Soc Am. 2018;66:420–7. https://doi.org/10.1093/cid/cix761.
Mohammadi H, Papp E, Cahill L, Rennie M, Banko N, Pinnaduwage L, et al. HIV antiretroviral exposure in pregnancy induces detrimental placenta vascular changes that are rescued by progesterone supplementation. Sci Rep. 2018;8:6552. https://doi.org/10.1038/s41598-018-24680-w.
Wong JMH, Kanga N, Dogra N, Ngoma MS, Serghides L, Silverman M. Perceived acceptability of progesterone to prevent preterm births and low birth weight among HIV-infected and HIV-uninfected Zambian pregnant women. Int J Womens Health. 2017;9:827–33. https://doi.org/10.2147/IJWH.S136191.
Noble A, Ning Y, Woelk GB, Mahomed K, Williams MA. Preterm delivery risk in relation to maternal HIV infection, history of malaria and other infections among urban Zimbabwean women. Cent Afr J Med. 2005;51:53–8.
Goldenberg RL, Culhane JF, Johnson DC. Maternal infection and adverse fetal and neonatal outcomes. Clin Perinatol. 2005;32:523–59. https://doi.org/10.1016/j.clp.2005.04.006.
Renaud F, Mofenson LM, Bakker C, Dolk H, Leroy V, Namiba A, et al. Surveillance of ARV safety in pregnancy and breastfeeding: towards a new framework. J Int AIDS Soc. 2022;25:e25922. https://doi.org/10.1002/jia2.25922.
Acknowledgements
We gratefully acknowledge the French ANRS (National Research Agency on HIV and hepatitis) for their funding. Laura Saint-Lary had a doctoral scholarship funded by the ANRS (ANRS n°12433 B112 AAP 2020-1). We warmly thank Sophie Desmonde for her helpful editing comments on the manuscript.
Funding
Laura Saint-Lary had a doctoral scholarship funded by the ANRS (ANRS n°12433 B112 AAP 2020–1). The interpretation of results expressed in this article arose from the authors and do not reflect the views of the funder. All authors had access to the data of the study.
Author information
Authors and Affiliations
Contributions
LSL, VL and AS contributed to the search strategy and selection criteria; CDM and CV verified and confirmed the definition of perinatal outcomes; LSL extracted the data of each selected study and contacted authors if necessary; LSL, JB and AS realized methodological quality analysis; LSL realized the statistical analysis; all authors reviewed and edited the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent of publication
Not applicable.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Saint-Lary, L., Benevent, J., Damase-Michel, C. et al. Adverse perinatal outcomes associated with prenatal exposure to protease-inhibitor-based versus non-nucleoside reverse transcriptase inhibitor-based antiretroviral combinations in pregnant women with HIV infection: a systematic review and meta-analysis. BMC Pregnancy Childbirth 23, 80 (2023). https://doi.org/10.1186/s12884-023-05347-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-05347-5