Abstract
Background
Calcification is common in advanced atheromatous plaque, but its clinical significance remains unclear. This study aimed to assess the prevalence of plaque calcification in the moderate-to-severe internal carotid artery stenosis and investigate its relationship with ipsilateral ischemia.
Methods
The retrospective study included 178 patients detected with proximal internal carotid artery (pICA) stenosis of ≥ 50% on multidetector computed tomography at Zhejiang Hospital from January 2019 to March 2023. Association between plaque calcification characteristics (calcification thickness, position, type, circumferential extent, calcium volume and calcium score) and ipsilateral cerebrovascular events was analyzed.
Results
The 178 patients (mean age 71.24 ± 10.02 years, 79.78% males) had 224 stenosed pICAs overall. Plaque calcification was noted in 200/224 (89.29%) arteries. Calcification rates were higher in older age-groups. Calcification volume (r = 0.219, p < 0.001) and calcification score (r = 0.230, p < 0.001) were correlated with age. Ipsilateral ischemic events were significantly more common in the noncalcification group than in the calcification group (χ2 = 4.160, p = 0.041). The most common calcification type was positive rim sign calcification (87/200, 43.50%), followed by bulky calcification (66/200, 33.00%); both were significantly associated with ischemic events (χ2 = 10.448, p = 0.001 and χ2 = 4.552, p = 0.033, respectively). Calcification position, thickness, and circumferential extent, and calcification volume and score, were not associated with ischemic events. In multivariate analysis, positive rim signs (OR = 2.795, 95%CI 1.182–6.608, p = 0.019) was an independent predictor of ischemic events.
Conclusions
Plaque calcification in proximal internal carotid artery is common, and prevalence increases with age. Calcification characteristics could be predictive of ipsilateral ischemic events. The positive rim sign within plaque is a high-risk factor for a future ischemic event.
Similar content being viewed by others
Internal carotid artery (ICA) stenosis is being frequently encountered in clinical practice due to aging of the population and improvements in vascular imaging techniques. ICA stenosis is an advanced stage of atherosclerosis, with widely varying clinical presentations; some patients may be asymptomatic while others may present with transient ischemic symptoms or severe ischemic stroke [1]. According to the degree of stenosis, ICA stenosis is classified as mild (< 50%), moderate (50-69%), or severe (70-99%) [2, 3]. The proximal internal carotid artery (pICA), where there is marked alteration in blood flow velocity, is the region most prone to stenosis and plaque formation. The degree of stenosis is related to risk of ipsilateral ischemic stroke and an important consideration when deciding whether to opt for surgical or interventional treatment [4].
In addition to the degree of stenosis, morphology and composition of the plaque are also valuable imaging parameters. Specific plaque features, such as intraplaque hemorrhage, large lipid-necrotic core, and plaque ulceration are known risk factors for future ischemic stroke [5, 6], but these characteristics are not routinely assessed. Calcification in atherosclerotic plaque, which has long been recognized, is believed to result from the interaction of factors such as chronic inflammation, autophagy defects, endoplasmic reticulum stress, and mitochondrial dysfunction [7]. Calcification was once considered a passive degenerative process and a possible contributor to plaque stability [8]; however, the understanding of vascular calcification has changed in recent years. In the coronary arteries, calcification is associated with significant vessel stenosis and is an established predictor of future cardiac events and sudden death [9, 10]. However, the significance of calcification in the cerebral vasculature is still incompletely understood. Some authors have found that calcification is a protective factor [11], while others claim that it is associated with increased risk of stroke [12,13,14]. One study found that the presence and severity of intracranial artery calcification are linked to a higher risk of stroke, but that calcification might actually have a protective effect when stenosis already exists [15]. There is consensus, however, that plaque calcification changes blood dynamics by inducing arterial remodeling processes and increasing arterial stiffness and interface stresses [8, 16]. For the clinician, assessment of calcification can help in determining plaque stability and stroke risk and in making treatment decisions, especially regarding the need for aggressive interventions. Multidetector computed tomographic angiography (MDCTA) can provide valuable information on luminal stenosis and plaque characteristics [6].
The aim of this study was to assess the incidence of plaque calcification in patients with moderate-to-severe pICA stenosis and to investigate the relationship between calcification and ipsilateral ischemia.
Method
Study design and participants
This retrospective observational study was conducted at Zhejiang Hospital after obtaining approval from the Zhejiang hospital ethics committee (2023-40-K). The need for informed consent was waived because of the retrospective nature of the study .
All patients diagnosed with pICA stenosis on carotid MDCTA between January 2019 and March 2023 were identified. pICA was defined as the part of the internal carotid artery extending 2 cm from the bifurcation of the common carotid artery. The degree of stenosis was calculated by two experienced radiologists using North American Symptomatic Carotid Endarterectomy Trial (NASCET) criteria on contrast computed tomographic angiography (CTA) images [3]. Patients were excluded from the study if (1) they had mild (< 50%) stenosis (n = 4825) or suspicion of occlusion (n = 53); (2) there was history of previous endarterectomy or stenting treatment (n = 15); (3) there were other possible causes for stenosis such as dissection (n = 28), thrombosis (n = 6), moyamoya disease (n = 3), and fibromuscular dysplasia (n = 2); or 5) there was incomplete CT imaging data (n = 3) or clinical data (n = 11). For patients who had undergone repeat CTA examinations (n = 86), only the data at the earliest detection of pICA stenosis were included for analysis. A total of 178 patients (with 224 stenosed pICAs) met the eligibility criteria. Figure 1 shows the patient selection process. The majority of the participants were from outpatient or inpatient visits to our neurology department and were associated with cerebrovascular symptoms; while some patients were detected by CTA screening for nonspecific symptoms such as dizziness, headache, and cognitive impairment. There were also a small percentage of asymptomatic screened patients.
Data collection
Two neurologists retrieved the baseline demographic and clinical data of patients from the electronic medical records. Data were collected on demographics (age, sex); lifestyle factors (cigarette smoking, alcohol drinking); comorbidities (hypertension, diabetes, coronary artery disease, atrial fibrillation); current medications (antiplatelet drugs and statins); and laboratory test results (white blood cell count, C-reactive protein, blood sugar, triglyceride, low-density lipoprotein, high-density lipoprotein, serum creatinine, blood urea nitrogen, glomerular filtration rate (GFR), and alkaline phosphatase). Only test results obtained one week before or after carotid MDCTA were collected.
MDCT technique
MDCTA was performed using a NeuViz scanner (Neusoft Medical Systems, China) or a dual-source Somatom Force scanner (Siemens, Germany). Scanning was performed from the aortic arch to the first cervical intervertebral disc. Established standard-of-care CTA protocols were followed. Multiplanar reformatted images were reviewed on a PACS workstation on CTA settings, with modifications made as required to depict CTA lumen markers and calcification. The images were evaluated by two senior radiologists.
Evaluation of calcification
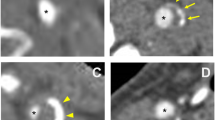
A standardized evaluation protocol was used for assessment of plaque calcification at the stenosis. Calcification was defined as a region with ≥ 1 contiguous pixels with CT attenuation ≥ 130 Hounsfield units in each image slice [17]. The calcification was graded according to location, circumferential extent, thickness, and type. According to location, the calcification was classified as inner (intimal), outer (near the adventitia), or mixed (both intimal and adventitial). According to circumferential extent, it was classified as single calcification (including spotty calcification) occupying < 90° of carotid wall circumference, occupying 90°-270° of carotid wall circumference, or occupying > 270° of carotid wall circumference [18]. Thickness of calcification in the plaque was measured on the largest longitudinal section of the plaque by using the centimeter scale accompanying the radiograph. Type of calcification was classified as superficial spotty calcification, bulky calcification, or rim calcification (Fig. 2). A superficial spotty calcification was defined as presence of calcification with diameter < 3 mm in the area adjacent to the vessel lumen with no visible gap to the lumen on any cross-sectional images, occupying only one side and extending < 90° of the artery circumference on cross-sectional images [17, 19]. Bulky calcification was defined as calcification measuring 2 mm in thickness. Positive rim calcification (positive rim sign) was defined as calcification measuring < 2 mm in thickness, with adjacent soft plaque measuring > 2 mm in thickness; conversely, negative rim sign was defined as calcification measuring < 2 mm in thickness, with adjacent soft plaque measuring < 2 mm in thickness [20].
Calcium volume and calcium burden was calculated on CTA using the Agatston scoring method [21]. Image data were transferred to a computer workstation (syngo.via; Siemens, Germany) for image postprocessing, and plaque calcification was quantified in noncontrast CT. A threshold of 130 Hounsfield units was used to identify calcification.
Patient grouping
Ischemic event was defined as a cerebral infarction or transient ischemic attack (TIA) on the ipsilateral side of the stenosis, with a time window of up to 3 months after symptom onset. The clinical information relies on clear medical history or confirmation by magnetic resonance imaging (MRI) or CT imaging. pICAs were classified into two groups: ischemia or nonischemia group based on the occurrence of ipsilateral ischemic episodes.
Statistical analysis
Statistical analysis was performed using SPSS 19 (IBM Corp., Armonk, NY, USA). Continuous variables were expressed as means ± standard deviation and compared using the Student’s t-test or the Mann-Whitney U test. Categorical variables were expressed as percentages and compared using the chi-squared test or the Fisher exact test. Correlation between calcification score and age was evaluated using Spearman rank correlation coefficient. Univariate and multivariate logistic regression analyses were used to identify the factors associated with the presence of calcification and ischemic event. Odds ratios (OR) and 95% confidence intervals (CI) were calculated. Statistical significance was at p ≤ 0.05.
Results
Patients
There were a total of 224 stenosed pICAs among the 178 patients included in this study (132 patients had unilateral stenosis and 46 had bilateral stenosis). The 178 patients included 142 (79.78%) males and 36 (20.22%) females. The mean age of the patients was 71.24 ± 10.02 years (range, 37–91 years). Comorbidities included hypertension (141/178, 79.21%), diabetes (53/178, 29.77%), coronary artery disease (38/178, 21.35%), and atrial fibrillation (11/178, 6.18%). There were 47/178 (26.40%) current smokers and 46/178 (25.84%) current drinkers. While 40/178 (22.47%) patients were on statins, 47/178 (26.40%) were on antiplatelet drugs. A total of 91/178 (51.12%) patients were admitted due to ischemic cerebral events (78 with anterior circulation ischemic events and 13 with posterior circulation ischemic events). While 69/178 (38.76%) patients had ipsilateral ischemic events, including 2 /178(1.12%) had bilateral stenosis and cerebral infarctions. Table 1 shows the characteristics of the study population.
Among the 224 stenosed pICAs, there were 122 (54.46%) cases of moderate stenosis and 102 (45.53%) cases of severe stenosis. The left pICA was stenosed in 114/224 (50.89%) cases and the right pICA in 110/224 (49.11%) cases.
Presence of calcification and correlation with age
Calcification was identified in 200/224 (89.29%) stenosed pICAs. Mean age was significantly higher in patients with calcification than in patients without calcification (71.98 ± 9.05 years vs. 64.92 ± 12.29 years; z = 2.627, p = 0.009). Prevalence of calcification tended to increase with age; the calcification rates were 80.00% (20/25), 85.93% (55/64), 91.21% (83/91), and 95.45% (42/44), respectively, in the < 60-, 60-69-, 70-79-, and \(\:\ge\:\)80-year age-groups (Fig. 3). Calcification volume (r = 0.219, p < 0.001) and calcification score(r = 0.230, p < 0.001) were correlated with age (Fig. 4). GFR was significantly lower in the calcification group than in the noncalcification group (82.00 ± 22.50 mL/min/1.73 m2 vs. 92.45 ± 22.93 mL/min/1.73 m2; z = − 2.025, p = 0.043). Sex composition, comorbidities, and personal history were comparable between the two groups (Table 2).
In multivariable logistic regression analysis, only age was an independent predictor of calcification (OR = 1.065, 95% CI: 1.016–1.116, p = 0.008). GFR was not independently associated with presence of calcification (OR = 0.991, 95% CI: 0.970–1.012, p = 0.388).
Relationship between calcification and ipsilateral ischemia
Of the 178 patients, 66 (including two patients with bilateral stenosis) had anterior circulation stroke and 3 patients experienced TIA prior to MDCT examination. The incidence of ipsilateral ischemic events was significantly higher in the noncalcification group than in the calcification group (12/24 vs. 59/200; χ2 = 4.160, p = 0.041).
In the calcification group, ipsilateral ischemic symptoms occurred in 59/200 (29.50%) cases but not in 141/200 (70.50%) cases. There was no significant difference in clinical data between the ischemic and non-ischemic cases (showed in Supplement Table). The mean thickness of calcification was 1.74 ± 0.91 mm (range, 0.10–5.60 mm). Calcium volume (z = − 0.171, p = 0.864) and calcium score (z = − 0.256, p = 0.798) were not significantly different between patients with and without ischemic symptoms. Occurrence of ipsilateral ischemia was not significantly associated with calcification thickness (p = 0.119), calcification location (p = 0.077), or circumferential extent of calcification (p = 0.066).
The most common calcification type was positive rim sign calcification (87/200, 43.50%), followed by bulky calcification (66/200, 33.00%), negative rim sign calcification (38/200, 19.00%), and superficial spotty calcification (27/200, 13.50%). Positive rim sign was significantly associated with ipsilateral ischemia (χ2 = 10.448, p = 0.001), as also bulky calcification (χ2 = 4.552, p = 0.033). Table 3 shows the distribution of different factors in the ischemia and nonischemia groups.
In univariate analysis, the positive rim sign was a risk factor for ipsilateral ischemic event (OR = 2.762, 95% CI 1.477–5.165, p = 0.001) and bulky calcification (OR = 0.469, 95%CI 0.232–0.948, p = 0.035) were protective factors. In multivariate analysis, after adjustments for age, sex, and stenosis degree, positive rim sign remained an independent predictor of ipsilateral ischemic event (OR = 2.795, 95%CI 1.182–6.608, p = 0.019). Table 4 shows the results of univariate and multivariate analysis.
Discussion
This study found that plaque calcification is present in 89.29% of moderately to severely stenosed proximal internal carotid arteries. The high prevalence indicates the important role of calcification in process of atherosclerotic stenosis. The precise mechanisms of calcification in atherosclerosis remain uncertain, but it appears to be related to aging. In this study, the prevalence of calcification increased with age. Calcification volume and scores also tended to increase with age. Previously identified risk factors for arterial calcification include diabetes mellitus, hypertension, smoking, elevated plasma cholesterol, elevated triglycerides, low HDL cholesterol, and obesity [14]; these are also risk factors for arterial stenosis, which may be the reason why they were comparable between patients with and without ischemic symptoms in this study.
Literature reports on the association between calcification and ischemic events are inconsistent. According to some studies, calcified plaques are stable plaques and associated with fewer ipsilateral ischemic events [11, 22], especially if calcification accounts for more than 45% of the total plaque volume [23]. Other studies have found that plaque calcification has no clinical significance [20, 24]. Some authors have reported a double peak in the symptom rates with increase in calcium score [25]. The inconsistency between studies might be due to differences in study populations, the definition of calcification types, and the methods used to quantify calcification. In this study, we discovered that there was a lower probability of an ischemia event occurring in the presence of carotid calcification (29.50% vs. 50.00%). The characteristics of calcification, however, are more significant in our understanding.
In our opinion, the clinical impact of arterial calcification is mainly decided by four factors: presence of calcification, calcium burden, location of calcification, and calcification type. Calcification with the rim sign is the most common type of calcification seen in clinical practice [20]. According to the maximum soft plaque thickness, it is classified as positive rim sign (> 2 mm soft plaque thickness) and negative rim sign (< 2 mm soft plaque thickness). In the present study, positive rim sign calcification was the calcification type most strongly associated with symptomatic status, with 36 of 59 cases being associated with ipsilateral ischemia. This finding is consistent with previous studies [20, 26]. The high risk may be related to the presence of a relatively large lipid-necrotic core and intraplaque hemorrhage. Eisenmenger et al. reported that the CTA rim sign of adventitial calcification with internal soft plaque is highly predictive of intraplaque hemorrhage [26], which is a characteristic of high-risk unstable plaque. The positive rim sign possibly indicates positive remodeling of the carotid. Arterial remodeling is thought to reflect adaptation of the vessel wall to mechanical and hemodynamic stimuli. Arterial remodeling can be inward (negative) or outward (positive) and hypertrophic or eutrophic [27]. Positive arterial remodeling is thought to be related to presence of vulnerable carotid plaque and risk of ischemic stroke [27, 28], but the mechanisms remain unclear.
In this study, other common types of calcification such as bulky calcification and superficial spotty calcification were not associated with risk of ischemic events. Bulky calcification, also called late-stage “macrocalcification”, may be linked to the healing process after an inflammatory response; the presence of more differentiated smooth muscle cells and a more organized extracellular matrix probably confers plaque stability [29]. Nevertheless, bulky calcifications have been found to be associated with cerebral ischemic events resulting from downstream microemboli [30], and it may also increase the difficulty of interventional surgery. Meanwhile, microcalcification, also called spotty calcification, is likely to exist in lipid-rich plaques and to be associated with inflammatory processes and high-risk plaque characteristics such as plaque ulceration and intraplaque hemorrhage [29]. Spotty calcification detected on coronary CTA is reported to be an important risk factor in patients with acute coronary syndrome [31]. Zhang et al. found that spotty calcification was markedly more prevalent in patients with stroke than in controls, with a threshold of more than three spotty calcifications indicating increased risk of stroke [19]. However, Saba et al. did not find any relationship between spotty calcification and risk of stroke [20]. The present study also found no association between superficial spotty calcification and ischemic events; this may have been because of the different definition used for spotty calcifications and the failure to consider its location and numbers. A previous study has found that intimal or superficial spotty calcifications are more likely to be associated with stroke occurrence than adventitial spotty calcifications [32]. Calcification closer to the lumen may cause greater stiffness mismatch and higher stress concentration [29]. In this study, due to the small number of plaques with superficial spotty calcifications, a more detailed analysis was not conducted.
Some limitations of this study should be acknowledged. First, this was a retrospective study with a small sample based on medical records. No additional investigation was carried out to validate the cerebral ischemic events in the study. The diversity of TIA symptoms raises the possibility of diagnostic bias. It is required to further validate the predictive value of these parameters for future ischemic events. Second, there is a potential for selection biases. Patients without an ischemic event but undergoing CTA for other reasons may exhibit better socioeconomic status, a healthier lifestyle, and a more favorable lipid profile compared to patients with symptomatic ischemic events. In order to ascertain the differences between the two groups, we conducted difference information regarding medication use and vascular-related disorders. However, there were still potentially ignored differences. Third, although statistical significance was discovered in multivariate regression, we did not further investigate the role of gender risk in the occurrence of ischemia events due to the limited sample size and gender imbalance. Additional research may be required. Fourth, the degree of ICA stenosis was established using NASCET criteria; these criteria are not applicable when there is collapse of the distal lumen, as is seen in severe stenosis [33]. The results may have also been impacted by the use of two different models of MDCT scanners. Fifth, we did not analyze the effect of other components within the plaque, vascular remodeling and collateral circulation status, which may affect the occurrence of ischemic events.
Conclusions
Calcification is common in stenosed proximal internal carotid arteries, with calcification prevalence increasing with age. Calcification characteristics may have more clinical significance than the presence of calcification. Plaque calcification with positive rim sign is a high-risk factor for ischemic events.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CTA:
-
Computed tomographic angiography
- CI:
-
Confidence intervals
- GFR:
-
Glomerular filtration rate
- HDL:
-
High-density lipoprotein
- ICA:
-
Internal carotid artery
- LDL:
-
Low-density lipoprotein
- MDCTA:
-
Multidetector computed tomographic angiography
- MRI:
-
Magnetic resonance imaging
- NASCET:
-
North American Symptomatic Carotid Endarterectomy Trial
- OR:
-
Odds ratios
- pICA:
-
Proximal internal carotid artery
- TIA:
-
Transient ischemic attack
References
Heck D, Jost A. Carotid stenosis, stroke, and carotid artery revascularization. Prog Cardiovasc Dis. 2021;65:49–54.
Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American symptomatic carotid endarterectomy trial collaborators. N Engl J Med. 1998;339(20):1415–25.
North American Symptomatic Carotid Endarterectomy Trial. Methods, patient characteristics, and progress. Stroke. 1991;22(6):711–20.
Bonati LH, Kakkos S, Berkefeld J, de Borst GJ, Bulbulia R, Halliday A, et al. European Stroke Organisation guideline on endarterectomy and stenting for carotid artery stenosis. Eur Stroke J. 2021;6(2):I.
Saba L, Saam T, Jager HR, Yuan C, Hatsukami TS, Saloner D, et al. Imaging biomarkers of vulnerable carotid plaques for stroke risk prediction and their potential clinical implications. Lancet Neurol. 2019;18(6):559–72.
Baradaran H, Gupta A. Extracranial Vascular Disease: carotid stenosis and plaque imaging. Neuroimaging Clin N Am. 2021;31(2):157–66.
Lee SJ, Lee IK, Jeon JH. Vascular calcification-new insights into its mechanism. Int J Mol Sci. 2020;21(8).
Jaminon A, Reesink K, Kroon A, Schurgers L. The role of vascular smooth muscle cells in arterial remodeling: focus on calcification-related processes. Int J Mol Sci. 2019;20(22).
Greenland P, Lloyd-Jones DM. Role of Coronary Artery Calcium Testing for Risk Assessment in Primary Prevention of Atherosclerotic Cardiovascular Disease: a review. JAMA Cardiol. 2022;7(2):219–24.
Razavi AC, Uddin SMI, Dardari ZA, Berman DS, Budoff MJ, Miedema MD, et al. Coronary artery calcium for risk stratification of Sudden Cardiac Death: the coronary artery Calcium Consortium. JACC Cardiovasc Imaging. 2022;15(7):1259–70.
Baradaran H, Al-Dasuqi K, Knight-Greenfield A, Giambrone A, Delgado D, Ebani EJ, et al. Association between Carotid Plaque Features on CTA and cerebrovascular ischemia: a systematic review and Meta-analysis. AJNR Am J Neuroradiol. 2017;38(12):2321–6.
Nandalur KR, Baskurt E, Hagspiel KD, Finch M, Phillips CD, Bollampally SR, et al. Carotid artery calcification on CT may independently predict stroke risk. AJR Am J Roentgenol. 2006;186(2):547–52.
Hou D, Yang X, Wang Y, Huang S, Tang Y, Wu D. Carotid siphon calcification predicts the symptomatic progression in Branch Artery Disease with Intracranial Artery stenosis-brief report. Arterioscler Thromb Vasc Biol. 2022;42(8):1094–101.
Goluke NMS, de Brouwer EJM, de Jonghe A, Claus JJ, Staekenborg SS, Emmelot-Vonk MH, et al. Intracranial artery calcifications: risk factors and association with cardiovascular disease and cognitive function. J Neuroradiol. 2022;49(3):281–7.
Wang X, Chen X, Chen Z, Zhang M. Arterial calcification and its Association with Stroke: implication of risk, prognosis, treatment response, and Prevention. Front Cell Neurosci. 2022;16:845215.
Gijsen FJH, Vis B, Barrett HE, Zadpoor AA, Verhagen HJ, Bos D, et al. Morphometric and mechanical analyses of calcifications and fibrous plaque tissue in carotid arteries for Plaque Rupture Risk Assessment. IEEE Trans Biomed Eng. 2021;68(4):1429–38.
Choi E, Byun E, Kwon SU, Kim N, Suh CH, Kwon H, et al. Carotid plaque composition assessed by CT predicts subsequent Cardiovascular events among subjects with carotid stenosis. AJNR Am J Neuroradiol. 2021;42(12):2199–206.
Babiarz LS, Yousem DM, Bilker W, Wasserman BA. Middle cerebral artery infarction: relationship of cavernous carotid artery calcification. AJNR Am J Neuroradiol. 2005;26(6):1505–11.
Zhang F, Yang L, Gan L, Fan Z, Zhou B, Deng Z, et al. Spotty calcium on Cervicocerebral Computed Tomography Angiography associates with increased risk of ischemic stroke. Stroke. 2019;50(4):859–66.
Saba L, Chen H, Cau R, Rubeis GD, Zhu G, Pisu F, et al. Impact analysis of different CT configurations of carotid artery plaque calcifications on cerebrovascular events. AJNR Am J Neuroradiol. 2022;43(2):272–9.
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr., Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827–32.
Masztalewicz M, Rotter I, Nowacki P, Szydlowski L, Zukowski M, Gutowski P. The parameters of carotid plaques’ calcifications and clinical nature of the lesions in the context of revascularization treatment. The enlargement of calcifications is still the most important. Folia Neuropathol. 2019;57(1):63–71.
Nandalur KR, Hardie AD, Raghavan P, Schipper MJ, Baskurt E, Kramer CM. Composition of the stable carotid plaque: insights from a multidetector computed tomography study of plaque volume. Stroke. 2007;38(3):935–40.
Xu X, Hua Y, Liu B, Zhou F, Wang L, Hou W. Correlation between calcification characteristics of carotid atherosclerotic plaque and plaque vulnerability. Ther Clin Risk Manag. 2021;17:679–90.
Katano H, Mase M, Nishikawa Y, Yamada K. Calcified carotid plaques show double symptomatic peaks according to agatston calcium score. J Stroke Cerebrovasc Dis. 2015;24(6):1341–50.
Eisenmenger LB, Aldred BW, Kim SE, Stoddard GJ, de Havenon A, Treiman GS, et al. Prediction of Carotid Intraplaque Hemorrhage using Adventitial calcification and plaque thickness on CTA. AJNR Am J Neuroradiol. 2016;37(8):1496–503.
Kashiwazaki D, Kuwayama N, Akioka N, Noguchi K, Kuroda S. Carotid plaque with expansive arterial remodeling is a risk factor for ischemic complication following carotid artery stenting. Acta Neurochir (Wien). 2017;159(7):1299–304.
Chen Z, Li M, Li M, Zhao Y, Zhu Y. Expansive arterial remodeling of carotid arteries in symptomatic ischemic patients. J Interv Med. 2018;1(2):82–5.
Balmos IA, Horvath E, Brinzaniuc K, Muresan AV, Olah P, Molnar GB et al. Inflammation, Microcalcification, and increased expression of Osteopontin are histological hallmarks of Plaque vulnerability in patients with Advanced Carotid artery stenosis. Biomedicines. 2023;11(3).
Wu XH, Chen XY, Fan YH, Leung TW, Wong KS. High extent of intracranial carotid artery calcification is Associated with downstream Microemboli in Stroke patients. J Stroke Cerebrovasc Dis. 2017;26(2):442–7.
Williams MC, Moss AJ, Dweck M, Adamson PD, Alam S, Hunter A, et al. Coronary artery plaque characteristics Associated with adverse outcomes in the SCOT-HEART Study. J Am Coll Cardiol. 2019;73(3):291–301.
Yang J, Pan X, Zhang B, Yan Y, Huang Y, Woolf AK, et al. Superficial and multiple calcifications and ulceration associate with intraplaque hemorrhage in the carotid atherosclerotic plaque. Eur Radiol. 2018;28(12):4968–77.
Johansson E, Fox AJ. Near-occlusion is a common variant of carotid stenosis: study and systematic review. Can J Neurol Sci. 2022;49(1):55–61.
Acknowledgements
We would like to express our gratitude to all the participants in the study.
Funding
This work was supported by the Key Research and Development Project of Zhejiang Provincial Department of Science and Technology(NO.2021C03105), Special Support Program for High Level Talents of Zhejiang Province (NO.2022R52038), Medical Science and Technology Project of Zhejiang Province (NO.2022KY484 and NO.2022KY468).
Author information
Authors and Affiliations
Contributions
FF, XL, SW, and SX conceived and designed the study. FF and JM analyzed MDCTA images; SZ and YL evaluated and acquired clinical data; RZ completed statistical analysis, SX drafted the manuscript. XL and SW revised the report. All authors read and approved the final manuscript. SW and SX are the guarantors and attest that all listed authors meet authorship criteria.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
The informed consent was waived because of the retrospective nature of the study, and the study was approved by the Ethics committee of Zhejiang Hospital (2023-40-k). All methods were carried out in accordance with relevant guidelines and regulation under the ‘Ethics approval and consent to participate’.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fu, F., Liu, X., Zhang, R. et al. Prevalence and clinical implications of calcification in internal carotid artery stenosis: a retrospective study. BMC Neurol 24, 279 (2024). https://doi.org/10.1186/s12883-024-03788-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-024-03788-9