Abstract
Background
Although antenatal care has the potential role to reduce maternal and child morbidity and mortality, utilization of a recommended number of antenatal care visits is still low in Ethiopia. Therefore, this study aimed to assess the determinants of recommended antenatal care visits in Ethiopia.
Method
Data from the 2019 mini-Ethiopian demographic and health survey (MEDHS) was used for this study. A total of 3916 women who gave birth 5 years preceding the MEDHS were included. A generalized linear mixed-effects (mixed-effects logistic regression) model was used to identify the determinants of recommended antenatal care service utilization. Finally, the adjusted odds ratio with a 95% confidence interval and random effects were reported.
Results
In the generalized linear mixed-effects model, women with primary education (AOR = 1.55, 95%CI 1.22–2.01), secondary and above education (AOR = 5.12, 95%CI 2.80–8.16), women from the middle (AOR = 1.25, 95%CI 1.01–1.71) and rich wealth index (AOR = 1.54, 95%CI 1.12–2.25), women who were exposed to media (AOR = 1.23,95%CI 1.01–1.57) and who use contraception (AOR = 1.45 95%CI 1.25–2.03), had higher odds of recommended antenatal care service utilization.
Conclusion
In this study, factors like maternal educational status, media exposure, wealth index and history of contraceptive utilization were significantly associated with recommended ANC visits in Ethiopia. Therefore, encouraging women for contraceptive service utilization, consulting women to be exposed to media and improving women’s wealth status will help to have recommended number of ANC visits by pregnant women in Ethiopia.
Similar content being viewed by others
Background
Antenatal care (ANC) is healthcare service provided to pregnant women at health institution by skilled healthcare providers. It is provided throughout pregnancy to ensure better maternal and neonatal outcomes through risk identification, prevention and management of pregnancy-related or concurrent diseases [1]. It has the potential role to reduce maternal and neonatal morbidity and mortality and then improve neonatal and maternal health [2,3,4,5,6]. The ANC visit reduces the risk of neonatal mortality by 34% in sub-Saharan Africa [5]. Similarly, having adequate number of ANC visits reduces occurrence of maternal and neonatal complications. For instance, having four or more ANC visits can reduce about 81.2, 61.3, 52.4 and 46.5% risk of having postpartum hemorrhage, early neonatal death, preterm labor and low-birth-weight, respectively [6]. In general, having adequate antenatal care visits is best strategy to minimize the adverse pregnancy outcomes [7].
Globally, about 90% of pregnant women access antenatal care with skilled health personnel at least once and 57% receive at least four antenatal care visits. In countries with the highest rates of maternal mortality, like Africa and Asia, even fewer women received at least four antenatal care visits, 53 and 49% respectively [8, 9]. Lack of relevant and high-quality antenatal care services is a major concern in sub-Saharan Africa [10].
Ethiopia is part of sub-Saharan African countries and one of the countries with the highest maternal mortality ratios in developing countries [9]. The main causes of maternal mortality in Ethiopia include postpartum hemorrhage, sepsis, pre-eclampsia, eclampsia and birthing complications [11]. Even if most of these causes are preventable, many women often do not have access to evidence-based interventions such as antenatal care (ANC) services during pregnancy, due to poverty, lack of information, and cultural practices [12]. According to recent evidence from the Mini Ethiopian demographic health survey, only 43% of pregnant women had attended at list four ANC visits [13]. Thus, having antenatal care visits at recommended level (at least four visits during pregnancy) is still a major concern in Ethiopia.
In the previous studies, education level, employment status, marital status [14,15,16], ,occupation, residence, distance to the health facility [17], age, residence parity, and geographic location were identified as determinants of recommended ANC visits [15, 18,19,20]. However, the previous studies used traditional models and fail to account the random effects on the outcome variable. Generalized linear mixed effects model is a robust model which produces the reliable estimates for fixed effects by adjusting random effects [21, 22]. As to our knowledge, previously there is limited evidence on determinants of recommended ANC visits in Ethiopia using this advanced robust statistical method. Besides, unlike that of pocket studies in Ethiopia [23,24,25] at different sub regions, this study provides policy level understanding of determinants of recommended ANC visit through analysis of data with national coverage. Therefore, we aimed to assess determinants of recommended antenatal care visits in Ethiopia through mixed effects modeling. This study produced valuable evidence for policy makers and program designers working on maternal and child health by supplementing and filling the gaps in the existing body of literatures.
Method
Data source, study design and setting
This study analyzed data from the 2019 Mini–Ethiopian Demographic and Health Survey (MEDHS) which is part of the worldwide MEASURE DHS project. Data was downloaded from the Measure DHS website through reasonable request after data use permission was fully guaranteed.
Sample size and sampling procedure
The Mini Ethiopian Demographic and Health Survey program (EDHS) had collected data on national representative samples of all age groups and key indicators including ANC utilization. The information on the sociodemographic, socioeconomic, and maternal-related variables was also included in the survey.
A stratified two-stage cluster sampling procedure was employed to select study participants. In the 2019 MEDHS survey, a total of 305 EAs (93 urban and 212 rural) were selected. From these enumeration areas, 149,093 households and from those households a total of 8885 reproductive-age women were included in the survey. The relevant information on the sampling procedure and data quality can be accessed elsewhere [9]. For the current study, a total of 3916 pregnant women/who gave birth in 5 years preceding the Mini Ethiopian demographic and health survey 2019 were included. The sampling weight was applied during the analysis to produce reliable estimates [26].
Dependent variable
The dependent variable for this study was recommended ANC visits which was defined as having at list four ANC visits during pregnancy. It was coded “1” for a woman who had four and above antenatal care visits,otherwise “0” [27].
Independent variables
After reviewing literature, educational status of mother (no formal education, primary, secondary and higher), maternal age (15–24, 25–29,30-34,35-39,40–49), parity (primipara, multipara, grand multipara), wealth status (poor, middle, rich), number of children, birth order, contraceptive utilization, media exposure (no, yes), place of residency (urban, rural) and the region which was categorized into urban (Addis Ababa, Dire Dawa, Harari), agrarian (Tigray, Amhara, Oromia and south nation nationality and peoples region) and pastoral (Somali, Afar, Gambela and Benishangul Gumuz) were considered as determinants of recommended ANC visits.
Data management and method of analysis
Data Extraction, recoding, and both descriptive and analytical analysis were carried out using STATA version 14 software. Weighting was done to restore the representativeness of the sample. Descriptive analysis was conducted and frequencies with percentages were reported. The Generalized mixed-effects analysis was fitted after checking the intracluster correlation coefficient to adjust for random effects and produce reliable estimates. Nonlinear mixed effects modeling (mixed effects logistic regression model) was employed since the dependent variable had binary outcome.
The odds ratio was used to estimate the association between the fixed effects and the likelihood of recommended ANC visits which were expressed at a 95% confidence level. Regarding the measures of variation (random effects) intracluster correlation coefficient (ICC) and median odds ratio were reported.
Results
Sociodemographic characteristics of study participants
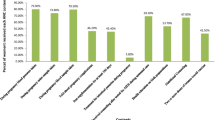
In this study, a total of 3916 women who gave birth 5 years preceding the MEDHS were included. More than half of (51.33%) of respondents had no formal education. The majority (63.70%) of respondents were exposed to media and nearly half (50.39%) of them were from poor households. Moreover, about 93.85 and 74% of participants were married and rural dwellers respectively. The majority of (55%) respondents didn’t use any contraceptive methods (Table 1).
Random effect analysis
In the null model, variance component analysis was performed to decompose the total variance of recommended antenatal care visits. The applicability of mixed effects analysis instead of the traditional logistic regression model was justified by the significance of the community variance [community variance = 3.06; standard error (SE) = 0.31; P-value = 0.001) and intracluster correlation coefficient (ICC). The ICC in the null model indicated that about 49% of the variation of recommended ANC visits was attributed to the random effects which need to be adjusted during modeling. Moreover, the MOR was 5.25 (MOR = 5.25, 95%CI 4.48–11.70) which implied that the odds of utilizing recommended ANC visit 5.25 times higher when mothers moved from high-risk communities to low-risk ones (Table 2).
Factors associated with recommended ANC utilization
In the mixed-effects logistic regression analysis, educational status, media exposure, wealth status, and contraceptive use were significantly associated with recommended ANC visits (p < 0.05).
The odds of having recommended ANC visits among women with primary and above primary education was 1.55 (AOR = 1.55, 95%CI 1.22–2.01) and 5.12 (AOR = 5.12, 95%CI 2.80–8.16) respectively times higher as compared to women with no formal education. Women from households with middle and rich wealth index had 25% (AOR = 1.25, 95%CI 1.01–1.71) and 54% (AOR = 1.54, 95%CI 1.12–2.25) increased odds of having recommended ANC visits as compared to those women from poor households. The likelihood of recommended ANC visits among women who were exposed to media was 1.23 (AOR = 1.23,95%CI 1.01–1.57) times higher as compared to unexposed women. The odds of having recommended ANC visits among women who had history of contraceptive use was increased by 45% (AOR = 1.45 95%CI 1.25–2.03) as compared to women who didn’t have history of contraceptive use (Table 2).
Discussion
This study aimed to assess the association between demographic, socioeconomic, and health care access-related factors with recommended ANC visits in Ethiopia. The odds of having recommended ANC visits among educated women was higher as compared to women with no formal education. This finding was supported by studies done in Nepal [28], East Africa [29] and Ethiopia [11, 30]. The possible explanation might be due to that educated women mostly live in urban Areas which helps them to easily access health institutions for service utilization [31]. Besides, women’s education helps to develop economic and decision-making power which will in turn improve maternal health service utilization [32].
Similarly, women from households with middle and rich wealth index had increased odds of having recommended ANC visits as compared to those women from poor households. This finding was similar to studies done in Georgia [33], India [34] and Ghana [15]. This might be due to the difficulty that women in poor households face to handle transportation and other healthcare-seeking costs [35]. Women with low economic status commonly show poor health care-seeking behavior and then poor health outcomes [36].
The likelihood of having recommended ANC visits among women who were exposed to media was higher as compared to unexposed women. This finding was consistent with studies done in Nepal [28], Bangladesh [37], Uganda [38] and Ethiopia [30]. This might be due to that media has a positive impact on safe motherhood for giving health promotion. Media also helps to develop health-seeking behavior and health care service utilization of women [39].
History of contraceptive utilization is also an important determinant of recommended ANC visit. The odds of recommended ANC visits among women with history of contraceptive use was increased as compared to women who didn’t use any contraceptive methods. This finding was similar to studies done in Tajikistan [40], Liberia [41] and Ethiopia [11]. The reason might be that the integration of family planning and other maternal health services might have given women an increased chance to have good awareness about ANC visits [42]. It might have also provided an opportunity for counseling which could avoid social barriers and encourage the ANC service utilization [38]. Besides, women’s contraceptive choice and utilization increases women’s autonomy in health-care-seeking decisions [43].
The strength of this study was that it applied the sampling weight to produce reliable estimates and used advanced model for analysis. However, due to the cross-sectional nature of the data temporal relationship between explanatory and outcome variable couldn’t be established.
Conclusion
In this study, different factors like maternal educational status, media exposure, wealth index and history of contraceptive use were significantly associated with recommended ANC visits in Ethiopia. Therefore, encouraging women for contraceptive service utilization and consulting them to access media and improving women’s wealth status through economic and social empowerment will help to enable them to have recommended ANC visits during pregnancy in Ethiopia.
Availability of data and materials
All relevant data are available and not owned by third body. The dataset analyzed during the current study is available from the corresponding author on reasonable request.
Abbreviations
- ANC:
-
Antenatal Care
- AOR:
-
Adjusted Odds Ratio
- CSA:
-
Central Statistical Agency
- EAs:
-
Enumeration Areas
- MEDHS:
-
Mini Ethiopia Demographic and Health Survey
- SNNP:
-
South Nation Nationality and People
- WHO:
-
World Health Organization
References
Organization WH. WHO recommendations on antenatal care for a positive pregnancy experience: world health Organization; 2016.
Carroli G, Rooney C, Villar J. How effective is antenatal care in preventing maternal mortality and serious morbidity? An overview of the evidence. Paediatr Perinat Epidemiol. 2001;15:1–42.
Campbell OM, Graham WJ, group LMSSs. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368(9543):1284–99.
Kuhnt J, Vollmer S. Antenatal care services and its implications for vital and health outcomes of children: evidence from 193 surveys in 69 low-income and middle-income countries. BMJ Open. 2017;7(11):e017122.
Wondemagegn AT, Alebel A, Tesema C, Abie W. The effect of antenatal care follow-up on neonatal health outcomes: a systematic review and meta-analysis. Public Health Rev. 2018;39(1):1–11.
Haftu A, Hagos H, Mehari M-A. Pregnant women adherence level to antenatal care visit and its effect on perinatal outcome among mothers in Tigray public health institutions, 2017: cohort study. BMC Res Notes. 2018;11(1):1–6.
Mpembeni RN, Killewo JZ, Leshabari MT, Massawe SN, Jahn A, Mushi D, et al. Use pattern of maternal health services and determinants of skilled care during delivery in southern Tanzania: implications for achievement of MDG-5 targets. BMC Pregnancy Childbirth. 2007;7(1):1–7.
Nations U. The millennium development goals report. New York: United Nations; 2015.
Csa I. Central statistical agency (CSA)[Ethiopia] and ICF. In: Ethiopia demographic and health survey, Addis Ababa, Ethiopia and Calverton, Maryland, USA; 2016.
Conrad P, Schmid G, Tientrebeogo J, Moses A, Kirenga S, Neuhann F, et al. Compliance with focused antenatal care services: do health workers in rural Burkina Faso, Uganda and Tanzania perform all ANC procedures? Tropical Med Int Health. 2012;17(3):300–7.
Mekonnen T, Dune T, Perz J, Ogbo FA. Trends and determinants of antenatal care service use in Ethiopia between 2000 and 2016. Int J Environ Res Public Health. 2019;16(5):748.
Tessema GA, Laurence CO, Melaku YA, Misganaw A, Woldie SA, Hiruye A, et al. Trends and causes of maternal mortality in Ethiopia during 1990–2013: findings from the global burden of diseases study 2013. BMC Public Health. 2017;17(1):1–8.
ICF. CICsaCEa. Mini Ethiopian demographic and health survey. Addis Ababa, Ethiopia and Calverton, Maryland, USA, 2019.
Ataguba JE-O. A reassessment of global antenatal care coverage for improving maternal health using sub-Saharan Africa as a case study. PLoS One. 2018;13(10):e0204822.
Sakeah E, Okawa S, Rexford Oduro A, Shibanuma A, Ansah E, Kikuchi K, et al. Determinants of attending antenatal care at least four times in rural Ghana: analysis of a cross-sectional survey. Glob Health Action. 2017;10(1):1291879.
Okedo-Alex IN, Akamike IC, Ezeanosike OB, Uneke CJ. Determinants of antenatal care utilisation in sub-Saharan Africa: a systematic review. BMJ Open. 2019;9(10):e031890.
Atuhaire S, Mugisha J. Determinants of antenatal care visits and their impact on the choice of birthplace among mothers in Uganda: a systematic review. Obstet Gynecol Int J. 2020;11(1):77–81.
Emelumadu O, Ukegbu A, Ezeama N, Kanu O, Ifeadike C, Onyeonoro U. Socio-demographic determinants of maternal health-care service utilization among rural women in Anambra state, south East Nigeria. Ann Med Health Sci Res. 2014;4(3):374–82.
Tarekegn SM, Lieberman LS, Giedraitis V. Determinants of maternal health service utilization in Ethiopia: analysis of the 2011 Ethiopian demographic and health survey. BMC Pregnancy Childbirth. 2014;14(1):1–13.
Pandey S, Karki S. Socio-economic and demographic determinants of antenatal care services utilization in Central Nepal. Int J MCH AIDS. 2014;2(2):212.
Olofsen E, Dinges DF, Van Dongen H. Nonlinear mixed-effects modeling: individualization and prediction. Aviat Space Environ Med. 2004;75(3):A134–A40.
Jiang J, Nguyen T. Linear and generalized linear mixed models and their applications: Springer; 2007.
Birmeta K, Dibaba Y, Woldeyohannes D. Determinants of maternal health care utilization in Holeta town, Central Ethiopia. BMC Health Serv Res. 2013;13(1):1–10.
Wilunda C, Quaglio G, Putoto G, Takahashi R, Calia F, Abebe D, et al. Determinants of utilisation of antenatal care and skilled birth attendant at delivery in south west Shoa zone, Ethiopia: a cross sectional study. Reprod Health. 2015;12(1):1–12.
Gebrekirstos LG, Wube TB, Gebremedhin MH, Lake EA. Magnitude and determinants of adequate antenatal care service utilization among mothers in southern Ethiopia. PLoS One. 2021;16(7):e0251477.
Institute EPH. Mini demographic and health survey. 2019.
Ministry of health-Ethiopia. Management protocol on selected obstetrics topics for hospitals. 2020.
Neupane B, Rijal S, Gc S, Basnet TB. Andersen’s model on determining the factors associated with antenatal care services in Nepal: an evidence-based analysis of Nepal demographic and health survey 2016. BMC Pregnancy Childbirth. 2020;20:1–11.
Tessema ZT, Minyihun A. Utilization and determinants of antenatal care visits in east African countries: a multicountry analysis of demographic and health surveys. Advances. Public Health. 2021;2021.
Tsegaye B, Ayalew M. Prevalence and factors associated with antenatal care utilization in Ethiopia: an evidence from demographic health survey 2016. BMC Pregnancy Childbirth. 2020;20(1):1–9.
Adewuyi EO, Auta A, Khanal V, Bamidele OD, Akuoko CP, Adefemi K, et al. Prevalence and factors associated with underutilization of antenatal care services in Nigeria: a comparative study of rural and urban residences based on the 2013 Nigeria demographic and health survey. PLoS One. 2018;13(5):e0197324.
Verney A, Reed BA, Lumumba JB, Kung'u JK. Factors associated with socio-demographic characteristics and antenatal care and iron supplement use in Ethiopia, Kenya, and Senegal. Maternal Child Nutr. 2018;14:e12565.
Miteniece E, Pavlova M, Shengelia L, Rechel B, Groot W. Barriers to accessing adequate maternal care in Georgia: a qualitative study. BMC Health Serv Res. 2018;18(1):1–12.
Kumar G, Choudhary TS, Srivastava A, Upadhyay RP, Taneja S, Bahl R, et al. Utilisation, equity and determinants of full antenatal care in India: analysis from the National Family Health Survey 4. BMC Pregnancy Childbirth. 2019;19(1):1–9.
Tekelab T, Chojenta C, Smith R, Loxton D. Factors affecting utilization of antenatal care in Ethiopia: a systematic review and meta-analysis. PLoS One. 2019;14(4):e0214848.
Shahrawat R, Meitei M, Joon V. Socio-economic disparity in care-seeking behaviours for ante-natal care and pregnancy complications among Indian women. Health Popul. 2014;1:27–39.
Islam MR, Odland JO. Determinants of antenatal and postnatal care visits among indigenous people in Bangladesh: a study of the Mru community; 2011.
Edward B. Factors influencing the utilisation of antenatal care content in Uganda. Australas Med J. 2011;4(9):516.
Mkandawire P. Gestational age at first antenatal care visit in Malawi. Matern Child Health J. 2015;19(11):2366–74.
Habibov N, Zainiddinov H. Do family planning messages improve antenatal care utilization? Evidence from Tajikistan. Sex Reprod Healthc. 2017;13:29–34.
Blackstone SR. Evaluating antenatal care in Liberia: evidence from the demographic and health survey. Women Health. 2019;59(10):1141–54.
Seiber EE, Hotchkiss DR, Rous JJ, Berruti AA. Maternal and child health and family planning service utilization in Guatemala: implications for service integration. Soc Sci Med. 2005;61(2):279–91.
Zhang Z, Cunningham K, Adhikari RP, Yogi S, Manandhar S, Rana PP, et al. Maternal decision-making input and health-seeking behaviors between pregnancy and the Child’s second birthday: a cross-sectional study in Nepal. Matern Child Health J. 2020;24(9):1121–9.
Acknowledgments
The authors would like to thank measure DHS for their permission to access the MEDHS datasets.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
HGA, KTA and AML are involved in the design and conception of the study, data analysis, interpretation, and write-up of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from institutional review board of wollo university to conduct this study. Permission for MEDHS data access was also obtained from International Review Board of Demographic and Health Surveys (DHS) program. All ethical procedures were performed in accordance with declaration of Helsinki guidelines. An informed consent was obtained from all literate participants above 15 years of age and from their legal guardians / parents of all illiterates as part of standard ethical review process of demographic and health survey. For this study, secondary data that hasn’t any personal identifying information linked to study participants was downloaded. No information obtained from the data set was disclosed to any third body.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ayalew, H.G., Asefa, K.T. & Liyew, A.M. Determinants of recommended antenatal care visits among pregnant women in Ethiopia: a generalized linear mixed-effects modeling. BMC Pregnancy Childbirth 22, 867 (2022). https://doi.org/10.1186/s12884-022-05213-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-05213-w