Abstract
Objective
To investigate the association between total sleep duration variability and stroke in the middle-aged and elderly population in China.
Methods
Data were collected from the 2011, 2013, 2015, and 2018 surveys of the China Health and Retirement Longitudinal Study (CHARLS). A total of 3485 participants, who had not experienced a stroke until 2015 and completed the follow-up in 2018, were enrolled to analyze the relationship between total sleep duration variability and new stroke. Total sleep duration was calculated by summing self-reported nocturnal sleep duration and daytime napping. The variability was determined by calculating the standard deviation (SD) of total sleep duration across the first three waves. A binary logistic regression model was utilized to analyze this association.
Results
Of the 3485 participants, 183 (5.25%) sustained a stroke event. A dose-response relationship was observed, indicating an increased stroke risk of 0.2 per unit (hours) increase in total sleep duration variability [OR (95% CI): 1.20 (1.01–1.42)]. Upon stratification by sex groups, this increased risk was significant only in men [OR (95% CI): 1.44 (1.12–1.83)].
Conclusion
Increased total sleep duration variability was associated with an increased risk of stroke in the middle-aged and elderly, independent of factors such as age, nocturnal sleep duration, napping habits, region of residence, hypertension, diabetes mellitus, dyslipidemia, BMI, smoking, drinking habits, and marital status. However, a more notable correlation was observed in males.
Similar content being viewed by others
Introduction
Early prevention of stroke—a clinical condition characterized by neurological deficits arising from disrupted cerebral blood flow [1],—is crucial, given its status as the second leading cause of death and the third leading cause of disability in adults globally [2]. Stroke causes are diverse, encompassing hypertension, diabetes, obesity, advanced age, smoking, and dyslipidemia. However, these traditional risk factors do not account for all stroke occurrences [3,4,5,6,7]. Recent research increasingly highlights the impact of sleep disturbances on stroke development [8,9,10,11].
Sleep, a vital physiological activity, is crucial for maintaining physical and mental health. Numerous studies have explored the correlation between sleep duration and stroke risk, suggesting non-linear [12], J-shaped [13], or U-shaped relationships [14]. Collectively, our study’s findings suggest that both excessive and insufficient sleep increase stroke risk [12,13,14,15].
In addition to sleep duration, sleep variability is an important indicator of sleep health [16]. Sleep variability refers to the regularity of sleep/wake patterns [17]. Excessive sleep variability can disrupt internal circadian rhythms, adversely affecting metabolism [18]. Research indicates that sleep variability is linked to elevated risks of obesity, dyslipidemia, hyperglycemia, hypertension, and metabolic syndrome [19].
However, the association between sleep duration variability and stroke remains underexplored [20]. This study aims to examine the link between total sleep duration variability and new stroke incidents, including sex-specific differences, in a middle-aged and elderly Chinese cohort (China Health and Retirement Longitudinal Study[CHARLS]).
Methods
Study population
CHARLS, a prospective, nationally representative, and population-based study, focuses on the economic, social, and health status of adults aged 45 and above. Commenced in 2011 with 17,596 randomly selected participants, the study has examined data on general health status, lifestyle habits, and demographic characteristics at two-year intervals. To date, four waves of data are available. The protocol received approval from the Ethical Review Committee of Peking University (approval numbers: IRB00001052-11015 for the main household survey and IRB00001052-11014 for biomarker collection). All participants signed the informed consent and repository consent that permitted their data to be shared after a detailed presentation of the risks and benefits related to study participation.
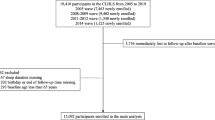
For this study, we excluded individuals with incomplete responses in the first three rounds of the sleep questionnaire (Supplementary material). Additionally, we excluded subjects who reported a stroke episode in the 2011, 2013, and 2015 surveys, and those with missing information in the 2018 stroke questionnaire (Supplementary material). We also excluded individuals missing complete information from the 2011 baseline. Ultimately, we analyzed a sample of 3,485 participants to investigate the association between total sleep duration variability and new stroke incidence. Further details about the enrollment process are provided in Fig. 1.
Assessment of total sleep duration variability
The total sleep duration over 24 h for each participant was calculated by adding the nocturnal sleep duration and daytime napping together [21]. Nocturnal sleep duration was obtained through the question: “In the previous month, how many hours of actual sleep did you get each night?” Meanwhile, daytime napping was assessed with: “In the previous month, how long did you nap for after lunch?“. For each participant, the standard deviation of total sleep duration was calculated using the total sleep time data from 2011, 2013, and 2015, representing the variability in total sleep duration.
Assessment of stroke
Stroke was the primary outcome of this study. Stroke incidence was assessed through self-reporting with the question: “Has a physician previously informed you that you have had a stroke?” An affirmative response was deemed indicative of a stroke occurrence. The primary outcome of interest was the occurrence of the first stroke event following the 2015 survey.
Assessment of covariates
The selection of covariates was guided by previous studies [11]. The selected socio-demographic characteristics included age, gender (male/female), educational attainment (primary and below/junior to secondary/undergraduate and above), marital status (married/unmarried), and residency (rural/urban). The categories “Married with spouse present” and “Married but not living with spouse” were classified as married, while “Separated”, “Divorced”, “Widowed”, and “Never married” were classified as unmarried. Lifestyle behaviors included smoking status (never/ever), alcohol consumption status (never/ever), and physical activity level (light/moderate/vigorous). Smoking status was categorized as “Never smoked” and “Ever smoked”, and alcohol consumption as “Never drunk” and “Ever drunk”. Clinical indicators included self-reported diagnoses of hypertension, diabetes mellitus, dyslipidemia, and body mass index (BMI). Nocturnal sleep duration and daytime napping at baseline were also considered to control for covariates.
Statistical analyses
Continuous variables were presented as the mean (SD) and compared using t-tests, while categorical variables were presented as counts and proportions and compared using Chi-square tests. Multivariable logistic regression analysis was used to examine the longitudinal correlation between total sleep duration variability and the incidence of new strokes. The multicollinearity of covariates (age, gender, educational attainment, marital status, residence, physical activity, smoking status, drinking status, hypertension, diabetes, BMI, dyslipidemia, nocturnal sleep duration, and daytime napping) was checked using the Variance Inflation Factor (VIF). A potential non-linear association between total sleep duration variability and stroke onset was examined using restricted cubic spline regression. In addition, subgroup and interaction analyses were performed. Statistical analyses were performed with R software, version 4.2.2 (http://www.R-project.org/). A two-sided P-value of < 0.05 was considered statistically significant.
Results
Baseline characteristics of study participants
During a 3-year follow-up period, 183 (5.25%) of 3485 participants without prior stroke history in 2015 developed a stroke. Statistically significant differences in age, marital status, and history of dyslipidemia, hypertension, and diabetes mellitus were observed, as depicted in Table 1. Compared with participants without a stroke, those with a stroke were more likely to be older (60.1 vs. 57.1), unmarried (14.8% vs. 9.0%), have diabetes (12.0% vs. 4.8%), have hypertension (44.3% vs. 21.1%), or have dyslipidemia (16.9% vs. 8.5%).
Compared to women, men were more likely to be older, married, highly educated, and have a history of smoking or drinking, with longer daytime napping and nocturnal sleep durations, as depicted in Table 2. However, they were less likely to have diabetes, hypertension, or dyslipidemia.
Total sleep duration variability & new stroke
Crude and adjusted logistic regression models were performed, yielding comparable results. After controlling for covariates (as listed in Table 3), a higher variability in total sleep duration was associated with an increased stroke risk. In the restricted cubic spline regression models, a linear correlation between total sleep duration variability and the risk of incident stroke was demonstrated in Fig. 2 (p = 0.413). Specifically, subjects with greater variability in total sleep duration exhibited a higher risk of stroke.
Females showed no significant association between total sleep duration variability and stroke risk (Table 4). However, in males, a significant association was noted, with increased total sleep duration variability linked to a higher risk of new stroke (OR = 1.43, 95% CI: 1.12–1.83).
Subgroup analyses indicated a stronger association between increased total sleep duration variability and stroke incidence in individuals who were older (age ≥ 60 years), male, were married, slept for 6–9 h per day, napped for more than 60 min per day, had dyslipidemia, and had a history of smoking or alcohol consumption (see Fig. 3). This association was particularly pronounced in males who were older (age ≥ 60 years), did not engage in daytime napping, had no history of hypertension or diabetes, and had a history of smoking or alcohol consumption (refer to Fig. 4). Nevertheless, no similar association was found in women (see Fig. 5).
Furthermore, an interaction was observed between total sleep duration variability and gender. Men demonstrated higher susceptibility to stroke with increased total sleep duration variability compared to women (as shown in Fig. 6).
Restricted cubic spline diagram illustrating the association between total sleep duration variability and incidence of new stroke, adjusted for gender, age, education, marital status, residence, smoking and drinking status, BMI, physical activity level, and history of hypertension, dyslipidemia, diabetes, nocturnal sleep duration, and napping duration at baseline. (Tsleep_sd: Total Sleep Duration Variability)
Sensitivity analysis
Similar results were obtained from sensitivity analyses, which excluded individuals who had used sedative-hypnotics during the initial three waves, as shown in Table 5. The association between sleep duration variability (assessed by the coefficient of variation of total sleep duration or the standard deviation of nocturnal sleep duration) and the risk of stroke in men persisted, as shown in Table 6.
Discussion
In this prospective cohort study, we found that among middle-aged and elderly individuals, increasing variability in total sleep duration over 4 years was significantly associated with an increased risk of new stroke. Additionally, a linear, positive correlation between total sleep duration variability and stroke risk was observed. This correlation was especially relevant in individuals over 60 years of age, males, those with a BMI > 28, married individuals, and those with a history of smoking or alcohol use.
More research has focused on the correlation between sleep duration at a single point in time and stroke risk, but research on the impact of prolonged changes in sleep duration on stroke risk is limited [15, 22, 23]. Findings from the Kailuan study, a prospective cohort study in a Chinese adult population, suggested that both stable low and increasing low sleep duration trajectories might be associated with a higher risk of subsequent first cardiovascular events, including atrial fibrillation, myocardial infarction, and stroke [15]. In the Tongji Dongfeng cohort study, individuals who consistently slept for ≥ 9 h per night or increased their sleep duration from 7 to 9 h to ≥ 9 h had a higher risk of stroke compared to those who consistently slept for 7–9 h per night. A previous study of a British population revealed that individuals who consistently slept for extended periods (> 8 h) or had a significant increase in sleep duration (from less than 6 h to > 8 h) were at least twice as likely to experience stroke compared to those who consistently slept for 6–8 h [23]. Previous research focused on the qualitative categorization of long-term variations in sleep duration, assessing the relationship between variously classified long-term sleep patterns and stroke risk. However, these studies did not establish a dose-response relationship between quantitatively measured changes in sleep duration and stroke risk. Therefore, our study employed the calculation of intra-individual standard deviation (SD) from three measurements of total sleep time over four years to provide a quantitative assessment of the long-term changes in total sleep duration for each participant.
To the best of our knowledge, this study is the first to investigate the association between sleep duration variability and stroke incidence. Previous research has primarily focused on the relationship between sleep variability and cardiovascular disease, along with its associated risk factors [24]. Findings indicate a correlation between total sleep duration variability and BMII [24], obesity/overweight [25], glycated hemoglobin26, hypertension [17, 26], cardiovascular disease [27], and metabolic syndrome [28]. Regarding our findings that increased total sleep duration variability might elevate stroke incidence, we hypothesize the following contributing mechanisms. First, inconsistent sleep patterns increase the likelihood of risk factors associated with cardiovascular disease [18], such as dyslipidemia, high blood pressure, and elevated blood glucose levels, potentially leading to stroke onset [29, 30]. Second, irregular sleep patterns may affect melatonin production. Melatonin plays a crucial role as an antioxidant and neuroprotectant within the body [31]. Experimental studies have demonstrated melatonin’s role in preventing the onset and progression of stroke [32, 33]. Third, sleep rhythm disorders may be linked to specific genetic abnormalities. Several circadian genes, such as clock, per2, and bmal1, regulate a broad spectrum of cardiovascular rhythms and processes, including blood pressure, endothelial function, and thrombosis [34,35,36,37]. There is a significant correlation between circadian genes and enzymes that regulate reactive oxygen species (ROS) [38]. Experimental studies indicated that the deficiency of the Per2 gene heightened susceptibility to ROS [39], and the downregulation of the Bmal1 gene disrupted redox defenses, leading to increased oxidative damage [40]. Fourth, irregular sleep disrupts the autonomic nervous system’s rhythm, thus affecting cardiovascular function [41, 42]. The autonomic nervous system is responsible for regulating the body’s stress response to a wide range of stressors, including acute and chronic risk factors for stroke, mitigating the effects of these stressors and restoring homeostasis [43, 44]. However, impaired function of the autonomic nervous system can disrupt the stress response and contribute to the onset of stroke [43]. Finally, irregular sleep patterns represent a mismatch between daily lifestyle activities, such as eating and exercising, and the body’s natural circadian rhythm. This can result in metabolic changes that are linked to obesity, ultimately increasing the occurrence of stroke [45,46,47].
In this study, a significant association between total sleep time variability and stroke was not observed in women. Previous studies have shown that men have a higher lifetime risk of ischemic stroke than women within most age strata [48]. Most of the women enrolled in the study were in either the perimenopausal or postmenopausal stage, characterized by low levels of estrogen. Studies indicate that estrogen hinders stroke progression through its anti-atherosclerotic effects on the vascular system and its modulation of adipogenesis. Additionally, estrogen reduces stroke damage by causing coronary artery vasodilation and providing neuroprotection to brain and glial cells during ischemia [49]. Thus, the lack of estrogen might play a significant role in the occurrence of stroke in women, and the relative importance of total sleep duration variability might be diminished.
This study is significant due to its longitudinal evaluation of changes in sleep duration over a 4-year period, its analysis of the quantitative and qualitative links between total sleep duration variability and stroke incidence, and its status as a prospective cohort study in a middle-aged and elderly population in China, offering more rational and credible findings from a broader societal sample. Furthermore, the study accounted for possible confounding factors and carried out thorough subgroup analyses, interaction analyses, and sensitivity analyses. However, it is important to acknowledge that this study has certain limitations. Firstly, participants’ self-reported information was used to evaluate sleep rather than an objective measure, possibly introducing error. a more objective and.
accurate measurement of sleep duration should be polysomnography (PSG) [50]. Secondly, participants’ self-reported their stroke diagnosis, based on the doctor’s judgment, which could be prone to bias. Thirdly, the study database did not evaluate details on other aspects of sleep, such as snoring, sleep apnea, and sleep quality. we could not obtain relevant data to assess sleep quality in CHARLS, which can be supplemented by follow-up studies. Finally, it should be noted that the findings of this study are relevant only to the Chinese population aged 45 or above and cannot be generalized to other populations.
Conclusion
In conclusion, this study reveals a dose-response relationship between the variability of total sleep duration and future stroke risk in the middle-aged and elderly Chinese population. This relationship is independent of age, nocturnal sleep duration, napping habits, area of residence, and a history of hypertension, diabetes mellitus, dyslipidemia, Body Mass Index (BMI), smoking status, alcohol consumption, and marital status. Stabilizing and minimizing fluctuations in sleep duration could play a role in preventing future stroke events. Particularly, it is crucial for men to focus on maintaining stable sleep patterns.
Data availability
The datasets analysed during the current study are available in the [CHARLS] repository, [https://charls.pku.edu.cn/]
References
Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(7):2064–89.
Collaborators GBDLRS, Feigin VL, Nguyen G, Cercy K, Johnson CO, Alam T, et al. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N Engl J Med. 2018;379(25):2429–37.
Ma Q, Li R, Wang L, Yin P, Wang Y, Yan C, et al. Temporal trend and attributable risk factors of stroke burden in China, 1990–2019: an analysis for the global burden of disease study 2019. Lancet Public Health. 2021;6(12):e897–906.
Phua CS, Jayaram L, Wijeratne T. Relationship between sleep duration and risk factors for stroke. Front Neurol. 2017;8:392.
David Spence J. Advances in stroke prevention. J Translational Intern Med. 2018;6(3):105–14.
Li J, Jiang S, Zhang Y, Tang G, Wang Y, Mao G, et al. H-type hypertension and risk of stroke in Chinese adults: a prospective, nested case-control study. J Translational Intern Med. 2015;3(4):171–8.
David Spence J. Dietary cholesterol and egg yolk should be avoided by patients at risk of vascular disease. J Translational Intern Med. 2016;4(1):20–4.
Petrov ME, Howard G, Grandner MA, Kleindorfer D, Molano JR, Howard VJ. Sleep duration and risk of incident stroke by age, sex, and race: the REGARDS study. Neurology. 2018;91(18):e1702–9.
Ge B, Guo X. Short and long sleep durations are both associated with increased risk of stroke: a meta-analysis of observational studies. Int J Stroke. 2015;10(2):177–84.
Helbig AK, Stöckl D, Heier M, Ladwig KH, Meisinger C. Symptoms of insomnia and sleep duration and their association with incident strokes: findings from the population-based MONICA/KORA Augsburg cohort study. PLoS ONE. 2015;10(7):e0134480.
Titova OE, Michaëlsson K, Larsson SC. Sleep duration and stroke: prospective cohort study and Mendelian randomization analysis. Stroke. 2020;51(11):3279–85.
Westerlund A, Bellocco R, Sundstrom J, Adami HO, Akerstedt T, Trolle Lagerros Y. Sleep characteristics and cardiovascular events in a large Swedish cohort. Eur J Epidemiol. 2013;28(6):463–73.
Li W, Wang D, Cao S, Yin X, Gong Y, Gan Y, et al. Sleep duration and risk of stroke events and stroke mortality: a systematic review and meta-analysis of prospective cohort studies. Int J Cardiol. 2016;223:870–6.
Ji A, Lou H, Lou P, Xu C, Zhang P, Qiao C, et al. Interactive effect of sleep duration and sleep quality on risk of stroke: an 8-year follow-up study in China. Sci Rep. 2020;10(1):8690.
Zhou L, Yu K, Yang L, Wang H, Xiao Y, Qiu G, et al. Sleep duration, midday napping, and sleep quality and incident stroke: the Dongfeng-Tongji cohort. Neurology. 2020;94(4):e345–56.
Buysse DJ. Sleep health: can we define it? Does it Matter? Sleep. 2014;37(1):9–17.
Lunsford-Avery JR, Engelhard MM, Navar AM, Kollins SH. Validation of the sleep regularity index in older adults and associations with cardiometabolic risk. Sci Rep. 2018;8(1):14158.
Chellappa SL, Vujovic N, Williams JS, Scheer F. Impact of circadian disruption on cardiovascular function and disease. Trends Endocrinol Metab. 2019;30(10):767–79.
Zhu B, Wang Y, Yuan J, Mu Y, Chen P, Srimoragot M, et al. Associations between sleep variability and cardiometabolic health: a systematic review. Sleep Med Rev. 2022;66:101688.
Brunetti V, Rollo E, Broccolini A, Frisullo G, Scala I, Della Marca G. Sleep and stroke: opening our eyes to current knowledge of a key relationship. Curr Neurol Neurosci Rep. 2022;22(11):767–79.
Li W, Taskin T, Gautam P, Gamber M, Sun W. Is there an association among sleep duration, nap, and stroke? Findings from the China health and retirement longitudinal study. Sleep Breath = Schlaf Atmung. 2021;25(1):315–23.
Wang YH, Wang J, Chen SH, Li JQ, Lu QD, Vitiello MV, et al. Association of longitudinal patterns of habitual sleep duration with risk of cardiovascular events and all-cause mortality. JAMA Netw Open. 2020;3(5):e205246.
Leng Y, Cappuccio FP, Wainwright NW, Surtees PG, Luben R, Brayne C, et al. Sleep duration and risk of fatal and nonfatal stroke: a prospective study and meta-analysis. Neurology. 2015;84(11):1072–9.
Patel SR, Hayes AL, Blackwell T, Evans DS, Ancoli-Israel S, Wing YK et al. The association between sleep patterns and obesity in older adults. International journal of obesity (2005). 2014;38(9):1159-64.
Häusler N, Marques-Vidal P, Haba-Rubio J, Heinzer R. Association between actigraphy-based sleep duration variability and cardiovascular risk factors - results of a population-based study. Sleep Med. 2020;66:286–90.
Brindle RC, Yu L, Buysse DJ, Hall MH. Empirical derivation of cutoff values for the sleep health metric and its relationship to cardiometabolic morbidity: results from the midlife in the United States (MIDUS) study. Sleep. 2019;42(9).
Huang T, Mariani S, Redline S. Sleep irregularity and risk of cardiovascular events: the multi-ethnic study of atherosclerosis. J Am Coll Cardiol. 2020;75(9):991–9.
Huang T, Redline S. Cross-sectional and prospective associations of actigraphy-assessed sleep regularity with metabolic abnormalities: the multi-ethnic study of atherosclerosis. Diabetes Care. 2019;42(8):1422–9.
Morris CJ, Purvis TE, Mistretta J, Hu K, Scheer F. Circadian misalignment increases C-reactive protein and blood pressure in chronic shift workers. J Biol Rhythms. 2017;32(2):154–64.
Morris CJ, Purvis TE, Hu K, Scheer FA. Circadian misalignment increases cardiovascular disease risk factors in humans. Proc Natl Acad Sci U S A. 2016;113(10):E1402–11.
O’Collins VE, Macleod MR, Cox SF, Van Raay L, Aleksoska E, Donnan GA, et al. Preclinical drug evaluation for combination therapy in acute stroke using systematic review, meta-analysis, and subsequent experimental testing. J Cereb Blood Flow Metab. 2011;31(3):962–75.
Pei Z, Pang SF, Cheung RT. Pretreatment with melatonin reduces volume of cerebral infarction in a rat middle cerebral artery occlusion stroke model. J Pineal Res. 2002;32(3):168–72.
Feng D, Wang B, Wang L, Abraham N, Tao K, Huang L et al. Pre-ischemia melatonin treatment alleviated acute neuronal injury after ischemic stroke by inhibiting endoplasmic reticulum stress-dependent autophagy via PERK and IRE1 signalings. J Pineal Res. 2017;62(3).
Viswambharan H, Carvas JM, Antic V, Marecic A, Jud C, Zaugg CE, et al. Mutation of the circadian clock gene Per2 alters vascular endothelial function. Circulation. 2007;115(16):2188–95.
Young ME, Brewer RA, Peliciari-Garcia RA, Collins HE, He L, Birky TL, et al. Cardiomyocyte-specific BMAL1 plays critical roles in metabolism, signaling, and maintenance of contractile function of the heart. J Biol Rhythms. 2014;29(4):257–76.
Anea CB, Zhang M, Stepp DW, Simkins GB, Reed G, Fulton DJ, et al. Vascular disease in mice with a dysfunctional circadian clock. Circulation. 2009;119(11):1510–7.
Curtis AM, Seo SB, Westgate EJ, Rudic RD, Smyth EM, Chakravarti D, et al. Histone acetyltransferase-dependent chromatin remodeling and the vascular clock. J Biol Chem. 2004;279(8):7091–7.
Putker M, O’Neill JS. Reciprocal control of the circadian clock and cellular redox state - a critical appraisal. Mol Cells. 2016;39(1):6–19.
Magnone MC, Langmesser S, Bezdek AC, Tallone T, Rusconi S, Albrecht U. The mammalian circadian clock gene per2 modulates cell death in response to oxidative stress. Front Neurol. 2014;5:289.
Musiek ES, Lim MM, Yang G, Bauer AQ, Qi L, Lee Y, et al. Circadian clock proteins regulate neuronal redox homeostasis and neurodegeneration. J Clin Invest. 2013;123(12):5389–400.
Burgess HJ, Trinder J, Kim Y, Luke D. Sleep and circadian influences on cardiac autonomic nervous system activity. Am J Physiol. 1997;273(4):H1761–8.
Huang T, Poole EM, Vetter C, Rexrode KM, Kubzansky LD, Schernhammer E, et al. Habitual sleep quality and diurnal rhythms of salivary cortisol and dehydroepiandrosterone in postmenopausal women. Psychoneuroendocrinology. 2017;84:172–80.
Koolhaas JM, Bartolomucci A, Buwalda B, de Boer SF, Flugge G, Korte SM, et al. Stress revisited: a critical evaluation of the stress concept. Neurosci Biobehav Rev. 2011;35(5):1291–301.
Ulrich-Lai YM, Herman JP. Neural regulation of endocrine and autonomic stress responses. Nat Rev Neurosci. 2009;10(6):397–409.
Arble DM, Bass J, Laposky AD, Vitaterna MH, Turek FW. Circadian timing of food intake contributes to weight gain. Obes (Silver Spring). 2009;17(11):2100–2.
Garaulet M, Gomez-Abellan P, Alburquerque-Bejar JJ, Lee YC, Ordovas JM, Scheer FA. Timing of food intake predicts weight loss effectiveness. International journal of obesity (2005). 2013;37(4):604–11.
Rong S, Snetselaar LG, Xu G, Sun Y, Liu B, Wallace RB, et al. Association of skipping breakfast with cardiovascular and all-cause mortality. J Am Coll Cardiol. 2019;73(16):2025–32.
Seshadri S, Wolf PA. Lifetime risk of stroke and dementia: current concepts, and estimates from the Framingham study. Lancet Neurol. 2007;6(12):1106–14.
Suzuki S, Brown CM, Wise PM. Mechanisms of neuroprotection by estrogen. Endocrine. 2006;29(2):209–15.
Rundo JV, Downey R. 3rd. Polysomnography. Handbook of clinical neurology. 2019;160:381–92.
Acknowledgements
Also, special thanks to all members of the CHARLS research team, all fieldworkers, and every interviewee.
Funding
This work was supported by grants from the National Natural Science Foundation of China (No. 82101537 and 82071206), Shanghai Science and Technology Commission (No. 22Y31900204), Shanghai Health Commission (No. 20234Y001), Science and Technology Commission of Chongming District (No.CKY2023-40), and China Postdoctoral Science Foundation (2023M732659).
Author information
Authors and Affiliations
Contributions
Jiangping Ma: Study design, data collection and, Formal analysis, Visualization, Writing an original draft. Nuo Ma: Study design, Writing e review & editing. Lu Zhang: Study design, data collection and, Visualization. Linghao Xu: Study design, data collection and, Visualization. Xueyuan Liu: Supervision, Project administration, Writing e review & editing, All authors read and approved the final manuscript. Guilin Meng: Supervision, Project administration, Writing e review & editing, All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The protocol received approval from the Ethical Review Committee of Peking University (approval numbers: IRB00001052-11015 for the main household survey and IRB00001052-11014 for biomarker collection). All participants signed the informed consent and repository consent that permitted their data to be shared after a detailed presentation of the risks and benefits related to study participation. The protocol was in accordance with the Declaration of Helsinki.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ma, J., Ma, N., Zhang, L. et al. Association of total sleep duration variability with risk of new stroke in the middle-aged and elderly Chinese population. BMC Neurol 24, 217 (2024). https://doi.org/10.1186/s12883-024-03727-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-024-03727-8