Abstract
Background
Preconception care (PCC) is care prior to conception to optimize parental health, and health of the future child, through biomedical and behavioral changes. Providing PCC to all women with a wish to conceive will improve perinatal health. PCC is especially important for women with a chronic disease, such as inflammatory bowel disease (IBD) and rheumatic diseases (RD). At present PCC is not part of routine care for these women. The aim of this study is to identify facilitators and barriers on a patient and professional level regarding the provision of PCC in women with IBD and RD.
Methods
An explorative survey study among women with IBD and RD, their treating physicians and obstetric professionals was performed. Patients with a wish to conceive, pregnant women or those with a recent pregnancy (< 1 year ago) visiting the outpatient clinic of a secondary and tertiary hospital and involved physicians and obstetric professionals were eligible.
Results
A total of 71% of the IBD patients (n = 22/31) and 35% of the RD patients (n = 20/58) received a PCC consultation. PCC consultation was considered easy to enter, short in time and patients felt comfortable. Patients (71% IBD; 62% RD) preferred a personal PCC consultation with their disease specific specialist together with an obstetrician. Patients specifically wanted to receive information about the safety of medication use and disease activity following delivery. Of the included healthcare professionals 67% (n = 31) agreed PCC was applicable to their patients. Main barrier to providing PCC was lack of time and unavailability of professionals. In total 41% (n = 16) of obstetric professionals felt they had the knowledge and skills to provide PCC compared to 33% (n = 1) and 75% (n = 3) of gastroenterologists and rheumatologists, respectively.
Conclusion
Lack of awareness and urgency for the effectuation can be seen as important barriers for implementation of PCC. Due to the explorative nature generalisation of the results is not allowed. In the future, adaptation of the curricula of healthcare professionals by implementing interventions for pregnancy planning and preparation will generate awareness. Modelling of the impact of PCC might prove useful in resolving the lack of urgency for PCC realization.
Similar content being viewed by others
Background
Preconception care (PCC) is care prior to conception for all women or couples to optimize parental health and the health of the future child through biomedical and behavioral changes [1]. General PCC involves counselling, health promotion and risk reduction. General practitioners (GPs) and midwives are usually responsible for providing general PCC. Women receive advice about folic acid supplementation and optimal lifestyle [2,3,4]. For women suffering from chronic diseases specialized PCC should be offered by a gynecologist or disease specific specialist [5]. Patients should be counseled on how their disease can affect pregnancy and the risks of pregnancy associated with their disease [6].
Specialized PCC is especially important for women with chronic diseases, like inflammatory bowel disease (IBD) and rheumatic diseases (RD). IBD, Crohn’s disease (CD) and ulcerative colitis (UC), is often diagnosed at a reproductive age, 50% being diagnosed before the age of 35 [7]. The presence of active disease during pregnancy is one of the most important risk factors for adverse pregnancy outcomes like spontaneous miscarriage, preterm delivery and low birth weight [8, 9]. Ideally, the disease should be in remission at least 6 months before conception. Lack of knowledge results in incorrect beliefs regarding pregnancy. The study from Ellul et al. showed that > 60% of the patients believed IBD might lead to a complicated pregnancy and the disease itself or medication use could cause harm to the fetus [10]. Walldorf et al. showed that there is significantly more childlessness amongst women with IBD and stress the importance of qualified counselling as early as possible [11]. Providing PCC in women with IBD is associated with medication compliance, reduced disease relapse during pregnancy and a protective factor for having children with a low birth weight and therefore a better outcome of pregnancy [12].
PCC is also essential for women with rheumatoid arthritis (RA). Despite remission of this auto-immune disease during pregnancy, more than half of the RA patients experience active disease during the third trimester. Low disease activity before pregnancy is associated with low disease activity during pregnancy [13]. Whereas high disease activity in women with RA can be associated with infertility and low birthweight [14, 15]. Therefore, it is important that the disease is in remission before conception.
A study by Chakravaty et al. regarding family planning in women with systemic inflammatory diseases, like IBD and RD, reported that patients had a preference for receiving PCC from a gynecologist. A disease specific specialist should only be involved for the treatment of the underlying chronic condition. Only a minority of the disease specific specialists reported providing PCC to female patients of reproductive age [16]. Hence, women with systemic inflammatory diseases are in need of consistent information about disease specific pregnancy risks which their disease specific medical specialists do not routinely provide.
It is important to improve the quality of specialized PCC and to ensure that PCC is available for patients with a chronic inflammatory disease at risk for pregnancy complications due to their underlying disease. The aim of this explorative survey study is to identify facilitators and barriers on a patient and healthcare professional level regarding PCC in women with IBD and RD.
Methods
Study design
The PPCD (Pregnancy Preparation for women with Chronic Diseases) study is an explorative survey study (MEC-2016-368). Questionnaires on a patient and professional level (additional files 1, 2, 3, 4 and 5) were used to identify the facilitators and barriers of PCC. These questionnaires were based on earlier validated questions from the HP4All2 study (MEC–2015–182, Healthy pregnancy 4 All-2, subproject protocol C ‘interconception care’) which focused on the effectiveness of programmatic PCC and systematic antenatal risk assessment by introducing and offering PCC to women visiting family clinics in the Netherlands [17]. Women eligible were between 18 and 42 years of age and visiting the outpatient clinic for their specific disease (i.e. IBD and RD). Their actual wish to conceive was asked. They had an actual or nearby future (< 1 year) wish to conceive, were pregnant or recently gave birth (< 1 year ago). Patients with a poor understanding of the Dutch language were excluded.
Healthcare professionals (medical specialists, residents, house-officers, midwives and consultants) working in the collaborating departments (i.e. Gastroenterology, Rheumatology and Obstetrics & Gynecology) were also asked to participate.
Study setting
Women were recruited from the departments of Gastroenterology and Obstetrics and Gynecology of a secondary hospital (Francisus Gasthuis & Vlietland, Rotterdam) and the departments of Gastroenterology, Rheumatology and Obstetrics and Gynecology of a tertiary hospital (Erasmus Medical Center, Rotterdam).
Study procedure
Women who met the inclusion criteria were asked to participate in this study during an outpatient visit with their disease specific specialist. They received an information letter and an informed consent form. Only after informed consent did participating patients receive an e-mail with a link to the online questionnaire using Lime Survey, which is an online tool for sending out questionnaires to specific groups. The questionnaire was completely anonymous. Healthcare professionals also received an e-mail with a link to another anonymous, online questionnaire.
Both questionnaires included questions to identify baseline characteristics (client level: 27 questions; professional level: 5 questions); facilitators and barriers of PCC (client level: 25 questions; professional level: 9 questions); knowledge, attitude and actions towards PCC (client level: 13 questions; professional level: 9 questions) and the most ideal form of a preconception consultation (i.e. a personal or a skype consultation) (client level: 2 questions; professional level: 9 questions). In the analysis responses to questions were translated into facilitators or barriers. For example: ‘How easy/difficult is it for you to visit a PCC consultation?’. This question was answered with a four-point scale from ‘very easy’ to ‘very difficult’ whereby very difficult and difficult were seen as barriers and very easy and easy as facilitators. Facilitators and barriers were reported for the domains: personal, medical, organizational and financial. Knowledge was arbitrarily judged as adequate if a patient had a score of > 80% correct answers [18, 19].
Statistical analysis
IBM SPSS Statistics version 24 was used to analyze data from both questionnaires. The baseline characteristics were determined for both patients and healthcare professionals. Frequency tables were used to analyze categorical and continuous data. Cross tables were used to report the results for knowledge, attitude and actions towards PCC. By analyzing the answers to both questionnaires, facilitators and barriers of PCC in women with IBD and RD were identified. All reported answers were considered as important and contributing to the questions and therefore included for analysis.
Study sample
Every year approximately 90 patients meeting our inclusion criteria are referred to the outpatient clinic of the department of Rheumatology at the tertiary hospital. Further, approximately each year 40 eligible IBD patients are referred to the outpatient clinics of the departments of both (secondary and tertiary) participating hospitals. We planned for an inclusion period of 1 year.
Results
Results at a patient level
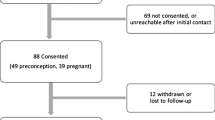
At the outpatient clinic 36 women with IBD and 63 women with RD were asked to participate. Eventually, the questionnaire was filled in by 31 women with IBD and 58 women with RD. Hence, the response rate was 92% for women with RD and 86% for women with IBD respectively. One response in the IBD group and six responses in the RD group were incomplete (missing 3.4%). The baseline characteristics of both groups are shown in Table 1. The majority of our patients were of Western origin. In total 55% (n = 17) of the women in the IBD group had CD and 42% (n = 13) had UC. The most common RD in our patients were RA (36%, n = 21) and ankylosing spondylitis (21%, n = 12). Regarding obstetric history, previous miscarriages were reported in 19% (n = 6) of women with IBD and in 32% (n = 18) of women with RD. At the time of enrollment 32% (n = 10) of the women in the IBD group and 45% (n = 26) of the women in the RD group were pregnant.
Facilitators and barriers of PCC reported by patients with IBD and RD are shown in Table 2. On a personal level, multiple facilitators were found. Women in both groups said visiting a PCC consultation would be easy to enter ((90%, n = 28 IBD) and (86%, n = 50 RD)). The majority of women with IBD and RD felt comfortable visiting a PCC consultation and did not think it took too much time. An important reason to visit a PCC consultation was a good preparation for pregnancy which was reported by 74% (n = 23) of women with IBD and 74% (n = 43) of women with RD.
On a medical level, the course of a previous pregnancy and the healthcare professional referring for PCC can be seen as facilitators for PCC. In 4 out of 13 IBD and 6 out of 36 RD patients a previous pregnancy coincided with adverse events. The adverse pregnancy outcome corresponded with a positive attitude to PCC. Furthermore, the advice to visit a PCC consultation when given by a disease specific specialist was considered of higher value in both groups compared to receiving the advice for PCC from a gynecologist, midwife or GP.
On an organizational level the majority of the patients in both groups prefer to see PCC posters everywhere. On a financial level 90% (n = 28) of women with IBD and 85% (n = 49) of women with RD said PCC consultations should be available for free.
In both groups the preferred healthcare professional to provide PCC was the gynecologist and in second place from their disease specific specialist (gastroenterologist or rheumatologist). The most ideal form of a PCC consultation was a personal combined consultation from both their disease specific specialist and gynecologist (Table 3).
Knowledge, attitude and actions towards general PCC of women with IBD and RD are described in an additional file (additional file 6). General knowledge on folic-acid supplementation was up to date in both groups as more than 80% understood the benefits of folic-acid supplementation. General knowledge on the effect of smoking on fertility was not up to date as less than 80% knew about the association with infertility.
The questionnaire also focused on the content of information patients would like to receive during a PCC consultation. Most of them wanted to receive information about medication use during pregnancy (97%, n = 30 IBD; 78%, n = 45 RD). Other important topics to be discussed were information about their disease after delivery and breastfeeding when using medication. In total 71% (n = 22) of the women with IBD and 35% (n = 20) of the women with RD visited a PCC consultation. They all felt that their questions were answered adequately and the majority found the consultation useful.
Results at a professional level
The online questionnaire was sent to healthcare professionals from the involved departments. Responses were received from 39 professionals from the department of Obstetrics and Gynecology, three from the department of Gastroenterology and four from the department of Rheumatology. Not all questionnaires were filled in completely (missing 5.4%). The baseline characteristics of the respondents are shown in additional file 7.
Facilitators and barriers of PCC were identified on an organizational and personal level (Table 4). At an organizational level, shortage of healthcare professionals (62%, n = 24) and lack of time (54%, n = 21) to provide PCC were reported as barriers by respondents from the department of Obstetrics and Gynecology. Only one respondent from the department of Gastroenterology and none of the respondents from the department of Rheumatology reported lack of time. At a personal level 64% (n = 25) of the obstetric professionals agreed that from a healthcare professionals’ perspective, PCC was applicable to their patients which was in agreement with the respondents from the departments of Rheumatology and Gastroenterology.
Knowledge, attitude and actions of healthcare professionals towards PCC are described in Table 5. From the Obstetrics and Gynecology department 41% of the respondents (n = 16) felt they had sufficient knowledge and skills to provide PCC. For the departments of Rheumatology and Gastroenterology this was the case in respectively 33% (n = 1) and 75% (n = 3).
Figure 1 (insert Fig. 1) shows which healthcare professionals were considered most suitable by healthcare professionals to provide PCC. In both women with IBD and RD the gynecologist and the disease specific specialist were mentioned as most suitable. Midwives and GPs were considered less suitable to provide PCC.
Healthcare professionals’ point of view: professionals suitable for PCC in women with IBD/RD. The profession of the healthcare professionals included in the answer to this question, depicted at the bottom of the figure, are respectively a gynecologist, a disease specialist, a midwife and a general practitioner. Ranking was performed according to a 5-point scale from ‘most certainly’ to ‘most certainly not’. Percentages were calculated based on number of respondents who filled in: ‘most certainly’ and ‘certainly’. The percentages reflect the suitability of the professional to provide PCC to women with IBD/RD according to the healthcare professionals, reflected as respondents, from respectively the department of Gastroenterology (dark blue), department of Rheumatology (blue) and department of Obstetrics and Gynecology (light blue)
Discussion
Main findings
Facilitators and barriers have been reported on a patient and healthcare professional level. Patients seem to have a positive attitude towards PCC. They are interested in receiving information about the impact of their disease on pregnancy and vice versa. Furthermore, they prefer to receive information about their medication use during pregnancy and lactation. The professionals also have a positive attitude towards PCC as they think it is important to contribute to PCC and they see the need for PCC for their patients. Despite the positive attitude towards PCC on a client and professional level, realization of PCC remains difficult.
Comparison to other studies
Studies have shown that women in general are interested in PCC and have a positive attitude towards PCC, however the uptake of PCC is low [3, 20]. The majority of women are hesitant about seeking PCC themselves, because they do not consider themselves part of the target group [3]. Our study found that 71% of the women in the IBD group experienced they had received a PCC consultation which is, crucial to mention, part of standard of care for women with IBD visiting the Department of Gastroenterology of our tertiary hospital. Only 35% of women with RD mentioned they received a PCC consultation. However, providing PCC, is standard of care in the outpatient department of RD of the tertiary hospital (additional file 6). These findings may be explained by variations in patient experience regarding discussion of the topic “pregnancy and pregnancy preparation” with their treating doctors.
Poels et al. reported several facilitators and barriers for general PCC. Some of the barriers identified were anxiety and fear of PCC, not being offered PCC and time and effort to visit a PCC consultation [20]. These were not identified as barriers in our study. The majority felt comfortable to visit a PCC consultation or thought such consultation did not take too much time. This could be due to the selected group of women who participated in our survey study.
The study from Chakravarty et al. showed that 32–56% of the gastroenterologists and rheumatologists routinely provided PCC to women of childbearing age [16]. Our study found that 67% of the gastroenterologists and 50% of the rheumatologists would provide PCC to all women who visit the clinic for routine care. However, the low number of included disease specific specialists of both departments in this study could affect these results.
Studies from Goossens et al. and M’Hamdi et al. about facilitators and barriers of PCC reported by healthcare providers mentioned more barriers than facilitators, including lack of knowledge and lack of time [21, 22]. This is partly in line with our findings. Some of the healthcare professionals reported to have lack of knowledge and time to provide PCC (Tables 4-5). Therefore, more information about PCC should be provided to healthcare professionals and more time should be created to implement PCC as part of standard-care.
A study regarding knowledge on folic acid supplementation showed that patients’ knowledge on this topic has increased over the years but remains limited. A study from Temel et al. showed an increase in knowledge from 30.7 to 36.8% in 2 years time [19]. In our study knowledge on folic acid supplementation was up to date in women with IBD and RD with more than 80% correct answers. On the contrary, knowledge of the effect of smoking on fertility was not up to date with less than 80% correct answers. These findings were supported by another study which showed that the majority of patients thought smoking did not affect fertility [23]. Several studies have shown that smoking by men and women is associated with delayed conception and adverse pregnancy outcomes [24,25,26]. The topics of folic acid supplementation and smoking should always be addressed during a PCC consultation.
In this study, we assessed patients’ knowledge using four questions from a validated Dutch questionnaire. However, it should be mentioned the CCPKnow (Crohn’s and Colitis Pregnancy Knowledge) score is available as a validated tool assessing patients’ knowledge [27]. Moreover, this educational tool has significantly improved IBD specific knowledge in patients.
Relevance of the findings
Research has shown that women are hesitant about seeking PCC themselves and only a minority of primary caregivers in the Netherlands recommends PCC in the form of a dedicated consultation [3, 4]. This study shows that only 28% (n = 11) of the healthcare professionals from the department of Obstetrics and Gynecology would provide PCC to all women of childbearing age. The majority (74%, n = 34) would provide PCC to women with known risk factors or questions about a future pregnancy (Table 5). Hence, a considerable group of women with an increased risk of pregnancy complications who would potentially benefit from a PCC consultation, do not receive this form of care. Hence, following this survey study aiming to provide PCC to all women of childbearing age, we would like to suggest at least to disease specific specialists that mentioning PCC to their patients generating awareness of the existence and importance of this kind of care is an urgent matter. Further, GPs and midwives could play a key role during everyday practice stating the availability and importance of a PCC consultation during routine appointments. Lastly, considering the lack of knowledge mentioned by the professionals, professionals could receive training on the importance of PCC and the possibilities how to deliver PCC to all women of childbearing age.
PCC can be provided by various healthcare professionals. Our patients preferred to receive PCC from either a gynecologist or their disease specific specialist. A personal consultation with both specialists was reported as the ideal form of a PCC consultation (Table 3). We consider collaboration between the departments of Rheumatology and Obstetrics and Gynecology at the Erasmus MC as best practice, as healthcare professionals already participate in multidisciplinary consultations and preconceptional referral of patients with a wish to conceive. At the moment, the department of Obstetrics and Gynecology and the department of Gastroenterology have separate PCC consultations in the Erasmus MC. We would recommend closer collaboration between both departments to improve the quality of PCC. Sellinger et al. describe how to provide guidance for clinicians involved in the care of pregnant patients with IBD [5]. They mention that close collaboration and joint decision-making between IBD and obstetric teams is necessary for optimal care. These recommendations are supported by the findings of Kashkooli et al. who show that compared to gastroenterologists, gynecologists have inferior knowledge on IBD and reproduction [28]. Healthcare professionals from different hospitals in the South-West of The Netherlands have developed a IBD health care pathway using uniform working methods and protocols resulting in more optimal and efficient care for patients [29]. Such mutual collaborations will be helpful to overcome issues evolving due to the lack of knowledge between healthcare professionals from different backgrounds. In addition, recent studies from Atrash and Jack describe several evidence-based clinical interventions and guidelines for PCC implementation which can be useful to further optimize multidisciplinary PCC consultations [30,31,32].
Lack of awareness of PCC has been reported in different studies as a barrier [20,21,22]. One patient said she never knew about the existence of PCC and she would have liked to know about disease related complications before her first pregnancy. The majority of our women with IBD or RD reported that PCC posters should be used to alert women in, amongst others, the waiting room of the midwife/GP. Sijpkens et al. showed that visual information in waiting rooms could result in an increased number of women visiting a PCC consultation [33].
Research regarding the opportunities to improve preconception counseling for those not yet planning a pregnancy should be performed. Also we believe, to improve womens’ knowledge on pregnancy preparation all healthcare professionals should take responsibility and ask women of childbearing age for a future wish to conceive. In addition, Sijpkens et al. following an international expert meeting on interconception care, showed that as a start for the implementation of PCC one should start talking about a future wish to conceive with women of fertile age whenever you have the chance to do so [34].
It is important to state the financial organization of the healthcare system in the Netherlands differs when compared to other countries. To visit a medical specialist a financial fee is covered by the mandatory social health insurance plan, so PCC is covered for all women who are treated by a medical specialist. Due to the course of the medical treatment for IBD and RD a financial motive involved as an organizational barrier for our participants is absent. This is in contrast to the financial organization of the healthcare system in the United Kingdom (UK) where there is a dependence on government funding [35]. Further, according to the organization of community based specialty care systems such as in the US/Australia with insured medical specialist care at patients’ request implementation of PCC may also be hampered by a financial barrier.
Moreover, researchers from the UK proposed an annual report card using metrics from multiple routine data sources as to hold governments and other stakeholders to account for delivering interventions, focusing on a population level as well as on an individual level, to improve preconception health [35]. As part of planning and preparation for a pregnancy, at an individual level, interventions should focus on conversations about pregnancy intention for which the training curricula of health care professionals should be adapted [35]. Additionally, implementation of training programs for patients and for both health and non-health professionals is also suggested as a solution to facilitate effective PCC by others [36, 37].
Strengths and limitations
One of the strengths of this study was the use of validated questions (based on the HP4All2 study) to identify facilitators and barriers of PCC [17]. Questionnaires were anonymous and easily accessible online. Questionnaires were filled in by patients and healthcare professionals, therefore facilitators and barriers could be identified on both levels. Furthermore, this study involved different areas of interest (department of Obstetrics and Gynecology, Gastroenterology and Rheumatology).
There were 46 healthcare professionals who filled in the questionnaire. Unfortunately, numbers of disease specialists included were low which can be seen as a limitation of the study. Due to the anonymity of the questionnaires, it was not possible to send personal reminders to fill in the questionnaires. However, in this study, we included a variety of healthcare professionals involved in PCC for women with IBD and RD, reflected by the qualification of the professionals as stated in additional file 7. The diversity of the included professionals adds to the strength of our study.
We were limited by the number of inclusions, as not all women visiting the outpatient clinics fulfilled our inclusion criteria. Also, we were dependent on the voluntary participation of women (with a chronic disease) further limiting our number and increasing our inclusion period beyond the calculated duration of the study.
Although the number of subjects did not meet our required sample size, the number of women included in our explorative study (58 women with RD and 31 women with IBD) is sufficient to identify facilitators and barriers of PCC for this specific group. The explorative nature provides a descriptive analysis and does not allow for generalisation of the results. The high response rate of the included participants (i.e. 92 and 86% for women with RD and IBD respectively) shows the included patients are highly motivated to share their opinion on facilitators and barriers regarding PCC which adds to the importance of this topic from their point of view. Yet, this study gives a good reflection of the way women with RD and IBD think about PCC and how they prepare themselves for a future pregnancy. Information on the exact status of the severity of the disease was not provided which can be seen as a limitation. Performing the study in a secondary and tertiary hospital the participants included reflect a representative population of women with IBD and RD.
We found that 71% of the patients with IBD visited a PCC consultation compared to 35% of the clients with RD. The study started in the RD group, later followed by the IBD group. In the first questionnaire we used a different word for a ‘preconception consultation’ which could have been misinterpreted by women. Moreover, this could be the reason for missing data on this question. During the study we substituted this word to a clearer word for ‘preconception consultation’ aiming for improved understanding of our survey question. In addition, despite the description of PCC in the questionnaire, it is possible women were not aware that PCC can be provided by various healthcare professionals such as for example their disease specific specialist. It is possible a larger number did receive PCC or were provided specific preconception information, which was not experienced as such, which can be seen as a limitation. Another explanation for the lower percentage of PCC in the RD group is the fact that many of the women visiting the outpatient clinic of Rheumatology were referred to the tertiary hospital after they had become pregnant subsequently lacking the opportunity to provide PCC in this center.
Finally, women reported they had to answer questions about a previous pregnancy, even though some of them had never been pregnant. It was not possible to skip the questions, so they answered that they did not have any problems during a previous pregnancy. This limitation for data interpretation was taken into account when constructing the results.
In this study, we included women with an actual or nearby future (< 1 year) wish to conceive, pregnant women or women who had recently given birth (< 1 year ago) which can be seen as a selection bias not including women without making plans for a pregnancy. However, answering the anonymous questionnaire some women reported a wish to conceive only after a period of 12 months or longer (Table 1). We consider these women not making actual plans also as important to answer the aim of our study due to their future child wish.
Conclusion
Facilitators and barriers have been reported on a patient and healthcare professional level. Lack of awareness of the topic of PCC in patients and lack of urgency for the effectuation of PCC can be seen as important barriers for implementation of this form of fundamental care in routine clinical practice. Due to the explorative nature generalisation of the results is not allowed. In the future, it is important that both caregivers and patients come to see PCC as normal standard care before starting a pregnancy. This can be reached by informing women of childbearing age during each regular visit with a healthcare professional. Practically, conversations about pregnancy intention will result from adaptations of the training curricula of healthcare professionals implementing interventions for pregnancy planning and preparation. Economic modelling of the impact of PCC might prove useful in resolving lack of urgency by demonstrating the effectiveness and leveraging resources such as time required for PCC realization.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CD:
-
Crohn’s disease
- UC:
-
Ulcerative colitis
- Erasmus MC:
-
Erasmus Medical Center
- GP:
-
General practitioner
- IBD:
-
Inflammatory bowel disease
- PCC:
-
Preconception care
- PPCD:
-
Pregnancy Preparation of women with Chronic Diseases
- RA:
-
Rheumatic arthritis
- RD:
-
Rheumatic diseases
References
Temel S, van Voorst SF, de Jong-Potjer LC, Waelput AJ, Cornel MC, de Weerd SR, et al. The Dutch national summit on preconception care: a summary of definitions, evidence and recommendations. J Community Genet. 2015;6(1):107–15.
Poels M, Koster MP, Franx A, van Stel HF. Healthcare providers’ views on the delivery of preconception care in a local community setting in the Netherlands. BMC Health Serv Res. 2017;17(1):92.
van der Zee B, de Beaufort ID, Steegers EA, Denktas S. Perceptions of preconception counselling among women planning a pregnancy: a qualitative study. Fam Pract. 2013;30(3):341–6.
van Voorst S, Plasschaert S, de Jong-Potjer L, Steegers E, Denktas S. Current practice of preconception care by primary caregivers in the Netherlands. Eur J Contracept Reprod Health Care. 2016;21(3):251–8.
Sellinger CCN, Cassere S, Nelson-Piercy C, Fraser A, Hall V, et al. Standards for the provision of antenatal care for patients with inflammatory bowel disease: guidance endorsed by the British Society of Gastroenterology and the British maternal and fetal medicine society. Frontline Gastroenterology. 2020;0:1–6.
College Perinatale Zorg. Preconceptie Indicatie Lijst 2018. Available from: https://www.nvog.nl/wp-content/uploads/2018/10/Preconceptie-Indicatie-Lijst-PIL.pdf.
Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142(1):46–54 e42 quiz e30.
Kanis SL, van der Woude CJ. Proper use of inflammatory bowel disease drugs during pregnancy. Dig Dis. 2016;34(Suppl 1):61–6.
Ali MF, He H, Friedel D. Inflammatory bowel disease and pregnancy: fertility, complications and treatment. Ann Gastroenterol. 2020;33(6):579–90.
Ellul P, Zammita SC, Katsanos KH, Cesarini M, Allocca M, Danese S, et al. Perception of reproductive health in women with inflammatory bowel disease. J Crohns Colitis. 2016;10(8):886–91.
Walldorf J, Brunne S, Gittinger FS, Michl P. Family planning in inflammatory bowel disease: childlessness and disease-related concerns among female patients. Eur J Gastroenterol Hepatol. 2018;30(3):310–5.
de Lima A, Zelinkova Z, Mulders AG, van der Woude CJ. Preconception care reduces relapse of inflammatory bowel disease during pregnancy. Clin Gastroenterol Hepatol. 2016;14(9):1285–92 e1.
de Man YA, Dolhain RJ, van de Geijn FE, Willemsen SP, Hazes JM. Disease activity of rheumatoid arthritis during pregnancy: results from a nationwide prospective study. Arthritis Rheum. 2008;59(9):1241–8.
Brouwer J, Hazes JM, Laven JS, Dolhain RJ. Fertility in women with rheumatoid arthritis: influence of disease activity and medication. Ann Rheum Dis. 2015;74(10):1836–41.
de Man YA, Hazes JM, van der Heide H, Willemsen SP, de Groot CJ, Steegers EA, et al. Association of higher rheumatoid arthritis disease activity during pregnancy with lower birth weight: results of a national prospective study. Arthritis Rheum. 2009;60(11):3196–206.
Chakravarty E, Clowse ME, Pushparajah DS, Mertens S, Gordon C. Family planning and pregnancy issues for women with systemic inflammatory diseases: patient and physician perspectives. BMJ Open. 2014;4(2):e004081.
Sijpkens MK, Lagendijk J, van Minde MRC, de Kroon MLA, Bertens LCM, Rosman AN, et al. Integrating interconception care in preventive child health care services: the healthy pregnancy 4 all program. Plos One. 2019;14(11):e0224427.
Denktas S, Bonsel GJ, Steegers EA. [Perinatal health in Rotterdam, the Netherlands-experiences after 2 years of ‘Ready for a baby’] Perinatale gezondheid in Rotterdam-ervaringen na 2 jaar ‘Klaar voor een kind’. Ned Tijdschr Geneeskd. 2012;156(29):A4289.
Temel S, Erdem O, Voorham TA, Bonsel GJ, Steegers EA, Denktas S. Knowledge on preconceptional folic acid supplementation and intention to seek for preconception care among men and women in an urban city: a population-based cross-sectional study. BMC Pregnancy Childbirth. 2015;15:340.
Poels M, Koster MP, Boeije HR, Franx A, van Stel HF. Why do women not use preconception care? A systematic review on barriers and facilitators. Obstet Gynecol Surv. 2016;71(10):603–12.
Goossens J, De Roose M, Van Hecke A, Goemaes R, Verhaeghe S, Beeckman D. Barriers and facilitators to the provision of preconception care by healthcare providers: a systematic review. Int J Nurs Stud. 2018;87:113–30.
M'Hamdi HI, van Voorst SF, Pinxten W, Hilhorst MT, Steegers EA. Barriers in the uptake and delivery of preconception care: exploring the views of care providers. Matern Child Health J. 2017;21(1):21–8.
Levis DM, Stone-Wiggins B, O'Hegarty M, Tong VT, Polen KN, Cassell CH, et al. Women's perspectives on smoking and pregnancy and graphic warning labels. Am J Health Behav. 2014;38(5):755–64.
Hull MG, North K, Taylor H, Farrow A, Ford WC. Delayed conception and active and passive smoking. The Avon longitudinal study of pregnancy and childhood study team. Fertil Steril. 2000;74(4):725–33.
Pineles BL, Hsu S, Park E, Samet JM. Systematic review and meta-analyses of perinatal death and maternal exposure to tobacco smoke during pregnancy. Am J Epidemiol. 2016;184(2):87–97.
Radin RG, Hatch EE, Rothman KJ, Mikkelsen EM, Sorensen HT, Riis AH, et al. Active and passive smoking and fecundability in Danish pregnancy planners. Fertil Steril. 2014;102(1):183–91 e2.
Wierstra K, Sutton R, Bal J, Ismond K, Dieleman L, Halloran B, et al. Innovative online educational portal improves disease-specific reproductive knowledge among patients with inflammatory bowel disease. Inflamm Bowel Dis. 2018;24(12):2483–93.
Kashkooli SB, Andrews JM, Roberts MB, Selinger CP, Leong RW. Inflammatory bowel disease-specific pregnancy knowledge of gastroenterologists against general practitioners and obstetricians. United European Gastroenterol J. 2015;3(5):462–70.
Beter Keten. Available from: https://www.beterketen.nl/home/.
Atrash HJB. Preconception care to improve pregnancy outcomes: clinical practice guidelines. J hum Growth Dev. 2020;30(3):353–62.
Atrash HJB. Preconception care: developing and implementing regional and national programs. J Hum Growth Dev. 2020;30(3):363–71.
Atrash HJB. Preconception care to improve pregnancy outcomes: the science. J Hum Growth Dev. 2020;30(3):334–41.
Sijpkens MK, van Voorst SF, de Jong-Potjer LC, Denktas S, Verhoeff AP, Bertens LCM, et al. The effect of a preconception care outreach strategy: the healthy pregnancy 4 all study. BMC Health Serv Res. 2019;19(1):60.
Sijpkens MK, van den Hazel CZ, Delbaere I, Tyden T, Mogilevkina I, Steegers EAP, et al. Results of a Dutch national and subsequent international expert meeting on interconception care. J Matern Fetal Neonatal Med. 2020;33(13):2232–40.
Stephenson J, Vogel C, Hall J, Hutchinson J, Mann S, Duncan H, et al. Preconception health in England: a proposal for annual reporting with core metrics. Lancet. 2019;393(10187):2262–71.
Goodfellow A, Frank J, McAteer J, Rankin J. Improving preconception health and care: a situation analysis. BMC Health Serv Res. 2017;17(1):595.
Laube R, Yau Y, Selinger CP, Seow CH, Thomas A, Wei Chuah S, et al. Knowledge and attitudes towards pregnancy in females with inflammatory bowel disease: an international, Multi-centre Study. J Crohns Colitis. 2020;14(9):1248–55.
Acknowledgements
We are grateful to all participating patients and healthcare professionals who took part in this study. We also want to thank H. Wintjes1 and C.J. van der Woude2 for making it possible to include patients from their outpatient clinics. We especially thank Eliza Rosenmöller for her contribution in completing analyzing the datasets. We would like to thank E. Joziasse – Fitzpatrick3 for her help with linguistic amendments of the manuscript.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors, LA, AR, RD, RW, AM, prepared and performed the study, participated in discussing and interpreting results and approved the final manuscript. LA analyzed the data. LA, AR, and AM wrote the first draft.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The establishment and data collection have obtained a license from the Medical Ethics Committee of the Erasmus MC (MEC-2016 368). Informed written consent was obtained from each participant.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Questionnaire for women with IBD. Questions on a patient level (women with IBD) used to identify the facilitators and barriers of PCC.
Additional file 2.
Questionnaire for women with RD. Questions on a patient level (women with RD) used to identify the facilitators and barriers of PCC.
Additional file 3.
Questionnaire for healthcare professionals involved in the treatment of women with IBD. Questions on a healthcare professional level (treating women with IBD) used to identify the facilitators and barriers of PCC.
Additional file 4.
Questionnaire for healthcare professionals involved in the treatment of women with RD. Questions on a healthcare professional level (treating women with RD) used to identify the facilitators and barriers of PCC.
Additional file 5.
Questionnaire for obstetric healthcare professionals. Questions on a healthcare professional level (obstetric professionals) used to identify the facilitators and barriers of PCC.
Additional file 6.
Questions used to identify knowledge, attitude and actions of women with IBD and RD towards PCC.
Additional file 7.
Baseline characteristics healthcare professionals.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Admiraal, L.A.C., Rosman, A.N., Dolhain, R.J.E.M. et al. Facilitators and barriers of preconception care in women with inflammatory bowel disease and rheumatic diseases: an explorative survey study in a secondary and tertiary hospital. BMC Pregnancy Childbirth 22, 238 (2022). https://doi.org/10.1186/s12884-022-04560-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-04560-y