Abstract
Background
Postural abnormalities (PA) are common in the advanced stages of Parkinson’s disease (PD), but effective therapies are lacking. A few studies suggested that spinal cord stimulation (SCS) could be a potential therapy whereas its effect is still uncertain. We aimed to investigate whether SCS had potential for benefiting PD patients with PA.
Methods
T8-12 SCS was operated on six PD patients with PA and all patients were followed for one year. Evaluations were made before and after SCS. Moreover, three patients were tested separately with SCS on-state and off-state to confirm the efficacy of SCS.
Results
Improvements in lateral trunk flexion degree, anterior thoracolumbar flexion degree and motor function were found after SCS. The improvements diminished while SCS was turned off.
Conclusions
Lower thoracic SCS may be effective for improving PA in PD patients, but further studies are needed to confirm this conclusion.
Trial registration
Chinese Clinical Trial Registry, ChiCTR1900024326, Registered on 6th July 2019; https://www.chictr.org.cn/showproj.aspx?proj=40835.
Similar content being viewed by others
Background
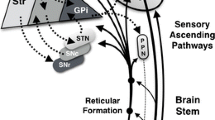
Parkinson’s disease (PD) is a common neurodegenerative disorder in which the main cause is basal ganglia dysfunction, resulting from degeneration of neurons in the dopaminergic nigrostriatal pathway [1]. Dopaminergic medication can usually ameliorate the patient’s symptoms in the early stages of PD, but its efficacy decreases with the disease progressing and is prone to some long-term motor side-effects. When the disease progresses to the advanced stage, patients develop specific symptoms which tend to be less responsive to dopaminergic therapy, such as axial symptoms [2]. And medications cannot maintain long-term efficacy [3]. So, exploring effective treatments for axial symptoms in PD is in utmost need and has been a hot topic in current PD clinical research.
Lately, some studies have explored the application of SCS in PD [4,5,6,7,8,9]. A case report found an antiparkinsonian effect of SCS in a patient implanted for lower limb neuropathic pain [9], and some studies reported SCS might benefit advanced PD patients’ motor and gait function [5, 7, 8]. However, a prospective trial had reported no clinically meaningful effect of SCS for PD [6]. Therefore, some valuable insights were provided, but the effect of SCS was still uncertain. A previous study of our team reported that PD patients with postural abnormalities (PA) featured a significant severity in motor dysfunction, decreased pelvic obliquity angle, and more doses of dopaminergic medications needed [10]. According to previous studies of SCS, we considered that SCS might be a supplementary therapy for these patients.
In the present study, we performed SCS surgery on spinal segments T8–12 of six PD patients with PA. All six patients completed evaluations and were followed for one year. Furthermore, three of them were tested separately with SCS on-state and off-state to confirm the efficacy of SCS. The aim of this study is to explore the application of SCS in treating PD patients with PA.
Methods
Patients
We performed the study at Ruijin Hospital, Shanghai Jiao Tong University School of Medicine from June 2019 to December 2021. This study was approved by the ethics committee of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine (2019-62), and registered at Chinese Clinical Trial Registry (ChiCTR1900024326). The protocol of the current study fitted the guidelines of the Declaration of Helsinki and its later amendments. Written informed consents were obtained from participants. Our study adhered to CONSORT guidelines.
PD patients actively seeking surgical treatment for postural disorders were recruited. PD was diagnosed according to the diagnostic criteria of the Movement Disorders Society (MDS) [11] by two experienced movement disorder specialists and patients were evaluated with the Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) [12] and the Hoehn-Yahr stage [13]. All participants met the following criteria: (a) age between 45 and 75 years, (b) no sign of dementia according to the Chinese version of the Mini-Mental State Examination (cMMSE) [14], (c) Hoehn-Yahr stage > 2, (d) PD patients with MDS-UPDRS Q 3.13-Posture scale > = 2 were recruited, and these patients’ postural abnormalities were minimally improved by levodopa in the “on” state, (e) no psychiatric disorders, (f) no history of other disorders involving the nervous system and musculoskeletal system, or of intracranial surgery or traumatic brain injury, (g) the reversibility during lying position had been verified in the patient. Patients were excluded at the baseline if they were unable to walk at least 5 m continuously without any assistance. The sagittal angle between a vertical line and a line connecting the trochanter with the edge of the acromion was evaluated to define anterior thoracolumbar flexion, and the coronal angle between a vertical line and a line passing through the C7 and L4 vertebrae was used to define lateral trunk flexion [15,16,17] (Fig. 1). We used web-based tools to measure the angles of lateral trunk flexion and anterior thoracolumbar flexion (http://www.neurologie.unikiel.de/de/axial-posturale-stoerungen/camptoapp) according to the recommendation of the consensus [18, 19].
Evaluations were made before the SCS surgery and 3, 6, 12 months after the SCS surgery. Three of all six patients were evaluated separately with SCS in the on- and off-states during follow-up (6 or 12 months). Evaluations of SCS off-state were made with the SCS system turned off for at least 24 h. Examiners were blinded during the on/off comparison. The patients were also evaluated using the Scale for Outcomes in PD-Autonomic (SCOPA-AUT) [20], 39-item quality of life questionnaire for Parkinson’s disease (PDQ-39) [21] and Wexner constipation score (WCS) [22].
SCS procedure
Two cylindrical percutaneous electrodes with eight contacts per lead (Model 3777, Medtronic) were implanted in the medial epidural space at spinal segments T8–12 under local anesthesia, with the electrode positioned to produce paresthesia fully covering the lower trunk and lower extremities including both legs and feet.
On the second day after lead implantation, the lead contacts were activated with an external stimulator, stimulating at 40–60 Hz to produce paresthesia covering the lower trunk and lower extremities. If the clinical response (A sign of postural improvement presented and no unwanted effects occurred) in the test phase (less than 4 weeks) was satisfactory, patients underwent second-stage surgery to implant a paddle lead with three columns of contacts (5–6–5 Model 39,565; Medtronic) into the epidural space of the thoracic spine (T8–T12) by partial laminectomy, under X -ray magnification. The lead was then connected with the pulse generator (Model 37,714, Medtronic) in the subcutaneous pocket at the abdomen.
One month after the surgical lead implantation, positional adaptation function was applied. Paresthesia was only clearly sensed when the patients were sitting or walking and was nearly imperceptible when they were lying down.
Statistical analysis
Statistical analysis was performed using SPSS V.22.0. The clinical data were used to calculate the mean and rate of change at each follow-up time. We analyzed measures of participants using paired Wilcoxon’s test depending on the type and distribution of dependent variables. P < 0.05 was considered statistically significant for all analyses. All tests were two-tailed.
Results
The demographic and clinical characteristics of all participants are shown in Table 1. The assessments were recorded on patients’ “medication-on” status after regular medications with SCS on-state. Evaluations made before the SCS surgery are shown in Table 2. During the one-year follow-up, no extra antiparkinsonian drugs were needed in all participants. There were significant differences in the degree of lateral trunk flexion (p < 0.027) and anterior thoracolumbar flexion (p < 0.028) before SCS surgery and at the one-year follow-up. There was no significant difference in the MDS-UPDRS III score (p > 0.05) before SCS surgery and at the one-year follow-up. After SCS, the mean lateral trunk flexion degree was improved by 58%, mean anterior thoracolumbar flexion degree was improved by 32% and the mean MDS-UPDRS-III score was improved by 9% (Table 1; Fig. 2). Scores of specific items in MDS-UPDRS III for patients before SCS surgery and at the one-year follow-up were presented in Supplementary Table 1. In majority of patients, the scores of MDS-UPDRS Q 3.3 (d/e) – Rigidity (Right Lower Extreme/Left Lower Extremity), MDS-UPDRS Q3.4 - Finger tapping and MDS-UPDRS Q 3.7 - Toe tapping are lower at the one-year follow-up. In all, the motor function of lower extremities was improved in most patients. Settings for SCS of each patient are shown in Fig. 3.
Three of the six patients were tested separately with SCS on-state and off-state to confirm the efficacy of SCS. All tests were performed at “medication-on” status. The results are shown in Table 3. Specific items of MDS-UPDRS III scores are presented in the Supplementary Table 2. The MDS-UPDRS III scores of all three patients were lower in the SCS on-state compared to the SCS off-state. The sagittal and coronal angles of Patient 1 and 2 improved in the SCS on-state compared to the SCS off-state. The sagittal angle of Patient 3 also improved in the SCS on-state compared to the SCS off-state. No significant improvement was observed in these patients in MDS-UPDRS part one or two, SCOPA-AUT, PDQ-39 or WCS (p > 0.05) (Table 4).
No adverse events were reported.
Discussion
To the best of our knowledge, there has been no study about SCS application with on- and off-states in PD patients with PA. In the present study, we performed SCS surgery on the lower thoracic spinal segments of six PD patients with PA. Patients completed evaluations and were followed for 12 months, and three of them were tested separately with SCS on-state and off-state. We found that SCS improved lateral trunk flexion degree and anterior thoracolumbar flexion degree, and controlled motor symptoms without increasing the intake of anti-parkinsonism medication.
The mechanism of how SCS works on posture is not very clear. SCS may differently affect two mechanisms of postural control – reactive and anticipatory. Also SCS seems to influence cortical motor circuits involving the supplementary motor area rather than neuronal circuitries involving the brainstem and spinal cord [23]. Simultaneously, our previous study has found decreased structure/functional connectivity between the supplementary motor area and insula in PD patients with PA compared with PD patients without PA [10]. And some studies found that there was modulation of activity in primary and secondary somatosensory cortices and insula during SCS [24, 25]. Therefore, supplementary motor area and insula could play important roles in mechanism of SCS improving PA in PD.
The application of SCS to PD motor symptoms has been studied with great interest for its potential value in treating motor symptoms and gait disturbance in PD. However, previous SCS trials showed contradictory results. Some clinical trials reported negative outcomes of cervical or thoracic SCS for treating PD [6, 26], while some other studies reported that thoracic SCS resulted in significant improvements in motor symptoms and gait dysfunction [5, 7, 8, 27]. The contradiction may be explained by the variety of inclusion criteria, stimulating sites and parameters, hardware and observing outcomes. We used similar protocols and settings of SCS as previous studies [5, 28]. In our study, according to sub-scores of MDS-UPDRS III, the motor function of lower extremities was improved in most patients. This finding was consistent with some previous studies [9, 24]. Some evidence indicated that therapeutic effect of SCS might be associated with spinal segment of stimulation, though no certain pattern was found [29, 30]. In the longitudinal follow-up and comparison of SCS on/off-state, we objectively recorded a positive clinical response in postural measurements. Notably, after SCS surgery, patients’ motor function was maintained without increasing the intake of anti-parkinsonism medication, though a fluctuation in the effects of SCS on motor symptoms was observed during the one-year follow-up. Our results indicated that lower thoracic SCS had potential for treating advanced PD patients with PA. Further studies with larger sample sizes and a double-blind design are needed to warrant this conclusion.
In this study, all patients were designed to subjected to a test phase less than four weeks prior to the formal implantation of the SCS electrodes. This phase allowed both the clinicians and the patients themselves to evaluate the clinical efficacy of SCS and the patient’s tolerance to SCS stimulation. A total of seven patients were included in this trial, one of whom withdrew from the study due to unsatisfactory clinical improvements during the test phase. The remaining six patients all experienced varying degrees of clinical improvement during the test phase. These improvements included a reduction in trunk posture inclination, relief of trunk and limb rigidity, or an increase in walking speed. However, in this study, some of the clinical improvements observed during the test phase were not sustained long-term post-SCS surgery. No adverse reactions were reported by any of the patients. The short-term and long-term effects of SCS on patients with PD constitute a highly valuable research topic. Clinical trials with a large number of participants are needed.
Though SCS improved lateral trunk flexion degree and anterior thoracolumbar flexion degree in the present study, no significant improvements were observed in terms of MDS-UPDRS II (Mean ± SD, pre-surgery vs. post-surgery: 15 ± 8 vs. 16 ± 3), which was consistent with a previous study [6]. Though we found some improvements in MDS-UPDRS Q 2.9 - Turning in bed, Q 2.11 - Getting out of bed, Q 2.12 - Walking and balance and Q 2.13 – Freezing in two patients, the total score of MDS-UPDRS II was not reduced in each patient. In addition, some previous studies reported that SCS may positively impact PDQ-39 scores [11, 27]. However, in our study, while a trend towards improvement was noted, no significant improvement was found in terms of PDQ-39 (Mean ± SD, pre-surgery vs. post-surgery: 41 ± 25 vs. 36 ± 21), which was consistent with a previous study [6]. One reason of no significant improvement in MDS-UPDRS II and PDQ-39 may be the small sample size of recruited patients. Simultaneously, the progression and heterogeneity of disease may be the other reasons. Besides, the improvement of clinical measurements is not always paralleled with health status and disease progression. Autonomic dysfunction is common in PD patients and some studies [31,32,33] have suggested that SCS could improve cardiac autonomic function, temperature regulation and constipation. Therefore, we tried to explore whether SCS could alleviate autonomic function in PD patients, which Scale for Outcomes in PD-Autonomic (SCOPA-AUT) and Wexner constipation score (WCS) before and after SCS in three recruited PD patients were observed. However, no significant improvements were observed.
Our study has some limitations. Firstly, the small sample size limited further statistical analysis. Secondly, the assessments were not blinded, as blinding in SCS trials is challenging. This is because patients can discern not only the occurrence of paresthesia but also the variations in frequencies and voltages. Thirdly, as some participants reported exacerbated symptoms after the SCS was turned off, including fatigue, soreness in the lower limbs and back, and other discomforts. In accordance with ethical standards and the principle of no damage, we did not enforce off-state evaluations for all patients. Meanwhile, four patients missed their six-month evaluations during COVID-19 period unfortunately. Among all six patients, we did not deliberately select who would participate in the off-state evaluations, but rather based on the patients’ own willingness and tolerance to the SCS being turned off. Ultimately, three patients participated in the evaluation of the SCS off state.
Conclusion
In conclusions, lower thoracic SCS may be effective for improving PA in PD patients. SCS has shown great promise as a supplementary therapy for PD patients with PA.
Data availability
All data included in this study will be shared by request from any qualified investigator.
Abbreviations
- PA:
-
Postural abnormalities
- PD:
-
Parkinson’s disease
- SCS:
-
Spinal cord stimulation
- MDS-UPDRS:
-
Movement Disorder Society Unified Parkinson’s Disease Rating Scale
- SCOPA-AUT:
-
Scale for Outcomes in PD-Autonomic
- PDQ-39:
-
39-item quality of life questionnaire for Parkinson’s disease
- WCS:
-
Wexner constipation score
References
Lang AE, Lozano AM. Parkinson’s disease. Second of two parts. N Engl J Med. 1998;339:1130–43. https://doi.org/10.1056/NEJM199810153391607.
Hely MA, Reid WG, Adena MA, Halliday GM, Morris JG. The Sydney multicenter study of Parkinson’s disease: the inevitability of dementia at 20 years. Mov Disord. 2008;23:837–44. https://doi.org/10.1002/mds.21956.
Ferraye MU, Debû B, Pollak P. Deep brain stimulation effect on freezing of gait. Mov Disord. 2008;23(Suppl 2):S489–94. https://doi.org/10.1002/mds.21975.
de Andrade EM, Ghilardi MG, Cury RG, Barbosa ER, Fuentes R, Teixeira MJ, et al. Spinal cord stimulation for Parkinson’s disease: a systematic review. Neurosurg Rev. 2016;39:27–35. https://doi.org/10.1007/s10143-015-0651-1. discussion 35.
Samotus O, Parrent A, Jog M. Long-term update of the effect of spinal cord stimulation in advanced Parkinson’s disease patients. Brain Stimul. 2020;13:1196–7. https://doi.org/10.1016/j.brs.2020.06.004.
Prasad S, Aguirre-Padilla DH, Poon YY, Kalsi-Ryan S, Lozano AM, Fasano A. Spinal cord stimulation for very advanced Parkinson’s disease: a 1-Year prospective trial. Mov Disord. 2020;35:1082–3. https://doi.org/10.1002/mds.28065.
Samotus O, Parrent A, Jog M. Spinal cord stimulation therapy for Gait Dysfunction in Advanced Parkinson’s Disease patients. Mov Disord. 2018;33:783–92. https://doi.org/10.1002/mds.27299.
Pinto de Souza C, Hamani C, Oliveira Souza C, Lopez Contreras WO, Dos Santos Ghilardi MG, Cury RG, et al. Spinal cord stimulation improves gait in patients with Parkinson’s disease previously treated with deep brain stimulation. Mov Disord. 2017;32:278–82. https://doi.org/10.1002/mds.26850.
Fénelon G, Goujon C, Gurruchaga JM, Cesaro P, Jarraya B, Palfi S, et al. Spinal cord stimulation for chronic pain improved motor function in a patient with Parkinson’s disease. Parkinsonism Relat Disord. 2012;18:213–4. https://doi.org/10.1016/j.parkreldis.2011.07.015.
Yao MS, Zhou LC, Tan YY, Jiang H, Chen ZC, Zhu L, et al. Gait characteristics and brain activity in Parkinson’s disease with concomitant postural abnormalities. Aging Dis. 2020;11:791–800. https://doi.org/10.14336/AD.2019.0929.
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord. 2015;30:1591–601. https://doi.org/10.1002/mds.26424.
Goetz CG, Stebbins GT, Tilley BC. Calibration of unified Parkinson’s disease rating scale scores to Movement Disorder Society-unified Parkinson’s disease rating scale scores. Mov Disord. 2012;27:1239–42. https://doi.org/10.1002/mds.25122.
Hoehn MM, Yahr MD. Parkinsonism: onset, progression and mortality. Neurology. 1967;17:427–42. https://doi.org/10.1212/wnl.17.5.427.
Cui GH, Yao YH, Xu RF, Tang HD, Jiang GX, Wang Y, et al. Cognitive impairment using education-based cutoff points for CMMSE scores in elderly Chinese people of agricultural and rural Shanghai China. Acta Neurol Scand. 2011;124:361–7. https://doi.org/10.1111/j.1600-0404.2010.01484.x.
Ou R, Liu H, Hou Y, Song W, Cao B, Wei Q, et al. Predictors of camptocormia in patients with Parkinson’s disease: a prospective study from southwest China. Parkinsonism Relat Disord. 2018;52:69–75. https://doi.org/10.1016/j.parkreldis.2018.03.020.
Doherty KM, van de Warrenburg BP, Peralta MC, Silveira-Moriyama L, Azulay JP, Gershanik OS, et al. Postural deformities in Parkinson’s disease. Lancet Neurol. 2011;10:538–49. https://doi.org/10.1016/S1474-4422(11)70067-9.
Schulz-Schaeffer WJ, Margraf NG, Munser S, et al. Effect of neurostimulation on camptocormia in Parkinson’s disease depends on symptom duration. Mov Disord. 2015;30(3):368–72. https://doi.org/10.1002/mds.26081.
Margraf NG, Wolke R, Granert O, et al. Consensus for the measurement of the camptocormia angle in the standing patient. Parkinsonism Relat Disord. 2018;52:1–5. https://doi.org/10.1016/j.parkreldis.2018.06.013.
Tinazzi M, Geroin C, Bhidayasiri R, et al. Task Force Consensus on Nosology and Cut-Off values for Axial Postural abnormalities in parkinsonism. Mov Disord Clin Pract. 2022;9(5):594–603. https://doi.org/10.1002/mdc3.13460. Published 2022 May 9.
Visser M, Marinus J, Stiggelbout AM, Van Hilten JJ. Assessment of autonomic dysfunction in Parkinson’s disease: the SCOPA-AUT. Mov Disord. 2004;19:1306–12. https://doi.org/10.1002/mds.20153.
Jenkinson C, Fitzpatrick R, Peto V, Greenhall R, Hyman N. The Parkinson’s Disease Questionnaire (PDQ-39): development and validation of a Parkinson’s disease summary index score. Age Ageing. 1997;26:353–7. https://doi.org/10.1093/ageing/26.5.353.
Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD. A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum. 1996;39:681–5. https://doi.org/10.1007/BF02056950.
de Lima-Pardini AC, Coelho DB, Souza CP, Souza CO, Ghilardi M, Garcia T, et al. Effects of spinal cord stimulation on postural control in Parkinson’s disease patients with freezing of gait. Elife. 2018;7. https://doi.org/10.7554/eLife.37727.
Stancák A, Kozák J, Vrba I, Tintera J, Vrána J, Polácek H, et al. Functional magnetic resonance imaging of cerebral activation during spinal cord stimulation in failed back surgery syndrome patients. Eur J Pain. 2008;12:137–48. https://doi.org/10.1016/j.ejpain.2007.03.003.
Rasche D, Siebert S, Stippich C, Kress B, Nennig E, Sartor K, et al. [Spinal cord stimulation in Failed-Back-Surgery-Syndrome. Preliminary study for the evaluation of therapy by functional magnetic resonance imaging (fMRI)]. Schmerz. 2005;19:497–500. https://doi.org/10.1007/s00482-005-0388-9.
Thevathasan W, Mazzone P, Jha A, Djamshidian A, Dileone M, Di Lazzaro V, et al. Spinal cord stimulation failed to relieve akinesia or restore locomotion in Parkinson disease. Neurology. 2010;74:1325–7. https://doi.org/10.1212/WNL.0b013e3181d9ed58.
Zhou PB, Bao M. Spinal cord stimulation treatment for freezing of gait in Parkinson’s disease: a case report. Brain Stimul. 2022;15:76–7. https://doi.org/10.1016/j.brs.2021.11.011.
Agari T, Date I. Spinal cord stimulation for the treatment of abnormal posture and gait disorder in patients with Parkinson’s disease. Neurol Med Chir (Tokyo). 2012;52(7):470–4. https://doi.org/10.2176/nmc.52.470.
Yadav AP, Nicolelis M. Electrical stimulation of the dorsal columns of the spinal cord for Parkinson’s disease. Mov Disord. 2017;32:820–32. https://doi.org/10.1002/mds.27033.
Thiriez C, Gurruchaga JM, Goujon C, Fénelon G, Palfi S. Spinal stimulation for movement disorders. Neurotherapeutics. 2014;11:543–52. https://doi.org/10.1007/s13311-014-0291-0.
Kreydin E, Zhong H, Lavrov I, Edgerton VR, Gad P. The Effect of non-invasive spinal cord stimulation on anorectal function in individuals with spinal cord Injury: a Case Series. Front Neurosci. 2022;16:816106. https://doi.org/10.3389/fnins.2022.816106. Published 2022 Feb 17.
Laskin JJ, Waheed Z, Thorogood NP, Nightingale TE, Noonan VK. Spinal Cord Stimulation Research in the Restoration of Motor, sensory, and autonomic function for individuals living with Spinal Cord Injuries: a scoping review. Arch Phys Med Rehabil. 2022;103(7):1387–97. https://doi.org/10.1016/j.apmr.2022.01.161.
Flett S, Garcia J, Cowley KC. Spinal electrical stimulation to improve sympathetic autonomic functions needed for movement and exercise after spinal cord injury: a scoping clinical review. J Neurophysiol. 2022;128(3):649–70. https://doi.org/10.1152/jn.00205.2022.
Acknowledgements
We thank all the patients for the study. We are very grateful to our funders for their support over the past years.
Funding
This work was supported by grants from the National Natural Science Foundation of China (82071415, 82001340 and 81873778); the Innovative research team of high-level local universities in Shanghai; and the Science and Technology Commission of Shanghai Municipality (19411968300).
Author information
Authors and Affiliations
Contributions
Liche Zhou: Data curation; Investigation; Methodology; Formal Analysis; Writing-Original Draft Preparation; Writing-Review&Editing. Fangzheng Chen: Writing-Original Draft Preparation; Writing-Review&Editing. Yixin Pan: Data curation; Investigation; Writing-Review&Editing. Linbin Wang: Funding acquisition; Data curation; Investigation; Writing-Review&Editing. Lu Xu: Investigation; Writing-Review&Editing. Peng Huang: Investigation; Writing-Review&Editing. Lijun Wang: Data curation; Investigation; Writing-Review&Editing. Ningdi Luo: Data curation; Investigation; Writing-Review&Editing. Puyu Li: Formal Analysis; Writing-Review&Editing. Dianyou Li: Conceptualization; Supervision; Writing-Review&Editing. Jun Liu: Conceptualization; Supervision; Project administration; Funding acquisition; Writing-Review&Editing.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine (2019-62). The protocol of the current study fitted the guidelines of the Declaration of Helsinki and its later amendments. Written informed consents were obtained from participants.
Consent for publication
Written informed consents for publication were obtained.
Competing interests
The authors declare that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, L., Chen, F., Pan, Y. et al. Spinal cord stimulation for postural abnormalities in Parkinson’s disease: 1-year prospective pilot study. BMC Neurol 24, 167 (2024). https://doi.org/10.1186/s12883-024-03673-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-024-03673-5