Abstract
Purpose
This review aimed to investigate the association of insulin resistance (IR) in women with recurrent pregnancy loss compared to women with normal pregnancy history.
Methods
PubMed, EMBASE, the Web of Science and Google Scholar databases were accessed to collect published observational studies that compared IR of recurrent pregnancy loss women with healthy women until the 6th of October 2022. Outcomes assessed in this review and meta-analysis included fasting blood glucose, fasting plasma insulin, homeostasis model assessment for IR, glucose to insulin ratio. Mean differences, odds ratios with 95% confidence interval were pooled using the fixed or random effect models. Sensitivity analyses were performed to validate the robustness of the results. Review Manager version 5.4.1 and Stata version 8.0 were used.
Results
A total of nineteen studies involving 4453 individuals were included. Recurrent pregnancy loss patients presented significantly higher fasting blood glucose, fasting plasma insulin, homeostasis model assessment for IR, and lower glucose to insulin ratios. Additionally, recurrent pregnancy loss patients had higher rates of IR as defined by abnormal fasting plasma insulin, homeostasis model assessment for IR, and glucose to insulin ratio. Sensitivity analyses validated the robustness of the results.
Conclusion
In the current review, we show that recurrent pregnancy loss is associated with a higher degree of IR and highlight the importance of screening and treatment of IR.
Similar content being viewed by others
Background
Recurrent pregnancy loss (RPL) affects approximately 2–5% of women [1]. Common causes of RPL include chromosomal abnormalities [2], uterine abnormalities [3], endocrine imbalances [4], autoimmune factors such as antiphospholipid syndrome [5], thrombophilia [6], and environmental factors such as tobacco use, caffeine intake, and alcohol use [7,8,9]. However, despite comprehensive evaluation, more than 50% of cases remain unexplained [10]. American Heart Association recommend to incorporate obstetric complications including preeclampsia, gestational diabetes, or pregnancy-induced hypertension as risk factors for development of cardiovascular disease in women [11]. A history of recurrent miscarriages was associated with higher risk of non-fatal and fatal stroke in a recent review [12]. These evidences suggest that cardiovascular and metabolic abnormalities may also predispose to RPL.
Previous studies have shown that insulin resistance (IR) may play a role in female reproduction. Tian et al. suggested that IR was an independent risk factor for spontaneous abortion in women who received infertility treatment [13]. Additionally, several studies show that IR may play a role in polycystic ovary syndrome (PCOS) since their underlying connection [14, 15]. For example, a recent systematic review and meta-analysis of the literature highlighted IR as a risk factor for spontaneous abortion in PCOS patients undergoing assisted reproduction [16]. Hyperinsulinemia and IR are also associated with poor reproductive outcomes in PCOS patients undergoing ovulation induction [17]. Previous studies have shown that insulin functioning and metabolism are changed during pregnancy and that IR has serious implications for pregnancy outcomes and long-term morbidity for both the mother and fetus [18]. However, the potential effect of IR on RPL remains to be elucidated. Thus far, several case–control studies have reported differences in IR between women with RPL and healthy controls. However, no comprehensive review exists on this topic.
In the current review, we aim to run a meta-analysis and systematically review relevant literature to establish the role of IR status in RPL patients relative to healthy controls.
Methods and materials
Literature search strategy
This systematic review and meta-analysis was constructed according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) [19] (Supplementary Table 1). The protocol was previously registered (INPLASY2021110055). Major electronic databases including PubMed, Embase, and Web of Science were used to source relevant literature published until the 6th of October 2022. Key search terms included: “recurrent miscarriage”, “insulin resistance”, and “case–control” (Supplementary Table 2). Google Scholar was also searched for related articles that may not be in the search databases. References from all included studies were also assessed to identify relevant articles not captured by the electronic searches.
Inclusion and exclusion criteria
Observational studies that compared IR parameters in RPL patients to control women with normal pregnancy history were included. IR parameters included fasting blood glucose (FBG), fasting insulin (FIN), homeostasis model assessment for insulin resistance (HOMA-IR), glucose to insulin ratio (GI ratio). Only studies that were published in English were included. Review articles, opinions, book chapters, letters, published abstracts, animal studies, case reports were excluded. For studies with no suitable control women (e.g. healthy pregnant women, women with healthy pregnancy history) to RPL women, they were excluded.
Study selection
Two authors (WYC and XL) independently scrutinized the titles and abstracts of all potential studies to strictly identify relevant studies according to the inclusion and exclusion criteria. Relevant studies that were considered for inclusion were then carefully reviewed. Any disagreement between the two authors was resolved by a third author (JX).
Data extraction
Two authors (WYC and XL) independently extracted data using the following format: the first author, year of publication, geographic region, sample size, study design, age of case and control, outcome measures, exclusion of known factors which contribute to RPL, and matched factors were recorded. Where a study with two or more publications was identified, only the most comprehensive or the most recent version was included. For publications that reported median and interquartile range, the mean and standard deviation was estimated [20].
Quality assessment
The quality of eligible observational studies was assessed using the Newcastle–Ottawa scale (NOS) [21]. The NOS assesses studies by scoring three aspects: viz selection, comparability, and exposure. The total NOS is scored out of 9 (the higher the score, the better). Each article was awarded a score out of four for selection bias (adequate definition of case, representativeness of the case, selection of control, definition of control), two for comparability (comparability between case and control), and four for bias in the exposure (ascertainment of exposure, consistency of the method of ascertainment for case and control, and non-response rate).
Statistical analyses
Review Manager version 5.4.1 and Stata version 8.0 were used to analyze the extracted data. The mean difference (MD) or odds ratio (OR) with 95% confidence interval (CI) were pooled to measure the effect size. The heterogeneity of studies was measured using the I2 index: a value below 40% indicated no heterogeneity; a value greater than 40% indicated the occurrence of heterogeneity. When no heterogeneity was observed, the fixed-effects model was used. The random-effects model was used when heterogeneity existed. Publication bias was assessed using funnel plot asymmetry, Egger’s (number of included studies < = 10) or Begg’s (number of included studies > 10) line regression test. To measure the effect of confounders on the effect size, subgroup analysis was performed. To confirm the robustness of the results, a sensitivity analysis was performed by systematically excluding each study included in the analysis. A P-value less than 0.05 was considered statistically significant.
Results
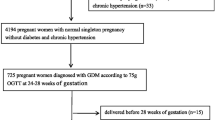
Following title and abstract screening of the literature search results, 1246 total studies were assessed of which 238 were duplicates and 937 were considered irrelevant. Of the remaining 71 records, 52 records were excluded due to only abstract (n = 9), assisted reproduction (n = 3), case report (n = 1), no control group (n = 7), PCOS (n = 9), no interested outcomes (n = 16), review (n = 6), replicate (n = 1) (Fig. 1). No additional studies were identified through Google Scholar and article references. Therefore, a total of 19 studies were eligible for data extraction and were included in the present meta-analysis [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40] (Fig. 1).
Characteristics of included studies
The studies included in this review were published between 2002 and 2022, and consist of 2223 RPL women and 2230 control women (Table 1). Among the studies assessed, six were conducted in the Middle East, six in Asia, three in Africa, two in North America, and two in Europe. All studies were case-controlled. The participant's mean age of RPL cases ranged from 24.8 to 35.8 years. Eight studies defined RPL as three or more consecutive miscarriages, eleven studies defined RPL as two or more consecutive miscarriages. Fourteen studies excluded known factors for RPL while five studies did not exclude such factors. Four studies measured outcomes during pregnancy, while fifteen studies measured outcomes in women who were not pregnant. Ten studies matched for one or more confounders, while nine studies did not match for confounding factors at all. FBG was assessed in eighteen studies. FIN was assessed in sixteen studies. HOMA-IR was assessed in eight studies. The GI ratio was assessed in five studies. The qualitative assessment of the data revealed that the data of all included studies were of medium to high quality (Table 2).
FBG
FBG was measured in eighteen of the studies (Fig. 2). Nineteen comparisons were made as one study had two comparisons. Our meta-analysis indicated higher levels of FBG among RPL women compared to the control group (I2 = 88% [83%-92%]). The funnel plot showed no obvious asymmetry indicative of a lack of evidence of publication bias (Supplementary Fig. 1). Furthermore, the Begg’s line regression test did not indicate publication bias (z = 0.91, P = 0.363). Additionally, the sensitivity analysis did not identify any single study which significantly altered the effect size. Subgroup analyses indicated that the geographic region, the definition of RPL, whether the patients were matched for confounders, measurement timing, and the exclusion of known factors were not associated with between-study heterogeneity (Table 3).
FIN
FIN was measured in sixteen studies included in this review (Fig. 3). Our meta-analysis showed higher levels of FIN among RPL women compared to the control group (I2 = 94% [92%-96%]). The funnel plots showed possible asymmetry (Supplementary Fig. 2); however, the Begg’s line regression test did not indicate publication bias (z = 1.53, P = 0.125). Additionally, the sensitivity analysis did not identify any single study which altered the effect size. Subgroup analyses indicated that factors such as whether the patients were matched for confounders and the exclusion of known factors associated with RPL were correlated with between-study heterogeneity (P = 0.0009; P = 0.02) (Table 4).
HOMA-IR
The meta-analysis of eight studies revealed a significantly higher level of HOMA-IR in RPL patients compared to healthy controls (I2 = 85% [72%-92%]) (Fig. 4). The funnel plots showed no obvious asymmetry indicative of a lack of publication bias (Supplementary Fig. 3). The Egger’s line regression test did not indicate publication bias for HOMA-IR (t = 2.50, P = 0.054). Furthermore, the sensitivity analysis did not identify any single study which altered the effect size. Subgroup analyses indicated that the geographic region, the definition of RPL, whether the patients were matched for confounders, measurement timing, and the exclusion of known factors were not associated with between-study heterogeneity (Table 5).
GI ratio
The meta-analysis of five studies revealed a significantly lower GI ratio in RPL patients compared to the controls (I2 = 89% [77%-95%]) (Fig. 5). The funnel plots showed no obvious asymmetry indicative of a lack of publication bias (Supplementary Fig. 4). The Egger’s line regression test did not indicate publication bias (t = -0.93, P = 0.420). Additionally, the sensitivity analysis did not identify any single study which altered the effect size. Subgroup analyses indicated that the exclusion of known factors associated with RPL was associated with between-study heterogeneity (P < 0.00001) (Table 6).
IR status
The meta-analysis revealed a significantly higher rate of IR in RPL patients defined by abnormal HOMA-IR, abnormal GI ratio and abnormal FIN compared to healthy controls (Fig. 6). The funnel plots showed no obvious asymmetry indicative of a lack of publication bias (Supplementary Figs. 5, 6, 7). The Egger’s line regression test indicated no publication bias for IR when defined by abnormal HOMA-IR (t = -0.02, P = 0.986), abnormal GI ratio (t = 0.90, P = 0.533) and abnormal FIN (t = 0.50, P = 0.705). Subgroup analysis to assess the association between IR status and RPL was not performed due to the limited number of studies included.
Discussion
The data from this meta-analysis suggested that glucose metabolism was associated with RPL. RPL women had higher FBG, FIN, and HOMA-IR, and a lower GI ratio relative to healthy controls. Additionally, RPL women were observed to have a higher rate of IR status.
First, homocysteine (HCY) and folate have been hypothesized to influence RPL in recent years. In animal and human studies, it has been shown that IR is associated with HCY [41]. One meta-analysis found that high HCY levels and low folate levels were significantly associated with RPL risk [42]. HCY is thought to contribute to blood hypercoagulability [43]. Further, HCY has been shown to inhibit proliferation and promote inflammatory responses in endothelial cells, impair endothelial function, and cause vascular injury [44]. Nelen et al. found that elevated maternal HCY is associated with defective chorionic villous vascularization [45]. Additionally, Han et al. reported that the exposure of mouse embryos to HCY induced cardiac defects [46]. The authors concluded that HCY may, therefore, be toxic to the embryo. Together, these data indicate that the association between IR and RPL might partly be explained by HCY.
Second, the placenta serves as the main interface between the mother and the fetus and it is understood that peripheral IR status is changed during pregnancy [47]. This increase results in a higher concentration of circulating maternal lipids and amino acids, thus providing glucose and additional nutrients to the fetus via placental transfer and contributing to fetal growth. In obese women during early pregnancy, the human placenta is responsive to the high concentration of maternal insulin. In these cases, this responsiveness is attributed to altered gene expression due to modulated mitochondrial steroid hormone production and energy metabolism [48]. In such pregnancies, IR status may influence placental dysfunction and cause pregnancy loss; however, this needs to be confirmed.
Third, efficient vessel functioning is vital during normal pregnancy. During early human pregnancy, extravillous trophoblast cells from the placenta invade the uterine decidual spiral arterioles and mediate the vessel remodeling to ensure that low pressure, high blood flow can be supplied to the placenta [49]. The development of new blood vessels is also essential to promote ovarian folliculogenesis and functional corpus luteum formation [50]. Insulin is a vasoactive hormone, and evidence suggests that arterial endothelial dysfunction and IR usually coexist [51]. Together, these lines of evidence suggest that IR might disrupt vessel function during pregnancy and lead to pregnancy loss.
Furthermore, IR may impair the procedure from oocyte development to embryo development. IR is associated with decreased percentage of mature eggs and poor embryo quality in [52, 53]. IR may also contributes to oxidative stress and disrupts mitochondrial function in mouse oocytes [54]. High-fat diet- induced IR mouse models had deteriorated uterine receptivity and decreased implantation sites and fetal numbers [55].
Previous study has provided evidence supporting the association between IR and spontaneous pregnancy loss. Tian et al. suggested that IR was an independent risk factor for spontaneous abortion in women undergoing assisted reproduction [13]. From our review of the literature, more studies investigated the association between IR and miscarriage in women with PCOS. For example, a recent systematic review and meta-analysis revealed that IR is a risk factor for spontaneous abortion in PCOS patients who underwent assisted reproductive technology [16]. In agreement with these lines of evidence, the results of our study found that IR was associated with women with RPL.
Meanwhile, subgroup analyses showed that geographic region, whether the patients were matched for confounders, and whether the exclusion of known factors might have a significant influence on the association between IR and RPL. The differences observed for the geographic region may reflect ethnic heterogeneity. Matched confounders might have associations with IR and, therefore, influence the subgroup analysis. Additionally, our results indicate that the relationship between IR and RPL was stronger when excluding known factors of RPL, suggesting the possible role of IR in unexplained RPL.
Several factors might influence our results. First, not all confounders related to IR were fully adjusted for in the included studies. For example, the BMIs of all the women were not similar between the RPL and control women. Furthermore, additional confounders that may affect a person’s IR parameters, such as smoking [56] and lifestyle [57] were not evaluated in most studies.
In the current review, RPL women were found to be associated with IR. The screening and prevention of IR may provide health benefits for women with RPL. Al-Biate et al. reported that metformin therapy in pregnant women with PCOS was associated with a significant reduction in the rate of early pregnancy loss [58]. Furthermore, in a case report, metformin was shown to be effective in RPL women with IR and PCOS [59]. However, more prospective research is needed to assess if interventions to treat IR can bring long-term benefits to pregnancy outcomes for RPL women.
The search strategy and systematic methods, including quality assessment, publication bias assessment, subgroup analyses and sensitivity analyses are among the strengths of this study. Our study has several limitations. First, the sample size for some indices was relatively small. Most studies were case–control studies, and we are unable to fully access the causality between IR and RPL. Furthermore, the diagnostic criteria for RPL were heterogeneous between studies. Additionally, the quality of several of the studies was not enough. Lastly, some covariates that may affect IR status, such as smoking, lifestyle, were not evaluated.
In conclusion, women with RPL were associated with IR and impaired FBG, FIN, HOMA-IR, and GI ratios. Our study provides improved insight into the understanding of the pathophysiology of women suffering from RPL. The early screening and management of IR may help to improve the pregnancy outcomes of women with RPL and future studies are warranted to further explore the underlying mechanism between IR and RPL.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- RPL:
-
Recurrent pregnancy loss
- IR:
-
Insulin resistance
- PCOS:
-
Polycystic ovary syndrome
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- FBG:
-
Blood glucose
- FIN:
-
Fasting insulin
- HOMA-IR:
-
Homeostasis model assessment for insulin resistance
- GI ratio:
-
Glucose to insulin ratio
- NOS:
-
Newcastle–Ottawa scale
- MD:
-
Mean difference
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- HCY:
-
Homocysteine
References
El Hachem H, Crepaux V, May-Panloup P, Descamps P, Legendre G, Bouet P-E. Recurrent pregnancy loss: current perspectives. Int J Womens Health. 2017;9:331–45.
Sugiura-Ogasawara M, Ozaki Y, Katano K, Suzumori N, Kitaori T, Mizutani E. Abnormal embryonic karyotype is the most frequent cause of recurrent miscarriage. Hum Reprod. 2012;27(8):2297–303.
Jaslow CR, Carney JL, Kutteh WH. Diagnostic factors identified in 1020 women with two versus three or more recurrent pregnancy losses. Fertil Steril. 2010;93(4):1234–43.
Anselmo J, Cao D, Karrison T, Weiss RE, Refetoff S. Fetal loss associated with excess thyroid hormone exposure. JAMA. 2004;292(6):691–5.
Opatrny L, David M, Kahn SR, Shrier I, Rey E. Association between antiphospholipid antibodies and recurrent fetal loss in women without autoimmune disease: a metaanalysis. J Rheumatol. 2006;33(11):2214–21.
Liu X, Chen Y, Ye C, Xing D, Wu R, Li F, Chen L, Wang T. Hereditary thrombophilia and recurrent pregnancy loss: a systematic review and meta-analysis. Hum Reprod. 2021;36(5):1213–29.
Stefanidou EM, Caramellino L, Patriarca A, Menato G. Maternal caffeine consumption and sine causa recurrent miscarriage. Eur J Obstet Gynecol Reprod Biol. 2011;158(2):220–4.
Zhang B-Y, Wei Y-S, Niu J-M, Li Y, Miao Z-L, Wang Z-N. Risk factors for unexplained recurrent spontaneous abortion in a population from southern China. Int J Gynaecol Obstet. 2010;108(2):135–8.
Keenan K, Grundy E, Kenward MG, Leon DA. Women’s risk of repeat abortions is strongly associated with alcohol consumption: a longitudinal analysis of a Russian national panel study, 1994–2009. PLoS ONE. 2014;9(3): e90356.
Practice Committee of the American Society for Reproductive Medicine. Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril. 2012;98(5):1103–11.
Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd-Jones DM, Newby LK, Piña IL, Roger VL, Shaw LJ, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women–2011 update: a guideline from the american heart association. Circulation. 2011;123(11):1243–62.
Liang C, Chung H-F, Dobson AJ, Hayashi K, van der Schouw YT, Kuh D, Hardy R, Derby CA, El Khoudary SR, Janssen I, et al. Infertility, recurrent pregnancy loss, and risk of stroke: pooled analysis of individual patient data of 618 851 women. BMJ. 2022;377:e070603.
Tian L, Shen H, Lu Q, Norman RJ, Wang J. Insulin resistance increases the risk of spontaneous abortion after assisted reproduction technology treatment. J Clin Endocrinol Metab. 2007;92(4):1430–3.
Sharif YH. Serum leptin level-insulin resistance-based correlation in polycystic ovary syndrome obese and non-obese sufferer female. J Popul Ther Clin Pharmacol. 2022;29(2):e11–9.
Joham AE, Norman RJ, Stener-Victorin E, Legro RS, Franks S, Moran LJ, Boyle J, Teede HJ. Polycystic ovary syndrome. Lancet Diabetes Endocrinol. 2022;10(9):668–80.
Sun Y-F, Zhang J, Xu YM, Cao ZY, Wang YZ, Hao GM, Gao BL. High BMI and Insulin Resistance Are Risk Factors for Spontaneous Abortion in Patients With Polycystic Ovary Syndrome Undergoing Assisted Reproductive Treatment: A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne). 2020;11:592495.
Zhang D, Yang X, Li J, Yu J, Wu X. Effect of hyperinsulinaemia and insulin resistance on endocrine, metabolic and fertility outcomes in women with polycystic ovary syndrome undergoing ovulation induction. Clin Endocrinol (Oxf). 2019;91(3):440–8.
Kampmann U, Knorr S, Fuglsang J, Ovesen P. Determinants of Maternal Insulin Resistance during Pregnancy: An Updated Overview. J Diabetes Res. 2019;2019:5320156.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135.
The Newcastle-Ottawa scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses [http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp].
Azizi R, Soltani-Zangbar MS, Sheikhansari G, Pourmoghadam Z, Mehdizadeh A, Mandipour M, Sandoghchian S, Danaii S, Koushaein L, Kafil HS, et al. Metabolic syndrome mediates inflammatory and oxidative stress responses in patients with recurrent pregnancy loss. J Reprod Immunol. 2019;133:18–26.
Baban RS, Ali NM, Al-Moayed HA. Serum leptin and insulin hormone level in recurrent pregnancy loss. Oman Med J. 2010;25(3):203–7.
Bahia W, Soltani I, Haddad A, Radhouani A, Mahdhi A, Ferchichi S, Almawi WY. Contribution ofADIPOQVariants to the Genetic Susceptibility of Recurrent Pregnancy Loss. Reprod Sci. 2021;28(1):263–70.
Celik N, Evsen MS, Sak ME, Soydinc E, Gul T. Evaluation of the relationship between insulin resistance and recurrent pregnancy loss. Ginekol Pol. 2011;82(4):272–5.
Craig LB, Ke RW, Kutteh WH. Increased prevalence of insulin resistance in women with a history of recurrent pregnancy loss. Fertil Steril. 2002;78(3):487–90.
Diejomaoh M, Jirous J, Al-Azemi M, Gupta M, Al-Jaber M, Farhat R, Mohd A. Insulin resistance in women with recurrent spontaneous miscarriage of unknown aetiology. Med Princ Pract. 2007;16(2):114–8.
Edugbe AE, James B, Akunaeziri UA, Egbodo CO, Imoh CL, Ajen AS, John O, Samaila M. Beta-cell dysfunction and abnormal glucose metabolism among non-diabetic women with recurrent miscarriages. Arch Gynecol Obstet. 2020;301(2):559–64.
El-Dorf AA-E, Ossman AME, El-Halwagy AE-S, Borg HM, Abd-ElBar ES. Use of serum leptin and insulin hormones levels as predictors of pregnancy outcome in pregnant women with history of recurrent early pregnancy loss. Middle East Fertil Soc J. 2016;21(1):36–40.
Hong Y, Xie QX, Chen CY, Yang C, Li YZ, Chen DM, Xie MQ. Insulin resistance in first-trimester pregnant women with pre-pregnant glucose tolerance and history of recurrent spontaneous abortion. J Biol Regul Homeost Agents. 2013;27(1):225–31.
Ispasoiu C-A, Chicea R, Stamatian FV, Ispasoiu F. High Fasting Insulin Levels and Insulin Resistance May Be Linked to Idiopathic Recurrent Pregnancy Loss: A Case-Control Study. Int J Endocrinol. 2013;2013:576926.
Jiang S, He F, Gao R, Chen C, Zhong X, Li X, Lin S, Xu W, Qin L, Zhao X. Neutrophil and Neutrophil-to-Lymphocyte Ratio as Clinically Predictive Risk Markers for Recurrent Pregnancy Loss. Reprod Sci. 2021;28(4):1101–11.
Jiao Y, Zhao J, Hu B, La X, Gong X, Huang Y, Cai X, Zhang Y. Toll-like receptor 4 gene is associated with recurrent spontaneous miscarriage in Uygur and Han women in Xinjiang. Exp Ther Med. 2016;12(5):3268–74.
Kazerooni T, Ghaffarpasand F, Asadi N, Dehkhoda Z, Dehghankhalili M, Kazerooni Y. Correlation between thrombophilia and recurrent pregnancy loss in patients with polycystic ovary syndrome: a comparative study. J Chin Med Assoc. 2013;76(5):282–8.
Lin Z, Li Q, Sun Y, Huang J, Wang W, Fu J, Xu J, Zeng D. Interactions between genetic variants involved in the folate metabolic pathway and serum lipid, homocysteine levels on the risk of recurrent spontaneous abortion. Lipids Health Dis. 2019;18:143.
Maryam K, Bouzari Z, Basirat Z, Kashifard M, Zadeh MZ. The comparison of insulin resistance frequency in patients with recurrent early pregnancy loss to normal individuals. BMC Res Notes. 2012;5:133.
Ota K, Yamagishi S, Kim M, Dambaeva S, Gilman-Sachs A, Beaman K, Kwak-Kim J. Elevation of soluble form of receptor for advanced glycation end products (sRAGE) in recurrent pregnancy losses (RPL): possible participation of RAGE in RPL. Fertil Steril. 2014;102(3):782–9.
Wang Y, Zhao H, Li Y, Zhang J, Tan J, Liu Y. Relationship between recurrent miscarriage and insulin resistance. Gynecol Obstet Invest. 2011;72(4):245–51.
Habets DHJ, Schiffer VMMM, Kraneburg LPA, de Krom FJW, Gürtekin I, van Bree BE, van Golde RJT, Wieten L, Spaanderman MEA, Al-Nasiry S. Preconceptional evaluation of women with recurrent pregnancy loss: the additional value of assessing vascular and metabolic status. BMC Pregnancy Childbirth. 2022;22(1):75.
Singh H, Chitkara A, Puri M, Goswami B, Bhattacharjee J. Occurrence of Insulin Resistance with Recurrent Pregnancy Loss of Unknown Etiology in North Indian Hospital-based Women Population: A Pilot Study. Int J Infertil Fetal Med. 2022;13(1):15–7.
Zhang X, Qu Y-Y, Liu L, Qiao Y-N, Geng H-R, Lin Y, Xu W, Cao J, Zhao J-Y. Homocysteine inhibits pro-insulin receptor cleavage and causes insulin resistance via protein cysteine-homocysteinylation. Cell Rep. 2021;37(2):109821.
Diao J, Luo L, Li J, Zhang S, Li Y, Qin J. Maternal homocysteine and folate levels and risk of recurrent spontaneous abortion: a meta-analysis of observational studies. J Obstet Gynaecol Res. 2020;46:2461-73.
Hensen ADO, Lijfering WM, Cannegieter SC, Rosendaal FR, van Hylckama VA. Hyperhomocysteinaemia and the risk of recurrent venous thrombosis: results from the MEGA follow-up study. Br J Haematol. 2019;187(2):219–26.
Jan M, Cueto R, Jiang X, Lu L, Sardy J, Xiong X, Yu JE, Pham H, Khan M, Qin X, et al. Molecular processes mediating hyperhomocysteinemia-induced metabolic reprogramming, redox regulation and growth inhibition in endothelial cells. Redox Biol. 2021;45:102018.
Nelen WL, Bulten J, Steegers EA, Blom HJ, Hanselaar AG, Eskes TK. Maternal homocysteine and chorionic vascularization in recurrent early pregnancy loss. Hum Reprod. 2000;15(4):954–60.
Han M, Evsikov AV, Zhang L, Lastra-Vicente R, Linask KK. Embryonic exposures of lithium and homocysteine and folate protection affect lipid metabolism during mouse cardiogenesis and placentation. Reprod Toxicol. 2016;61:82–96.
Alvarado-Flores F, Kaneko-Tarui T, Beyer W, Katz J, Chu T, Catalano P, Sadovsky Y, Hivert M-F, O'Tierney-Ginn P: Placental miR-3940–3p is associated with maternal insulin resistance in late pregnancy. J Clin Endocrinol Metab. 2021;106:3526-35.
Catalano PM, Shankar K. Obesity and pregnancy: mechanisms of short term and long term adverse consequences for mother and child. BMJ. 2017;356:j1.
Chen JZJ, Sheehan PM, Brennecke SP, Keogh RJ. Vessel remodelling, pregnancy hormones and extravillous trophoblast function. Mol Cell Endocrinol. 2012;349(2):138–44.
Patil K, Hinduja I, Mukherjee S. Alteration in angiogenic potential of granulosa-lutein cells and follicular fluid contributes to luteal defects in polycystic ovary syndrome. Hum Reprod. 2021;36(4):1052–64.
Zheng C, Liu Z. Vascular function, insulin action, and exercise: an intricate interplay. Trends Endocrinol Metab. 2015;26(6):297–304.
Wang H, Zhang Y, Fang X, Kwak-Kim J, Wu L. Insulin Resistance Adversely Affect IVF Outcomes in Lean Women Without PCOS. Front Endocrinol (Lausanne). 2021;12:734638.
Cai WY, Luo X, Song J, Ji D, Zhu J, Duan C, Wu W, Wu XK, Xu J. Effect of Hyperinsulinemia and Insulin Resistance on Endocrine, Metabolic, and Reproductive Outcomes in Non-PCOS Women Undergoing Assisted Reproduction: A Retrospective Cohort Study. Front Med (Lausanne). 2021;8:736320.
Ou XH, Li S, Wang ZB, Li M, Quan S, Xing F, Guo L, Chao S-B, Chen Z, Liang XW, et al. Maternal insulin resistance causes oxidative stress and mitochondrial dysfunction in mouse oocytes. Hum Reprod. 2012;27(7):2130–45.
Chen M, Li J, Zhang B, Zeng X, Zeng X, Cai S, Ye Q, Yang G, Ye C, Shang L, et al. Uterine Insulin Sensitivity Defects Induced Embryo Implantation Loss Associated with Mitochondrial Dysfunction-Triggered Oxidative Stress. Oxid Med Cell Longev. 2021;2021:6655685.
Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2007;298(22):2654–64.
Akter S, Kurotani K, Nanri A, Pham NM, Sato M, Hayabuchi H, Mizoue T. Dairy consumption is associated with decreased insulin resistance among the Japanese. Nutr Res. 2013;33(4):286–92.
Al-Biate MAS. Effect of metformin on early pregnancy loss in women with polycystic ovary syndrome. Taiwan J Obstet Gynecol. 2015;54(3):266–9.
Palomba S, Falbo A, Orio F, Russo T, Tolino A, Zullo F. Metformin hydrochloride and recurrent miscarriage in a woman with polycystic ovary syndrome. Fertil Steril. 2006;85(5):1511.e1513-1511.e1515.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
JX designed the study and critically revised the manuscript. WYC and XL performed data analysis. WYC, XL, HYL, KYF collected data. WYC and XL drafted the manuscript. All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary table 1.
PRISMA checklist.
Additional file 2:
Supplementary Table 2. Search strategy.
Additional file 3: Supplementary Figure 1.
Funnel plot in the meta-analysis on the association of FBG between RPL and control group. Supplementary Figure 2. Funnel plot in the meta-analysis on the association of FIN between RPL and control group. Supplementary Figure 3. Funnel plot in the meta-analysis on the association of HOMA-IR between RPL and control group. Supplementary Figure 4. Funnel plot in the meta-analysis on the association of GI ratio between RPL and control group. Supplementary Figure 5. Funnel plot in the meta-analysis on the association of IR by abnormal HOMA-IR between RPL and control group. Supplementary Figure 6. Funnel plot in the meta-analysis on the association of IR by abnormal GI ratio between RPL and control group. Supplementary Figure 7. Funnel plot in the meta-analysis on the association of IR by abnormal FIN between RPL and control group.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cai, WY., Luo, X., Lv, HY. et al. Insulin resistance in women with recurrent miscarriage: a systematic review and meta-analysis. BMC Pregnancy Childbirth 22, 916 (2022). https://doi.org/10.1186/s12884-022-05256-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-05256-z