Abstract
Background
Information on the frequency and clinical features of advanced HIV disease (AHD) in pregnancy and its effects on maternal and perinatal outcomes is limited. The objective of this study was to describe the prevalence and clinical presentation of AHD in pregnancy, and to assess the impact of AHD in maternal and perinatal outcomes in Mozambican pregnant women.
Methods
This is a prospective and retrospective cohort study including HIV-infected pregnant women who attended the antenatal care (ANC) clinic at the Manhiça District Hospital between 2015 and 2020. Women were followed up for 36 months. Levels of CD4 + cell count were determined to assess AHD immune-suppressive changes. Risk factors for AHD were analyzed and the immune-suppressive changes over time and the effect of AHD on pregnancy outcomes were assessed.
Results
A total of 2458 HIV-infected pregnant women were enrolled. The prevalence of AHD at first ANC visit was 14.2% (349/2458). Among women with AHD at enrolment, 76.2% (260/341) were on antiretroviral therapy (ART). The proportion of women with AHD increased with age reaching 20.5% in those older than 35 years of age (p < 0.001). Tuberculosis was the only opportunistic infection diagnosed in women with AHD [4.9% (17/349)]. There was a trend for increased CD4 + cell count in women without AHD during the follow up period; however, in women with AHD the CD4 + cell count remained below 200 cells/mm3 (p < 0.001). Forty-two out of 2458 (1.7%) of the women were severely immunosuppressed (CD4 + cell count < 50 cells/mm3). No significant differences were detected between women with and without AHD in the frequency of maternal mortality, preterm birth, low birth weight and neonatal HIV infection.
Conclusions
After more than two decades of roll out of ART in Mozambique, over 14% and nearly 2% of HIV-infected pregnant women present at first ANC clinic visit with AHD and severe immunosuppression, respectively. Prompt HIV diagnosis in women of childbearing age, effective linkage to HIV care with an optimal ART regimen and close monitoring after ART initiation may contribute to reduce this burden and improve maternal and child survival.
Similar content being viewed by others
Background
Prevalence of HIV infection (13.2%) in Mozambique continues being one of the highest worldwide [1]. Women living with HIV outnumbers men living with HIV; in some areas up to 30% of pregnant women attending antenatal care (ANC) clinics are HIV-infected [2, 3] while the rate of vertical transmission remains high across the country (13.4%) [4]. Efforts have been mounted in the last years to control the HIV epidemic. Significantly, the implementation of the Option B + in 2013 that includes provision of lifelong antiretroviral therapy (ART) to all HIV-infected pregnant and lactating women [5,6,7]. As a result, the number of HIV-infected individuals receiving ART has increased (1.402.902 people by December 2020), and the proportion of patients with advanced HIV disease (AHD) has significantly decreased from 73% in 2004 to 37% in 2014 [4, 8].
Despite these positive achievements, the high frequency of AHD among infected individuals is an important public health issue due to its high burden on the health system and the society as a whole, likely jeopardizing the achievement of the UNAIDS 95–95-95 targets in Mozambique [9]. Patients with AHD are at high risk of death from opportunistic infections (mostly tuberculosis, severe bacterial infections, and cryptococcal meningitis) [10, 11] even if they are on ART, and this risk increases with the reduction in CD4 cell count [12].
Previous studies on the burden of AHD in Mozambique were conducted in the general population focusing on the frequency of AHD at ART initiation [13]. No published information exists in the country on the burden and clinical presentation of AHD in pregnant women at ANC enrolment, which is critical to guide care management in this particularly vulnerable population. HIV infection in pregnancy is a well-known risk factor for poor pregnancy outcomes [14, 15]. In the absence of ART, HIV-infected pregnant women have eight times higher risk of maternal mortality than HIV-uninfected women [16,17,18]. Additionally, there is limited information on the duration of the immune-suppressive status in the post-partum period in women with AHD [18,19,20], and even less data on the effects of AHD on pregnancy outcomes, in Mozambique and in other southern African countries where the burden of the HIV epidemic is also high.
The objective of this study was to describe, in a rural area of southern Mozambique, the proportion of pregnant women presenting with AHD at first ANC clinic visit, its clinical presentation, risk factors for AHD, the immune-suppressive changes over time and the effects of AHD on pregnancy outcomes.
Methods
Study area
The study was conducted in Manhiça District, located 80 km north of the capital Maputo. The Centro de Investigação em Saúde de Manhiça (CISM) runs a Demographic and Health Surveillance System (DHSS) since 1996 [21]. There are twenty-one health centers in the District, one rural hospital and one referral District hospital, Manhiça District Hospital (MDH). The area is endemic for malaria [22, 23]. The HIV prevalence in women attending the ANC clinics was estimated to be 29% in 2010 and 23% in 2021 (3, Nhampossa et al., unpublished).
HIV control program in Mozambique
At first diagnosis, HIV-infected individuals are registered in the HIV National Program Registry and receive a unique numeric identifier (NID), which allows patient tracking throughout the continuum of care [24]. A blood sample for CD4 + cell count is collected at diagnosis and repeated only if therapeutic failure is suspected, while HIV viral load is measured six months after ART initiation [25]. First line ART in adults consisting of tenofovir (TDF) /lamivudine (3TC) /efavirenze (EFV) or zidovudine (AZT) /3TC /nevirapine (NVP) and second line consisting of AZT /3TC /lopinavir-ritonavir (LPV/r) or abacavir (ABC) /3TC /LPVr were administered until 2019, transitioning to TDF + 3TC + dolutegravir (DTG) since then [26, 27]. All pregnant women attending the first ANC clinic are offered HIV testing. If the HIV test result is negative, then HIV testing is repeated every three months until the end of breastfeeding. If the HIV test is positive, prevention of mother to child transmission (PMTCT) of HIV with antiretroviral (ARV) drugs is provided on a monthly basis throughout pregnancy and breastfeeding. Cotrimoxazole prophylaxis (CTXp) is also given during pregnancy to HIV-infected women and continued until cessation of breastfeeding, regardless of the CD4 + cell count. Furthermore, tuberculosis prophylaxis with isoniazid is administered to the mother if she has not received it before or during pregnancy. Case management continues at the integrated chronic disease clinic after the end of pregnancy. Monthly clinical follow up of children born to HIV-infected women starts at one month of age to assess HIV infection status and nutritional and psychomotor development, and it ends three months after weaning, when the last HIV PCR is done. HIV-exposed infants receive ARV (AZT plus NVP) prophylaxis from birth up to 12 weeks of age together with CTXp beginning at four weeks of age. If HIV infection is confirmed in the infant, ART is initiated and CTXp maintained.
Study design
This is a prospective and retrospective cohort study nested in the International Epidemiological Databases to Evaluate AIDS in Southern Africa (IeDEA-SA Platform), including an observational cohort of HIV-exposed and infected children and their mothers who were registered at the MDH [28]. Clinical information for the period prior to 2013 was retrieved from the clinical files, while from 2013 onwards prospectively collected during the ANC visit. All HIV-infected pregnant women living in the Manhiça’s DHSS area, enrolled at the MDH-ANC clinic and who consented to be included in the study from January 2015 to March 2020 were included and followed up for 36 months and their children for a month. The CISM DHSS and the ePTS (MoH electronic HIV patient tracking systems) databases were used to retrieve information on participant’s vital status and their CD4 + cell count over time, respectively.
Definitions
Advanced HIV disease was defined as a CD4 + cell count < 200 cells/mm3 and/or WHO clinical stage III-IV. Severely immunosuppression was defined as a CD4 + cell count < 50cells/mm3 [12]. The value of the CD4 count at each time point of interest (6, 12, 18, 24, and 36 months) was estimated with the closest CD4 count value within ± 3 months of the time point of interest.
A difference in CD4 + cell count of 25 cells/mm3 between two measurements performed at an interval of about six months was considered clinically significant [29, 30]. Less than expected improvement in the CD4 + cell count was defined when the difference between two measurements performed at an interval of about six months was < 25 cells/mm3. Maternal education level was stratified into two groups, namely, no formal education (no education or did not complete primary education) and some formal education (at least completed primary education). Maternal underweight was defined as a body mass index (BMI) lower than 18.5, calculated from the women’s weight in kilograms divided by the square of her height in meters (kg/m2) [31]; anemia was defined as a hemoglobin concentration lower than 11 g/dL [32]; and the late postpartum period up as six weeks postpartum [33]. Preterm birth was defined as a gestational age at birth less than 37 weeks and low birth weight as a weight less than 2500 g [34].
Statistical analysis
Analyses were conducted using Stata® software (version 14.0) (StataCorp LP, College Station, TX, USA). A descriptive analysis was performed with frequencies and percentages. Differences in the distribution of socio-demographic, clinical variables, and pregnancy and perinatal outcomes between pregnant women with and without AHD were assessed with the Fisher’s exact test for categorical variables and Mann–Whitney U test for continuous variables. Description of immune-suppressive changes included variation in CD4 + cell count median over time, the calculation of the difference of CD4 + cell count between visits and frequencies of women with less than expected improvement in the CD4 + cell count over time. The Jonckheere-Terpstra statistical test was used to assess trend of CD4 count over time (months after 1st ANC visit). The difference of CD4 + cell count between the first antenatal visit and six-month visit, and between the first antenatal and 12-months visit for all the pregnant women (total and stratified by AHD and without AHD) was calculated and summarized with the mean and a 95% confidence interval. Logistic regression was performed to evaluate: a) the association between AHD proportion and visit year and b) the factors associated with the two main outcomes: AHD at the first ANC visit and “less than expected improvement in the CD4 + cell count” in the postpartum visit. The adjustment covariates included in logistic regression analysis were those previously described in the literature [29, 30, 35, 36], i.e., age group, gestational age, ART at first ANC visit, ART regimen, body mass index and gravidity for AHD at the first ANC visit, and age group, gestational age, time on ART, WHO clinical stage and AHD for “less than expected improvement in the CD4 cell count” in the postpartum visit. Death rates were calculated and compared using a time-to-event analysis (Kaplan–Meier plot) and the p-value from long-rank test used to compare the two survival curves). Due to the large amount, the missing values were imputed using the Multivariate Imputation by Chained Eqs. [37]. Logistic regression was used to impute binary variables and polytomous logistic regression was used for categorical variables with more than two categories. No numeric variable needed imputation. A two-sided p-value < 0.05 was considered to indicate statistical significance in all the study analysis.
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki and the National Bioethics Committee of Mozambique approved the study protocol in 2011 (327/CNBS/11), followed by subsequent annual renewals until the year 2020. After informing the pregnant women about the study objectives and methods, women consented for their participation, and that of their children, by signing a written informed consent. One copy of the consent form was handled to the participant.
Results
Frequency and temporal trends of advanced HIV disease
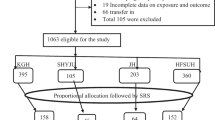
Out of 2458 HIV-infected pregnant women who attended the first ANC clinic between 2015 and 2020, 349 (14.2%) presented with AHD (Fig. 1). Of them, 214 (61.3%) had a CD4 + cell count of < 200 cells/mm3, 124 (35.5%) were on WHO clinical stage III-IV, and 11 (3.2%) had both a CD4 + cell count of < 200 cells/mm3 plus WHO clinical stage III-IV. Forty-two (1.7%) women were severely immunosuppressed (< 50cells/mm3). No significant differences were detected in the annual proportion of women enrolling ANC with AHD over the five-year study period (p = 0.070) (Fig. 2).
Characteristics of participants and risk factors for advanced HIV disease at first antenatal care clinic visit
Socio-demographic and clinical characteristics of enrolled women at first ANC clinic visit are shown in Table 1 according to AHD status. Pregnant women with AHD were significantly older than those without AHD (median age 30 versus 27 years, p < 0.001). The proportion of women with AHD increased with age, being 10.6% (25/236) for women aged < 20, 12.1% (73/601) for women aged 20–24, 13.9% (182/1314) for women aged 25–34 and 22.5% (69/307) for women older than35 years (p = < 0.001). Median of CD4 + cell counts was 166 cells/mm3 (IQR: 97–477) and 548 cells/mm3 (IQR: 386–758) in women with and without AHD, respectively (p < 0.001). Women with AHD had been on ART for longer time than women without AHD (22.4 months versus 12.9; p < 0.001). Most [76.2% (32/42)] of severely immunosuppressed pregnant women were already on ART. Among women who were not on ART at first ANC visit, 14.5% (89/610) presented with AHD. The proportion of women receiving the AZT/3TC/NVP regimen was higher in those with AHD than in those without it [36 (10.9% (36/331) versus 3.6% (71/1991); p < 0.001]. The frequency of women on TB prophylaxis was significantly lower among those with AHD than in women without it [33.8% (118/349) versus 41.6% (878/2109); p = 0.006]. Tuberculosis was the only opportunistic infection diagnosed in women with AHD [4.9% (17/349)]. There were no differences in women’s educational level, marital status and gestational age by AHD diagnosis.
Independent risk factors for presenting AHD at first ANC clinic are shown in Table 2. After adjusting for covariates, the odds of AHD increased with age compared to women aged < 20 (p = 0.029) (aOR = 1.35, 95% CI: 0.66; 2.76 in women aged 20–24), (aOR = 1.87, 95% CI: 0.97; 3.60 in women aged 25–34) and (aOR = 2.52; 95% CI: 1.21; 5.25 in women aged > 35 years). The odds of AHD were higher among women receiving the AZT/3TC/NVP regimen (aOR = 3.29, 95% CI: 1.91; 5.67) and AZT/ 3TC / LPV/r or ABC regimen (aOR = 8.59, 95% CI: 2.56; 28.85; p = < 0.001) compared to women on the TDF/3TC/EFV regimen. The Multivariate Imputation by Chained Equations sensitivity analyses did not find substantial differences, suggesting no major impact of missing data on the results (Tables 2b-Supplementary Information).
Immunological changes and risk factors for CD4 + cell count reduction
Figure 3 presents the median CD4 + cell count over time in pregnant women with and without AHD. We observed an increasing trend of the median CD4 + cell count in women without AHD during the 36 months follow-up (p < 0.001), however, this remained constantly below 200 cells/mm3 in women presenting with AHD at first ANC clinic visit.
In 12.5% (161/1288) of women (with and without AHD) at the six months visit and in 14.2% (148/1038) of them at the 12 months visit, there was a “less than expected improvement in CD4 + cell counts”. The reduction in CD4 + cell counts was of 274.5 cells/mm3 (95% CI: -323.76, -225.2) and 117.7 cells/mm3 (95% CI: -180.8, -54.5), at the six- and 12-months visits, respectively (Table 3). Table 4 shows the proportion of women with a “less than expected improvement in the CD4 + cell count” over time. Although not statistically significant, increases in the CD4 cell count at the 12- and 18-month visits (both coinciding with the breastfeeding period) were less common in women with AHD compared to those without it.
Factors associated with a “less than expected improvement in CD4 cell counts” at the six -month visits were age, WHO clinical stage and CD4 cell counts at first ANC visit. Women aged 20–24 years (aOR = 2.27, 95% CI: 1.17; 4.40), those severely immunocompromised in WHO clinical stage IV (aOR = 9.59; 95% CI: 2.94;31.27) and with a CD4 cell count ≥ 200 (aOR = 1.92, 95% CI: 0.97;3.83) had higher odds of a “less than expected improvement in the CD4 cell count” while on ART compared to younger women (aged < 20 years), those in WHO clinical stage I-II and with a CD4 cell count < 200, respectively. Likewise, the Multivariate Imputation by Chained Equations sensitivity analyses did not find substantial differences, suggesting no major impact of missing data on the results (Tables 5b-Supplementary Information) Table 5.
Maternal and neonatal outcomes
Information on maternal and neonatal outcomes was available for 1534 out of 2458 study participants (62%) (Table 6). Median follow-up was 1150 (IQR: 634.5–1527) days in women with AHD and 1046 (IQR: 562–1494) in women without AHD. Most women were on ART at the time of delivery [188 (96.4%) of those with AHD and 1298 (97.4%) of those without it] and one month after delivery [195 (99.0%) of those with AHD and 1331 (99.8%) of those without it]. No significant differences were detected between women with and without AHD regarding the type of delivery, frequency of prematurity, low birth weight, neonate HIV status and birth defects. Fifteen maternal deaths were reported during the 36 months study follow-up. No significant differences were detected between women with and without AHD regarding maternal mortality in women with AHD [1.1% (4/349)] versus [0.5% (11/2109)] (OR: 2.1; 95%CI 0.70–6.98; p = 0.309). The majority of these deaths occurred within six months after the first ANC clinic visit (40%) and among women who were not receiving ART at enrolment (53.3%). According to the Kaplan–Meier survival curves up until 36 months after the first ANC visit, all pregnant women with and without AHD appeared to have similar probabilities for death (p = 0.750).
Discussion
To our knowledge, this study is the first one describing the burden, clinical presentation and risk factors for AHD in Mozambican pregnant women. Despite the roll out of ART in the last two decades in the country, we observed that at first ANC visit over 14% of HIV-infected pregnant women presented with AHD and about 2% of them were severely immunosuppressed. In addition, there were no significant changes in the annual frequency of pregnant women with AHD starting ANC between 2015 and 2020. This unacceptable and constant high rate of AHD among pregnant women has important clinical and public health implications, including the strengthening of ongoing HIV-control efforts specially focused in women of childbearing age. The proportion of women with AHD in this cohort was lower than the 37% estimated in the general population in Mozambique, although this figure is from 2014 [8], and similar to reports in pregnant women from neighboring South Africa (12%) and Tanzania (12-14%) [13, 38, 39]. The results of this study showed that a high proportion (76.2%) of pregnant women with AHD had been on ART for a long period (nearly 2 years), suggesting suboptimal case management regarding detection of low adherence and/or treatment failure before the current pregnancy. In fact, despite reports of high prevalence of HIV drug resistance in pregnant women in Mozambique [40], only a small proportion (3%) of women with AHD were receiving the second line ART regimen (AZT/3TC/LPV/r or ABC), while 10.9% were on the less effective AZT/3TC/NVP regimen [41]. Over 14% of the women who presented with AHD at the first ANC visit were not receiving ART indicating timeworn HIV infection before the current pregnancy and a missed opportunity of being enrolled on ART before HIV disease progression. In the current study, tuberculosis was the only opportunistic infection identified in pregnant women with AHD; however, this does not exclude the existence of other opportunistic infections [12]. It could be hypothesized that since bacterial infections often present with acute symptoms, women with these infections may have sought medical assistance before attending the ANC clinic. In addition, the provision of cotrimoxazole prophylaxis may have been effective in reducing the risk of bacterial infections [42,43,44]. Additionally, as in other low-income settings, limited access to diagnostic facilities may explain the low detection of opportunistic infections, supporting the need for availability of accurate diagnostic tests in these settings [45, 46]. There was an increasing trend of the median CD4+ cell counts in women without AHD during the 36 months follow-up, however, this remained constantly below 200 cells/mm³ in women with AHD at first ANC visit. Furthermore, fewer women with AHD had an increase in CD4 cell counts over time during post-partum suggesting that a possible improvement in ART adherence during pregnancy did not continue after delivery. Thus, approaches to increase ART adherence after delivery will be useful to prevent mother-to-child HIV transmission through breastfeeding while improving women’s health. The CD4 drop in pregnancy (about 50 cells) is not a real reduction in CD4 cells but the same amount in a larger amount of blood due to hemodilution. The drop is only temporary, which is more in the first trimester of pregnancy and in primigravidae [19]. In this study, we calculated variation in CD4 cell counts from the first ANC visit, on what he median (IQR) gestational age at ANC enrolment was 21 [15,16,17,18,19,20,21,22,23,24,25] weeks, therefore, after the first trimester of pregnancy. In 12.5% of the HIV-infected women with AHD at the six month visit and in 14.2% of the HIV-infected women without AHD at the 12 month visit after the first ANC, a “less than expected improvement in CD4+ cell counts” was observed, with a reduction in the CD4+ cell count of 274.5 cells/mm³ and of 117.7 cells/mm³, respectively. This finding indicates that AHD would not be detected in many women with borderline CD4+ cell counts (CD4+ cell count <200 cells/mm³ for AHD definition) in the absence of repeated measurements of CD4+ cell counts. Currently, viral load measurement is recommended to monitor the ART response, however, in Mozambique, only 61% of people living with HIV on ART had had at least one viral load test [47]. Therefore, efforts are needed to improve access to viral load testing facilities. In addition, given the high burden of infectious diseases in many low-income settings these results support the recommendation for continued CTXp for all women of childbearing age regardless of the CD4+ cell count [42,43,44]. Our findings are consistent with previous studies showing that older age and ART regimen (AZT/3TC/NVP and AZT/3TC/LPV/r or ABC) are risk factors for presenting AHD [12, 35, 36], and also with reports showing that older age and being on WHO Clinical Stage IV were risk factors for “less than expected improvement in CD4 cell counts” [29, 48]. Assessment of these factors may help to identify HIV-infected pregnant women with AHD and thus, prioritize case management and prevention of disease progression. The fact that women with CD4<200 cell counts at the first ANC visit had a lower risk of “less than expected improvement in CD4 cell counts” six months later could be explained by the fact that women identified with AHD may be more closely monitored compared with those without it, which might improve adherence to ART. In any case, the confounding effect of some other variable not included in the logistic regression analysis and which could explain our discordant results cannot be ruled out. We found no differences in the frequency of adverse maternal and perinatal outcomes between women with and without AHD, which might be explained by the overall high ART adherence rate at the end of pregnancy. At the time of delivery and one month postpartum, the majority of women were retained on ART. These results support the benefits of ART on preventing adverse pregnancy outcomes among women with AHD disease [49, 50]. While some limitations of the study have been discussed previously, other methodological limitations should be mentioned. The descriptive study design did not allow us to make direct assessments of the impact of different interventions implemented during study period. Other limitation of this study is due to the fact that since March 2019, repeated CD4+ cell counts measurements were only performed in women with suspicion of AHD, and therefore, in the last year of the study, the proportion of women with a “less than expected improvement in CD4+ cell counts” after the first ANC visit may have been overestimated. In addition, information on participant’s vital status (mortality) were retrieve from HDSS data base with poor information on the mortality causes. Finally, due to the retrospective design of part of the study, there were missing values in some important study variables, such as viral load, limiting the identification of women who may have had immunological discordant response to ART and validity of all the analyses. Nevertheless, the Multivariate Imputation by Chained Equations sensitivity analyses did not find substantial differences, suggesting no major impact of missing data and consistency of the results.
Conclusion
After more than two decades of ART roll out, 14% of HIV-infected pregnant women presented with AHD disease at first ANC visit in this area of southern Mozambique. In order to achieve progress towards the UNAIDS 95/95/95 goals for 2025 in HIV-infected pregnant women, prompt HIV diagnosis in women of childbearing age, effective linkage to HIV care with an optimal ART regimen and close monitoring after ART initiation, are fundamental strategies that must be urgently implemented to improve maternal and child survival.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ABC:
-
Abacavir
- ANC:
-
Antenatal care
- AHD:
-
Advanced HIV disease
- ART:
-
Antiretroviral therapy
- ARV:
-
Antiretroviral
- AZT:
-
Zidovudine
- CISM:
-
Centro de Investigação em Saúde de Manhiça
- CTXp:
-
Cotrimoxazole prophylaxis
- DHSS:
-
Demographic and Health Surveillance System
- DTG:
-
Dolutegravir
- EFV:
-
Efavirenze
- IeDEA-SA:
-
International Epidemiological Databases to Evaluate AIDS in Southern Africa
- LPV/r:
-
Lopinavir-ritonavir
- NID:
-
Numeric identifier
- NVP:
-
Nevirapine
- PMTCT:
-
Prevention of mother to child transmission
- TDF:
-
Tenofovir
- 3TC:
-
Lamivudine
References
UNAIDS. Country factsheets [Internet]. Available from: https://www.unaids.org/es/regionscountries/countries/mozambique. Accessed 20 Nov 2021.
Inquérito de Indicadores de Imunização, Malária e HIV/SIDA em Moçambique (IMASIDA) 2015: Relatório de Indicadores Básicos de HIV. Instituto Nacional de Saúde, Instituto Nacional de Estatística de Moçambique. 2017. Available from: https://dhsprogram.com/pubs/pdf/AIS12/AIS12.pdf. Accessed 23 Nov 2021.
González R, Munguambe K, Aponte J, Bavo C, Nhalungo D, Macete E, et al. High HIV prevalence in a southern semi-rural area of Mozambique: a community-based survey. HIV Med. 2012;13(10):581–8. https://doi.org/10.1111/j.1468-1293.2012.01018.x.
MISAU. 2020 HIV/AIDS Report. Mozambique Ministry of Health. 2021. Available from: https://www.misau.gov.mz/index.php/relatorios-anuais2021. Accessed 20 Nov 2021.
Acceleration Plan for the Response to HIV/AIDS. Mozambique Ministry of Health. 2013. Available from: http://www.misau.gov.mz/index.php/planos-estrategicos-do-hiv. Accessed 20 Nov 2021.
WHO. Consolidated Guidelines on The Use of Antiretroviral Drugs for Treating And Preventing HIV infection [Internet]. WHO. 2013 [cited 2010 Jul 20]. Available from: http://apps.who.int/iris/bitstream/10665/85321/1/9789241505727_%0Aeng.pdf?ua=1. Accessed 22 Nov 2021.
World Health Organization. HIV/AIDS Programme. Programmatic Update. Use of Antiretroviral Drugs for Treating Pregnant Women and Preventing HIV Infections in Infants. Available from: https://apps.who.int/iris/bitstream/handle/10665/70892/WHO_HIV_2012.6_por.pdf?sequence=1&isAllowed=y. 2021. Accessed 28 Dec 2021.
Auld AF, Shiraishi RW, Couto A, Mbofana F, Colborn K, Alfredo C, et al. A Decade of Antiretroviral Therapy Scale-up in Mozambique. JAIDS J Acquir Immune Defic Syndr. 2016;73(2):e11-22. https://doi.org/10.1097/QAI.0000000000001137.
UNAIDS. Understanding fast-track accelerating action to end the AIDS epidemic by 2030. 2015. Available from: https://www.unaids.org/sites/default/files/media_ asset/ JC2686_WAD2014report_en.pdf. Accessed 28 Dec 2021.
Ford N, Shubber Z, Meintjes G, Grinsztejn B, Eholie S, Mills EJ, et al. Causes of hospital admission among people living with HIV worldwide: a systematic review and meta-analysis. lancet HIV. 2015;2(10):e438-44. https://doi.org/10.1016/S2352-3018(15)00137-X.
Low A, Gavriilidis G, Larke N, -Lajoie M-R B, Drouin O, J Stover, et al. Incidence of Opportunistic Infections and the Impact of Antiretroviral Therapy Among HIV-Infected Adults in Low- and Middle-Income Countries: A Systematic Review and Meta-analysis. Clin Infect Dis. 2016;62(12):1595–603. https://doi.org/10.1093/cid/ciw125.
World Health Organization. guidelines for managing advanced hiv disease and rapid initiation of antiretroviral therapy, July 2017 WHO [Internet]. Available from: http://apps.who.int/iris/bitstream/handle/10665/255884/9789241550062-eng.pdf;jsessionid=11829ECD3684DE92B900B713F4C6255F?sequence=1. Accessed 20 Nov 2021.
Auld AF, Shiraishi RW, Oboho I, Ross C, Bateganya M, Pelletier V, et al. Trends in Prevalence of Advanced HIV Disease at Antiretroviral Therapy Enrollment — 10 Countries, 2004–2015. MMWR Morb Mortal Wkly Rep. 2017;66(21):558–63. https://doi.org/10.15585/mmwr.mm6621a3.
Cates JE, Westreich D, Edmonds A, Wright RL, Minkoff H, Colie C, et al. The Effects of Viral Load Burden on Pregnancy Loss among HIV-Infected Women in the United States. Infect Dis Obstet Gynecol. 2015;2015:362357. https://doi.org/10.1155/2015/362357.
Chilaka VN, Konje JC. HIV in pregnancy - An update. Eur J Obstet Gynecol Reprod Biol. 2021;256:484–91. https://doi.org/10.1016/j.ejogrb.2020.11.034.
Calvert C, Ronsmans C. The contribution of HIV to pregnancy-related mortality: a systematic review and meta-analysis. AIDS. 2013;27(10):1631–9. https://doi.org/10.1097/QAD.0b013e32835fd940.
Calvert C, Ronsmans C. Pregnancy and HIV disease progression: a systematic review and meta-analysis. Trop Med Int Heal. 2015;20(2):122–45. https://doi.org/10.1111/tmi.12412 (Epub 2014 Oct 31).
Ekouevi DK, Inwoley A, Tonwe-Gold B, Danel C, Becquet R, Viho I, et al. Variation of CD4 Count and Percentage during Pregnancy and after Delivery: Implications for HAART Initiation in Resource-Limited Settings. AIDS Res Hum Retroviruses. 2007;23(12):1469–74. https://doi.org/10.1089/aid.2007.0059.
Byrns M, Elwood C, Capmas P, Kakkar F, Boucher M, Money D, et al. Variation of CD4 count in pregnant women living with HIV. Am J Obstet Gynecol. 2020;223(6):962–3. https://doi.org/10.1016/j.ajog.2020.08.122.
Wall KM, Rida W, Haddad LB, Kamali A, Karita E, Lakhi S, et al. Pregnancy and HIV Disease Progression in an Early Infection Cohort from Five African Countries. Epidemiology. 2017;28(2):224–32. https://doi.org/10.1097/EDE.0000000000000590.
Nhacolo A, Jamisse E, Augusto O, Matsena T, Hunguana A, Mandomando I, et al. Cohort profile update: Manhiça health and demographic surveillance system (HDSS) of the Manhiça health research centre (CISM). Int J Epidemiol. 2021 Jan 16; https://doi.or/https://doi.org/10.1093/ije/dyaa218.
Bassat Q, Guinovart C, Sigaúque B, Aide P, Sacarlal J, Nhampossa T, et al. Malaria in rural Mozambique. Part II: Children admitted to hospital. Malar J. 2008;7. https://doi.or/https://doi.org/10.1093/ije/dyaa218.
Aide P, Aponte JJ, Renom M, Nhampossa T, Sacarlal J, Mandomando I, et al. Safety, immunogenicity and duration of protection of the RTS,S/ASO2<inf>D</inf> malaria vaccine: One year follow-up of a randomized controlled phase I/IIb trial. PLoS One. 2010;5(11). https://doi.org/10.1371/journal.pone.0013838.
Lambdin BH, Micek MA, Koepsell TD, Hughes JP, Sherr K, Pfeiffer J, et al. An assessment of the accuracy and availability of data in electronic patient tracking systems for patients receiving HIV treatment in central Mozambique. BMC Health Serv Res. 2012;12:30. https://doi.org/10.1186/1472-6963-12-30.
MISAU. Introdução de Normas Clinicas Atualizadas e dos Modelos Diferenciados de Serviços, para o seguimento do paciente HIV positivo – CIRCULAR 2. 2019. Available from: https://comitetarvmisau.co.mz/docs/orientacoes_nacionais/ Circular_Normas_Cli%CC%81nicas_08_03_19.pdf. Accessed 12 Jan 2022.
MISAU. Tratamento Antiretroviral e Infecções Oportunistas do Adulto, Adolescente, Grávida e Criança. 2016. Available from: file:///C:/Users/tnhampossa/Downloads/ Tratamento%20Antiretroviral%20e%20Infec%C3%A7%C3%B5es%20Oportunistas%20no%20Adulto%20Adolescente%20Gr%C3%A1vida%20e%20Crian%C3%A7a%20-%20Gui%C3%A3o%20de%20Bolso%20(1).pdf. Accessed 14 May 2017.
MISAU. Circular Normas Clínicas 08.03.19 - COMITÉ TARV [Internet]. Available from: omitetarvmisau.co.mz/docs/orientacoes_nacionais/Circular_Normas_Clínicas_08_03_19.pdf. Accessed 12 Jan 2022.
Zaniewski E, Tymejczyk O, Kariminia A, Desmonde S, Leroy V, Ford N, et al. IeDEA-WHO Research-Policy Collaboration: contributing real-world evidence to HIV progress reporting and guideline development. J virus Erad. 2018 Nov 15;4(Suppl 2):9–15. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6248847/. Accessed 12 Jan 2022.
Mocroft A, Phillips AN, Gatell J, Ledergerber B, Fisher M, Clumeck N, et al. Normalisation of CD4 counts in patients with HIV-1 infection and maximum virological suppression who are taking combination antiretroviral therapy: an observational cohort study. Lancet (London, England). 2007;370(9585):407–13. https://doi.org/10.1016/S0140-6736(07)60948-9.
Loutfy MR, Genebat M, Moore D, Raboud J, Chan K, Antoniou T, et al. A CD4+ Cell Count <200 Cells per Cubic Millimeter at 2 Years After Initiation of Combination Antiretroviral Therapy Is Associated With Increased Mortality in HIV-Infected Individuals With Viral Suppression. JAIDS J Acquir Immune Defic Syndr. 2010 Dec 1;55(4):451–9. https://doi.org/10.1097/qai.0b013e3181ec28ff.
Ahmed T, Hossain M, Sanin KI. Global Burden of Maternal and Child Undernutrition and Micronutrient Deficiencies. Ann Nutr Metab. 2012;61(s1):8–17. https://doi.org/10.1159/000345165.
Adam I, Ali AA. Anemia During Pregnancy. In: Nutritional Deficiency. InTech; 2016.
Romano M, Cacciatore A, Giordano R, La Rosa B. Postpartum period: three distinct but continuous phases. J Prenat Med. 2010 Apr;4(2):22–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22439056
Taha Z, Ali Hassan A, Wikkeling-Scott L, Papandreou D. Factors Associated with Preterm Birth and Low Birth Weight in Abu Dhabi, the United Arab Emirates. Int J Environ Res Public Health. 2020;17(4):1382. https://doi.org/10.3390/ijerph17041382.
Jiang H, Liu J, Tan Z, Fu X, Xie Y, Lin K, et al. Prevalence of and factors associated with advanced HIV disease among newly diagnosed people living with HIV in Guangdong Province. China J Int AIDS Soc. 2020;23(11):e25642. https://doi.org/10.1002/jia2.25642.
Lebelonyane R, Mills LA, Mogorosi C, Ussery F, Marukutira T, Theu J, et al. Advanced HIV disease in the Botswana combination prevention project: prevalence, risk factors, and outcomes. AIDS. 2020;34(15):2223–30. https://doi.org/10.1097/QAD.0000000000002627.
Buuren S van, Groothuis-Oudshoorn K. mice. Multivariate Imputation by Chained Equations in R. J Stat Softw. 2011;45(3). https://doi.org/10.18637/jss.v045.i03.
Malaba TR, Phillips T, Le Roux S, Brittain K, Zerbe A, Petro G, et al. Antiretroviral therapy use during pregnancy and adverse birth outcomes in South African women. Int J Epidemiol. 2017;46(5):1678–89. https://doi.org/10.1093/ije/dyx136.
Shayo GA, Moshiro C, Spiegelman D, Mugusi FM, Chalamilla G, Msamanga G, et al. Prevalence and risk factors for skin diseases among antiretroviral-naïve HIV-infected pregnant women in Dar es Salaam. Tanzania Int J Dermatol. 2014;53(10):1249–58. https://doi.org/10.1111/ijd.12455.
Rupérez M, Noguera-Julian M, González R, Maculuve S, Bellido R, Vala A, et al. HIV drug resistance patterns in pregnant women using next generation sequence in Mozambique Ceccherini-Silberstein F, editor. PLoS One. 2018;13(5):e0196451. https://doi.org/10.1371/journal.pone.0196451.
Cain LE, Phillips A, Lodi S, Sabin C, Bansi L, Justice A, et al. The effect of efavirenz versus nevirapine-containing regimens on immunologic, virologic and clinical outcomes in a prospective observational study. AIDS. 2012 Aug 24;26(13):1691–705. https://doi.org/10.1097/QAD.0b013e328354f497.
Suthar AB, Vitoria MA, Nagata JM, Anglaret X, Mbori-Ngacha D, Sued O, et al. Co-trimoxazole prophylaxis in adults, including pregnant women, with HIV: a systematic review and meta-analysis. Lancet HIV. 2015 Apr;2(4):e137-50. https://doi.org/10.1016/S2352-3018(15)00005-3.
Campbell JD, Moore D, Degerman R, Kaharuza F, Were W, Muramuzi E, et al. HIV-Infected Ugandan Adults Taking Antiretroviral Therapy With CD4 Counts >200 Cells/ L Who Discontinue Cotrimoxazole Prophylaxis Have Increased Risk of Malaria and Diarrhea. Clin Infect Dis. 2012 Apr 15;54(8):1204–11. https://doi.org/10.1093/cid/cis013.
Polyak CS, Yuhas K, Singa B, Khaemba M, Walson J, Richardson BA, et al. Cotrimoxazole Prophylaxis Discontinuation among Antiretroviral-Treated HIV-1-Infected Adults in Kenya: A Randomized Non-inferiority Trial. Carr A, editor. PLOS Med. 2016;13(1):e1001934. https://doi.org/10.1371/journal.pmed.1001934.
Johansen ØH, Abdissa A, Zangenberg M, Mekonnen Z, Eshetu B, Bjørang O, et al. Performance and operational feasibility of two diagnostic tests for cryptosporidiosis in children (CRYPTO-POC): a clinical, prospective, diagnostic accuracy study. Lancet Infect Dis. 2021 May;21(5):722–30. https://doi.org/10.1016/S1473-3099(20)30556-9.
McNerney R. Diagnostics for Developing Countries. Diagnostics (Basel, Switzerland). 2015 May 19;5(2):200–9. https://doi.org/10.3390/diagnostics5020200.
MISAU. 2021 HIV/AIDS Report. 2022. Available from: https://www.misau.gov.mz/index.php/relatorios-anuais
Loutfy MR, Genebat M, Moore D, Raboud J, Chan K, Antoniou T, et al. A CD4+ cell count <200 cells per cubic millimeter at 2 years after initiation of combination antiretroviral therapy is associated with increased mortality in HIV-infected individuals with viral suppression. J Acquir Immune Defic Syndr. 2010 Dec;55(4):451–9. https://doi.org/10.1097/qai.0b013e3181ec28ff.
Fowler MG, Qin M, Fiscus SA, Currier JS, Flynn PM, Chipato T, et al. Benefits and Risks of Antiretroviral Therapy for Perinatal HIV Prevention. N Engl J Med. 2016;375(18):1726–37. https://doi.org/10.1056/NEJMoa1511691.
Uthman OA, Nachega JB, Anderson J, Kanters S, Mills EJ, Renaud F, et al. Timing of initiation of antiretroviral therapy and adverse pregnancy outcomes: a systematic review and meta-analysis. Lancet HIV. 2017 Jan;4(1):e21-30. https://doi.org/10.1016/S2352-3018(16)30195-3.
Acknowledgements
The authors thank all study participants and the healthcare workers from Centro de Investigação em Saúde de Manhiça and Manhiça District Hospital who assisted with data collection, and the district health authorities for their collaboration on the on-going research activities in the Manhiça district.
Funding
Data collection was supported by the International Epidemiology Databases to Evaluate AIDS IeDEA. CISM is supported by the Government of Mozambique and the Spanish Agency for International Development (AECID). TN (corresponding author) is supported by a career development fellowship co-funded by the EDCTP (European and Developing Countries Clinical Trials Partnership) and the Calouste Gulbenkian Foundation (grant number: TMA2017CDF-1927 – Preg_multidrug).
Author information
Authors and Affiliations
Contributions
Project conception and protocol design: TN, CM Coordination of clinical data collection: TN, MM, GB Statistical analysis and interpretation of data: AN, AC, TN, LQ, RG, LG, CM Contributed to the writing of the manuscript: TN, RG, LG, AC, LQ, ES, KM, CM Reviewed the draft and approved the decision to submit the paper: all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki and the National Bioethics Committee of Mozambique approved the study protocol in 2011 (327/CNBS/11), with subsequent annual renewals until the year 2020. After informing the pregnant women about the study objectives and methods, women consented for their participation, and that of their children, by signing a written informed consent. One copy of the consent form was handled to the participant.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table 2-b
. Independent risk factors for advanced HIV disease (according to multiple imputation analyses).
Additional file 2: Table 5-b
. Factors associated with less than expected improvement in the CD4+ cell count over time by advanced HIV disease status (according to multiple imputation analyses).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nhampossa, T., González, R., Nhacolo, A. et al. Burden, clinical presentation and risk factors of advanced HIV disease in pregnant Mozambican women. BMC Pregnancy Childbirth 22, 756 (2022). https://doi.org/10.1186/s12884-022-05090-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-05090-3