Abstract
Background
There is an international trend to shorten the postpartum length of stay in hospitals, driven by cost containment, hospital bed availability and a movement toward the ‘demedicalization’ of birth. The aim of this systematic literature review is to determine how early postnatal discharge policies from hospitals could affect health outcomes after vaginal delivery for healthy mothers and term newborns.
Methods
A search for systematic reviews, meta-analyses, and primary studies was carried out in OVID MEDLINE, Embase, CINAHL, Econlit and the Cochrane Library (Cochrane Database of Systematic Reviews, DARE and HTA databases). The AMSTAR checklist was used for the quality appraisal of systematic reviews. The quality of the retrieved studies was assessed by the Cochrane Collaboration’s tools. The level of evidence was appraised using the GRADE system.
Results
Seven RCTs and two additional observational studies were found but no comprehensive economic evaluation. Despite variation in the definition of early discharge, the authors of the included studies, concerning early discharge and conventional length of stay, reported no statistical difference in maternal and neonatal morbidity, maternal and neonatal readmission rates, infant mortality, newborn weight gain, neonatal hyperbilirubinemia, or breastfeeding rates. The authors reported conflicting results regarding postpartum depression and competence of mothering, ranging from no difference according to length of stay to better results for early discharge. The level of evidence of the vast majority of outcomes was rated as low to very low.
Conclusions
Because of the lack of robust clinical evidence and full economic evaluations, the current data neither support nor discourage the widespread use of early postpartum discharge. Before implementing an early discharge policy, Western countries with longer length of hospital stay may benefit from testing shorter length of stay in studies with an appropriate design. The issue of cost containment in implementing early discharge and the potential impact on the current and future health of the population exemplifies the need for publicly funded clinical trials in such public health area. Finally, trials testing the range of out-patient interventions supporting early discharge are needed in Western countries which implemented early discharge policies in the past.
Background
In Western countries, there is a trend to shorten the postpartum length of stay in hospital driven by cost containment, hospital bed availability and a movement toward ‘demedicalisation’ of childbirth [1]. Although this trend was initiated as early as the 1940s in the United States [2] other countries followed later. Thus, while the average postpartum length of stay in Swedish hospitals was 6 days in the 1970s [3] it declined to 2.3 days in 2010 [4], reflecting a similar duration to that observed, the same year, in the Netherlands (2.1 days), New-Zealand, Ireland and the United States (2.0 days) [4]. In addition to shorter hospital stays, early postpartum discharge for healthy mothers and newborns was introduced to promote a more family-centred approach to birth allowing greater involvement of fathers, less sibling rivalry, improved rest and sleep for the mother, less exposure of the dyad mother-newborn to nosocomial infections, enhancement of maternal confidence in caring for the baby, and finally, less conflicting advice on breastfeeding [5]. However, concerns about early discharge arose regarding potential adverse outcomes such as delays in detecting and preventing maternal morbidities and neonatal pathologies [6], earlier weaning, lack of professional support, higher prevalence of postpartum depression and increased hospital readmissions for both mothers and infants [5]. Societal concerns about maternal and newborn welfare in the context of early discharge led the United States to vote the Newborns’ and Mothers’ Health Protection Act in 1996 making it mandatory for health insurers to cover postpartum hospitalisation for a minimum of 48 h after vaginal delivery and 96 h after a caesarean section [2]. Therefore, early discharge after vaginal birth is considered as less than 48 h in the United States. However, to date there is no standard definition of early postpartum discharge because of large variations in the usual average length of stay for vaginal delivery between countries (i.e. in 2011, the mean length of stay for single spontaneous delivery was 5.2 days in Hungary, 4.2 in France, 4.0 in Belgium, 2.8 in Australia, 1.7 in Canada and 1.5 in the United Kingdom) [4]. Consequently, early postpartum discharge varies from 12 to 72 h depending on the country [7].
As in some other Western countries, Belgium experiences an average hospital stay for vaginal deliveries of 4 days. Decision makers willing to introduce earlier hospital discharge need evidence based information about the effect of such policies on neonatal and maternal health outcomes. Therefore, this literature systematic review aims to determine how, early discharge policies with or without home care (support) affect health outcomes after a vaginal birth for healthy mothers and term newborns (≥ 37 weeks) in Western countries.
Method
Eligibility and search strategy
Studies included in this systematic review compare ‘early discharge of healthy mothers and newborns after a vaginal birth with or without home care’ with standard length of hospital stay as defined in the time and place where the studies were conducted.
Caesarean sections necessitate longer hospital stays and more complicated postnatal care. Therefore, we selected all studies that included vaginal birth of live singleton term infants with or without instrumental assistance. All studies must include hospital deliveries overseen by a health care professional in Western countries. Studies describing deliveries by caesarean sections, the presence of postpartum haemorrhage, substance abuse during the pregnancy, disability, domestic violence, low birth weight, preterm baby, or home birth were excluded.
Women’s views about length of stay or satisfaction with care are not included in this review because these outcomes are highly context-specific. As international comparisons are influenced by a wide range of confounders such as time, subjective wellbeing, type of care organisation… [8] and because of the lack of information regarding these confounders in the publications, the adjustment is challenging and will not be reviewed here.
This review was conducted according to the PRISMA statement [9]. The search for systematic reviews, meta-analyses, and primary studies was carried out by an information specialist (NF) and validated by other co-authors in OVID MEDLINE, Embase, CINAHL, Econlit and the Cochrane Library (Cochrane Database of Systematic Reviews, DARE and HTA database). MESH terms and related keywords were used in an extensively searched (detailed search strategies by databases are available in Additional file 1). Two independent researchers (NB, LS) performed the selection, the quality appraisal, and the data extraction of the studies. During the selection process, a Cochrane review of early postnatal discharge from hospital for healthy mothers and term infants was found [5]. This high quality review (see AMSTAR evaluation in Additional file 1) included only randomised controlled trials (RCTs) in a broader population than our population of interest. Therefore, relevant evidence was extracted from this review [5] to focus on our specific research question. In addition, the update presented here considered all comparative studies whatever the design, published until August 2015. Non-randomised studies were included only if they described an outcome that was not previously described in a RCT. Because health care organisations are perpetually evolving, we limited our search to new outcomes supported by non-randomised comparative studies during the update period.
The health outcomes under consideration were mortality, morbidity, hospital readmission rates for both mother and child. Additional neonatal outcomes (jaundice and weight gain) and maternal outcomes (counselling and psychological function). Breastfeeding rates were also studied.
Assessment of methodological quality of evidence
The AMSTAR checklist was used for the quality appraisal of the systematic reviews [10]. The quality appraisal of RCTs and non-randomised studies was performed using the "Cochrane Collaboration’s tool for assessing risk of bias" [11].
Statistical analyses
Categorical data were presented using risk ratios (RR) with 95% confidence intervals (95% CI). The mean difference with 95% CI was used to report continuous data. Statistical analyses for pooling intervention effects were performed using Review Manager 5.3®.
Level of evidence
Level of evidence was categorized in 4 levels (high, moderate, low and very low) according to the GRADE system [12].
Results
Results of the search
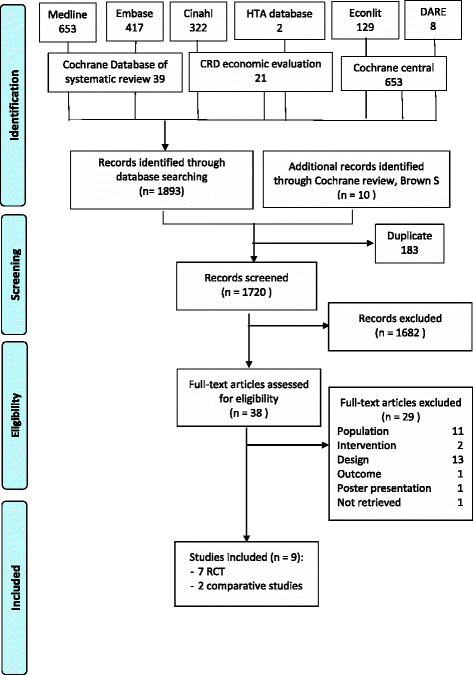
From the Cochrane review, ten RCTs were extracted for full text examination. From those, three trials were excluded because deliveries by caesarean section were included and results were not reported separately for vaginal deliveries [13,14,15].
During the update process, no systematic reviews, meta-analyses, or RCTs were found. After a first sifting based on title and abstract, 16 non-randomised studies were retrieved for further analysis on full text [1, 2, 6, 16,17,18,19,20,21,22,23,24,25,26,27,28]. Finally, 2 non-randomised studies were included in our review [16, 27].
The present systematic review includes 5 RCTs and two non-randomised studies (see Fig. 1 – Flow chart). Characteristics of the included studies are reported in Table 1. A list of excluded studies is provided in Additional file 1.
Definition of early hospital discharge
No standard definition of ‘early discharge’ from hospital was found across trials. A variation in the discharge time from less than 24 h to 72 h was seen. Similarly, the ‘usual length of stay’ ranged from 48 h to 5 days. In the five included trials, all early discharge programs proposed post-discharge home visits by nurses or midwives. However, prenatal preparation for early discharge was not always foreseen. In the two included non-randomised studies, early discharge was defined as a length of stay of maximum 24 h. While one study only proposed a medical visit 7 days after delivery to assess newborn health status, the other study organised two or three home visits, during the first week, performed by two nurse-midwives with experience in neonatal care.
Early discharge and maternal health outcomes
Morbidity
Four trials reported data on maternal morbidity [29,30,31,32]. Among these, three studies did not find any difference in complication rates between early discharge and conventional length of stay [29, 31, 32]. The most frequently reported pathologies were urinary tract infection, episiotomy infection, mastitis and other mammary pathologies and endometritis. In contrast, Hellman et al. found a small significant difference in favour of conventional length of stay in comparison with early discharge in febrility, lochia, involution of the uterus, and breast engorgement at 3 weeks of puerperium [30]. No pooling estimation of the rate of complications was done because of the poor quality of data reporting and the large differences in the time frame of morbidity rate measurement.
Complication rate
A non-randomised study, performed in a general hospital in Mexico, found no significant difference, during the first week postpartum, between reported complication rate by the mothers discharged at 24 h or less and those discharged later (OR (95% CI) = 0.95 (0.41–2.20). In this study, the prenatal care was assessed according to the Official Mexican Norm (NOM-007-SSA2–1993) [33]. The authors found that women with an early discharge and satisfactory prenatal care had a 64% lower odds for presenting symptoms within the first week postpartum compared with women with being discharged later and from whom prenatal control was unsatisfactory (OR 0.36; 95% CI: 0.17–0.76) [27].
Counseling
Hellman et al. showed that mothers discharged early were statistically significantly more likely to require more advice during the follow-up period for themselves or for their newborn in comparison with conventional length of stay mothers [30] (see Table 1). Information requested about newborns related to feeding, bowels, hygiene and care of the umbilical cord whereas breast care, perineal care, personal hygiene and exercise were the most reported topics for advice for mothers.
Readmission
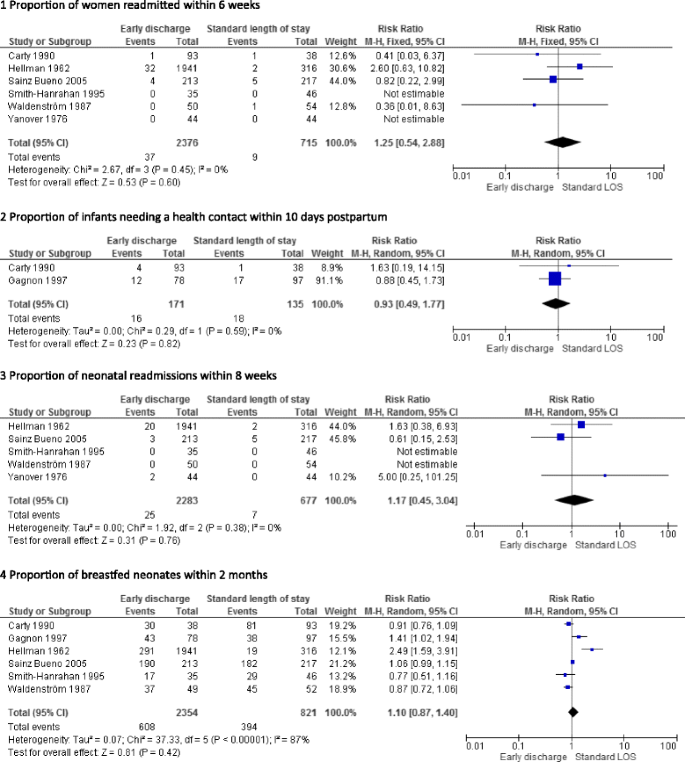
No significant differences in maternal readmission rates during the postpartum period were found in four trials [29,30,31,32, 34, 35]. Figure 2 presents a pooled risk ratio (95% confidence interval) (RR (95%CI) of 1.25 (0.54–2.88) for maternal readmissions occurring from week 1 to 6 after birth.
Psychological functioning
-
Depression
Carty and Bradley found a significant difference in mean scores on the Beck Depression Index (p < 0.05) between mothers with length of stay ≤24 h and those with a four-day stay (see Table 1). Mothers with a shorter postpartum stay had better emotional well-being at 1 month than those with a standard duration hospital stay. However, no difference was found between a length of stay of 25 to 48 h and one of 4 days [29].
Sainz-Bueno et al. showed no difference in anxiety and depression between early discharged mothers and those with conventional duration stays measured by the hospital anxiety and depression (HAD) scale [31]. Nevertheless, it should be noted that 2.8% of the mothers had scores on HAD scale at 1 week postpartum indicating a requirement of psychiatric monitoring. Among those, 0.5% required psychiatric admission. At 1 month post-delivery, this proportion reached 2.3%. Nevertheless, no difference was found between early discharge and conventional stay mothers.
Waldenström et al. found no difference in the proportions of women reporting a depressed mood during the first 6 weeks after birth between early discharge (26%) and conventional stay (34%) [35]. Reported depressed mood peaked during the 2nd and 3rd week after the birth.
Because of existing differences in the scales used for measuring depression, no pooling of data was performed.
-
Competence of mothering
Gagnon et al. measured competence in mothering using the Perceived Maternal Task Performance Scale at 1 month [36]. Competence in mothering included mothers’ ability to assess their infant’s needs and their own abilities to feed their newborn and to perform caregiving activities. The authors found no significant difference between mean scores between mothers discharged between 6 h and 36 h post-delivery and those discharged between 42 to 72 h.
Another randomised trial assessed women’s confidence in their mothering skills using an eight-item scale [29]. The authors reported a significantly higher score at 1 week in mothers discharged within 24 h than those discharged 4 days post-delivery (see Table 1). After a month, this difference did not remain. In addition, no differences were noted between very early discharged mothers (between 12 and 24 h) and early discharged mothers (between 25 and 48 h).
-
Sense of security
Askelsdottir et al. reported a greater sense of security in the first postnatal week for early discharged women [16]. However, those women had more negative emotions towards breastfeeding compared with women with conventional length of stay. Because there is no difference in parity between the 2 groups, an explanation can be found in a higher educational level of mothers included in the group with conventional length of stay. Contact between the mother, newborn and partner did not differ between the two lengths of stay.
Early discharge and neonate health outcomes
Mortality
Only one trial assessed the mortality rate in newborns at 3 weeks of life [30]. The authors found mortality rates of 0.24% and 0.46% in newborns with early discharged conventional babies and length of stay respectively. These proportions were not statistically different.
Morbidity
Two trials reported the proportion of newborns needing a health contact within 10 days postpartum [29, 36]. Pooling of results does not show any difference between early discharged newborns and those who stayed longer in hospital after birth (see Fig. 2).
Yanover et al. concluded that no significant differences in type or in occurrence of neonatal morbidities were observed during the follow-up period [32]. Unfortunately, no data were reported. After 3 weeks, Hellman et al. did not find any significant difference in complication rates between early discharged newborns and those with conventional duration stays [30] (see Table 1).
Weight gain
Two trials analysed the difference in weight gain of newborns with early discharge and conventional length of stay [30, 36]. The first study did not find any significant differences in daily rates of infant weight gain during the first 10 days of life [36] (see Table 1). The second trial focused on weight gains at 3 weeks of life [30]. No significant difference was found between early discharged newborns and infants with a standard length of stay.
Neonatal hyperbilirubinemia
One trial studied the occurrence of hyperbilirubinemia [36] and reported that there was no difference in identification of significant neonatal hyperbilirubinemia (see Table 1). However, a significantly reduced crude relative risk for bilirubin testing (RR [CI 95%]: 0.39 [0.17–0.94]) was observed in early discharged neonates. Notwithstanding, the proportion of tested newborns eligible for phototherapy were not significantly different (RR [CI 95%]: 1.26 [0.33–4.93]).
Readmission
No significant differences in neonatal readmission rates were found in the three trials reporting data on this outcome [30,31,32, 34, 35]. The pooled RR for neonatal readmissions occurring within 3 to 8 weeks of birth is presented in Fig. 2 and does not show any increased risk of readmission in early discharged neonates.
Breastfeeding
Six trials reported data on partial or exclusive breastfeeding from 3 weeks to 9 months. Pooled estimates are presented in Fig. 2 and show that early discharge mothers were equally likely to breastfeed their neonates than those with a conventional length of stay. Waldenström et al. found no difference in breastfeeding rate at 6 months according to the length of stay [35]. Sainz-Bueno et al. studied breastfeeding rates up to 9 months and did not find any differences between the groups at any time except at 3 months with a significantly higher rate in early discharged mothers (see Table 1).
A non-randomised study reported that early discharge mothers (between 12 to 24 h postpartum) described less positive emotions towards breastfeeding compared with other mothers (conventional length of stay from 24 to 48 h postpartum) [16]. Emotions towards breastfeeding were measured using the 2 domains of the Alliance scale (Alliance scale mean score (SD) Breastfeeding strain: early discharge: 2.4 (1.31), conventional length of stay: 1.7 (0.93); p = 0.001/Breastfeeding uncomfortable early discharge: 2.9 (1.61), conventional length of stay: 2.2 (1.07); p = 0.028).
Quality assessment of included studies and level of evidence
The only systematic review included [5] was rated at a level of 9/11 with the AMSTAR check list (see Additional file 1). Despite its high quality, the review was only used as a source of evidence because the research questions were slightly different with our review allowing the inclusion of caesarean sections within its scope. The quality appraisal of all RCTs matching our inclusion criteria is shown in Additional file 1. The lack of blinding of participants and personnel was not feasible and was not considered a risk of bias in the context of postpartum care because it does not affect the outcomes assessed. Methods used to ensure allocation concealment were reported in three trials [29, 31, 36] while the remaining two did not provided information on this methodological item. None of the included studies indicated if outcomes assessment was blinded. In addition to the specific bias linked to their non-randomised design, the two comparative studies presented other bias such as single centre design, selection biases or small sample size. Details on quality assessment of these studies are reported in Additional file 1.
The level of evidence is documented in Additional file 1. Despite RCT design, the vast majority of outcomes are rated as low or very low level of evidence. Outcomes regarding counselling, neonatal mortality rate and rate of health contact for newborns within 10 day of life are rated as moderate.
Discussion
Based on the available evidence, early postpartum discharge seems to be clinically safe for both mothers and newborns. These results are in line with a previously published review [5] which was restricted to RCTs but included caesarean sections. Early hospital discharge in caesarean section deliveries did not seem to affect outcome such as breastfeeding rate, maternal and infant readmission. However, confounders such as type of health system (public versus private), opportunities for antenatal preparation and for postnatal domiciliary midwife support or type of postpartum intervention cannot be studied because of poor reporting. Therefore, mixing data from vaginal delivery and caesarean section must considered with caution. Despite of this precaution, evidence must be interpreted with caution for two main reasons.
Firstly, the concept of early hospital discharge and that of conventional length of stay varied greatly between trials, making an interpretation or comparison across studies difficult. Among the selected studies, a discharge was considered early when the mother-infant dyad was discharged from 6 h to 72 h after birth. Currently, there are considerable variations in length of stay between Western countries. In Sweden, early discharge corresponds to a length of stay of 6 h after birth [3, 37], while in France, a discharge after a length of stay of less than 72 h is considered as early [19]. In the US, a minimum period of 48 h is ensured by law after a resurgence of jaundice cases and an increase in re-admissions among both mothers and children [1, 2]. However, Evan et al. [1] demonstrated that the extension of the postpartum length of stay to 48 h had little impact on re-admission rates for vaginally delivered newborns and was not cost saving. A lack of home postpartum follow-up may explain the absence of saving. Many Western countries already practiced early postpartum discharge for more than a decade. For these countries, what was once considered early discharge is now a conventional length of postnatal stay. This may explain the lack of recent published RCTs on the subject. However, countries with longer lengths of stay such as France and Belgium may benefit from testing shorter lengths of stay in studies with an appropriate design.
The second reason to interpret the findings with caution relates to the quality of the included studies. GRADE assessment highlighted numerous limitations in methods leading to (very) low level of evidence (see Additional file 1), except for three outcomes with moderate level of evidence (counselling, neonatal mortality rate at 3 weeks, and need for neonatal health contact within 10 days). The outcome related to satisfaction, only reported in the RCTs, was not discussed in this systematic review because trials were performed from 10 to 39 years ago, and thus societal expectations on health care are likely to have dramatically changed. Among the main methodological limitations found in the included studies were: small sample sizes that lead to insufficient power, a large number of lost to follow-up, one study with poor reporting of outcomes using graphical presentation but no discussion on the data in numerical terms, and heterogeneity in results across studies, leading to conflicting conclusions.
In addition, the selection criteria of study participants in RCTs were too restrictive, including well-educated women, mothers living in a stable relationship with their partners and low socioeconomic risk, preventing the generalisation of findings to the real world population. Selection bias was also observed in one non-randomised study [27] because more healthy mothers and newborns without financial difficulties were included in the early discharged group.
Besides the cautions in evidence interpretation, approximating the number of mother-infant dyads that can benefit from early discharge is challenging. Yanover et al. estimated that 25% of all deliveries are eligible for early discharge (i.e. after approximately 1 day). The authors used the readiness of the family as a necessary condition for discharge [32]. This criterion is indeed crucial for a successful early discharge programme because of a positive association between unreadiness at postpartum discharge and, on the one hand, health care use and, on the other hand, poorer health outcomes within 4 weeks after discharge [18]. The readiness to be discharged can be defined as the agreement between the mother and the medical staff (i.e. paediatrician and obstetrician) that both mother and newborn will not be likely to benefit from a longer hospital stay. If one of the involved parties anticipates any potential benefits for mother or infant to stay longer, the dyad is considered as unready [18].
Therefore, early discharge criteria cannot only focus on clinical parameters as described in Sainz et al. [31] but should also include additional criteria regarding the prenatal preparation and the setting of home postpartum follow-up as foreseen in the French guideline on early postpartum discharge [38]. In addition, prenatal preparation, content, frequency and duration of home follow-up were extremely different across studies hampering our ability to highlight best practices in these domains. In a Cochrane systematic review, the authors assessed the outcomes for women and babies of different home-visit schedules up to 42 days after birth whatever the length of hospital stay [39]. They concluded that postnatal home visits may promote infant health and maternal satisfaction but the frequency, timing and duration of such postnatal care visits should be based upon local needs. As in our systematic review, an optimal package of home postnatal care cannot be defined. However, several countries are developing a range of strategies to deliver seamless individualized follow-up support using telemedicine tools such as video conferencing or apps [40]. Nevertheless, all those strategies are unlikely to respond fully to the existing concerns about continuity of care. In addition, the shift of the follow-up tasks from hospital to home with physically or virtually present carers raises concerns about medical responsibility and legal accountability. Finally, the availability of professionals to provide the home care is an essential prerequisite for the successful transition from hospital to postpartum home care without impairing the home care for other conditions [41], creating unmet needs, or using informal support workers as doulas [42]. Due to the risk of variations in content and quality of care provided by fragmented services across multiple carers, offering a seamless transition from hospital to home is challenging.
Cost containment is one of the drivers to endorse an early postpartum discharge policy. Only two trials included in our systematic review addressed the cost issue. In the first study implemented in the USA [32],the authors analysed an early discharge programme, which included 24 h hospital length of stay and daily home visits by trained nurses for 4 days after birth. From a hospital perspective, this programme provided a minimum of 30% immediate savings in daily costs versus conventional stay (48 h or more), excluding saving generated by allocating vacated beds and rooms to other patients or purposes. The cost calculation was based on expenses for salaries of nurse practitioners, paramedical personnel, and medical consultants, as well as automobile expenses and home-care supplies. In the second study performing a cost calculation from a payer perspective in Spain [31], the implementation of an early discharge programme provided savings ranging from 18 to 20% in comparison with convention hospital length of hospital stay. This early discharge programme was made up of a less than 48 h length of hospital stay, 1 home visit after discharge by nurses qualified in puerperal and neonatal care, a practice consultation between 7 to 10 days after birth and a follow-up by phone at 1, 3 and 6 months. By comparison, the conventional discharge programme followed the same pattern except for the length of stay, which was longer than 48 h and the absence of home visits. The cost calculation took into account costs related to length of hospital stay, maternal – neonatal readmission, maternal – neonatal consultations, maternal – neonatal reassessment at 1 week and costs related to telephone follow-up. Cost containment due to the implementation of an early discharge policy is highly dependent on the perspective taken into account as well as on the type of health insurance system in place.
Estimation of possible cost savings cannot be performed without developing well designed RCTs including costs data collection. The collection of cost data must be designed to take into account not only hospital or payer perspectives, but also the societal perspective. In addition, the hidden costs for new mothers created by a potential shift from publicly funded hospital maternity care to private home-based postpartum care must be carefully scrutinized to prevent gaps in quality and accessibility of care [42].
Finally, developing quality indicators to monitor each early postpartum discharge programme is also crucial. Quality indicator assessment allows for adjusting early postpartum discharge policy when needed. However, the development of indicators is challenging because some indicators (e.g. satisfaction, overall support, well-being …) are qualitative and, thus more difficult to standardize [43].
Conclusions
The current available literature provides little scientific evidence to guide postpartum discharge policy planning. The evidence based on RCTs is old, with the most recent trial published 10 years ago, and the quality of evidence of these trials is poor. The more recent evidence is based only on two very poor quality non-randomised studies. In addition, the concept of early discharge itself is very variable across studies leading to health outcomes being measured at variable times after delivery. Despite these limitations, early discharge seems to be safe for both mother and newborn. Breastfeeding did not seem to be affected. Because of the lack of robust clinical evidence and full economic evaluations, the current data neither support nor discourage the widespread use of early postpartum discharge. Before implementing an early discharge policy, Western countries with longer length of hospital stay such as France and Belgium may benefit from testing shorter length of stay in studies with an appropriate design (e.g. randomised). The issue of cost containment in implementing early discharge and the potential impact on the current and future health of the population exemplifies the need for publicly funded clinical trials in such public health area. Finally, trials testing the range of out-patient interventions supporting early discharge are needed in Western countries which implemented early discharge policies in the past.
Abbreviations
- CI:
-
Confidence interval
- HAD scale:
-
Hospital anxiety and depression scale
- OR:
-
Odd ratio
- RR:
-
Risk ratio
References
Evans WN, Garthwaite C, Wei H. Nber: the impact of early discharge laws on the health of newborns. J Health Econ. 2008;27(4):843–70.
Fink AM. Early hospital discharge in maternal and newborn care. JOGNN. 2011;40(2):149–56.
Johansson K, Aarts C, Darj E. First-time parents' experiences of home-based postnatal care in Sweden. Ups J Med Sci. 2010;115(2):131–7.
OECD. Average length of stay: childbirth. Health: Key Tables from OECD, No. 51. 2014. doi:10.1787/l-o-s-childbirth-table-2014-1-en.
Brown S, Small R, Argus B, Davis PG, Krastev A. Early postnatal discharge from hospital for healthy mothers and term infants. Cochrane Database Syst Rev. 2009;3:CD002958.
De Luca D, Carnielli VP, Paolillo P. Neonatal hyperbilirubinemia and early discharge from the maternity ward. Eur J Pediatr. 2009;168(9):1025–30.
Danbjorg DB, Wagner L, Clemensen J. Do families after early postnatal discharge need new ways to communicate with the hospital? A feasibilility study. Midwifery. 2014;30(6):725–32.
Larsson B, Larsson G, Chantereau M, Staël von Holstein K. International comparisons of patients' views on quality of care. Int J Health Care Qual Assur Inc Leadersh Health Serv. 2005;18(1):62–73.
Moher M, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items fir systematic reviews and meta-analyses: the Prisma statement. PLoS Med. 2009;6(6):e1000097.
Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, Porter AC, Tugwell P, Moher D, Bouter LM. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology. 2007;7:10.
Higgins .JP.T, Green S (editors): Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]; 2011.
Balshem HHM, Schunemann HJ, Oxman AD, Kunz R, Brozek J. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–6.
Boulvain M, Perneger TV, Othenin-Girard V, Petrou S, Berner M, Irion O. Home-based versus hospital-based postnatal care: a randomised trial. BJOG. 2004;111:807–13.
Brooten D, Roncoli M, Finkler S, Arnold L, Cohen A, Mennuti M. A randomized trial of early hospital discharge and home follow up of women having caesarean birth. Obstet Gynecol. 1994;84(5):832–8.
Winterburn S, Fraser R. Does the duration of postnatal stay influence breast-feeding rates at one month in women giving birth for the first time? A randomized control trial. J Adv Nurs. 2000;32(5):1152–7.
Askelsdottir B, Lam-de Jonge W, Edman G, Wiklund I. Home care after early discharge: impact on healthy mothers and newborns. Midwifery. 2013;29(8):927–34.
Barker K. Cinderella of the services - ‘the pantomime of postnatal care’. Br J Midwifery. 2013;21(12):842.
Bernstein HH, Spino C, Lalama CM, Finch SA, Wasserman RC, McCormick MC. Unreadiness for postpartum discharge following healthy term pregnancy: impact on health care use and outcomes. Acad Pediatr. 2013;13(1):27–39.
Cambonie G, Rey V, Sabarros S, Baum TP, Fournier-Favre S, Mazurier E, Boulot P, Picaud JC. Early postpartum discharge and breastfeeding: an observational study from France. Pediatr Int. 2010;52(2):180–6.
Chanot A, Semet JC, Arnaud C, Dali-Youcef A, Abada K, Gayzard B, Lancelin F, Pax-Chochois S, Alves N, Curat AM et al: L'hospitalisation a domicile apres une sortie precoce de maternite. Soins 2009, Pediatrie, Puericulture.(246):24–26.
Chanot AA, Semet JC, Arnaud C, Dali-Youcef A, Abada K, Gayzard B, Lancelin F, Pax-Chochois S, Alves N, Curat AM, et al. Sorties precoces de maternite et hospitalisation a domicile: experience ariegeoise. Archives de Pediatrie. 2009;16(6):706–8.
De Carolis MP, Cocca C, Valente E, Lacerenza S, Rubortone SA, Zuppa AA, Romagnoli C. Individualized follow up programme and early discharge in term neonates. Ital J Pediatr. 2014;40:70.
Farhat R, Rajab M. Length of postnatal hospital stay in healthy newborns and re-hospitalization following early discharge. N Am J Med Sci. 2011;3(3):146–51.
Ghedin BS, Cancelier ACL, Feuerschuette OHM, Silveira SK. Healthy newborn length of hospital stay: influence on breastfeeding and neonatal morbidity. J Perinat Med. 2011;39(S1):159.
Gotink MJ, Benders MJ, Lavrijsen SW, Rodrigues Pereira R, Hulzebos CV, Dijk PH. Severe neonatal hyperbilirubinemia in the Netherlands. Neonatology. 2013;104(2):137–42.
Lain SJ, Roberts CL, Bowen JR, Nassar N. Early discharge of infants and risk of readmission for jaundice. Pediatrics. 2015;135(2):314–21.
Ramirez-Villalobos D, Hernandez-Garduno A, Salinas A, Gonzalez D, Walker D, Rojo-Herrera G, Hernandez-Prado B. Early hospital discharge and early puerperal complications. Salud Publica de Mexico. 2009;51(3):212–8.
Straczek H, Vieux R, Hubert C, Miton A, Hascoet JM. Sorties precoces de maternite : quels problemes anticiper ? Archives de Pediatrie. 2008;15(6):1076–82.
Carty E. C B: a randomized, controlled evaluation of early postpartum hospital discharge. Birth. 1990;17(4):199–204.
Hellman LM, Kohl SG. Early hospital discharge in obstetrics. Lancet. 1962;1:227–33.
Sainz Bueno JA, Romano MR, Teruel RG, Benjumea AG, Palacin AF, Gonzalez CA, Manzano MC. Early discharge from obstetrics-pediatrics at the hospital de Valme, with domiciliary follow-up. Am J Obstet Gynecol. 2005;193(3 Pt 1):714–26.
Yanover MJ, Jones D, Miller MD. Perinatal care of low-risk mothers and infants. Early discharge with home care. N Engl J Med. 1976;294(13):702–5.
Norma Oficial Mexicana “NOM-007-SSA2–1993": Atención de la Mujer durante el Embarazo, Parto y Puerperio y del Recién Nacido. Mexico City: Diario oficial de la Federación 1995.
Smith-Hanrahan C, Deblois D. Postpartum early discharge: impact of maternal fatigue and functional ability. Clin Nurs Res. 1995;4(1):50–66.
Waldenström U, Lindmark G. Early and late discharge after hospital birth. A comparative study of parental background characteristics. Scand J Soc Med. 1987;15:159–67.
Gagnon A, Edgar L, Kramer M, Papageorgiou A, Waghorn K, Klein MC. A randomized trial of a program of early postpartum discharge with nurse visitation. Am J Obstet Gynecol. 1997;176(1):205–11.
Lindberg I, Christensson K, Ohrling K. Parents’ experiences of using videoconferencing as a support in early discharge after childbirth. Midwifery. 2009;25(4):357–65.
Haute Autorité de Santé: Sortie de maternité après accouchement : conditions et organisation du retour à domicile des mères et de leurs nouveau-nés In.; 2014.
Yonemoto N, Dowswell T, Nagai S, Mori R. Schedules for home visits in the early postpartum period. Cochrane Database Syst Rev. 2013;7.
Danbjorg DB, Wagner L, Kristensen BR, Clemensen J. Intervention among new parents followed up by an interview study exploring their experiences of telemedicine after early postnatal discharge. Midwifery. 2015;31(6):574–81.
Cusack CL, Hall WA, Scruby LS, Wong ST. Public health nurses’ (Phns) perceptions of their role in early postpartum discharge. Can J Public Health. 2008;99(3):206–11.
Benoit C, Stengel C, Phillips R, Zadoroznyj M, Berry S. Privatisation & marketisation of post-birth care: the hidden costs for new mothers. Int J Equity Health. 2012;11:61.
Escuriet R, White J, Beeckman K, Frith L, Leon-Larios F, Loytved C, Luyben A, Sinclair M, van Teijlingen E, EU COST Action IS0907, et al. Assessing the performance of maternity care in Europe: a critical exploration of tools and indicators. BMC Health Serv Res. 2015;15:491.
Acknowledgements
Koen Van den Heede (PhD) and Jillian Harrison, KCE, for reviewing the final draft.
Funding
The research was funded by KCE (Belgian Healthcare Knowledge centre). The funding body played no role in the collection, analysis, interpretation of data or in writing the manuscript.
Availability of data and materials
Search strategy, methodological quality assessment of the evidence, list of excluded studies and grading of evidence are provided as additional materials.
Author information
Authors and Affiliations
Contributions
NB led the conception and design of the study, acquired the data, analysed and interpreted the data, wrote the first draft of the manuscript, revised critically and edited all versions. LSM made substantial contributions to the conception and design of the study, acquired the data and reviewed critically the manuscript for intellectual content. CD made substantial contributions to the conception and design of the study and reviewed critically the manuscript for intellectual content. NF designed the search strategy and reviewed critically the manuscript for intellectual content. WC made substantial contributions to the conception and design of the study, acquired the data and reviewed critically the manuscript for intellectual content. All authors approved the final manuscript and are accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval and consent to participate were not needed because of the study design (literature review).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Additional materials report detailed search strategy by database, assessment of the evidence using AMSTAR and Cochrane risk of bias tools, list of excluded studies including full references and level of evidence using GRADE system. (DOCX 125 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Benahmed, N., San Miguel, L., Devos, C. et al. Vaginal delivery: how does early hospital discharge affect mother and child outcomes? A systematic literature review. BMC Pregnancy Childbirth 17, 289 (2017). https://doi.org/10.1186/s12884-017-1465-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-017-1465-7