Abstract
Background
Maternity care in South Asia is available in both public and private sectors. Using data from demographic surveillance sites in Bangladesh, Nepal and rural and urban India, we aimed to compare institutional delivery rates and public-private share.
Methods
We used records of maternity care collected in socio-economically disadvantaged communities between 2005 and 2011. Institutional delivery was summarized by four potential determinants: household asset index, maternal schooling, maternal age, and parity. We developed logistic regression models for private sector institutional delivery with these as independent covariates.
Results
The data described 52 750 deliveries. Institutional delivery proportion varied and there were differences in public-private split. In Bangladesh and urban India, the proportion of deliveries in the private sector increased with wealth, maternal education, and age. The opposite was observed in rural India and Nepal.
Conclusions
The proportion of institutional delivery increased with economic status and education. The choice of sector is more complex and provision and perceived quality of public sector services is likely to play a role. Choices for safe maternity are influenced by accessibility, quantity and perceived quality of care. Along with data linkage between private and public sectors, increased regulation should be part of the development of the pluralistic healthcare systems that characterize south Asia.
Similar content being viewed by others
Background
Skilled birth attendance by a qualified healthcare provider is a critical requirement for safe maternity. Despite progress over the last two decades, inadequate care during pregnancy and delivery is largely responsible for an annual estimated 287 000 maternal and 2.9 million neonatal deaths worldwide [1]. Globally, about two-thirds of births take place in a health facility. However, in sub-Saharan Africa and South Asia - which together contribute over 85 % of maternal deaths - only half of deliveries are institutional [2].
The last two decades have seen considerable increases in institutional delivery rates in South Asia: from 4 to 29 % in Bangladesh between 1993 and 2011, from 26 to 79 % in India between 1992 and 2011, and from 8 to 35 % in Nepal between 1996 and 2011 [3–8]. There are, however, substantial urban-rural disparities in utilization of delivery care services. In most sub-Saharan African and South Asian countries, the proportion of institutional births in urban areas is double that in rural areas (76 %:40 %) [2]. In Bangladesh (2011), 49 % of urban women delivered in a health facility, compared with 23 % of rural women [4]. Comparative proportions were 71 and 31 % in India, and 52 and 15 % in Nepal [9].
National governments have taken measures to encourage institutional delivery and accelerate the slow and uneven improvement in maternal and neonatal health indicators. In 2007, Bangladesh introduced a pilot maternity voucher scheme through which mothers receive a payment for attending antenatal care and delivery at a public or private facility, or at home with a skilled birth attendant [10]. The scheme has reached more than 10 million people (~7 % of the population) across 31 sub-districts [11, 12]. Nepal began a safe delivery incentive scheme in 2005 and free deliveries have been available at government facilities since 2009 through the Aama Surakshya programme [13]. The Government of India launched the Janani Suraksha Yojana (JSY) - a national conditional cash transfer scheme - in 2005 to incentivize women of lower socioeconomic position to deliver at health facilities [14]. Launched in the same year, the Accredited Social Health Activist (ASHA) program, part of the National Health Mission, promotes institutional delivery for pregnant women in rural areas. ASHAs are trained local female community health volunteers who receive performance-based incentives for identifying pregnant women and helping them access health facilities [14, 15].
A linked approach is to encourage greater private sector participation in healthcare delivery. Concerns about the ability of governments to finance health services adequately, the poor performance of public service delivery systems [16], and the desire to expand client choice have led some countries to encourage the expansion of private sector healthcare [17]. In 2007, the Government of Gujarat, India, launched the Chiranjeevi Yojana, a public-private partnership in which the state pays accredited private obstetricians a fee for providing maternity services for poorer women [18, 19]. Some argue that inclusion of the private sector could allow governments to better target the poor and other vulnerable populations [20], and a trend toward increased share in maternal health service provision has been seen over the last decade. In many low-income countries the private sector now manages 40–50 % of health infrastructure and has broad and deep reach [21]. In Bangladesh, private sector institutional delivery care increased from 8 to 17 % between 2007 and 2011, in India from 11 to 21 % between 1993 and 2005, and in Nepal from 4 to 7 % between 2006 and 2011 [4, 8, 9].
Uptake of delivery care services is challenged by a range of factors and identifying and improving them is a priority. The literature suggests that, in addition to availability, distance, cost and quality of services, socio-economic and socio-demographic position are important predictors of institutional delivery [22–28]. Recent studies have highlighted associations with women’s economic status, educational status, age, and parity [29–31]. Our objective in this analysis was to document the share of private maternity care in different settings. Using data collected in community-based studies in Bangladesh, Nepal, and India, we aimed to examine the proportions of institutional deliveries provided by the private sector. We also examined the influence on place of delivery of household economic status, maternal education, age, and parity.
Methods
Study populations
We sourced information on maternity care from the surveillance systems of four cluster randomized controlled trials conducted in socio-economically disadvantaged communities between 2005 and 2011. They were run in three underserved rural districts in Bangladesh (Bogra, Maulvibazaar, and Faridpur) [32], in Dhanusha district in the southern Nepal Terai [33], in rural Jharkhand and Odisha states in eastern India [34], and in informal settlements in Mumbai [35]. Table 1 describes the characteristics of each study, including the types of health facilities available.
Health system contexts
Bangladesh made steady progress in almost all the health-related Millennium Development Goals (MDGs) over the past decade, through public and private sector activities. It attained the MDG 4 target for reduction in child mortality rate and has a falling maternal mortality ratio (MMR), one of the MDG 5 indicators. To achieve the MDG 5 target of births attended by skilled health personnel, the maternal health voucher scheme was operational in two of the three districts covered by our study (Faridpur and Maulvibazaar). Public facilities in all three districts included district hospitals, maternal and child welfare centres, and upazilla health complexes. Private facilities included small-to-medium-size clinics, BRAC (non-government) facilities, and larger private hospitals.
Nepal attained the MDG 4 target for reduction in child mortality and marginally attained the MDG 5 target for reduction in MMR. There has been some consideration of how this was achieved, given a widespread breakdown in governance during the insurrection, but a national Maternity Incentive Scheme (MIS) was implemented in 2005 and was operational during data collection. Dhanusha district had one zonal hospital, a private medical college hospital equipped for comprehensive obstetric care, public health posts, and a range of small private facilities. At the time of data collection the MIS was available only through public health providers.
India almost attained the MDG 4 and MDG 5 targets. The rural data from India were collected between 2005 and 2008. The JSY was launched in 2005 and beginning to be operational in study areas towards the end of 2008, so that its impact was unlikely to be reflected. In the urban setting, mothers with Below Poverty Line cards were eligible for the JSY cash incentive for delivery at a health facility [36]. The urban India study included informal settlements in Mumbai with a wealth of public and private providers [37]. Public facilities included primary, secondary, and tertiary institutions run by the municipal corporation. Municipal and government health infrastructure together constituted half of the inpatient care available in the city, the rest being provided by private hospitals and clinics.
Data collection
The participants were women of reproductive age (15–49 years) who delivered in the study areas during the data collection period and who consented to be interviewed around six weeks after delivery. All the sites operated vital registration systems that monitored births, stillbirths, and neonatal deaths identified by female community-based informants covering 250–350 households each. Reports were verified by trained interviewers and informants remunerated for correct identification. In Bangladesh, rural India, and urban India, women were visited six weeks after delivery for a postpartum interview. In Nepal, births in the study area were registered and interviews conducted after all births in small clusters and in a random sample of 10 births per month in larger clusters. Interviews were predominantly based on closed questions about antenatal, delivery, and postnatal events.
Dependent variables
The outcome of interest was institutional delivery in the public or private sector, based on the reported type or name of the institution.
Independent variables
We chose variables purposively from the available dataset, to reflect socioeconomic position (household asset index, maternal schooling) and demography (maternal age, parity). Household economic position was defined by tertiles of an asset index developed from standardized weights of the first component of a principal components analysis [38, 39]. Scores were calculated separately for each site. Maternal education was categorized as none, primary, secondary, or higher. Maternal age was categorized as under 20, 20–24, 25–29, or 30+ years. Gravidity was represented by a binary variable: primigravid or multigravid.
Statistical analysis
The original trials were designed to evaluate the impact of participatory women’s groups on maternal and neonatal health outcomes [32–35, 40], and we restricted our analysis to residents of control areas who reported a birth in the trial period. We summarized sites of delivery and choice of provider by socio-economic and socio-demographic position, with frequencies and percentages. The denominators were all deliveries for institutional delivery, and institutional deliveries for private sector delivery. We entered private sector institutional delivery as the dependent variable in a series of univariable logistic regression models, including a random effect for cluster, for each of the four independent variables. A multivariable model included all four of them as covariates. The analysis was run for each trial separately in Stata13 (Stata, College Station, TX, USA).
Ethical approval
Data for the study originated with trials that had received ethical approval from the ethics committee of the Diabetic Association of Bangladesh, an independent ethics committee in Jamshedpur, Jharkhand, India, the Nepal Health Research Council, the Municipal Corporation of Greater Mumbai and the Independent Ethics Committee for Research on Human Subjects (Mumbai, India), and the ethics committee of the Institute of Child Health, University College London.
Results
The data described 52 750 deliveries across four sites: 23 608 in rural Bangladesh, 14 079 in rural Nepal, 8978 in rural India, and 6085 in informal slum settlements in urban India. Table 2 summarises characteristics of the participants. In rural Nepal and India, most women had not been to school. Generally, when women had done so they had attended up to secondary level at all sites. Adolescent pregnancy appeared more common in rural Nepal, and women had their pregnancies later in urban India. About one-third of women were delivering their first child.
Table 3 summarizes the proportions of deliveries that were home or institutional, and, when institutional, public or private. There was variation between sites in the proportion of institutional delivery, which was routine in urban informal settlements (92 %), but used by less than 30 % of women at other sites. In the event of institutional delivery, there were substantial differences in public-private split, which was 84:16 in rural Nepal, but 23:77 in rural India. The two phases of the rural Bangladesh dataset showed obvious changes over time: the first was collected from 2005 to 2007 and the second from 2009 to 2011. Institutional deliveries were uncommon in the first phase (17 %) and more than half (55 %) of them took place in public facilities. In the second phase, institutional delivery had risen to 29 % and now favored the private sector (58 %). Institutional delivery rates were low in rural Nepal (25 %). The type of institution was not known in 124 cases, but fell predominantly to the public sector (84 %). Institutional delivery was uncommon in the dataset from rural India. When it was chosen, the private sector was preferred in 77 % of cases. Preference for the private sector was much greater in rural than in urban India (42 %). The results for women in informal settlements in urban India included only those who delivered in Mumbai, and not those who went back to their places of origin for delivery (1387).
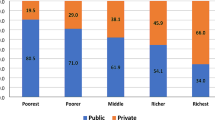
Figure 1 summarizes type of delivery care provider by socio-economic and socio-demographic position (Additional file 1: Table S1). The proportion of institutional delivery increased with economic status and higher educational attainment across all sites. Younger women were more likely to deliver at an institution, although teenagers were slightly less likely to do so than women in their early twenties in rural India and Bangladesh in the earlier phase. When deliveries were institutional, the proportion of private sector use increased with wealth and education, although the difference in urban India was only marked for women with higher education. Greater proportions of younger women delivered in the private sector at rural sites, but private sector delivery increased with age in urban India. Greater proportions of women in their first pregnancies delivered in the private sector, although the difference was small in urban India.
Table 4 summarizes the findings of logistic regression models with private institutional delivery as the dependent variable. Public-private split differed across the sites. Increasing economic status was associated with greater odds of private sector delivery in rural Bangladesh and urban India, but there was a suggestion that poorer women had greater odds of private sector delivery in rural Nepal and India. Increasing maternal education was associated with greater odds of private sector delivery in rural Bangladesh and in the highly educated in urban India, but lesser odds in rural India. The association of increasing maternal age with increasing odds of private sector delivery was confirmed in rural Bangladesh (phase 1) and urban India, but not in rural Nepal and India (although the numbers were smaller). Primigravid women had greater odds of private institutional delivery in rural Bangladesh and urban India, but lesser odds in rural Nepal and rural India.
Discussion
Findings
Our analysis of data from 52 750 births in three South Asian countries over six years showed broad variation in rates of institutional delivery and public-private split across study sites and between socio-economic and socio-demographic groups. There were substantial differences in institutional delivery proportion between rural and urban areas, by a factor of about three. There were also socio-economic and socio-demographic disparities in institutional maternity care, with women from lower socio-economic and educational backgrounds less likely to have institutional delivery. Use of the private sector differed between sites. In Bangladesh and urban India, it was greater for wealthier, better educated, and older women. The opposite was observed in rural India and, perhaps, in rural Nepal (the numbers were small), in which greater proportions of poorer, less educated, multigravid women delivered at private rather than public facilities.
Limitations
Our analysis had some limitations. All the participants could be classified as poor according to international metrics. We used principal components analysis to generate asset indices for each site, but the index distributions were highly positively skewed to a degree to which normalization by transformation was not possible. For this reason, quantiles of asset index did not yield groups of equal size from some of the sites. Secondly, classification of institutions as public or private was not possible using the raw data in <1 % of cases. We should also be aware of the variable nature of private care, particularly in terms of its categorization as for-profit or not-for-profit. Institutions such as charitable trusts and non-government organisations were classified as private when in some cases – Bangladesh being a good example – the cost to clients may have been similar to the costs of public sector care. Finally, there have been increases in institutional delivery since the study period. More recent data from the rural India site, for example, suggest that the proportion had reached 50 % by 2011 [41].
Institutional delivery
The finding of low prevalence of institutional delivery in South Asian countries is consistent with previous research. At three of the four sites, less than one-third of births were institutional. In rural Bangladesh, institutional delivery rates in the first and second phases were low and corroborate national Demographic and Health Survey (DHS) data for the corresponding periods (11 % in 2007 and 23 % in 2011) [4, 42]. In Nepal, home birth continues to predominate, especially in rural areas, and our findings validate the low proportion of institutional delivery reported by the Ministry of Health and Population (25 %) [8]. Neither 24-h comprehensive obstetric care nor the Maternity Incentive Scheme were available at private health facilities in the Nepal site at the time of the study, which may explain the lower usage in this area. In rural India, one-in-five births was institutional, compared with a District Level Household and Facility Survey (DLHS) national figure of 38 % in 2007–8 [43]. This difference is probably due to the fact that the Jharkhand and Odisha sites were home to a high proportion of underserved tribal communities with poor access to health services. In contrast, residents of urban India have access to a range of health services in both public and private sectors. Most of the births in urban Mumbai were institutional (92 %), and this agrees with roughly concomitant data from the third National Family Health Survey (83 %) [44]. The urban-rural differences were somewhat predictable. A systematic review of determinants of maternal health service use found that urban, wealthier women were more likely to have institutional deliveries [45]. Explanations include the fact that women in urban areas tend to be better educated, live nearer to health services, have access to more extensive transport systems, and may have greater autonomy and access to information [46, 47].
Determinants
Our findings support those of studies that show economic conditions to be an important predictor of institutional delivery [48, 49]. Women of low economic position are less likely to use maternal health services, and we observed a systematic increase in institutional delivery with increasing wealth at all sites. Our analysis also corroborates the findings of studies which suggest that maternal education [50], household wealth, and urban-rural residence have important and consistent effects on utilization of health services for delivery [23, 28, 51–53]. Education is a key determinant of access and utilization. Fewer women had schooling in rural areas of Nepal (26 %) and India (32 %) and we saw fewer institutional deliveries in these areas. In comparison, a higher proportion of women reported institutional delivery in Bangladesh, where educational attainment was higher (72 % of women reported some schooling in phase 1 and 82 % in phase 2). The proportion of institutional delivery was also higher in urban India, where 56 % of women reported completing secondary education. Other determinants of healthcare uptake include age and parity. Most of our study participants were young and one-third were primigravid. Several South Asian studies have shown that women in their first pregnancies are more likely to deliver at a health facility and with a skilled birth attendant [8, 23, 27, 54]. Our findings suggested a substantial influence of parity on utilization of delivery care, with younger women more likely to have their first birth in a health facility.
Uptake of private sector delivery
Private sector delivery is increasing over time, with positive associations with wealth and education, previous private sector delivery, and – to a lesser extent – primiparity [55]. In rural Nepal, Bangladesh, and urban India, the public sector was still a major provider of care for women who chose institutional delivery. Availability of better public health infrastructure combined with accessibility may have led to increased utilization compared with the private sector in urban informal settlements in India. A shift from public sector to private sector delivery was seen in the second phase of the Bangladesh study.
Private sector healthcare is heterogeneous in the South Asian context of medical pluralism. Bangladesh is served by a mix of public and private sector providers in which not-for-profit facilities play a major part. India, by contrast, has a dominant private sector. Around 70 % of total health expenditure in 2012 was private, 61 % was out-of-pocket, and 75 % of outpatient visits and 62 % of inpatient episodes were in the private sector. Out-of-pocket expenditure at public sector facilities was low, at 2 % [56]. Nepal can be classified as having a “stratified private sector shaped by low incomes and public sector characteristics” [57]. Around 61 % of total health expenditure in 2012 was private, 49 % was out-of-pocket, and 65 % of outpatient visits and 46 % of inpatient episodes were in the private sector. Out-of-pocket expenditure at public sector facilities was 7 % [57].
Bangladesh has seen a steady increase in institutional deliveries [50]. DHS analyses suggest a rise from 2 % in 1996 to 17 % in 2011 [20], most of which was accounted for by use of the private sector [55]. Wealth-related inequality in institutional delivery seems to have fallen [20, 50], more rapidly in urban than in rural areas, and the private sector is becoming the major provider of maternity care [58]. Much of this private provision is not-for-profit [59], and the nongovernmental health sector is now double the size of the government sector [60]. Similar trends were observed in rural India, where more than three-quarters of institutional deliveries were in private facilities. DHS estimates suggest an increase in institutional delivery of about 7 % between 1998 and 2005, most of which was accounted for by the private sector [55]. In this case, private care is predominantly for-profit. Unlike in Bangladesh and India, most of the increase in institutional deliveries in Nepal was accounted for by the public sector [55], although private delivery increased from 1 % in 1996 to 10 % in 2011 [20].
Preference for private healthcare
Healthcare quality can be seen as a combination of service quality (the user experience) and technical quality (the clinical process). Service quality appears to be higher in the private sector [61–64], and users generally consider private care to be better than public in terms of responsiveness, longer opening hours, appointment systems, shorter waiting times, confidentiality, cleanliness, and privacy [65, 66]. These qualities may appeal to those who can afford them because they respond to women’s busy schedules and desire for positive experiences of health care [67]. The technical quality of private sector services may not be as good as in the public sector [63, 64], but this does not apply across the board: mapping of health facility signal functions across Bangladesh in 2007–2008 suggested that emergency obstetric services such as caesarean section and blood transfusion were available at a higher proportion of private than of public sector health facilities [68], and recent considerations have emphasized the benefits of pluralism [60]. In rural India, and possibly in rural Nepal, concerns about the availability and quality of care may have exacerbated other geographic, financial and social barriers, deterring women from delivering in health facilities unless they experienced antepartum or intrapartum complications [69, 70]. Comprehensive obstetric care was available in the Nepal site only at the regional public hospital and one or two private facilities. If institutional deliveries were often a response to anticipated or actual complications, women may have preferred the private sector if they thought that skilled care, and particularly emergency obstetric care, would be more readily available there.
Economic status is believed to be the strongest influence on choosing between a private-for-profit or public facility for institutional delivery [71]. In Bangladesh and urban India, women from wealthier backgrounds were more likely to deliver at private facilities [72]. In rural Nepal and India, amongst the subset of the population that delivered at institutions that were less poor, better educated, more likely to be younger and primigravida than those delivering at home, economic status was negatively associated with private care. Wealthier women in rural India may have had access to better quality public services, or have been more empowered to navigate their way through the public system. It is also possible that poorer women and those from tribal and Scheduled Caste communities may have feared discrimination in public facilities and avoided them as a result [62, 73–75], despite the burden of out-of-pocket expenditure on private care [76]. Incentive programs have increased institutional delivery in the public sector, but there is a pressing need to monitor quality of care [16]. A recent evaluation of the JSY suggests that the scheme has led to an increase in births in public facilities and substitution away from the private sector. Importantly, poorer women were more likely than wealthier women to give birth in a public health facility in response to the scheme [77], although it did not compensate fully for the financial stress of complicated deliveries [78]. In rural Nepal, the Maternity Incentive Scheme was introduced around the beginning of our data collection and at that time less poor and more educated women were more likely to access it [79]. Since the incentive was only available through public providers, it may have been that over most of the data collection period better-educated and less poor women came to know of it and responded to it by choosing public sector institutional delivery, whilst poorer families were less aware of the scheme and sought private care when they perceived deliveries to be high-risk.
Conclusions
Although some suggest that the gap between health infrastructure and attainment would best be filled through public-private partnership [80], the evidence for the potential of large, private for-profit services to provide healthcare at scale for low-income groups in low- and middle-income countries is limited and mostly includes providers in urban and peri-urban India [66]. As economic wherewithal and education increase, families move toward institutional delivery. The choice of sector is more complex and the provision and perceived quality of public sector services is likely to play a role, as are institutional delivery incentive schemes. Where a mix of public and private services is available, families arrange for young women to deliver in either. We think that the precise split depends on the reputation of public sector services: fairly good in Mumbai (58 % of institutional deliveries) and less good than private sector services in rural Bangladesh (42 %). This proposition holds for rural Nepal and rural India too, but is augmented by limitations to available services. In rural Nepal, the small proportion of women who chose institutional delivery did so at public sector facilities, which may be less about reputation than about the availability and affordability of private sector delivery in rural areas. Choices for safe maternity are influenced by accessibility, quantity, and perceived quality of care, and the balance between public and private provision shifts with time and place. We need more information on healthcare uptake and activities, including linkage of records from private for-profit and not-for-profit services [60]. We recommend, as have others [59], the inclusion of more refined descriptors of place of institutional delivery in national and subnational surveys.
We support calls for increases in the numbers and training of skilled human resources in the public sector [68]. There is also some evidence that disrespect and abuse associated with maternity services can be reduced through interventions that work with policymakers, train providers, and strengthen links between facility and community [81].
The evidence base for interventions to improve private sector quality in low- and middle-income countries is limited [59]. In a recent review, Montagu and Goodman discuss four approaches: prohibition of private practice, encouragement and subsidy for delivery of selected services, purchase of private services by the public sector, and operational constraint through regulation. In the context of fairly open economies, the first of these - prohibition - has had only limited success. Encouragement of institutional delivery is best represented by the incentive schemes already operational in all three countries, and purchase is best represented by systems like the Chiranjeevi Yojana or by voucher programs [82, 83].
We support calls for regulation, accreditation, and accountability frameworks [60, 64, 84]. Constraint through statutory regulation such as licensing, quality control, or prescription limitations continues to be problematic. There are also some obstacles to self-regulation. Regulation by professional organisations has to take account of the fact that practitioners may work in both private and public sectors, and voluntary accreditation has cost implications and relies on the involvement of a majority of providers. Nevertheless, increased regulation – along with data linkage – should be part of the rational development of the pluralistic healthcare systems that characterize south Asia.
Abbreviations
- aOR:
-
Adjusted odds ratio
- ASHA:
-
Accredited Social Health Activist. India National Health Mission
- BRAC:
-
Bangladesh Rural Advancement Committee (Building Resources Across Communities)
- CI:
-
Confidence interval
- DHS:
-
Demographic and Health Survey
- DLHS:
-
District Level Household and Facility Survey, India
- JSY:
-
Janani Suraksha Yojana. India safe delivery incentive program
- MDG:
-
Millennium Development Goal
- MIRA:
-
Mother and Infant Research Activities, Nepal
- MMR:
-
Maternal mortality ratio
- OR:
-
Odds ratio
- SNEHA:
-
Society for Nutrition, Education and Health Action, Mumbai, India
- UCL:
-
University College London
References
WHO, UNICEF. Countdown to 2015: maternal, newborn & child survival. Building a future for women and children: the 2012 report. Geneva: World Health Organization and United Nations Children’s Fund; 2012.
UN. The Millennium Development Goals Report 2015. New York: United Nations; 2015.
Mitra SN, Nawab Ali M, Islam S, Cross AR, Saha T. Bangladesh Demographic and Health Survey 1993–1994. Calverton: National Institute of Population Research and Training (NIPORT), Mitra and Associates, Macro International Inc; 1994.
National Institute of Population Research and Training (NIPORT), Mitra and Associates, ICF International. Bangladesh Demographic and Health Survey 2011. Dhaka and Calverton: NIPORT, Mitra and Associates, ICF International; 2013.
International Institute for Population Sciences. Macro International: National Family Health Survey (NFHS 1), 1992–93. Mumbai: IIPS; 1995.
Ministry of Health and Family Welfare. Family welfare statistics in India. New Delhi: Government of India, Statistics Division; 2011.
Pradhan A, Aryal R, Regmi G, Ban B, Govindasamy P. Nepal Family Health Survey 1996. Calverton, Maryland and Kathmandu: His Majesty’s Government, Nepal, Ministry of Health; New ERA; Macro International Inc; 1997.
Ministry of Health and Population, New ERA, ICF International. Nepal Demographic and Health Survey 2011. Calverton: Ministry of Health and Population, New ERA, ICF International; 2012.
Wang W, Alva S, Wang S, Fort A. Levels and trends in the use of maternal health services in developing countries. DHS Comparative Reports No. 26. Calverton: ICF Macro; 2011.
Ministry of Health and Family Welfare. Health Bulletin 2013. Dhaka: Government of the People’s Republic of Bangladesh, Management Information System, Directorate of Health Services; 2014.
Schmidt J-O, Ensor T, Hossain A, Khan S. Vouchers as demand side financing instruments for health care: A review of the Bangladesh maternal voucher scheme. Health Policy. 2010;96:98–107.
Ahmed S, Khan MM. A maternal health voucher scheme: what have we learned from the demand-side financing scheme in Bangladesh? Health Policy Plan. 2011;6:25–32.
Witter S, Khadka S, Nath H, Tiwari S. The national free delivery policy in Nepal: early evidence of its effects on health facilities. Health Policy Plan. 2011;26 Suppl 2:ii84–91.
Lim SS, Dandona L, Hoisington JA, James SL, Hogan MC, Gakidou E. India’s Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: an impact evaluation. Lancet. 2010;375:2009–23.
Ministry of Health and Family Welfare. Guidelines for Janani-Shishu Suraksha Karyakram (JSSK). New Delhi: Government of India; 2011.
Kumar S, Dansereau E. Supply-side barriers to maternity-care in India: a facility-based analysis. PLoS One. 2014;9:e103927.
Newbrander W, Moser P. The future of health sector reform in Asia. In: Newbrander W, Moser P, editors. Private Health Sector Growth in Asia Issues and implications. New York: Wiley; 1997. p. 221–34.
De Costa A, Vora KS, Ryan K, Sankara Raman P, Santacatterina M, Mavalankar D. The state-led large scale public private partnership ‘Chiranjeevi Program’ to increase access to institutional delivery among poor women in Gujarat, India: How has it done? What can we learn? PLoS One. 2014;9:e95704.
Mohanan M, Bauhoff S, La Forgia G, Babiarz KS, Singh K, Miller G. Effect of Chiranjeevi Yojana on institutional deliveries and neonatal and maternal outcomes in Gujarat, India: a difference-in-differences analysis. Bull WHO. 2014;92:187–94.
Hotchkiss DR, Godha D, Do M. Expansion in the private sector provision of institutional delivery services and horizontal equity: evidence from Nepal and Bangladesh. Health Policy Plan. 2014;29 Suppl 1:i12–9.
Harding A. Partnerships with the private sector in health: what the international community can do to strengthen health systems in developing countries. Washington DC: Center for Global Development; 2009.
Sharma SR, Poudyal AK, Devkota BM, Singh S. Factors associated with place of delivery in rural Nepal. BMC Public Health. 2014;14:306.
Agha SB, Carton TW. Determinants of institutional delivery in rural Jhang, Pakistan. Int J Equity Health. 2011;10:31.
Ministry of Health and Population. Annual report: Department of Health Services. 2068/69 (2011/2012). Kathmandu: Government of Nepal; 2012.
Islam N, Islam MT, Yoshimura Y. Practices and determinants of delivery by skilled birth attendants in Bangladesh. Reproductive Health. 2014;11:86.
Anwar I, Sami M, Akhtar N, Chowdhury M, Salma U, Rahman M, Koblinsky M. Inequity in maternal health-care services: evidence from home-based skilled-birth-attendant programmes in Bangladesh. Bull WHO. 2008;86:252–9.
Dhakal S, van Teijlingen E, Raja EA, Dhakal KB. Skilled care at birth among rural women in Nepal: practice and challenges. J Health Popul Nutr. 2011;29:371–8.
Jat TR, Ng N, San Sebastion M. Factors affecting the use of maternal health services in Madhya Pradesh state of India: a multilevel analysis. Int J Equity Health. 2011;10:59.
Abeje G, Azage M, Setegn T. Factors associated with Institutional delivery service utilization among mothers in Bahir Dar City administration, Amhara region: a community based cross sectional study. Reprod Health. 2014;11:22.
Feyissa TR, Genemo GA. Determinants of institutional delivery among childbearing age women in Western Ethiopia, 2013: unmatched case control study. PLoS One. 2014;9:e97194.
Kawakatsu Y, Sugishita T, Oruenjo K, Wakhule S, Kibosia K, Were E, Honda S. Determinants of health facility utilization for childbirth in rural western Kenya: cross-sectional study. BMC Pregnancy Childbirth. 2014;14:265.
Azad K, Barnett S, Banerjee B, Shaha S, Khan KS, Rego AR, Barua S, Flatman D, Pagel C, Prost A, et al. Effect of scaling up women’s groups on birth outcomes in three rural districts in Bangladesh: a cluster-randomised controlled trial. Lancet. 2010;375:1193–202.
Shrestha BP, Bhandari B, Manandhar DS, Osrin D, Costello A, Saville N. Community interventions to reduce child mortality in Dhanusha, Nepal: study protocol for a cluster randomized controlled trial. Trials. 2011;12:136.
Tripathy P, Nair N, Barnett S, Mahapatra R, Borghi J, Rath S, Rath S, Gope R, Mahto D, Sinha R, et al. Effect of a participatory intervention with women’s groups on birth outcomes and maternal depression in Jharkhand and Orissa, India: a cluster-randomised controlled trial. Lancet. 2010;375:1182–92.
Shah More N, Bapat U, Das S, Alcock G, Patil S, Porel M, Vaidya L, Fernandez A, Joshi W, Osrin D. Community mobilization in Mumbai slums to improve perinatal care and outcomes: a cluster randomized controlled trial. PLoS Med. 2012;9:e1001257.
Ministry of Health and Family Welfare. Janani Suraksha Yojana: guidelines for implementation. New Delhi: Government of India; 2006.
Shah More N, Alcock G, Bapat U, Das S, Joshi W, Osrin D. Tracing pathways from antenatal to delivery care for women in Mumbai, India: cross-sectional study of maternity in low-income areas. International Health. 2009;1:71–7.
Filmer D, Pritchett L. Estimating wealth effects without expenditure data - or tears: an application to educational enrollments in states of India. Demography. 2001;38:115–32.
Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21:459–68.
Fottrell E, Azad K, Kuddus A, Younes L, Shaha S, Nahar T, Aumon BH, Hossen M, Beard J, Hossain T, et al. The effect of increased coverage of participatory women’s groups on neonatal mortality in Bangladesh: A cluster randomized trial. JAMA Pediatr. 2013;167(9):816–25.
Sarbani Roy S, Mahapatra R, Rath S, Bajpai A, Singh V, Rath S, Nair N, Tripathy P, Gope RK, Sinha R, et al. Improved neonatal survival after participatory learning and action with women’s groups: a prospective study in rural eastern India. Bull WHO. 2013;91:426–33.
National Institute of Population Research and Training (NIPORT), Mitra and Associates, ICF International. Dhaka and Calverton. Maryland: NIPORT, Mitra and Associates, ICF International; 2007. p. 2009.
International Institute for Population Sciences. District Level Household and Facility Survey 2007–08. Mumbai: Government of India Ministry of Health and Family Welfare; 2010.
Government of India Ministry of Health and Family Welfare. National Family Health Survey, India (NFHS-3 2005–06). Mumbai: International Institute for Population Sciences; 2007.
Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bull WHO. 2007;85:812–9.
Teferra AS, Alemu FM, Woldeyohannes SM. Institutional delivery service utilization and associated factors among mothers who gave birth in the last 12 months in Sekela District, north west of Ethiopia: a community-based cross sectional study. BMC Pregnancy Childbirth. 2012;12:74.
Afful-Mensah G, Nketiah-Amponsah E, Boakye-Yiadom L. Rural–urban differences in the utilization of maternal healthcare in Ghana: the case of antenatal and delivery services. Afr Soc Sci Rev. 2014;6:42–63.
Gabrysch S, Campbell O. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy Childbirth. 2009;9:34.
Tsawe M, Moto A, Netshivhera T, Ralesego L, Nyathi C, Susuman AS. Factors influencing the use of maternal healthcare services and childhood immunization in Swaziland. Int J Equity Health. 2015;14(1):32.
Anwar I, Nababan HY, Mostari S, Rahman A, Khan JAM. Trends and inequities in use of maternal health care services in Bangladesh, 1991–2011. PLoS One. 2015;10, e0120309.
Tey NP, Lai SL. Correlates of and barriers to the utilization of health services for delivery in South Asia and Sub-Saharan Africa. Scientific World Journal. 2013;2013:423403.
Ahmed S, Creanga AA, Gillespie DG, Tsui AO. Economic status, education and empowerment: implications for maternal health service utilization in developing countries. PLoS One. 2010;5(6):e11190.
Chakraborty N, Islam MA, Chowdhury RI, Bari W, Akhter HH. Determinants of the use of maternal health services in rural Bangladesh. Health Promot Int. 2003;18(4):327–37.
Wagle RR, Sabroe S, Nielsen BB. Socioeconomic and physical distance to the maternity hospital as predictors for place of delivery: an observation study from Nepal. BMC Pregnancy Childbirth. 2004;4(1):8.
Pomeroy AM, Koblinsky M, Alva S. Who gives birth in private facilities in Asia? A look at six countries. Health Policy Plan. 2014;29:i38–47.
Prinja S, Bahuguna P, Gupta R, Sharma A, Rana SK, Kumar R. Coverage and financial risk protection for institutional delivery: how universal is provision of maternal health care in India? PLoS One. 2015;10:e0137315.
Mackintosh M, Channon A, Karan A, Selvaraj S, Cavagnero E, Zhao H. What is the private sector? Understanding private provision in the health systems of low-income and middle-income countries. Lancet. 2016;388:596–605.
Kamal N, Curtis S, Hasan MS, Jamil K. Trends in equity in use of maternal health services in urban and rural Bangladesh. Int J Equity Health. 2016;15:27.
McPake B, Hanson K. Managing the public-private mix to achieve universal health coverage. Lancet. 2016;388:622–30.
Ahmed SM, Evans TG, Standing H, Mahmud S. Harnessing pluralism for better health in Bangladesh. Bangladesh: innovation for universal health coverage 2. Lancet. 2013;382:1746–55.
Bhatia J, Cleland J. Health care of female outpatients in south-central India: comparing public and private sector provision. Health Policy Plan. 2004;19(6):402–9.
Ergler CR, Sakdapolrak P, Bohle HG, Kearns RA. Entitlements to health care: why is there a preference for private facilities among poorer residents of Chennai, India? Soc Sci Med. 2010;72:327–37.
Basu S, Andrews J, Kishore S, Panjabi R, Stuckler D. Comparative performance of private and public healthcare systems in low- and middle-income countries: a systematic review. PLoS Med. 2012;9:e1001244.
Morgan R, Ensor T, Waters H. Performance of private sector health care: implications for universal health coverage. Lancet. 2016;388:606–12.
Mills A, Brugha R, Hanson K, McPake B. What can be done about the private health sector in low-income countries? Bull WHO. 2002;80:325–30.
Tung E, Bennett S. Private sector, for-profit health providers in low and middle income countries: can they reach the poor at scale? Globalization Health. 2014;10:52.
Alcock G, Das S, Shah More N, Hate K, More S, Pantvaidya S, Osrin D, Houweling TA. Examining inequalities in uptake of maternal health care and choice of provider in underserved urban areas of Mumbai, India: a mixed methods study. BMC Pregnancy Childbirth. 2015;15:231.
Alam B, Mridha MK, Biswas TK, Roy L, Rahman M, Chowdhury ME. Coverage of emergency obstetric care and availability of services in public and private health facilities in Bangladesh. Int J Gynecol Obstet. 2015;131:63–9.
Singh PK, Kumar C, Rai RK, Singh L. Factors associated with maternal healthcare services utilization in nine high focus states in India: a multilevel analysis based on 14 385 communities in 292 districts. Health Policy Plan. 2013;29:542–59.
Jeffery P, Jeffery R. Only when the boat has started sinking: a maternal death in rural north India. Soc Sci Med. 2010;71:1711–8.
Kesterton AJ, Cleland J, Sloggett A, Ronsmans C. Institutional delivery in rural India: the relative importance of accessibility and economic status. BMC Pregnancy Childbirth. 2010;10:30.
Shah More N, Bapat U, Das S, Barnett S, Costello A, Fernandez A, Osrin D. Inequalities in maternity care and newborn outcomes: one-year surveillance of births in vulnerable slum communities in Mumbai. Int J Equity Health. 2009;8(1):21.
Maiti S, Unisa S, Agrawal PK. Health care and health among tribal women in Jharkhand: a situational analysis. Stud Tribes Tribals. 2005;3:37–56.
Saroha E, Altarac M, Sibley L. Caste and maternal health care service use among rural Hindu women in Maitha, Uttar Pradesh, India. J Midwifery Women’s Health. 2008;53:e41–7.
Nayar KR. Social exclusion, caste & health: a review based on the social determinants framework. Indian J Med Res. 2007;126:355–63.
Sinha RK, Chatterjee K, Nair N, Tripathy PK. Out-of-pocket and catastrophic health expenditure: a cross-sectional assessment of a rural district of the state of Jharkhand in India. J Disease Global Health. 2015;4:130–40.
Powell-Jackson T, Masumder S, Mills A. Financial incentives in health: new evidence from India’s Janani Suraksha Yojana. J Health Econ. 2015;43:154–69.
Govil D, Purohit N, Gupta SD, Mohanty SK. Out-of-pocket expenditure on prenatal and natal care post Janani Suraksha Yojana: a case from Rajasthan, India. J Health Popul Nutr. 2016;35:15.
Powell-Jackson T, Neupane B. Evaluation of the Safe Delivery Incentive Programme: final report of the evaluation. Kathmandu: Support to the Safe Motherhood Programme; 2008.
Dutta S, Lahiri K. Is provision of healthcare sufficient to ensure better access? An exploration of the scope for public-private partnership in India. Int J Health Policy Management. 2015;4:467–74.
Abuya T, Ndwiga C, Ritter J, Kanya L, Bellows B, Binkin N, Warren CE. The effect of a multi-component intervention on disrespect and abuse during childbirth in Kenya. BMC Preg Childbirth. 2015;15:224.
Njuki R, Abuya T, Kimani J, Kanya L, Korongo A, Mukanya C, Bracke P, Bellows B, Warren CE. Does a voucher program improve reproductive health service delivery and access in Kenya? BMC Health Serv Res. 2015;15:206.
Bellows BW, Conlon CM, Higgs ES, Townsend JW, Nahed MG, Cavanaugh K, Grainger CG, Okal J, Gorter AC. A taxonomy and results from a comprehensive review of 28 maternal health voucher programmes. J Health Popul Nutr. 2013;31(4 Suppl 2):106–28.
Montagu D, Goodman C. Prohibit, constrain, encourage, or purchase: how should we engage with the private health-care sector? Lancet. 2016;388:613–21.
Acknowledgments
PCP would like to acknowledge the assistance of Badrun Nahar Bithi, assistant data manager, and Sanjit Kumer Shaha, surveillance manager. SNEHA would like to acknowledge the work of Ujwala Bapat, Sarita Patil, Leena Vaidya, Maya Porel, Latika Chordhekar, Danlaxmi Solanki, surveillance supervisors, field investigators, programme officers, and sakhis.
Funding
The work on this analysis was supported by the Economic and Social Research Council and the UK Department for International Development (ES/I033572/1). The Perinatal Care Project Bangladesh trial received funding from the Big Lottery Fund (IS/2/010281409) and the Wellcome Trust (85417MA/Z/08/Z). The Dhanusha Nepal trial received funding from the UBS Optimus Foundation, USAID, DfID and The Wellcome Trust. The Ekjut India trial was funded by the Health Foundation (1748/3001). The SNEHA India trial received funding from the ICICI Foundation for Inclusive Growth and The Wellcome Trust (081052). TAJH was also supported by a Research Excellence Initiative grant from Erasmus University. SD, GA and DO were supported by The Wellcome Trust (091561/Z/10/Z). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
The individual datasets analysed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
Study conception: SD, GA, DO, TH. Methodology: SD, GA, DO. Formal analysis, SD, GA, DO. Data collection: SD, GA, AK, BPS, SR, NSM, NS. Data curation: SD, AK, BPS, SR, NS. First manuscript draft: SD, DO. Critical review, commentary, revision of manuscript: SD, GA, KA, AK, DSM, BPS, NN, SR, NSM, NS, DO, TH. Manuscript preparation, data visualization: SD, DO. Supervision: KA, DSM, NN, NSM, NS, DO, TH. Project administration: KA, AK, DSM, BPS, SR, NS, DO, TH. Funding acquisition: DO, TH. All authors read and approved the final manuscript.
Competing interests
None of the authors has a competing interest.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1: Table S1.
Type of delivery care by socio-economic and socio-demographic position. (DOCX 44 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Das, S., Alcock, G., Azad, K. et al. Institutional delivery in public and private sectors in South Asia: a comparative analysis of prospective data from four demographic surveillance sites. BMC Pregnancy Childbirth 16, 273 (2016). https://doi.org/10.1186/s12884-016-1069-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-016-1069-7