Abstract
Background
Perinatal depression is of substantial public health importance in low and middle income countries. The study aimed to evaluate the impact of a mental health intervention delivered by non-specialist health workers on symptom severity and disability in women with perinatal depression in Uganda.
Methods
Pregnant women in the second and third trimester were consecutively screened using the Luganda version of the 9-item Patient Health Questionnaire (PHQ-9). Women who scored ≥5 on the PHQ-9 and who were confirmed to have depression by a midwife were recruited into a treatment cohort and offered a psychological intervention in a stepped care fashion. Women were assessed with PHQ-9 and WHODAS-2.0 at baseline and again at 3 and 6 months after the intervention. Negative regression analysis was done to examine change in PHQ-9 and WHODAS-2.0 scores from baseline to end line. Data were analysed using STATA version 14.
Results
A total of 2652 pregnant women (98.3%) consented to participate in the study and 153 (5.8%) were diagnosed as depressed. Over a quarter (28.8%) reported having experienced physical interpersonal violence (IPV) while (25.5%) reported sexual IPV in the past year. A third (34.7%) of women diagnosed with depression received 4 or more group PST sessions. There was a mean reduction in PHQ-9 score of 5.13 (95%CI − 6.79 to − 3.47, p < 0.001) and 7.13 (95%CI − 8.68 to − 5.59, p < 0.001) at midline and endline, respectively. WHODAS scores reduced significantly by − 11.78 points (CI 17.64 to − 5.92, p < 0.001) at midline and − 22.92 points (CI 17.64 to − 5.92, p < 0.001) at endline. Clinical response was noted among 69.1% (95%CI 60.4–76.6%) and 93.7% (95%CI 87.8–96.8%) of respondents at midline and endline, respectively.
Conclusion
An evidence based psychological intervention implemented in primary antenatal care by trained and supervised midwives in a real-world setting may lead to improved outcomes for women with perinatal depression. Future randomised studies are needed to confirm the efficacy of this intervention and possibility for scale up.
Similar content being viewed by others
Background
Globally, depression accounts for the largest proportion of the burden associated with mental and neurological disorders in women of child-bearing age [1, 2]. Perinatal depression is the most common mental health complication in the perinatal period [2, 3], with an estimated prevalence of 11.9% [4]. This burden is projected to grow dramatically in the next decade [5]. The prevalence of perinatal depression in Africa is even higher than global estimates. In a systematic review of studies among African perinatal populations, the pooled prevalence of antenatal depression was 26% and for postnatal depression was 17% [6]. In Uganda, the prevalence of perinatal depression ranges between 5 and 10% in pregnant women, [7,8,9]. In the postpartum period, between 6 and 40% of HIV and non-HIV perinatal populations are at risk for depression [7, 10, 11].
Perinatal depression has adverse effects on the mother, her child and family [12,13,14]. Previous studies have reported an association of perinatal depression with complications in labour and premature birth, low birth weight, low Apgar scores, diarrhoeal episodes, detrimental changes in fetal heart rate and motor activity as well as increased neonatal intensive care unit admission [12, 15, 16], resulting in compromised child development [3, 17]. Untreated perinatal depression is a risk factor for suicidal ideation and suicide completion in the mother [18, 19], as well as one contributing factor to infanticide [20].
Integration of mental health into primary health care is recommended to address health systems challenges in low-resource settings [21,22,23]. However, there is still a pervasive lack of routine perinatal mental health care in LMICs, more so in rural settings [13]. The lack of integration between maternal health services, child health services, and mental health services in primary care creates a large gap in the identification and treatment of perinatal mental disorders [24].
Previous studies provided evidence that problem solving therapy (PST) is effective for depression in general primary health care, as well as in perinatal populations [25, 26]. However, studies on how to integrate and evaluate the impact of such evidence-based interventions in real world primary care environments in LMICs are largely missing. The Programme for Improving Mental Health Care (PRIME) was a multi-country study consortium which aimed to generate evidence on the implementation and scaling up of integrated packages of care for priority mental disorders in primary and maternal health care in five LMICs, including Uganda [27]. Under this program, a district Mental Health Care Plan (MHCP) was developed in each country to provide a framework for implementation and evaluation of the impact of integrating evidence-based interventions in a real-world, primary care setting. A detailed description of the development and components of the Uganda district MHCP has been published elsewhere [28].
In this study we aimed to evaluate the impact of a midwife-delivered intervention on depressive symptom severity and disability among pregnant women 6 months after initiation of treatment for perinatal depression in rural Uganda, as part of the PRIME MHCP.
Methods
The study was conducted in Kamuli district, located in Eastern Uganda. Kamuli’s district has a population of 490,000 rural, poor of little education and engaged is subsistence activity [29]. The district has a high birth rate and population density [30]. More detail on the demographic characteristics of Kamuli has been previously published in the district’s situation analysis [31].
Routine antenatal care in Kamuli is provided at all the primary health care facilities located at different geographical divisions of the district. Kamuli district has 4 sub counties served by 2 (one public and one private) general hospitals (level 5), two level 4 health centers and four level 3 health centers. All these facilities offer both antenatal and postnatal care. The public general hospital is also staffed with a psychiatric clinical officer as well as 2 psychiatric nurses. The district is served by a regional referral hospital in the neighbouring district of Jinja, which is over 60 km away from Kamuli district where complicated cases can be referred to a gynaecologist. A psychiatrist is also available at this referral Hospital. The recruitment of participants in the present study was conducted in five primary care facilities: two level 4 health centres, three level 3 health centres and one general hospital.
We conducted an uncontrolled before-after intervention study with assessments pre-treatment (baseline), 3 months (midline) and 6 months (endline) after baseline or at 2 months postpartum, whichever came first. A single group cohort was selected because we sought to establish the feasibility and acceptability of the intervention, as well as the feasibility of the assessment procedures in this setting, to lay the foundation for a future randomised controlled trial.
Pregnant women were eligible to participate in the study if they were in their second or third trimester of pregnancy, if they resided in the area of study, were aged 18 years or above and spoke the study languages (English or Luganda). Pregnant women were ineligible if in labour, non-residents, and if they had been identified by midwife physical examination as having physical complications related to pregnancy e.g. pre-eclampsia, diabetes or spontaneous abortion.
Sample size was calculated based on a 20% attainment of Clinical response, defined as a 50% reduction of depression symptoms at 6 months, with 90% power, two-sided alpha of 0.05. Sample size calculation was based on a one-sample analysis. An attrition rate of 15–20% at the end of the study was expected. The target sample size was therefore set at 150.
Pregnant women were consecutively screened in the antenatal clinic waiting areas between November 2015 and December 2016. These were recruited from all high-volume public health facilities that offered antenatal and postnatal care. Out of 7 public health facilities in Kamuli district, 5 were considered high volume (with monthly attendance of 500 or more) and were selected. The public facilities (as opposed to private ones) were selected owing to our intention to scale up the intervention in future in public health facilities.
Screening was done by trained non-midwife research assistants using the Luganda version of the 9-item Patient Health Questionnaire (PHQ-9) that had been validated for use in Kamuli in Uganda [32]. Findings from this validation study indicated that the optimum trade-off between sensitivity and positive predictive value (PPV) for probable depression was achieved at a cut-off of ≥5. All women who scored ≥5 on the PHQ-9 in our study were referred to a midwife for confirmation of the depression diagnosis using the World Health Organisation (WHO) Mental Health Gap Action Program Intervention Guide (mhGAP-IG) algorithm [22]. Women who were confirmed to have depression were recruited into a treatment cohort, given information about the aims of the study by the research assistants and invited to provide written consent to participate.
The MHCP was a complex intervention in a real-world setting. The broad components of the MHCP have been previously elaborated [33]. Table 1 below shows the components of the MHCP intervention as it applied to the perinatal setting. This included training of primary care based midwives in assessing, diagnosing and treating perinatal depression in a primary maternal care setting; provision of an adapted evidence based treatment, group based problem solving therapy (PST); providing interpersonal violence support; antidepressant medication for those who had severe symptoms such as suicide as well as supervision and support of the primary care midwives by specialist mental health personnel.
A stepped care approach was used whereby all women who had PHQ-9 score of 5 or more and were confirmed on mhGAP to be depressed were offered the monthly midwife-led Group Problem Solving Therapy (GPST) sessions during their scheduled antenatal visits. Thirty midwives were trained but twenty participated fully in the study. Some dropped out due to routine transfer to other districts and varying assignments in the facilities. Others oversaw health units with administration and support responsibilities to other midwives and were therefore uninterested citing heavy workloads. Training was done by a psychiatrist, a psychiatric clinical officer and a clinical psychologist. Midwives were also trained in assessment and treatment of depression using the WHO mhGAP algorithms. This training took place from August to September 2015. A 3-month period of embedding the intervention was allowed before recruitment started. Two 2-day refresher training courses were conducted for the midwives at 3-month intervals over the recruitment period. Refresher training was done by the same training team. The trained midwives were similar in the sense that they all held a diploma in midwifery and all worked in a similar public health environment.
Bernal’s framework for adapting psychological interventions in LMIC [34, 35] was used to develop a contextually appropriate version of PST. The Bernal’s framework proposes areas for adaptation including 1) language used e.g., translation; 2) using non-specialist mental health workers as therapists; 3) content addressing day to day stressors; 4) methods e.g., incorporating into existing service schedules, 5) storytelling and use of locally familiar examples; and 6) adapted techniques e.g. minimal or no use of written materials and homework among other adaptations. The group PST was adapted by being offered in local language, task shifting it to primary care midwives, providing in in routine antenatal schedules, including care for common stressors such as interpersonal violence (IPV) support and included psycho-education about maternal depression causes and treatment on top of training in problem solving skills.
Women who were found to score ≥ 5 on the PHQ-9 and reported to have suicidal thoughts or suicidal attempts in the past 2 weeks were referred to a visiting specialist psychiatry clinical officer (PCO) attached to the health facility for medication prescription and monitoring, in addition to group PST. Referrals to the PCO were also initiated for participants who presented with persistent depressive symptoms (PHQ-9 score of ≥5) during the midline and endline assessments. The GPST sessions had an average size of 12–15 mothers. A minimum dose of 4 sessions was offered but women could return for more sessions if they needed to. Sessions took place monthly to coincide with their regular antenatal visits, were conducted in a private convenient space within the health facility premises and lasted for 1.5 to 2 h. In these closed PST groups women were guided through the four steps of PST, including 1) identifying and defining the problem, 2) weighing alternative solutions, 3) choosing and implementing the most feasible solution, and 4) evaluating the outcome. In each session, one chosen problem per woman was discussed. Often these problems were common to a number of women in the group and would therefore be handled collaboratively and reported back verbally at the next session. No written homework was expected. IPV support was provided by a team from the Uganda Women’s Network (UWONET), a local non-government organisation providing such support who attended at least one group session to provide information and support to the women.
Monthly supportive supervision was conducted by a visiting mental health specialist (psychiatric clinical officer (PCO) or psychologist) to support midwives in addressing capacity needs and gaps. The supervisors (who were part of the training team) met with the midwives at the clinics to ensure that accurate/correct confirmation of diagnosis was occurring. From time to time, they sat in on the group sessions as observers to identify areas for support to the midwives regarding PST process which formed the content of the refresher trainings. They also provided support in dealing with any challenges the midwives were encountering along the way.
Baseline questionnaires were administered at the participant’s homes within 7 days of recruitment. Midline (3 months from baseline) and endline (6 months from baseline) assessments were also done at home with a window of 2 weeks before or after the appointed date for the interview. All data collection was conducted on an Android mobile device linked to the Mobenzi online application.
Demographic and socio-economic characteristics were assessed using questions adapted from the Uganda Demographic and Health Surveys [32]. Variables assessed included age, sex, education attainment, occupation as well as economic status, employment status and income. History of physical and sexual abuse was assessed using the Abuse Assessment Screen and alcohol use was assessed using the Alcohol Use Disorder Identification Test (AUDIT). Further variables assessed included perceived social support (Oslo Social Support Scale) and accommodation. The full questionnaire can be found in supplementary file 2.
The Primary outcome variables were clinical response and disability score. Clinical response was defined as at least a 50% improvement in the depression symptom score on the PHQ-9. The PHQ-9 has previously been validated in African populations including pregnant women in Ethiopia and Uganda [32, 36]. The nine items of the PHQ-9 are based on the nine diagnostic criteria for major depressive disorder in the DSM-IV [37]. Each item is scored on a Likert scale with symptoms rated as 0 (not at all), 1 (several days), 2 (more than half the days) and 3 (nearly every day) during the past 2 weeks. The sum of the scores indicates whether the respondent has mild (PHQ score 5–9), moderate (PHQ score 10–14) or severe (PHQ score > 15) levels of depressive symptoms.
The World Health Organization (WHO) disability assessment schedule 2.0 (WHODAS 2.0) [38] was used to assess disability. The WHODAS 2.0 is a generic assessment tool for health and disability, which is appropriate for use across cultures in adult populations and was found to be reliable across 19 countries. Each item is measured on a 5-point Likert scale and item scores are summed up to give the degree of functional limitation. Greater WHODAS scores indicate greater functional impairment [39].
To screen for alcohol use disorders (AUD), the 10-item AUDIT was used. The AUDIT was designed to identify hazardous drinkers, harmful drinkers and people with alcohol dependence. The tool was designed by WHO and can be used in both community and clinical settings. Each item concerns the frequency of different drinking behaviours and consequences over the past 12 months. Responses are scored from 0 (never occurs) to 4 (daily). The sum of scores indicate whether the respondent engages in hazardous (score 8–15), harmful (score 16–19) or dependent (score ≥ 20) drinking behaviours, using cut-offs defined by the WHO [40, 41].
In Uganda, the AUDIT has not been validated in perinatal populations but has been shown to have good psychometric properties in post conflict populations in the northern part of the country [42]. The later study elucidated the performance of the AUDIT at different cut off points (≥3, ≥5, ≥8) for problematic drinking and recommended a cut off of 3 or more for screening in population studies. Our study opted to use a cut off of 8 in accordance with the cut-point used other LMICs [41, 42], in order to pick up problematic drinking with more certainty.
The Oslo Social Support Scale (OSSS-3) consists of three items and was used to assess participants’ perceived level of social support. It has been recommended for epidemiological and population-based surveys. The sum score ranges from 3 to 14, with high values representing strong levels and low values representing poor levels of social support. The OSSS-3 sum score can be operationalized into three broad categories of social support [43] namely poor social support (score 3–8), moderate social support (score 9–11) and strong social support (score 12–14). Although the OSSS-3 tool has not been validated in Ugandan, it has been validated among Nigerian students and was found to have good discriminate validity [44].
The Abuse Assessment Screen was developed as a clinical tool to assess frequency, severity and perpetrators of violence against women [45]. It is short and easy to administer. It assesses mainly physical and sexual violence. Although it has not been validated in African populations, it has been found useful and easy to use in other populations around the world [46].
Data were migrated from the Mobenzi online application to STATA version 14 where they were analysed. Data were summarized using frequency tables. The two-sided ᾳ-level was set at 0.05. Reduction of at least 50% in PHQ-9 scores from baseline to endline (clinical response), our primary outcome, is reported. PHQ-9 scores were not normally distributed, so differences in scores across demographic categories were assessed using non-parametric tests, namely the Mann-Whitney U Test or the Kruskal Wallis test. Univariate negative binomial regression analysis was conducted to assess change in PHQ-9 and WHODAS from baseline to midline and from baseline to endline. Change in PHQ-9 scores from baseline to endline across demographic characteristics (education, employment status and food insecurity), perceived social support and IPV [47] was also assessed. This was done using univariate binomial regression models, this time including each demographic variable as an interaction term. For this, education was binarized into uneducated vs. educated, and social support binarized into low/moderate support (OSSS-3 score < 12) vs high support (OSSS-3 score > 11). Change in PHQ-9 scores by number of sessions attended was also assessed using the same analysis.
Results
Respondent characteristics at baseline
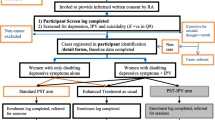
A total of 2698 pregnant women were approached and 2652 (98.3%) consented to participate in the study. Of these, 153 (5.8%) screened positive and were diagnosed as depressed by the midwife and so were included in our study. Of these, 139 (90.8%) were followed-up at 3 months and 138 (90.2%) were followed-up at 6 months. Fig. 1 demonstrates the flow of participants in a consort diagram. The participants lost to follow-up did not present any demographic or clinical differences from those who were assessed at 6 months.
Baseline characteristics of the study sample are shown in Table 2 below. The largest percentage of women (33.3%) were aged between 26 and 30 years. Only 19% were above the age of 30 years and about half (56.2%) were in the 2nd trimester of pregnancy at recruitment. The majority of women (79%) reported being married or being in a stable relationship with a male partner. Only 18% of the respondents had completed secondary school education, and a third (n = 53, 34.6%) reported being illiterate. About two-thirds of women in the study did not have any form of employment, with 17% reported having food insecurity. Over a quarter of participants had experienced physical IPV (n = 44, 28.8%) or sexual IPV (n = 39, 25.5%) in the past year.
The median PHQ-9 score at baseline was 8 (interquartile range (IQR) = 7–10). Participants who were unemployed, who were food insecure and who reported physical IPV all had significantly greater PHQ-9 scores at baseline compared to those who were employed, food secure or did not experience physical IPV. However, there was no significant association between baseline PHQ-9 scores and any of the other demographic characteristics, or with sexual IPV. The median (IQR) scores at baseline for the WHODAS and OSS-3 were 31 [19,20,21,22,23,24,25,26,27,28,29,30,31,32, 34,35,36,37,38,39,40,41,42,43] and 11 [10,11,12,13], respectively. A total of 20 participants (13.1%) reported having poor perceived social support. Nearly all participants reported not drinking alcohol at baseline (n = 136, 93.8%), so AUDIT score was not included in the subsequent analyses.
The total number of sessions attended by the respondents ranged from 0 to 7. A third of participants received 4 or more sessions (n = 51, 34.7%). A minority of participants only received 1 session (n = 12, 8.2%). Twenty-seven (27, 18.4%) participants received no sessions at all. Only 5 (3.3%) of the participants received antidepressants.
Impact of the intervention on individual depression and functioning outcomes
The mean PHQ-9 score at baseline was 9.0 (SD 2.62). There was a significant reduction in mean PHQ-9 score at midline (β = − 5.13, CI − 6.79 to − 3.47, p < 0.001) as well as at endline (− 7.13, CI − 8.68 to − 5.59, p < 0.001) (See Table 3). Clinical response, defined as 50% or more reduction in symptom score PHQ-9 was observed among 69.1% (95%CI 60.38–76.56%) and 93.7% (95%CI 87.84–96.84%) of respondents at midline and endline, respectively. Similarly, the mean WHODAS score changed significantly from 30.5 (13.91) at baseline by − 11.78 points (CI 17.64 to − 5.92, p < 0.001) at midline and − 22.92 points (CI 17.64 to − 5.92, p < 0.001) at endline.
Factors associated with change in PHQ-9 scores at endline
Demographic and intervention characteristics associated with the outcome on PHQ-9 scores from baseline to endline are shown in Table 4. Neither education, employment status nor food insecurity were associated with change in PHQ-9 scores at endline. The change in PHQ-9 scores from baseline to endline also did not differ between participants who reported physical IPV (β = − 1.26, 95%CI − 4.80 to 2.28) or sexual IPV (β = − 6.91, 95%CI − 3.28 to 3.88) compared to those who did not report any IPV at baseline. Also, participants with poor or moderate social support at baseline did not report a different change in PHQ-9 scores compared to those with strong (β = − 0.17, 95%CI − 3.26 to 2.92) social support. Finally, change in PHQ-9 scores from baseline to endline was not different between participants who did not attend any sessions compared to those who attended 1–3 sessions (β = − 0.59, 95%CI − 4.85 to 3.68) or 4–7 sessions (β = 0.80, 95%CI − 5.27 to 3.67).
Discussion
In this study we aimed to evaluate the impact of a midwife delivered intervention on perinatal depression symptom severity and functional disability among pregnant women 6 months after initiation of treatment in Kamuli District in rural Uganda. Our results showed significant improvement in the clinical and functional outcomes of perinatally depressed women after 6 months. Clinical response was noted in 93.7% of individuals attending PST group sessions. Depression care has been previously integrated in PHC settings and found to be effective in reducing morbidity [25, 48, 49]. However, it has not been widely studied in perinatal settings in LMICs. This study is the first of its kind in a real world primary care perinatal setting in Uganda.
Group PST has been shown to be effective in treatment of depression and other common mental disorders in primary care LMIC [50]. For example, Chibanda and others (2014) found that it was feasible and acceptable to provide PST as a low-cost intervention delivered by lay health workers for perinatal women in primary health care [51]. Given the relatively good uptake of the group intervention in our study, the findings imply that GPST may not only be feasible to integrate in primary perinatal services but may also be acceptable to perinatal women in Uganda.
In this study, we provided a pragmatic psychological intervention, adapted group PST, delivered monthly at the time when mothers were scheduled to return to the clinic for antenatal checks. The relevance of the intervention was enhanced by adding in IPV support sessions. The latter could have enabled women to find a safe space to talk about violence in their life and to rest in the knowledge of where and how to get support. There is a lack of evidence regarding the effect of IPV enhanced PST in LMICs, especially in Africa. Although a previous metanalysis of 15 studies in LMICs did not show any relationship between psychological intervention outcomes and presence or absence of IPV in women with common mental disorders including depression [47], other studies in Iran and Pakistan showed possible beneficial effects with IPV enhanced narrative exposure and group cognitive behavioral therapy respectively. Although we did not find a significant association between the women’s experience of IPV and their clinical outcomes we are unable to conclude on whether our adapted PST enhanced with IPV support impacted clinical response. Whether the presence or absence of IPV impacts response to psychological therapy for women with perinatal depression in low resource settings like Uganda needs to be further evaluated.
Social determinants for depression such as level of education, employment status, food insecurity, physical IPV, sexual IPV and status or level of social support have been deemed important to address when providing perinatal depression care in low resource settings [52]. In our study these factors were not significantly associated with change in PHQ-9 scores among our perinatal women. It is possible that the factors associated with the change in PHQ-9 scores in our sample were multiple and complex and not easy to isolate in this study. Additionally, previous researchers have suggested that adaptation of PST to suit local settings may improve both intervention acceptability and outcomes [25, 53]. The adaptation of our PST intervention in this study was possibly an enabler, making our treatment more acceptable and ensuring improved outcomes for depressed perinatal women following Group PST.
The adaptations in our study included providing the PST in groups rather than individually. The group mode of PST delivery may have provided mothers with additional peer support and opportunities to practice interpersonal skills which may explain the improved PHQ-9 and WHODAS scores at endline. Conducting sessions in the local language, well understood by the majority of the population, enabled the women to engage with therapy while scheduling sessions at the time of the scheduled antenatal visits (usually monthly) rather than weekly, may have improved accessibility. One would argue that such a low intensity intervention would not be effective to produce the intended outcomes in symptom severity and function. In fact in a trial of a psychological intervention involving PST and other methods for perinatal women in Khayelitsha, South Africa was found to have no effect on depression outcomes [54]. This prompted the researchers to call for reflection on the strategy of low intensity task shifted psychological interventions in low resource settings. Our pragmatic low intensity intervention, indicates that GPST can be feasibly and acceptably delivered by trained and supervised primary care midwives to depressed perinatal women, but further research using a randomized controlled trial design is needed to test its effectiveness.
Intimate partner violence has previously been documented as a causal factor for depression among pregnant women [55, 56], a key factor for persistence of depression in the perinatal period [55, 56] and a barrier for attendance and active participation in group therapeutic interventions [57,58,59]. Intimate partner violence was a common problem reported among the perinatal women in this study. Enhancing Group PST with IPV support therefore may have provided the needed resources to help women deal with this problem and hence improve treatment outcomes. A previous review of studies on effect of psychological interventions among women with common mental disorders showed that having suffered interpersonal violence did not influence the women’s response to treatment [47]. In this study, we were unable to conclude whether the IPV intervention had an effect on perinatal depression or its response to treatment, given the limited IPV intervention. Nevertheless this may be an important component to include in a future trial, as part of an integrated package of care.
More research is needed to determine whether and how IPV impacts response to psychological interventions in women with perinatal depression. This study, nonetheless, offers optimism about a feasible and acceptable treatment option for depressed perinatal women in LMICs.
There are barriers to integrating mental health into primary care that have been highlighted by previous authors [48] which may apply to perinatal settings as well. Our multi component MHCP attempted to address some of these barriers such as lack or inadequate staffing with mental health specialists, low or no mental health literacy among primary health care workers, lack of access to psychological treatments in primary care and stigma associated with a diagnosis such as depression. Working with midwives and enhancing their ability to facilitate Group PST sessions may have not only increased the accessibility and adherence to the Group PST sessions but also may have reduced self and social stigma often associated with mental health care.
Primary health care workers including midwives and nurses are the first and often the only point of health care contact for the majority of women seeking perinatal services in Uganda. By ensuring training of the midwives, we improved their perinatal depression literacy and therefore enhanced depression identification and chance of treatment. However, this would not have been sufficient to produce outcomes in the perinatal women. Previous studies suggest the importance of supervision and support to non-specialist therapists following training in evidence-based practice for mental health care [52, 60, 61]. A lack of this may lead to deterioration of knowledge and therapeutic skills as well as low therapist confidence and fidelity to a therapy. This may result in less than expected clinical outcomes for patients. Supportive supervision and the practical refresher trainings provided to midwives in Kamuli may have been a key motivation to midwives to continue providing GPST and improved quality of the intervention which led to positive clinical outcomes. Further work is needed to clarify what content, quality, method and dose of supportive supervision is required for trained non specialist health workers and how this influences sustainability of care and patient outcomes.
Limitations in this study included the fact that the population studied, though typical of many rural populations in Uganda, may not be representative of all Ugandan perinatal women. Further still this was not a controlled study, but rather a pragmatic intervention study in a real world primary care setting. It is possible that the positive outcomes could have been due to spontaneous remission, regression to the mean or related to another unmeasured intervention or environmental trends. Further randomized controlled studies are needed to confirm the efficacy and effectiveness of this low intensity integrated task shifted GPST in a low resource primary perinatal care setting in Uganda. Nonetheless, this pilot provides useful information about the feasibility and acceptability of GPST and the study instruments that were used in this context. It also provides a tested platform for a future randomized controlled trial.
Conclusion
These limitations above notwithstanding, this study provides much needed preliminary evidence that a midwife delivered group problem solving therapy is feasible and acceptable and may lead to significant reduction in depression symptom severity and functional disability at 6 months among women with perinatal depression in primary care in low income settings. This has implications for improvement of access to maternal depression care in perinatal care settings in LMICs where there is, usually, a severe lack of mental health specialists. The effect of IPV on perinatal depression severity and response to the GPST could not be conclusively elucidated in this study. Further research is needed to clarify the effect of IPV on perinatal depression and on treatment response. We also recommend that more rigorous randomized controlled studies be carried out to confirm the efficacy and effectiveness of GPST in treatment of perinatal depression in such low resourced primary care settings.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PST:
-
Problem solving therapy
- IPV:
-
Intimate partner violence
- LMICs:
-
Low and middle income countries
- MHCP:
-
Mental health care plan
- PHQ:
-
Patient health questionnaire
- WHODAS:
-
World health organisation disability assessment scale
- AUDIT:
-
Alcohol use disorder identification test
- OSSS:
-
Oslo social support scale
- DSM:
-
Diagnostic and statistical manual
- UWONET:
-
Uganda women’s network
- PRIME:
-
Programme for improved mental health care
References
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2013;380(9859):2163–96.
Howard LM, Molyneaux E, Dennis C-L, Rochat T, Stein A, Milgrom J. Non-psychotic mental disorders in the perinatal period. Lancet. 2014;384(9956):1775–88. https://doi.org/10.1016/S0140-6736(14)61276-9.
Tran TD, Biggs B-A, Tran T, Simpson JA, de Mello MC, Hanieh S, et al. Perinatal common mental disorders among women and the social and emotional development of their infants in rural Vietnam. J Affect Disord. 2014;160:104–12. https://doi.org/10.1016/j.jad.2013.12.034.
Woody CA, Ferrari AJ, Siskind DJ, Whiteford HA, Harris MG. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord. 2017;219:86–92. https://doi.org/10.1016/j.jad.2017.05.003.
Bhat A, Grote NK, Russo J, Lohr MJ, Jung H, Rouse CE, et al. Collaborative care for perinatal depression among socioeconomically disadvantaged women: adverse neonatal birth events and treatment response. Psychiatr Serv. 2017;68(1):17–24. https://doi.org/10.1176/appi.ps.201600002.
Dadi AF, Akalu TY, Baraki AG, Wolde HF. Epidemiology of postnatal depression and its associated factors in Africa: a systematic review and meta-analysis. PLoS One. 2020;15(4):e0231940. https://doi.org/10.1371/journal.pone.0231940.
Kaida A, Matthews LT, Ashaba S, Tsai AC, Kanters S, Robak M, et al. Depression during pregnancy and the postpartum among HIV-infected women on antiretroviral therapy in Uganda. J Acquir Immune Defic Syndr. 2014;67(Suppl 4):S179.
Natamba BK, Achan J, Arbach A, TO O, Ghosh S, Mehta S, et al. Reliability and validity of the center for epidemiologic studies-depression scale in screening for depression among HIV-infected and -uninfected pregnant women attending antenatal services in northern Uganda: a cross-sectional study. BMC Psychiatry. 2014;14(1):303. https://doi.org/10.1186/s12888-014-0303-y.
Ndege J. Prevalence and factors associated with depression in pregnancy at mulago hospital, uganda a dissertation submitted to the directorate of research and graduate training in partial fulfillment of the requirement [Internet]. 2018 [cited 2020 Oct 10]. Available from: http://www.dspace.mak.ac.ug/bitstream/handl.
Nakku JN, Nakasi G, Mirembe F. Postpartum major depression at six weeks in primary health care: prevalence and associated factors. African health sciences. 2006;6(4).
Kakyo TA, Muliira JK, Mbalinda SN, Kizza IB, Muliira RS. Factors associated with depressive symptoms among postpartum mothers in a rural district in Uganda. Midwifery. 2012;28(3):374–9.
Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384(9956):1800–19. https://doi.org/10.1016/S0140-6736(14)61277-0.
Baron EC, Hanlon C, Mall S, Honikman S, Breuer E, Kathree T, et al. Maternal mental health in primary care in five low-and middle-income countries: a situational analysis. BMC Health Serv Res. 2016;16(1):53. https://doi.org/10.1186/s12913-016-1291-z.
Gelaye B, Rondon MB, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry. 2016;3(10):973–82. https://doi.org/10.1016/S2215-0366(16)30284-X.
Ross J, Hanlon C, Medhin G, Alem A, Tesfaye F, Worku B, et al. Perinatal mental distress and infant morbidity in Ethiopia: a cohort study. Arch Dis Child Fetal Neonatal Ed. 2011;96(1):F59–64. https://doi.org/10.1136/adc.2010.183327.
Jarde A, Morais M, Kingston D, Giallo R, MacQueen GM, Giglia L, et al. Neonatal outcomes in women with untreated antenatal depression compared with women without depression: a systematic review and meta-analysis. JAMA Psychiatry. 2016;73(8):826–37. https://doi.org/10.1001/jamapsychiatry.2016.0934.
World Health Organization. Maternal mental health and child health and development in low and middle income countries: report of the meeting, Geneva, Switzerland, 30 January-1 February, 2008.
Gentile S. Suicidal mothers. J Inj Violence Res. 2011;3(2):90–7. https://doi.org/10.5249/jivr.v3i2.98.
Alhusen JL, Frohman N, Purcell G. Intimate partner violence and suicidal ideation in pregnant women. Arch Womens Ment Health. 2015;18(4):573–8. https://doi.org/10.1007/s00737-015-0515-2.
Tang D, Siu B. Maternal infanticide and filicide in a psychiatric custodial institution in Hong Kong. East Asian Arch Psychiatr. 2018;28(4):139–43.
Hanlon C, Wondimagegn D, Alem A. Lessons learned in developing community mental health care in Africa. World Psychiatry. 2010;9(3):185–9. https://doi.org/10.1002/j.2051-5545.2010.tb00308.x.
World Health Organization. mhGAP: Mental Health Gap Action Programme: scaling up care for mental, neurological and substance use disorders. Geneva: World Health Organization; 2008.
Saraceno B, van Ommeren M, Batniji R, Cohen A, Gureje O, Mahoney J, et al. Barriers to improvement of mental health services in low-income and middle-income countries. Lancet. 2007;370(9593):1164–74. https://doi.org/10.1016/S0140-6736(07)61263-X.
Chopra M, Daviaud E, Pattinson R, Fonn S, Lawn JE. Saving the lives of South Africa’s mothers, babies, and children: can the health system deliver? Lancet. 2009;374(9692):835–46. https://doi.org/10.1016/S0140-6736(09)61123-5.
Chibanda D, Mesu P, Kajawu L, Cowan F, Araya R, Abas MA. Problem-solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV. BMC Public Health. 2011;11(1):828. https://doi.org/10.1186/1471-2458-11-828.
Danasabe M, Elias N. Islamic problem solving therapy for postpartum depression among Muslim postpartum women in Nigeria. Asian J Multidiscip Stud. 2017;5(2):69–79.
Lund C, Tomlinson M, De Silva M, Fekadu A, Shidhaye R, Jordans M, et al. PRIME: a programme to reduce the treatment gap for mental disorders in five low-and middle-income countries. PLoS Med. 2012;9(12):e1001359. https://doi.org/10.1371/journal.pmed.1001359.
Kigozi FN, Kizza D, Nakku J, Ssebunnya J, Ndyanabangi S, Nakiganda B, et al. Development of a district mental healthcare plan in Uganda. Br J Psychiatry. 2016;208(s56):s40–6. https://doi.org/10.1192/bjp.bp.114.153742.
Uganda Demographic and Health Survey 2016. Kampala, Uganda and Rockville, Maryland, USA: UBOS and ICF. 2018.
Uganda Bureau of Statistics National Population and Housing Census Final Report 2014. Uganda Bureau of Statistics; 2016.
Hanlon C, Luitel NP, Kathree T, Murhar V, Shrivasta S, Medhin G, Ssebunnya J, Fekadu A, Shidhaye R, Petersen I, Jordans M. Challenges and opportunities for implementing integrated mental health care: a district level situation analysis from five lowand middle-income countries. PloS one. 2014;9(2):e88437.
Nakku JEM, Rathod SD, Kizza D, Breuer E, Mutyaba K, Baron EC, et al. Validity and diagnostic accuracy of the Luganda version of the 9-item and 2-item patient health questionnaire for detecting major depressive disorder in rural Uganda. Glob Ment Heal. 2016;3:6–9.
Nakku JE, Rathod SD, Garman EC, Ssebunnya J, Kangere S, De Silva M, et al. Evaluation of the impacts of a district-level mental health care plan on contact coverage, detection and individual outcomes in rural Uganda: a mixed methods approach. Int J Ment Heal Syst. 2019;13(1):1–3.
Bernal G, Sáez-Santiago E. Culturally centered psychosocial interventions. J Community Psychol. 2006;34(2):121–32.
Chowdhary N, Sikander S, Atif N, Singh N, Ahmad I, Fuhr DC, et al. The content and delivery of psychological interventions for perinatal depression by non-specialist health workers in low and middle income countries: a systematic review. Best Pract Res Clin Obstet Gynaecol. 2014;28(1):113–33. https://doi.org/10.1016/j.bpobgyn.2013.08.013.
Woldetensay YK, Belachew T, Tesfaye M, Spielman K, Biesalski HK, Kantelhardt EJ, et al. Validation of the patient health questionnaire (PHQ-9) as a screening tool for depression in pregnant women: Afaan Oromo version. PLoS One. 2018;13(2):e0191782. https://doi.org/10.1371/journal.pone.0191782.
First MB, Gibbon M, Spitzer RL, Benjamin LS. User’s guide for the structured clinical interview for DSM-IV axis II personality disorders: SCID-II: American Psychiatric Pub; 1997. American Psychiatric Publishing, Inc.
Üstün TB. Measuring health and disability: manual for WHO disability assessment schedule WHODAS 2.0: World health Organization; 2010.
Andrews G, Kemp A, Sunderland M, Von Korff M, Ustun TB. Normative data for the 12 item WHO Disability Assessment Schedule 2.0. PloS one. 2009;4(12):e8343.
Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: the alcohol use disorders identification test guidelines for use in primary care. Geneva Switz: World Health Organization; 2001.
Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The alcohol use disorders identification test. In: Guidel Use Prim Care. 2nd ed. New York: World Heal Organ; 2002.
Blair AH, Pearce ME, Katamba A, Malamba SS, Muyinda H, Schechter MT, Spittal PM. The alcohol use disorders identification test (AUDIT): exploring the factor structure and cutoff thresholds in a representative post-conflict population in northern Uganda. Alcohol Alcohol. 2017;52(3):318–27.
Bøen H, Dalgard OS, Bjertness E. The importance of social support in the associations between psychological distress and somatic health problems and socio-economic factors among older adults living at home: a cross sectional study. BMC geriatrics. 2012;12(1):1–2.
Abiola T, Udofia O, Zakari M. Psychometric properties of the 3-item oslo social support scale among clinical students of Bayero University Kano, Nigeria. Malaysian J Psychiatry. 2013;22(2):32–41.
Soeken KL, McFarlane J, Parker B, Lominack MC. The abuse assessment screen: a clinical instrument to measure frequency, severity, and perpetrator of abuse against women. Sage ser violence against women 1998.
Antoniou E, Ioannidi-Kapolou E, Daglas M, Vivilaki V, Karamitros D, Dafermos V, Iatrakis G. Abuse assessment screen (AAS) questionnaire: the Greek validation. Clin Exp Obstetrics Obstet. 2010;37(4):313.
Keynejad RC, Hanlon C, Howard LM. Psychological interventions for common mental disorders in women experiencing intimate partner violence in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Psychiatry. 2020;7(2):173–90. https://doi.org/10.1016/S2215-0366(19)30510-3.
Abas M, Baingana F, Broadhead J, Iacoponi E, Vanderpyl J. Common mental disorders and primary health care: current practice in low-income countries. Harvard Rev Psychiatry. 2003;11(3):166–73. https://doi.org/10.1080/10673220303954.
Patel V, Garrison P, de Jesus MJ, Minas H, Prince M, Saxena S. The Lancet's series on global mental health: 1 year on. Lancet. 2008;372(9646):1354–7. https://doi.org/10.1016/S0140-6736(08)61556-1.
Cuijpers P, van Straten A, Warmerdam L. Problem solving therapies for depression: a meta-analysis. Eur Psychiatry. 2007 Jan 1;22(1):9–15. https://doi.org/10.1016/j.eurpsy.2006.11.001.
Chibanda D, Shetty AK, Tshimanga M, Woelk G, Stranix-Chibanda L, Rusakaniko S. Group problem-solving therapy for postnatal depression among HIV-positive and HIV-negative mothers in Zimbabwe. J Int Assoc Provid AIDS Care. 2014;13(4):335–41. https://doi.org/10.1177/2325957413495564.
Honikman S, Sigwebela S, Schneider M, Field S. Perinatal depression and anxiety in resource-constrained settings: interventions and health systems strengthening. South African Health Rev. 2020;2020(1):30–40.
Sampson M, Villarreal Y, Rubin A. A problem-solving therapy intervention for low-income, pregnant women at risk for postpartum depression. Research on social work practice. 2016;26(3):236–42.
Lund C, Schneider M, Garman EC, Davies T, Munodawafa M, Honikman S, Bhana A, Bass J, Bolton P, Dewey M, Joska J. Task-sharing of psychological treatment for antenatal depression in Khayelitsha, South,Africa: Effects on antenatal and postnatal outcomes in an individual randomised controlled trial. Behav Res Ther. 2020;130:103466.
Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26(4):289–95. https://doi.org/10.1016/j.genhosppsych.2004.02.006.
Bitew T, Hanlon C, Kebede E, Honikman S, Onah MN, Fekadu A. Antenatal depressive symptoms and utilisation of delivery and postnatal care: a prospective study in rural Ethiopia. BMC Pregnancy Childbirth. 2017;17(1):206. https://doi.org/10.1186/s12884-017-1383-8.
Chisholm D, Knapp MRJ, Knudsen HC, Amaddeo F, Gaite L, Van Wijngaarden BOB, et al. Client socio-demographic and service receipt inventory–European version: development of an instrument for international research: EPSILON study 5. Br J Psychiatry. 2000;177(S39):s28–33. https://doi.org/10.1192/bjp.177.39.s28.
Ugarriza DN. Group therapy and its barriers for women suffering from postpartum depression. Arch Psychiatr Nurs. 2004;18(2):39–48. https://doi.org/10.1053/j.apnu.2004.01.002.
Nakimuli-Mpungu E, Wamala K, Okello J, Alderman S, Odokonyero R, Mojtabai R, et al. Group support psychotherapy for depression treatment in people with HIV/AIDS in northern Uganda: a single-Centre randomised controlled trial. Lancet HIV. 2015;2(5):e190–9. https://doi.org/10.1016/S2352-3018(15)00041-7.
Murray LK, Dorsey S, Bolton P, Jordans MJD, Rahman A, Bass J, et al. Building capacity in mental health interventions in low resource countries: an apprenticeship model for training local providers. Int J Ment Health Syst. 2011;5(1):30. https://doi.org/10.1186/1752-4458-5-30.
Beidas RS, Kendall PC. Training therapists in evidence-based practice: a critical review of studies from a systems-contextual perspective. Clin Psychol Sci Pract. 2010.
Acknowledgments
We are grateful to all our study participants who gave their time to respond to our questionnaires as well as to the midwives who accepted to engage with this work, despite their busy schedules. We thank the Kamuli district administration for enabling us to do this work in the health facilities.
Funding
This study is an output of the PRogramme for Improving Mental health carE (PRIME) which was funded by UK aid from the UK Government (GB-1-201446); however, the views expressed do not necessarily reflect the UK Government’s official policies. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
JN conceptualized the manuscript, designed the study methodology and, supported the review and editing process; ON was part of the investigation team, collaborated in the design of the methodology, drafted the original manuscript, supported review and editing; EG provided technical support in design of study methodology, oversaw the data curation, conducted formal analysis and supported the review and editing; SH provided technical support in design of methodology and manuscript, and supported review and editing; CH supported Conceptualization of the manuscript, provided technical assistance in methodology design and interpretation of study findings, and editing of manuscript, FK supported Conceptualization, interpretation of study results and supported review and editing; CL provided technical support in conceptualization, Methodology design, Review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval of the protocol for the study was obtained from Makerere University school of medicine research and ethics committee (REC REF 2014–147), the Uganda National Council of Science and Technology (Kampala, Uganda), the University of Cape Town (South Africa), and the World Health Organization (Geneva, Switzerland). Institutional approval was also obtained from the district administration.
All participants provided written, informed consent by signing a study consent form. For those who were illiterate, the contents of the consent form were read to them in local language by a research assistant before they appended a thumb print. All patients who were found to be at risk of suicide were referred to the mental health specialist at the district hospital. All adverse events during the cohort study were documented in a register of adverse events.
Consent for publication
Not Applicable.
Competing interests
The authors have declared that there are no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Prime Cohort Questionnaire. The file comprises of the study tool used during the PRIME cohort surveys at baseline, Midline (at 3 months) and Endline (at 6 months).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nakku, J.E.M., Nalwadda, O., Garman, E. et al. Group problem solving therapy for perinatal depression in primary health care settings in rural Uganda: an intervention cohort study. BMC Pregnancy Childbirth 21, 584 (2021). https://doi.org/10.1186/s12884-021-04043-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-021-04043-6