Abstract
Background
Caesarean section (CS) is an important medical intervention for reducing the risk of poor perinatal outcomes. However, CS trends in sub-Saharan Africa (SSA) continue to increase yet maternal and neonatal mortality and morbidity remain high. Rwanda, like many other countries in SSA, has shown an increasing trend in the use of CS. This study assessed the trends and factors associated with CS delivery in Rwanda over the past two decades.
Methods
We used nationally representative child datasets from the Rwanda Demographic and Health Survey 2000 to 2019–20. All births in the preceding 3 years to the survey were assessed for the mode of delivery. The participants’ characteristics, trends and the prevalence of CS were analysed using frequencies and percentages. Unadjusted and adjusted logistic regression analyses were used to assess the factors associated with population and hospital-based CS in Rwanda for each of the surveys.
Results
The population-based rate of CS in Rwanda significantly increased from 2.2% (95% CI 1.8–2.6) in 2000 to 15.6% (95% CI 13.9–16.5) in 2019–20. Despite increasing in all health facilities over time, the rate of CS was about four times higher in private (60.6%) compared to public health facilities (15.4%) in 2019–20. The rates and odds of CS were disproportionately high among women of high socioeconomic groups, those who resided in Kigali city, had multiple pregnancies, and attended at least four antenatal care visits while the odds of CS were significantly lower among multiparous women and those who had female babies.
Conclusion
Over the past two decades, the rate of CS use in Rwanda increased significantly at health facility and population level with high regional and socio-economic disparities. There is a need to examine the disparities in CS trends and developing tailored policy guidelines to ensure proper use of CS in Rwanda.
Similar content being viewed by others
Background
The burden for maternal and neonatal mortality remains disproportionately high in many low- and middle-income countries (LMICs) [1, 2]. About 99% of all global maternal deaths occurred in LMICs between 1990 and 2010 with an estimated two-thirds occurring in sub-Saharan Africa (SSA) [1, 2]. Despite the high maternal deaths in SSA, Rwanda recorded a 79% decline in maternal mortality ratio between 2000 and 2017 [1]. This reduction has been accelerated by increased access and use of skilled and competent care by women during the pregnancy continuum. However, about 73% of the global maternal deaths remain due to direct obstetric causes including obstetric interventions and complications [3] despite most of them being preventable. The provision of basic and comprehensive emergency obstetric and newborn care (EmONC) within a continuum of care is essential to reduce maternal and newborn morbidity and mortality [4, 5].
Caesarean section (CS) is an important comprehensive EmONC signal function and medical intervention for reducing risks of perinatal morbidity and mortality [6]. The proportion of delivery by CS is used to estimate the level of access and use of the intervention in saving maternal and child health at a population level [7]. Over the past few decades, global trends have shown a steady increase in CS use [8]. Gibbons and colleagues found that half of the countries surveyed globally had CS rates of above 15% [9] while Betran and colleagues estimated that by 2030, 29% of women will be giving birth through CS globally; about 7% in SSA and 63% in Eastern Asia [10]. Countries in SSA are also reporting high CS rates despite the high burden of preventable maternal and neonatal mortality [1]. However, huge disparities in CS use exist in SSA countries with some countries like South Sudan reporting rates lower than 1% while others like Ghana reporting a prevalence of 16% [11, 12].
These observed global increases in CS are driven majorly by medical and non-medical factors [6, 9]. Medically, CS deliveries are indicated in high risk conditions such as placenta previa, breech presentation, contracted pelvis, post-term pregnancy and hypertensive disorders [13]. However, CS deliveries have been conducted due to non-medical factors including maternal age, socioeconomic status, literacy levels, occupation, religion and culture [12, 14] and other demand-driven factors such as private practice and the cost of accessing CS [12]. In LMICs, the causes for the increasing CS use remain unclear though socioeconomic factors have been shown to contribute to the increase [6, 15]. The World Health Organization (WHO) recommends an optimal CS rate of 10–15% where rates below the lower limit suggest the unmet need for CS while rates above the upper limit suggest overuse of CS [16, 17]. The use of CS without medical indication is of no significance in reducing maternal and child mortality [6, 7], with recent evidence showing no beneficial effect of CS rates of above 10% on perinatal mortality rate [7].
Although Rwanda has made great strides in reducing maternal and child mortality in recent years, there is a risk of reversing these gains through the overuse of CS which has been associated with increased risk of adverse outcomes especially for constrained health systems in many LMICs [18, 19]. Rwanda, like many countries in SSA, has shown a consistent rise in the use of CS, which is estimated to account for between 13% [20] to 25.9% [21] of all deliveries. A recent study reported CS rates of 64% in private health facilities in Rwanda [11]. In addition, evidence indicates that if uncontrolled, the use of CS will continue to rise and with it the risk of adverse consequences [20]. Therefore, understanding the trends and patterns of CS use is the mainstay of preventing risks and developing context-specific evidence for policies to reduce maternal and neonatal mortality. However, comprehensive evidence on trends and patterns of CS use is lacking in Rwanda. This study used national-level data from the Rwanda Demographic and Health Survey between 2000 and 2019–20 to assess the trends and factors associated with CS delivery in Rwanda at both population and hospital levels.
Methods
Study setting
Rwanda is a low-income, agricultural and landlocked country with approximately 11 million people living in five regions covering an area of 26,338 km2 [21]. It has an average of 4.4 persons per household [22] and a gross domestic product per capita of US $780.80 [23]. About half (48%) of its population is under 19 years of age and 39% live below the poverty line with a life expectancy at birth of 71.1 years for women and an adult literacy rate of 80% among 15–49 years old women. In addition, 87.3% of the population has health insurance and access to health services; spending an average of 47.4 min to reach a health centre [21]. In 2016, CS in Rwanda were conducted in 27 (75%) of the 36 districts, provincial and referral hospitals [21].
Data source and sample
The study used the child datasets from the Rwanda Demographic Health Surveys (RDHS) conducted in 2000, 2005, 2010, 2014–15 and 2019–20 using stratified, two-stage cluster sampling [22, 24–27]. Households were stratified into urban or rural and all eligible women 15–49 years in selected households were interviewed using standard DHS questionnaires. All babies born within the preceding 3 years of each survey and with complete data were included in the population-based analysis while only babies delivered at a hospital were included in the hospital-based analysis. Of the 75,777 children born within the 3 years preceding each survey, 34,144 children were included after excluding 41,633 children with missing observations in the outcome variable as explained by the guide to DHS statistics [28] (Suppl. Fig. 1).
Measures
We conceptualized our study variables using the framework adapted from Kizito and Schuemacher [29] as shown in Fig. 1. The outcome variable was delivery by CS, which was categorized into “Yes” or “No”. Women were asked if they had been delivered by CS within the 3 years preceding the survey. Since it is possible for women to have more than one CS in 3 years, we used the participants’ unique identifiers and weighted samples to account for the clustering of CS. The explanatory variables included in the study were identified from a review of literature on factors associated with CS use [12, 14, 30–35]. Supplementary Table 1 operationalises these variables. The explanatory variables were categorised into maternal, child and household characteristics. Intervening variables were a set of variables acting on the explanatory variables and included access to information (Yes or No), place of delivery (private, public and home/others) and antenatal care (ANC) attendance (< 4 and ≥ 4 visits and missing). Maternal characteristics included residence (urban or rural), maternal age at birth (< 20, 20–34 and ≥ 35 years), education status (no formal, primary and secondary or higher), marital status (in-a-union and not-in-a-union), occupation (not working, agricultural and formal employment), parity (1, 2–4, ≥5) and region (East, West, South, North and Kigali City). Child characteristics included the weight of the baby (normal [2500-4000 g], low birth weight [< 2500 g] and big baby [> 4000 g]), low birth weight and big baby) [36], sex of the baby (male or female) and type of pregnancy (singleton or multiple). Household characteristics included household income and partner’s education (no formal, primary and secondary or higher).
Statistical analysis
We performed analyses of datasets using Stata version 17.0 (Stata Corporation, College Station, TX). We applied design based analysis using DHS sample weights and adjusted for sample errors using svy command. Participants’ characteristics and trends in the prevalence of CS were analysed using frequencies and percentages. To assess the factors associated with population-based and hospital-based CS, bivariate and multivariable logistic regression models were performed for each of the surveys. Variance inflation factor was used to assess multicollinearity. All variables included in the unadjusted model were hierarchically included in the adjusted model due to their importance in explaining CS and guided by the conceptual framework by Kizito and Schuemacher [29]. We reported both the unadjusted and adjusted odds ratios and considered significance at a p-value of less than or equal to 0.05. Only children with complete data were included in the analyses. The reporting in this study were guided by the STROBE guidelines for cross-sectional studies (Suppl. Table 3) [37].
Ethics
The study used anonymised open-access secondary data from the RDHS, which received ethical approvals from the Rwanda National Ethics Committee and the Institutional Review Board of ICF International. The data were accessed upon approval of data request to the DHS program and were used as per the data agreement. Additional information on the ethical approvals and processes for the surveys can be obtained from the published reports [21, 23–25].
Results
Respondents’ characteristics
Overall, the study included 34,144 children born within the 3 years preceding each survey (Suppl. Fig. 1). A majority of the children were born to middle-aged women (20–34 years), women who resided in rural areas, had a primary level of education, had two to four children, and had attended less than four ANC visits across the years. An almost equal proportion of participants lived in the West, East, and South provinces of Rwanda with the smallest proportion of participants living in Kigali City (Table 1).
Trends in the prevalence of CS in Rwanda
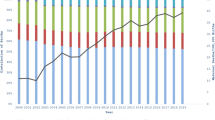
Overall, the rate of CS increased significantly from 2.2% (95% CI 1.8–2.6) in 2000 to 15.6% (95% CI 13.9–16.5) in 2019–20 (Fig. 2). The rate was consistently high among women 15–19 years of age, women residing in urban areas, those with secondary or higher levels of education, from the richest households, with access to information, on paid employment, and those who had one child, male babies, and multiple pregnancies across the years (Table 2).
We found regional disparities in the prevalence of CS across the years. Kigali city had a significantly higher prevalence than the other regions; with a three times increase in CS from 8.8% in 2000 to 26.4% in 2019–20. The Northern region had the lowest prevalence of CS despite a 10 times increase between 2000 (1.3%) and 2019–20 (13.2%) (Table 2).
There was an upward trend in the prevalence of CS in both public and private health facilities. The prevalence of CS in public facilities increased by about seven percentage points from 8.2% (95% CI 6.8–10.0) in 2000 to 15.4% (95% CI 14.1–16.8) in 2019–20. On the other hand, the rate of CS use was about four times high in private facilities from 13.6% (95% CI 7.4–23.8%) in 2000 to 60.6% (95% CI 47.2–72.5) in 2019–20; though the 2019–20 rate was a 20% decrease from the 2014–15 rate (Table 2). The prevalence of CS between public and private health facilities in 2010, 2014–15 and 2019–20 differed significantly despite having almost similar rates in 2005 (Table 2).
Factors associated with CS in Rwanda
Based on the unadjusted logistic regression models, there was an association between CS and residential area, education, employment, wealth, women’s age, access to media, parity, ANC attendance, multiple births, baby’s sex and birth weight (Suppl. Table 2).
Table 3 presents the results of the population-based multivariable logistic regression models for each of the four surveys. Overall, there were varied associations between CS and maternal age, occupation, wealth, ANC attendance, parity, sex and size of the child, and region of residence over the years. Across the surveys, women with multiple pregnancies, with ≥4 ANC visits, and from the richest households had higher odds of CS, while multiparous women and women with female babies had lower odds of CS. Women with female babies had 19–27% lower odds of CS compared to male babies between 2005 and 2019–20 while those with 5 or more children has 65–85% lower odds of CS compared to those with one child between 2010 and 2019–20. Women with multiple pregnancies had 3.2 to 6.5 times higher odds of CS than singleton pregnancy between 2005 and 2019–20.
In 2000, women working in the agricultural sector had lower odds of CS (aOR: 0.27, 95% CI 0.10–0.72), while in 2014, women in formal employment had higher odds of CS (aOR: 1.92, 95% CI 1.34–2.77). Partner education and marital status were associated with higher odds of CS in 2005 and 2010, respectively. In 2019–20, highest wealth quintiles, attendance of four or more ANC visits (aOR: 1.44, 95% CI 1.18–1.75), and multiple pregnancies (aOR: 3.24, 95% CI 1.84–5.70) were associated with higher odds of CS while residence in the North region (aOR: 0.62, 95% CI 0.40–0.96), having 5 or more children (aOR: 0.35, 95% CI 0.23–0.54) and female babies (aOR: 0.81, 95% CI 0.68–0.96) were associated with higher odds of CS (Table 3).
The results from the hospital-based model revealed a similar direction of association as those of the population-based model except for higher odds of CS among women who delivered big babies in 2000 (aOR: 2.00, 95% CI 1.11–3.61), 2014–15 (aOR: 1.57, 95% CI 1.22–2.03), 2019–20 and (aOR: 1.84, 95% CI 1.34–1.52) (Table 4).
Discussion
Over the past two decades, the rate of CS in Rwanda significantly increased from 2.2 to 15.6%, with disproportionately high rates among high socioeconomic groups and in urban areas, private health facilities and Kigali City. The rising trend in CS in Rwanda mirrors the global trend which shows an average annual increase of 4% [8]. The current CS rate of 15.6% in Rwanda is three times the rate in SSA, [10] and more than twice the average rate in Eastern and Southern African [38] though a previous study in Rwanda has shown a higher CS rate of 21% [39]. The increasing CS rate in Rwanda could indicate increased access to EmONC services and the high utilization of skilled delivery [40]. The current rate of CS is slightly above the 10–15% WHO threshold for beneficial CS and likely to continue increasing if measures are not taken. Importantly, despite a 20% decrease in the prevalence of CS in private hospitals between 2014 and 2019–20, there is a need to continue to monitor CS in private health facilities where the rate was four times higher compared to public health facilities in 2019–20.
Overall, women of high socioeconomic status (education, occupation, and wealth) had increased odds of CS delivery, which reflects findings from previous studies [11, 41–44]. CS is a high-cost procedure in most settings making it accessible mostly to the rich. However, in Rwanda, a majority of women are covered under the community-based health insurance schemes that have increased access to affordable healthcare by minimising the out-of-pocket expenditure and reducing the socioeconomic disparities in access and use of CS [20]. This is further evidenced by the increased proportion of institutional deliveries from 27%26 in 2000 to 28% [24], 69% [25], 91% [22] and 93% [21] in the year 2005, 2010, 2015 and 2019–20 respectively. Moreover, women with high education levels are associated with ANC attendance [43, 45, 46], providing them with an opportunity to receive health education and counselling and early detection of risks. Mothers with high-risk pregnancies are also more likely to utilise ANC services than those with normal pregnancies though ANC attendance could also be indicative of better access to healthcare including CS. Sayinzoga et al. further attributed improved maternal health services including access to CS use to established network of follow up for pregnant women, infrastructural development and proper leadership in health service delivery [47]. This could explain why about 75% of the districts in Rwanda provided CS services in 2016.
Multiple pregnancies are high-risk and one of the obstetric indications for CS [48, 49]. In our study, women with multiple pregnancies had higher odds of CS similar to previous studies [41, 50, 51]. In 2014, the rate of CS among women with multiple pregnancies was three times the average rate of CS in Rwanda, having doubled within the preceding five years. However, in 2019–20, the rate of CS among women with multiple pregnancies reduced by 10 percentage points while that of singleton significantly increased to 23.3%. Hence, there is a need to review the indication for CS among women with multiple and singleton pregnancies to guide clinicians on women who are likely to benefit from the procedure and avoid unnecessary CS in this group.
Our study found lower odds of CS delivery among women who gave birth to female babies compared to those who delivered male babies similar to previous studies [52–57]. Male babies tend to be heavier than female babies [58–60] and are at an increased risk of adverse pregnancy outcomes [58]. We also found that women with two or more children had lower odds of CS delivery compared to primiparous women. This finding is consistent with previous studies in Kenya [61] and Ethiopia [51] and could be possibly attributed to poor dissolution of cervical collagen fibre in primigravid women due to their inexperience in labour [62]. Also, women who may have delivered their first baby via CS may have had successful vaginal delivery after a previous CS [63].
Big babies in the population-based analyses had lower odds of CS but had higher odds of CS in the hospital-based analyses compared to normal-weight babies. Hospital-based studies have found a similar association between CS and big babies [64]. Large babies present difficulty in delivery possibly due to insufficient passage and prolonged labour. The lower odds of CS among big babies in the population-based analyses could be attributed to a delay in weighing of the babies delivered at home, who may have gained weight by the time of presenting at a health facility but also the fact that having a big baby is not an indication for CS and thus most big babies are delivered vaginally.
Our study adds to the evidence on CS in Rwanda by examining the population- and hospital-based trends and factors associated with CS in Rwanda over the past two decades using repeated nationally representative data making the findings generalisable to Rwanda. Our study, however, has some limitations that should be considered when interpreting the findings. First, there is a potential for overestimation or underestimation due to self-reporting of most variables and that the variables were measured at the time of the survey rather than at the time of delivery. Second, the dataset had missing observations and the study only included variables available from the dataset and could have missed important factors that predict CS in Rwanda. Finally, we could not assess the differences between the private and public health facilities due to the small sample of women who delivered in private health facilities.
Conclusion
Over the past 20 years, the rate of CS in Rwanda has seen an upward trend increasing seven times between 2000 and 2019–20 at health facility and population-level with persistent regional disparities over the years. The rates and odds of CS have been disproportionately high among women of high socioeconomic groups, and those who resided in urban areas and Kigali City, used private health facilities, had multiple pregnancies, and attended at least four antenatal care visits. Women in Rwanda seem to have increased access to and use of CS. However, the significant increase in the rate of CS is of concern due to the potential of unnecessary CS. Therefore, there is a need to examine the guidelines for CS use in Rwanda to ensure proper indications for use of CS are adopted for beneficial outcomes.
Availability of data and materials
The Rwanda Demographic Health Survey data used in this study is available on the Demographic Health Survey website at www.dhsprogram.com on request.
Abbreviations
- ANC:
-
Antenatal Care
- AOR:
-
Adjusted Odds Ratio
- BMI:
-
Body Mass Index
- CI:
-
Confidence Interval
- COR:
-
Crude Odds Ratio
- CS:
-
Caesarean Section
- DHS:
-
Demographic Health Surveys
- SSA:
-
Sub-Saharan Africa
- SDGs:
-
Sustainable Development Goals
- WHO:
-
World Health Organization
References
World Health Organization. Trends in maternal mortality 2000 To 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations population division. Geneva: World Health Organization; 2019. p. 104.
United Nations inter-agency Group for Child Mortality Estimation (UN IGME). Levels & Trends in child mortality: report 2020 - estimates developed by the UN inter-agency Group for Child Mortality Estimation. New York: United Nations Children's Fund; 2020.
Lawn JE, Blencowe H, Oza S, You D, Lee ACC, Waiswa P, et al. Every newborn: progress, priorities, and potential beyond survival. Lancet. 2014;384(9938):189–205.
Bullough C, Meda N, Makowiecka K, Ronsmans C, Achadi EL, Hussein J. Current strategies for the reduction of maternal mortality. BJOG. 2005;112(9):1180–8.
Campbell OM, Graham WJ, Lancet maternal survival series steering group. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368(9543):1284–99.
Betran AP, Torloni MR, Zhang JJ, Gulmezoglu AM, WHO working group on caesarean section. WHO statement on caesarean section rates. BJOG. 2016;123(5):667–70.
Betran AP, Torloni MR, Zhang J, Ye J, Mikolajczyk R, Deneux-Tharaux C, et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod Health. 2015;12:57.
Betrán AP, Ye J, Moller A-B, Zhang J, Gülmezoglu AM, Torloni MR. The increasing trend in caesarean section rates: global, regional and national estimates: 1990-2014. PLoS One. 2016;11(2):e0148343.
Gibbons L, Belizan JM, Lauer JA, Betran AP, Merialdi M, Althabe F. Inequities in the use of cesarean section deliveries in the world. Am J Obstet Gynecol. 2012;206(4):331.e331-e319.
Betran AP, Ye J, Moller AB, Souza JP, Zhang J. Trends and projections of caesarean section rates: global and regional estimates. BMJ Global Health. 2021;1;6(6):e005671.
Boatin AA, Schlotheuber A, Betran AP, Moller AB, Barros AJ, Boerma T, Torloni MR, Victora CG, Hosseinpoor AR. Within country inequalities in caesarean section rates: observational study of 72 low and middle income countries. bmj. 2018;360.
Yaya S, Uthman OA, Amouzou A, Bishwajit G. Disparities in caesarean section prevalence and determinants across sub-Saharan Africa countries. Global Health Res Policy. 2018;3:19.
Lavender T, Hofmeyr GJ, Neilson JP, Kingdon C, Gyte GM. Caesarean section for non‐medical reasons at term. Cochrane database of systematic reviews. 2012(3).
Nilsen C, Ostbye T, Daltveit AK, Mmbaga BT, Sandoy IF. Trends in and socio-demographic factors associated with caesarean section at a Tanzanian referral hospital, 2000 to 2013. Int J Equity Health. 2014;13(1):87.
Bayou YT, Mashalla YJS, Thupayagale-Tshweneagae G. Patterns of caesarean-section delivery in Addis Ababa, Ethiopia. Afr J Prim Health Care Fam Med. 2016;8(2):1–6.
World Health Organization. Appropriate technology for birth. Lancet. 1985;2:436–7.
Chu K, Cortier H, Maldonado F, Mashant T, Ford N, Trelles M. Cesarean Section Rates and Indications in Sub-Saharan Africa: A Multi-Country Study from Medecins sans Frontieres. PLoS One [Internet]. 2012;7(9):e44484. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0044484. [cited 2021 Aug 11].
Souza JP, Gülmezoglu AM, Lumbiganon P, Laopaiboon M, Carroli G, Fawole B, et al. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: the 2004-2008 WHO global survey on maternal and perinatal health. BMC Med. 2010;8(1):1–0.
Lumbiganon P, Laopaiboon M, Gülmezoglu AM, Souza JP, Taneepanichskul S, Ruyan P, et al. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007–08. Lancet. 2010;375(9713):490–9.
Odhiambo J, Ruhumuriza J, Nkurunziza T, Riviello R, Shrime M, Lin Y, et al. Health facility cost of cesarean delivery at a Rural District Hospital in Rwanda Using Time-Driven Activity-Based Costing. Matern Child Health J. 2019;23(5):613–22.
National Institute of Statistics of Rwanda (NISR). Rwanda Statistical Yearbook 2020. Kigali: National Institute of Statistics of Rwanda; 2020.
National Institute of statistics of Rwanda, finance Mo, economic planning/Rwanda, Ministry of Health/Rwanda, ICF international. Rwanda demographic and health survey 2014-15. Kigali: National Institute of statistics of Rwanda, Ministry of Finance and economic planning/Rwanda, Ministry of Health/Rwanda, and ICF International; 2016.
The World Bank. Macro poverty outlook country-by-country analysis and projections for the developing world spring meetings 2021. Washington DC: International Bank for Reconstruction and Development / The World Bank; 2021.
Institut national de la Statistique du Rwanda - INSR, ORC macro. Rwanda demographic and health survey 2005. Calverton: INSR and ORC Macro; 2006.
National Institute of Statistics of Rwanda - NISR, Ministry of Health - MOH/Rwanda, ICF International. Rwanda Demographic and Health Survey 2010. Calverton: NISR/Rwanda, MOH/Rwanda, and ICF International; 2012.
Office National de la Population - ONAPO/Rwanda, ORC Macro. Rwanda EnquÍte Démographique et de Santé 2000. Kigali: Ministére de la Santé, Office National de la Population and ORC Macro; 2001.
National Institute of statistics of Rwanda, Ministry of Health Rwanda, ICF international. Rwanda demographic and health survey 2019-20 final report. Kigali, Rwanda and Rockville, Maryland, USA: National Institute of Statistics of Rwanda and ICF International; 2021. p. 619.
Croft TN, Marshall AM, Allen CK, Arnold F, Assaf S, Balian S. Guide to DHS statistics. Rockville: ICF; 2018. p. 645.
Kizito O. Determinants of caesarean section rates in private-not-for-profit healthcare facilities: St. Joseph’s Hospital_ Kitovu. http://www.editorialmanager.com/cogentmed [Internet]. 2021 Jan 1 [cited 2022 Apr 21];8(1). Available from: https://www.tandfonline.com/doi/abs/10.1080/2331205X.2021.1928939
Wu JM, Viswanathan M, Ivy JS, North Carolina research collaborative on mode of D. A conceptual framework for future research on mode of delivery. Matern Child Health J. 2012;16(7):1447–54.
Jadoon B, Mahaini R, Gholbzouri K. Determinants of over and underuse of caesarean births in the eastern Mediterranean region: an updated review. East Mediterr Health J. 2019;25(11):837–46.
Azami-Aghdash S, Ghojazadeh M, Dehdilani N, Mohammadi M, Asl Amin Abad R. Prevalence and causes of cesarean section in Iran: systematic review and Meta-analysis. Iran J Public Health. 2014;43(5):545–55.
Gebreegziabher Hailu A, Kebede Fanta T, Tekulu Welay F, Etsay Assefa N, Aregawi Hadera S, Aregawi Gebremeskel G, et al. Determinants of cesarean section deliveries in public hospitals of Addis Ababa, Ethiopia, 2018/19: a case-control study. Obstet Gynecol Int. 2020;2020:9018747.
Hernandez-Vasquez A, Chacon-Torrico H, Bendezu-Quispe G. Differences in the prevalence of cesarean section and associated factors in private and public healthcare systems in Peru. Sex Reprod Healthcare. 2020;26:100570.
Karim F, Ali NB, Khan ANS, Hassan A, Hasan MM, Hoque DME, et al. Prevalence and factors associated with caesarean section in four hard-to-reach areas of Bangladesh: findings from a cross-sectional survey. PLoS One. 2020;15(6):e0234249.
Boulet SL, Alexander GR, Salihu HM, Pass MA. Macrosomic births in the united states: determinants, outcomes, and proposed grades of risk. Am J Obstet Gynecol [Internet]. 2003;188(5):1372–8. Available from: https://pubmed.ncbi.nlm.nih.gov/12748514/. [cited 2022 Apr 21].
Ev E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–8.
Boerma T, Ronsmans C, Melesse DY, Barros AJD, Barros FC, Juan L, et al. Global epidemiology of use of and disparities in caesarean sections. Lancet. 2018;392(10155):1341–8.
Kakoma JB. Cesarean section indications and anthropometric parameters in Rwandan nulliparae: preliminary results from a longitudinal survey. Pan Afr Med J. 2016;24.
Gurusamy PSR, Janagaraj PD. A success story: the burden of maternal, neonatal and childhood mortality in Rwanda - critical appraisal of interventions and recommendations for the future. Afr J Reprod Health. 2018;22(2):9–16.
Adewuyi EO, Auta A, Khanal V, Tapshak SJ, Zhao Y. Cesarean delivery in Nigeria: prevalence and associated factors-a population-based cross-sectional study. BMJ Open. 2019;9(6):e027273.
Cavallaro FL, Cresswell JA, Franca GV, Victora CG, Barros AJ, Ronsmans C. Trends in caesarean delivery by country and wealth quintile: cross-sectional surveys in southern Asia and sub-Saharan Africa. Bull World Health Organ. 2013;91(12):914–922D.
Leone T, Padmadas SS, Matthews Z. Community factors affecting rising caesarean section rates in developing countries: an analysis of six countries. Soc Sci Med. 2008;67(8):1236–46.
Taye MG, Nega F, Belay MH, Kibret S, Fentie Y, Addis WD, et al. Prevalence and factors associated with caesarean section in a comprehensive specialized hospital of Ethiopia: a cross-sectional study; 2020. Ann Med Surg (Lond). 2021;67:102520.
Nambile Cumber S. Importance of antenatal care services to pregnant women at the Buea regional hospital Cameroon. J Fam Med Health Care. 2016;2(4):23–9.
Chigbu CO, Iloabachie GC. The burden of caesarean section refusal in a developing country setting. BJOG. 2007;114(10):1261–5.
Sayinzoga F, Bijlmakers L. Drivers of improved health sector performance in Rwanda: a qualitative view from within. BMC Health Serv Res. 2016;16(1):1–0.
Robson MS. Classification of caesarean sections. Fetal Matern Med Rev. 2001;12(1):23–39.
Robson MS. Use of indications to identify appropriate caesarean section rates. Lancet Glob Health. 2018;6(8):e820–1.
Akinola OI, Fabamwo AO, Tayo AO, Rabiu KA, Oshodi YA, Alokha ME. Caesarean section--an appraisal of some predictive factors in Lagos Nigeria. BMC Pregnancy Childbirth. 2014;14(1):217.
Yisma E, Smithers LG, Lynch JW, Mol BW. Cesarean section in Ethiopia: prevalence and sociodemographic characteristics. J Matern Fetal Neonatal Med. 2019;32(7):1130–5.
Antonakou A, Papoutsis D. The effect of fetal gender on the delivery outcome in primigravidae women with induced labours for all indications. J Clin Diagn Res. 2016;10(12):QC22.
Bekedam DJ, Engelsbel S, Mol BW, Buitendijk SE, van der Pal-de Bruin KM. Male predominance in fetal distress during labor. Am J Obstet Gynecol. 2002;187(6):1605–7.
Khalil MM, Alzahra E. Fetal gender and pregnancy outcomes in Libya: a retrospective study. Libyan J Med. 2013;8(1).
Liu Y, Li G, Zhang W. Effect of fetal gender on pregnancy outcomes in northern China. J Matern Fetal Neonatal Med. 2017;30(7):858–63.
Schildberger B, Leitner H. Foetal gender and obstetric outcome. Geburtshilfe Frauenheilkd. 2016;76(3):255–60.
Weissmann-Brenner A, Simchen MJ, Zilberberg E, Kalter A, Dulitzky M. Combined effect of fetal sex and advanced maternal age on pregnancy outcomes. Med Sci Monit. 2015;21:1124–30.
Di Renzo GC, Rosati A, Sarti RD, Cruciani L, Cutuli AM. Does fetal sex affect pregnancy outcome? Gend Med. 2007;4(1):19–30.
Dunn L, Prior T, Greer R, Kumar S. Gender specific intrapartum and neonatal outcomes for term babies. Eur J Obstet Gynecol Reprod Biol. 2015;185:19–22.
Sheiner E, Levy A, Katz M, Hershkovitz R, Leron E, Mazor M. Gender Does Matter in Perinatal Medicine. Fetal Diagn Ther. 2004;19(4):366–9.
van der Spek L, Sanglier S, Mabeya HM, van den Akker T, Mertens PLJM, Houweling TAJ. Socioeconomic differences in caesarean section – are they explained by medical need? An analysis of patient record data of a large Kenyan hospital. Int J Equity Health. 2020;19(1):117.
Vrouenraets FP, Roumen FJ, Dehing CJ, van den Akker ES, Aarts MJ, Scheve EJ. Bishop score and risk of cesarean delivery after induction of labor in nulliparous women. Obstet Gynecol. 2005;105(4):690–7.
Kalisa R, Rulisa S, van Roosmalen J, van den Akker T. Maternal and perinatal outcome after previous caesarean section in rural Rwanda. BMC Pregnancy Childbirth. 2017;17(1):272.
Tarimo CS, Mahande MJ, Obure J. Prevalence and risk factors for caesarean delivery following labor induction at a tertiary hospital in North Tanzania: a retrospective cohort study (2000-2015). BMC Pregnancy Childbirth. 2020;20(1):173.
Acknowledgements
We thank Measure DHS for granting us access to the data.
Funding
This study did not receive any funding.
Author information
Authors and Affiliations
Contributions
PMK and LN conceptualised the study and obtained the data. CA, JO, GM and SG analysed the data and interpreted the results. All the authors wrote and reviewed the initial drafts and approved this final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study used anonymised secondary data from the RDHS, which received ethical approval from the Rwanda National Ethics Committee and the Institutional Review Board of ICF International [21, 23–25]. All data collection procedures were performed in accordance with the declaration of Helsinki on protection of human subjects. We accessed the data upon approval of request to the DHS program and were used as per the data agreement.
Consent for publication
Not applicable.
Competing interests
Authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Figure 1
: Flowchart of the study sample.
Additional file 2: Supplementary Table 1
. Operational definition of the study variables.
Additional file 3: Supplementary Table 2
. Factors associated with caesarean section at population level.
Additional file 4: Supplementary Table 3
. STROBE Statement—Checklist of items that should be included in reports of cross-sectional studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kibe, P.M., Mbuthia, G.W., Shikuku, D. et al. Prevalence and factors associated with caesarean section in Rwanda: a trend analysis of Rwanda demographic and health survey 2000 to 2019–20. BMC Pregnancy Childbirth 22, 410 (2022). https://doi.org/10.1186/s12884-022-04679-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-04679-y