Abstract
Background
Self-care behaviors during pregnancy significantly impacts mother and children's health. This study aimed to explore the self-care behaviors and the associations of these behaviors with the psychological well-being of women during pregnancy, as well as the mediating effects of different social support with these associations.
Methods
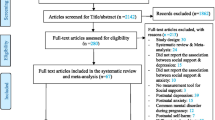
A cross-sectional data of 562 pregnant women at Hanoi Obstetrics & Gynecology Hospital and Ca Mau Obstetrics & Pediatrics in Vietnam were analyzed. Questions about self-care behaviors, pregnancy characteristics, social support, and psychological well-being were asked. Multivariate regression models were performed. Structural Equation Modeling (SEM) was employed to test the mediating effects of different social support with the association between self-care behaviors and psychological well-being.
Findings
Only 13% of pregnant women often or always did physical exercise at least three times a week, and 40% consumed enough fiber and five servings of vegetables a day. Only 78.7% always avoided alcohol drinking, and 53.9% of pregnant women avoided being exposed to second-hand smoking and 71,7% avoided using traditional medicine without physicians’ prescriptions. Around 66% of pregnant women always or often had prenatal care checkups as scheduled. Information sources, social support and childbirth expectation were major drivers for self-care practices. SEM model showed that social support mediated the relationship between maternal health behaviors and mental well-being.
Conclusion
This study highlighted the remarkable gaps in self-care practices among our pregnant women, which were significantly associated with their mental well-being. Social support-oriented consultancy and interventions should be warranted for improving behaviors and the mental well-being of pregnant women in Vietnam.
Similar content being viewed by others
Introduction
Prenatal behaviors are major attributable to the success of pregnancy. World Health Organization (WHO) recommends that pregnant women should be consulted about health behaviors such as healthy diet, physical activity, daily intake of food supplements, and avoidance of substance use and abuse before pregnancy [1]. Healthy practices positively affect the health condition of pregnant women and the development of their offspring [2], while unhealthy behaviors can result in many physical and psychological consequences, as well as increasing the risk of birth defects, miscarriage or preterm birth [3,4,5,6]. However, unhealthy practices are prevalent while healthy behaviors are not sufficient in this population. For example, prior meta-analyses estimated that approximately 10% of pregnant women used alcohol [7], 0.8 to 8.1% smoked tobacco [8], and 60% consumed low-energy diets [9]. Low education, low socioeconomic status, unemployed, poor social support or unplanned pregnancy were associated with a higher likelihood of being engaged with unhealthy practices [10,11,12,13]. Meanwhile, only 15% of pregnant women adhered to recommendations for physical activity [14] and 3% followed recommended diets with four food groups [15].
A holistic approach to health considers multidimensional factors of well-being, including physical, mental, emotional, social, intellectual as well as spiritual. Therefore, besides practicing healthy physical behaviors, having good psychological wellness is an important part of the pregnancy period since it is associated with pregnancy outcomes. Psychological stress and prenatal depression in pregnant women in both short and long terms cause an imbalance in homeostasis and weaken the body’s immune responses, raising the risk of preeclampsia, preterm birth or miscarriage [16, 17]. In addition, poor psychological well-being during the prenatal period is a significant predictor of postpartum depression [18] as well as associated with various adverse outcomes in children [19]. In literature, health behaviors have bidirectional relationships with the psychological well-being of pregnant women [20]. Women with unhealthy lifestyles tend to simultaneously experience mental health problems such as depression and/or anxiety [21]; whereas, women exhibiting more depressive symptoms were more likely to engage in unhealthy behaviors (e.g. tobacco smoking, alcohol drinking or cocaine using) [22]. Further investigation into such a relationship would potentially provide insights for improving the mental wellness of pregnant women and consequently the health condition of the mothers and their children.
Social support has a critical role in changing lifestyles and improving both physical and psychological health outcomes in mothers [23]. Previous studies revealed the influences of social support on the success of pregnancy and mothers’ postnatal health conditions through assisting them in maintaining psychological wellbeing [24, 25], feeling less anxious [26,27,28,29], or reducing stress [30, 31]. Lower social support of pregnant women was associated with lower birth weight infants [32], worse labor progress, and babies with lower Apgar scores than women with higher social support [33]. Existing literature also reported the role of social support mediating the relationship between depression and birth outcomes. Depressed women receiving lower social support gave birth to babies with lower Apgar scores than those with higher social support [34]. Social support has been shown to have a similar buffering impact on birth weight among women experiencing stress [35]. In addition, pregnant women having high satisfaction with their marital relationship are more likely to have healthy diets [36]. However, whether social support buffers associations between health behaviors and psychological well-being of pregnant women have not been sufficiently explored. Understanding this mediating effect is critical for designing interventions to improve pregnancy care. This study aimed to examine health behaviors among pregnant women and their associated factors, as well as the mediating effects of social support on the relationships between health behaviors and psychological well-being in this population.
Methods
Study design and participants
A cross-sectional study was conducted in two obstetric medical centers including Hanoi Obstetrics & Gynecology Hospital and Ca Mau Obstetrics & Pediatrics Provincial Hospital from January to February 2021. Criteria for selecting participants as follows: (1) Aged 18 and older; (2) Agree to participate in research; (3) Being pregnant and not being delivered at the time of the study; (4) Did not have any cognitive impairment or any disabilities which might limit the ability to answer the interview questionnaire.
We computed the sample size by using the formula for estimating a population proportion with relative precision, including the following parameters: confidence level α = 0.05, expected proportion = 0.15 (the proportion of pregnant women adhered to physical activity recommendations [14]), and relative precision = 0.2. The necessary sample size was 545 pregnant women. We added 10% of the sample size for preventing drop-out, resulting in 600 pregnant women for the final sample size. The sampling process was performed parallel in both hospitals. The pregnant women were conveniently approached and recruited to this study when they visited the antenatal clinics for regular care. At the end of the study period, a total of 675 women were recruited. After excluding those not completing questions about health behaviors, psychological well-being and social support, the final sample size for analysis was 562 (completion rate 83.3%). The Institutional Review Board of Hanoi Obstetrics & Gynecology Hospital granted the study protocol (Code: 07 QĐ/PS‐TTĐT CĐT).
Data collection and measurement
We developed a structured questionnaire and used face-to-face interviews for collecting data. Participants were initially screened from the eligibility criteria before being invited to be enrolled in the study. Then, women agreeing to participate would be invited to a private room for the interview. We firstly informed a short introduction about the study and participants’ rights and benefits. Next, the data collector (i.e. trained nurses or undergraduate medical students) interviewed them by using the questionnaire. Each interview lasted 15–20 min. The structure of the questionnaire included: 1) Demographic information; 2) Pregnancy characteristics; 3) Health behaviors during pregnancy; 4) Psychological wellbeing, and 5) Social support.
Health behaviors
In this study, we asked pregnant women to report the frequency of fifteen recommended health behaviors for pregnancy that they performed during the pregnancy period. Each behavior had five options for response: 1 = None; 2 = Rarely; 3 = Sometimes; 4 = Often; and 5 = Always.
Psychological well-being
The World Health Organization-5 Well-being scale was utilized to assess participants’ mental well-being in the last two weeks [37]. Participants were asked to respond to five questions about different psychological aspects, using a 6-point Likert scale ranging from 0 (at no time) to 5 (all of the time). The total score was calculated and converted to a new transformed score from 0 to 100, which a higher score meant a higher level of psychological well-being. The results of previous studies have discovered that the Cronbach’s alpha of The World Health Organization-5 Well-being scale was 0.85 [38].
Social support
The Perinatal Infant Care Social Support (PICSS) instrument was used to evaluate social support [39]. Participants were asked to rate how strongly they agreed with twenty-two statements using a 4-point Likert scale from 1 “Totally disagree” to 4 “Totally agree”. This scale measured social support in four subscales: Informational support (7-item scores from 7 to 28); Instrumental support (7-item scores from 7 to 28); Emotional support (4-item scores from 4 to 16); Appraisal support (4-item scores from 4 to 16). The Cronbach’s alpha was excellent at 0.9727.
Demographic and pregnancy characteristics
Demographic characteristics such as age, education, occupation, health insurance status, living arrangement, partner’s age, partner’s education, and monthly household income. Pregnancy characteristics consisted of complications of pregnancy, source of maternal care information (health professional, internet/social network, friends/relatives, radio & television, smartphone application, newspapers & book, phone message, or poster/banner). Expectancy of having a baby and fear of childbirth were asked with 10-point rating scales from 0 “No having expectation” or “No fear” to 10 “Very strong expectation” or “Extreme fear”, respectively.
Data analysis and statistical method
Data management and analysis were performed using Stata version 15.0 software (Stata Corporation). A listwise deletion approach was used to handle the missing data. A significance level of p < 0.05 was used. The Chi-square test for categorical variables and the Mann–Whitney test for continuous variables were used to make comparisons between urban and rural pregnant women. To investigate the scale of items and enhance the interpretability of this research, the exploratory factor analysis was employed to define factors with a threshold of an eigenvalue of 1.6 by scree test, in which the curve had been flattened. An orthogonal varimax rotation with Kaiser normalization was used. A value of 0.29 was chosen as the cut-off point for factor loading. The result of the Kaiser–Meyer–Olkin test was 0.7676, suggesting that the sample size was adequate for EFA. The p-value of Bartlett’s Test of Sphericity was less than 0.01 (χ2 = 3873.431; Degrees of freedom = 105; p-value = 0.000), which indicated that EFA was helpful for restructuring the health behavior scale. Cronbach's alpha was used to assess the internal consistency of each factor. The score of each factor was calculated by summing the score of all items within the factor and then dividing it by the number of items in this factor. The score ranged from 1 to 5, which a higher score indicated a higher level of behavior engagement.
Multivariate Tobit regression models were carried out to explore the association of health practices demographic characteristics, pregnancy characteristics, and social support. To minimize the models, stepwise forward selection strategies were used with a log-likelihood ratio test at a p-value of 0.2. Structural equation modeling (SEM) was utilized to examine the mediating effect of social support between health behaviors and psychological well-being, adjusting for age and pregnancy status. For obtaining both direct and indirect/mediated directions, the SEM builder employs the maximum likelihood method. The built SEM model then was evaluated by goodness-of-fit indices involving Root Mean Square Error of Approximation (RMSEA), Comparative Fit Index (CFI), Standardized Root Mean Square Residual (SRMR).
Results
Demographic characteristics are shown in Table 1. A total of 562 pregnant women participated in the study. The mean age of women was 29.1 years old (SD = 5.3). More than half of the sample lived in an urban setting, and 85.3% of pregnant women in urban settings came from the North of Vietnam. The mean monthly income of households in urban was above two times higher than that of households in rural. Two-third of pregnant women in urban areas lived with partners, yet this rate in rural areas was only 48.6%.
Table 2 shows that pregnant women accessed various sources of information and there were significant differences in these sources between women in the urban areas and rural areas. To women in urban settings, the internet/social network was the main source of information (76.4%), while women in rural areas received information mostly from health providers (83.5%). Phone messages and posters/banners were not popular choices with only 7.8% and 5.3% of pregnant women receiving information from those sources, respectively. The expectation of having a baby in this study was high with a mean score of 7.8 (SD = 2.1, range score 0–10), and there was a significant difference between pregnant women of different areas (p < 0.01). The mean score of fear of childbirth among pregnant women in urban areas was 5.7 (SD = 2.9); which was significantly higher than those in rural settings (mean = 5.3, SD = 1.5) (p < 0.01). The mean score PICSS Informational support, PICSS Instrumental support, PICSS Emotional support, PICSS Appraisal support was 21.6 (SD = 2.7, range score 7–28), 21.5 (SD = 2.7, range score 7–28), 12.3 (SD = 1.5, range score 4–16), and 12.3 (SD = 1.4, range score 4–16), respectively.
The construct validity and reliability of maternity care practice from pregnant women are reported in Table 3. From factor analysis, three dimensions were reclassified namely “Healthy behaviors”, “Risk behavior avoidance” and “Health-seeking behaviors”. Cronbach’s alpha was accepted across domains, ranging from 0.60 to 0.80.
Figure 1 shows different health behaviors of pregnancy. More than two-thirds of pregnant women often or always took vitamins and minerals, iron and folic acid, and calcium as recommended. However, only 13% of pregnant women often or always did physical exercise at least three times a week. The rates of pregnant women taking enough fiber a day and five servings of vegetables a day were more than 40%. More than 90% of pregnant women always avoided substance uses such as tobacco smoking and addictive substances, but only 78.7% always avoided alcohol drinking. There was only about 53.9% of pregnant women avoided exposing second-hand smoking and 71,7% avoided using traditional medicine without physicians’ prescriptions. Around 66% of pregnant women always or often had prenatal care checkups as scheduled. There were only approximately 30% of women who often or always consulted medical staff for their maternal health and 27% of women who often or always discussed with health staff about maternity care.
Table 4 reveals that a higher level of healthy behaviors practices was positively associated with a higher expectation of having a child (Coef. = 0.05, 95%CI = 0.00–0.10) and higher appraisal support (Coef. = 0.05; 95%CI = 0.00–0.09), but negatively related to the fear of childbirth (Coef. = -0.03; 95%CI = -0.03-—0.01). In terms of risk behaviors avoidance, high education, living with partners, and considering relatives/radio, television/internet, social networks were associated with lower levels of risk behaviors avoidance. Meanwhile, a higher level of risk behaviors avoidance practices was positively associated with the Southern region (Coef. = 0.38, 95%CI = 0.08–0.69), high expectation of having a child (Coef. = 0.08; 95%C = 0.03–0.14), and high appraisal support (Coef. = 0.06, 95%CI = 0.01–0.11).
Regarding health-seeking behaviors, living with partners and in the Southern region was negatively related to these practices; whereas, higher husband’s age, having maternity problems, considering health professionals as information sources and high instrumental support were positively associated with health-seeking behavior practices.
Figure 2 illustrates the SEM model to show the mediating effects of social support on the associations between self-care practices and the mental well-being of pregnant women. The goodness-of-fit indices were acceptable with RMSEA = 0.153, CFI: 0.903, SRMR = 0.030. The model showed healthy behaviors and risk behavior avoidances were significantly associated with the mental well-being of pregnant women. Social support was found to have a positive relationship with mental well-being.
The estimations of the models, direct and indirect SEM paths and 95% Confident interval are presented in Table 5. Social support was only found to improve the relationship between healthy behaviors and mental well-being. The indirect effect of social support accounted for 11.9% of the total effect and 13.5% of the direct effect.
Discussion
This study suggested substantial gaps in health behaviors among pregnant women in Vietnam. While the frequency of risk behaviors such as alcohol use or second-hand smoking exposure was relatively high, the performance of healthy behaviors such as physical activity, vegetables/vitamins, and mineral supplements consumption was insufficient. This study also revealed the potential role of social support in improving their psychological well-being via mediating effects of health behaviors.
In the current study, we found that the health behaviors among Vietnamese pregnant women were critical health issues. The rates of risky behaviors such as alcohol use, tobacco use and second-hand smoking exposure in our sample were relatively similar or higher when compared to the previous findings in Vietnamese women in general and pregnant women in particular [40, 41]. Moreover, the result indicated approximately a third of our pregnant women used traditional medicine or herbal medicine without physicians’ prescriptions. It should be noted that the efficiency and effectiveness of traditional medicine, especially among pregnant women, were still limited [42]. Moreover, the usage of traditional medicine in Vietnam was frequently used without scientific studies [43], and there was a common belief that herbal medicine possessed no adverse effects [44]. Therefore, there is a need to increase the knowledge of pregnant women of self-medication to prevent side effects of traditional medicine on mothers and unborn children. In addition, the prevalence of healthy behavior among pregnant women was lower than in previous studies. The rate of physical activity during pregnancy (women who often or always did exercise at least 3 times a week) was around 12%. The result of this study was in line with that in Brazil (13.4% in the third trimester) [45], but lower than the level of physical activity of Chinese pregnant women (57.1%) [46]. The reason might be most pregnant women in this study was housewife and office worker, they tended to spend more time on housework rather than doing exercise or sport [47]. Moreover, it should be noticed that the questionnaire used in this study mentioned only physical exercise but not domestic work or work activities. Additionally, the rates of taking iron and folic acid were higher compared to a previous study conducted in Vietnam (25.8%) [48]. This result was similar to that reported in China (66.7%) [49], but higher than that of Japan (20.5%) [50], and Korea (10.5%) [51].
More than 60% of pregnant women visited maternity as scheduled. However, a similar prevalence of women did not consult or ask health care workers about maternity care. It could be justified that our samples used the internet/social network as one of the most common sources of information. Due to the rise of internet access over the last decade, many women have access to a wide variety of pregnancy, birth and parenting information [52]. The privacy, accessibility, and breadth of information available on the internet might be reasons why women prefer the Internet to other sources of information [53,54,55]. Women could use the internet to improve their comprehension of knowledge offered by their maternity care provider or to decide whether they should pursue additional advice [54]. Notably, the use of internet/social networks, relatives and radio/television as the information sources decreased the level of risk behavior avoidance practice. These informal sources were raised concerns about the accuracy of available information [52]. Women may have a lack of skills to appraisal information they found from these sources [52]. Despite health professionals as the main source of information for major pregnant women, we found only an association between this information source and health-seeking behaviors, why no relationship was found between this source and the other two behavior groups. This issue could be justified by two explanations: 1) There was homogeneity in other behaviors between the groups with and without using health professionals as a source of information; hence, the study could only find differences in health-seeking behaviors; or 2) Pregnant women in this study did not practice healthy behaviors or risks behavior avoidance according to the health professionals’ recommendations, raising a question about the role of health workers in providing maternal health information. Longitudinal follow-up studies should be conducted in the future to assess the role of health professionals in the self-care practices of pregnant women in Vietnam.
In this study, childbirth expectation among pregnant women was associated with the increase of the level of healthy behavior practices, and risk behavior avoidance, which might be explained by the maternal–fetal relationship [56]. We also found that fear of childbirth decreased the level of healthy behavior practices. It should be explained by the physiological side-effect of pregnancy (e.g., muscle pain, or backaches, which might hinder them to practice healthy behaviors such as physical activities. Besides, our result was consistent with the previous study, which confirmed that social support affected health-related behaviors such as smoking or dietary habits [57] and was a protective factor for pregnant women [57, 58]. In this study, appraisal support was related to both healthy behavior and risk behavior avoidance practices. Pregnant women were encouraged to turn one another for appraisal support in the form of sharing experiences, appreciating her childcare skills, understanding her need for help, and receiving feedback from health providers about her childcare skills. This result was in line with the previous study, which confirmed appraisal support had a positive impact in reducing risky behaviors among pregnancy [59, 60].
In the current research, healthy behaviors improved the mental well-being of pregnant women, which was consistent with a previous study [61]. With mediating effect of social support, the relationship between these variables was stronger. However, we also found out that risky behavior avoidance decreased mental well-being. It should be noted that, in our sample, more than 50% of pregnant women avoided being exposed to second-hand smoking. The source of smoking mainly came from restaurants, cafeterias, homes or workplaces [62]. We supposed that finding a smoke-free restaurant, asking husband or father-in-law or coworkers not to smoke caused pressure for pregnant women. However, social support helped mediate this relationship and increase mental well-being. Social support may indirectly increase maternal mental well-being by acting as a buffer against potential adverse effects of stressful events [23].
Several important implications could be drawn from study findings. First, our results suggest that there is a need to improve health literacy between healthcare providers and pregnant women. Communication is not just a one-way but an active social process. Besides, our findings point to a need to introduce reliable information sources (e.g. websites, television channels, etc.) with guidance from health experts to ensure that pregnant women received accurate information. Second, interventions to mitigate the influences of negative behaviors on the mental well-being of pregnant women should integrate social support as the main component to cope with stressful situations. Meanwhile, in non-stressful situations, social support would provide a positive personal emotional experience.
The strength of our study lies in the large sample size of 562 pregnant women, which increased the generalizability of the findings. Moreover, as we developed survey questions based on standardized scales, the reliability of analyses was substantially improved. We acknowledged several possible limitations of our review. First, as our study design was cross-sectional, it is unable to conclude causality between risk factors and outcomes. Second, recall bias and social desirability response bias might be caused by the self-reported questionnaire. Third, the convenience sampling procedure used to select pregnant women was prone to bias. Moreover, we only obtained data from pregnant women seeking antenatal care at two hospitals; thus, our survey might not be completely representative of all pregnant women in Vietnam. Finally, while gathering quantitative statistics on a variety of health behaviors, we did not compile evidence on all aspects of pregnant women's lifestyles, for example, protein consumption or nutrition education.
Conclusion
To conclude, this study highlighted the remarkable gaps in self-care practices among our pregnant women, which were significantly associated with their mental well-being. Information sources, social support and childbirth expectation were major drivers for self-care practices. Social support-oriented consultancy and interventions should be warranted for improving behaviors and the mental well-being of pregnant women in Vietnam.
Availability of data and materials
The data that support the findings of this study are available from the Hanoi Medical University but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Hanoi Medical University (contact bach.ipmph2@gmail.com).
Abbreviations
- WHO:
-
World Health Organization
- PICSS:
-
Perinatal Infant Care Social Support
- SEM:
-
Structural equation modeling
- RMSEA:
-
Root Mean Square Error of Approximation
- CFI:
-
Comparative Fit Index
- SRMR:
-
Standardized Root Mean Square Residual
References
World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. World Health Organization; 2016. https://www.who.int/publications/i/item/9789241549912.
Górniaczyk A, Czech-Szczapa B, Sobkowski M, Chmaj-Wierzchowska K. Maternal health-related behaviours during pregnancy: a critical public health issue. Eur J Contracept Reprod Health Care. 2017;22(4):321–5.
Brand JS, Hiyoshi A, Cao Y, Lawlor DA, Cnattingius S, Montgomery S. Maternal smoking during pregnancy and fractures in offspring: national register based sibling comparison study. BMJ. 2020;368:l705.
Mojibyan M, Karimi M, Bidaki R, Rafiee P, Zare A. Exposure to Second-hand Smoke During Pregnancy and Preterm Delivery. Int J High Risk Behav Addict. 2013;1(4):149–53.
Dejong K, Olyaei A, Lo JO. Alcohol Use in Pregnancy. Clin Obstet Gynecol. 2019;62(1):142–55.
Riley EP, Infante MA, Warren KR. Fetal alcohol spectrum disorders: an overview. Neuropsychol Rev. 2011;21(2):73.
Popova S, Lange S, Probst C, Gmel G, Rehm J. Estimation of national, regional, and global prevalence of alcohol use during pregnancy and fetal alcohol syndrome: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e290–9.
Lange S, Probst C, Rehm J, Popova S. National, regional, and global prevalence of smoking during pregnancy in the general population: a systematic review and meta-analysis. Lancet Glob Health. 2018;6(7):e769–76.
Poudevigne MS, O’Connor PJ. A review of physical activity patterns in pregnant women and their relationship to psychological health. Sports Med. 2006;36(1):19–38.
Tesfaye G, Demlew D, G/tsadik M, Habte F, Molla G, Kifle Y, Gebreegziabhier G. The prevalence and associated factors of alcohol use among pregnant women attending antenatal care at public hospitals Addis Ababa, Ethiopia, 2019. BMC Psychiatry. 2020;20(1):337.
Addila AE, Bisetegn TA, Gete YK, Mengistu MY, Beyene GM. Alcohol consumption and its associated factors among pregnant women in Sub-Saharan Africa: a systematic review and meta-analysis’ as given in the submission system. Subst Abuse Treat Prev Policy. 2020;15(1):29.
de Wolff MG, Backhausen MG, Iversen ML, Bendix JM, Rom AL, Hegaard HK. Prevalence and predictors of maternal smoking prior to and during pregnancy in a regional Danish population: a cross-sectional study. Reprod Health. 2019;16(1):82.
Azene AG, Aragaw AM, Wubetie HT, Wassie GT, Tsegaye GW, Derebe MA, Mitiku HD. Dietary diversity among pregnant women and associated factors in Ethiopia: Systematic review and meta-analysis. PLoS One. 2021;16(6):e0251906.
Evenson KR, Wen F. National trends in self-reported physical activity and sedentary behaviors among pregnant women: NHANES 1999–2006. Prev Med. 2010;50(3):123–8.
Morton SM, Grant CC, Wall CR, Carr PEA, Bandara DK, Schmidt JM, Ivory V, Inskip HM, Camargo CA. Adherence to nutritional guidelines in pregnancy: evidence from the Growing Up in New Zealand birth cohort study. Public Health Nutr. 2014;17(9):1919–29.
Traylor CS, Johnson JD, Kimmel MC, Manuck TA. Effects of psychological stress on adverse pregnancy outcomes and nonpharmacologic approaches for reduction: an expert review. Am J Obstet Gynecol MFM. 2020;2(4):100229.
Accortt EE, Cheadle AC, DunkelSchetter C. Prenatal depression and adverse birth outcomes: an updated systematic review. Matern Child Health J. 2015;19(6):1306–37.
Guintivano J, Manuck T, Meltzer-Brody S. Predictors of Postpartum Depression: A Comprehensive Review of the Last Decade of Evidence. Clin Obstet Gynecol. 2018;61(3):591–603.
Vehmeijer FOL, Guxens M, Duijts L, El Marroun H. Maternal psychological distress during pregnancy and childhood health outcomes: a narrative review. J Dev Orig Health Dis. 2019;10(3):274–85.
Surita FG, Paulino DSM, Pinho-Pompeu M. Health-related Behaviors in Pregnancy: A Key to Achieve Better Outcomes. Rev Bras Ginecol Obstetr. 2020;42:121–3.
Baskin R, Hill B, Jacka FN, O’Neil A, Skouteris H. The association between diet quality and mental health during the perinatal period. A systematic review. Appetite. 2015;91:41–7.
Zuckerman B, Amaro H, Bauchner H, Cabral H. Depressive symptoms during pregnancy: relationship to poor health behaviors. Am J Obstet Gynecol. 1989;160(5):1107–11.
Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–57.
Rashid A, Mohd R. Poor social support as a risk factor for antenatal depressive symptoms among women attending public antennal clinics in Penang, Malaysia. Reprod Health. 2017;14(1):144.
Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol. 2010;202(1):5–14.
Akiki S, Avison WR, Speechley KN, Campbell MK. Determinants of maternal antenatal state-anxiety in mid-pregnancy: Role of maternal feelings about the pregnancy. J Affect Disord. 2016;196:260–7.
Azimi M, Fahami F, Mohamadirizi S. The relationship between perceived social support in the first pregnancy and fear of childbirth. Iran J Nurs Midwifery Res. 2018;23(3):235.
Gümüşsoy S, Keskin G, Çiçek Ö, Yiğitoğlu S, Kirazlı G, Yıldırım GÖ. Psychological problem areas of pregnant women diagnosed with abortus imminens as a result of assisted reproductive techniques: a comparative study. Perspect Psychiatr Care. 2021;57(1):73–81.
Nath A, Venkatesh S, Balan S, Metgud CS, Krishna M, Murthy GVS. The prevalence and determinants of pregnancy-related anxiety amongst pregnant women at less than 24 weeks of pregnancy in Bangalore, Southern India. Int J Women’s Health. 2019;11:241.
Chadwick KA, Collins PA. Examining the relationship between social support availability, urban center size, and self-perceived mental health of recent immigrants to Canada: a mixed-methods analysis. Soc Sci Med. 2015;128:220–30.
Faramarzi M, Pasha H. The role of social support in prediction of stress during pregnancy. J Babol Univ Medical Sci. 2015;17(11):52–60.
Feldman PJ, Dunkel-Schetter C, Sandman CA, Wadhwa PD. Maternal social support predicts birth weight and fetal growth in human pregnancy. Psychosom Med. 2000;62(5):715–25.
Collins NL, Dunkel-Schetter C, Lobel M, Scrimshaw SC. Social support in pregnancy: psychosocial correlates of birth outcomes and postpartum depression. J Pers Soc Psychol. 1993;65(6):1243.
Nylen KJ, O’Hara MW, Engeldinger J. Perceived social support interacts with prenatal depression to predict birth outcomes. J Behav Med. 2013;36(4):427–40.
Sanguanklin N, McFarlin BL, Park CG, Giurgescu C, Finnegan L, White-Traut R, Engstrom JL. Effects of the 2011 flood in Thailand on birth outcomes and perceived social support. J Obstet Gynecol Neonatal Nurs. 2014;43(4):435–44.
Waite L. Why marriage matters strengthening marriage round table. In: Washington DC: Springer; 1997.
Organization WH. Wellbeing measures in primary health care/the DEPCARE project: report on a WHO meeting, Stockholm, Sweden 12–13 February 1998. In: Wellbeing measures in primary health care/the DEPCARE project: report on a WHO meeting, Stockholm, Sweden 12–13 February 1998: 1998; 1998.
Mortazavi F, Mousavi S-A, Chaman R, Khosravi A. Validation of the World Health Organization-5 Well-Being Index; assessment of maternal well-being and its associated factors. Turk Psikiyatri Dergisi. 2015;26(1):1–7.
Leahy-Warren P, McCarthy G, Corcoran P. First-time mothers: social support, maternal parental self-efficacy and postnatal depression. J Clin Nurs. 2012;21(3–4):388–97.
Nguyen CL, Nguyen PTH, Chu TK, Van Ha AV, Pham NM, Van Duong D, Van Do D, Tang HK, Binns CW, Lee AH. Cohort profile: Maternal lifestyle and diet in relation to pregnancy, postpartum and infant health outcomes in Vietnam: a multicentre prospective cohort study. BMJ Open. 2017;7(9):e016794.
Van Minh H, Giang KB, Ngoc NB, Hai PT, Huyen DTT, Khue LN, Lam NT, Nga PTQ, Xuyen NT. Prevalence of tobacco smoking in Vietnam: findings from the Global Adult Tobacco Survey 2015. Int J Public Health. 2017;62(1):121–9.
Zamawe C, King C, Jennings HM, Mandiwa C, Fottrell E. Effectiveness and safety of herbal medicines for induction of labour: a systematic review and meta-analysis. BMJ Open. 2018;8(10):e022499.
Nguyen LT, Kaptchuk TJ, Davis RB, Nguyen G, Pham V, Tringale SM, Loh YL, Gardiner P. The use of traditional Vietnamese medicine among Vietnamese immigrants attending an urban community health center in the United States. J Altern Complement Med. 2016;22(2):145–53.
Fakeye TO, Adisa R, Musa IE. Attitude and use of herbal medicines among pregnant women in Nigeria. BMC Complement Altern Med. 2009;9(1):1–7.
Nascimento SL, Surita FG, Godoy AC, Kasawara KT, Morais SS. Physical activity patterns and factors related to exercise during pregnancy: a cross sectional study. PLoS One. 2015;10(6):e0128953.
Xiang M, Zhang J, Liang H, Zhang Z, Konishi M, Hu H, Nishimaki M, Kim H-K, Tabata H, Shimizu H. Physical activity and dietary intake among Chinese pregnant women: an observational study. BMC Pregnancy Childbirth. 2019;19(1):1–8.
Hailemariam TT, Gebregiorgis YS, Gebremeskel BF, Haile TG, Spitznagle TM. Physical activity and associated factors among pregnant women in Ethiopia: Facility-based cross-sectional study. BMC Pregnancy Childbirth. 2020;20(1):92.
Ha AVV, Zhao Y, Binns CW, Pham NM, Nguyen CL, Nguyen PTH, Chu TK, Lee AH. Low prevalence of folic acid supplementation during pregnancy: A multicenter study in Vietnam. Nutrients. 2019;11(10):2347.
Xing X-Y, Tao F-B, Hao J-H, Huang K, Huang Z-H, Zhu X-M, Xiao L-M, Cheng D-J, Su P-Y, Zhu P. Periconceptional folic acid supplementation among women attending antenatal clinic in Anhui, China: data from a population-based cohort study. Midwifery. 2012;28(3):291–7.
Yamamoto S, Wada Y. Awareness, use and information sources of folic acid supplementation to prevent neural tube defects in pregnant Japanese women. Public Health Nutr. 2018;21(4):732–9.
Kim M-H, Han J-Y, Cho Y-J, Ahn H-K, Kim J-O, Ryu H-M, Kim M-Y, Yang J-H, Nava-Ocampo AA. Factors associated with a positive intake of folic acid in the periconceptional period among Korean women. Public Health Nutr. 2009;12(4):468–71.
Grimes HA, Forster DA, Newton MS. Sources of information used by women during pregnancy to meet their information needs. Midwifery. 2014;30(1):e26–33.
Eriksson-Backa K. Who uses the web as a health information source? Health Informatics J. 2003;9(2):93–101.
Lowe P, Powell J, Griffiths F, Thorogood M, Locock L. “Making it all normal”: the role of the internet in problematic pregnancy. Qual Health Res. 2009;19(10):1476–84.
Lagan BM, Sinclair M, George Kernohan W. Internet use in pregnancy informs women’s decision making: a web-based survey. Birth. 2010;37(2):106–15.
Van den Bergh B, Simons A. A review of scales to measure the mother–foetus relationship. J Reprod Infant Psychol. 2009;27(2):114–26.
Harley K, Eskenazi B. Time in the United States, social support and health behaviors during pregnancy among women of Mexican descent. Soc Sci Med. 2006;62(12):3048–61.
Elsenbruch S, Benson S, Rücke M, Rose M, Dudenhausen J, Pincus-Knackstedt MK, Klapp BF, Arck PC. Social support during pregnancy: effects on maternal depressive symptoms, smoking and pregnancy outcome. Hum Reprod. 2007;22(3):869–77.
Caldeira V, Woodin EM. Social support as a moderator for alcohol-related partner aggression during the transition to parenthood. J Interpers Violence. 2012;27(4):685–705.
Masho SW, Do E, Adekoya S. Social support and smoking during pregnancy. J Women’s Health Care. 2014;3:1000179.
Ulrich F, Petermann F. Consequences and possible predictors of health-damaging behaviors and mental health problems in pregnancy–a review. Geburtshilfe Frauenheilkd. 2016;76(11):1136.
Ngo CQ, Phan PT, Vu GV, Chu HT, Nguyen TT, Nguyen MH, Phan HT, Ong BM, Vu GT, Pham KTH. Prevalence and sources of second-hand smoking exposure among non-smoking pregnant women in an urban setting of Vietnam. Int J Environ Res Public Health. 2019;16(24):5022.
Acknowledgements
The authors would like to acknowledge supports by all pregnant women who participated in the study.
Funding
This study was funded by NUS iHeathtech Other Operating Expenses (R-722–000-004–731) and NUS Department of Psychological Medicine Other Operating Expenses (R-177–000-003–001).
Author information
Authors and Affiliations
Contributions
LDN LHN LTN HTTN AND LGV HSAN SHN conceived of the study, and participated in its design and implementation and wrote the manuscript. LDN LHN LPD TMTV BXT CAL CSSH RCMH analyzed the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board of the Hanoi Obstetrics and Gynecology Hospital approved the study protocol (Code: 07 QD/PS-TTĐT). Participants were asked to give written or verbal informed consent and were informed that they could withdraw at any time. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nguyen, L.D., Nguyen, L.H., Ninh, L.T. et al. Women’s holistic self-care behaviors during pregnancy and associations with psychological well-being: implications for maternal care facilities. BMC Pregnancy Childbirth 22, 631 (2022). https://doi.org/10.1186/s12884-022-04961-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-04961-z