Abstract
Background
Stroke survivors suffer an overall loss of social participation. However, the interventions aiming at improving social participation have not yet been well-established. There is a need to synthesize existing knowledge on clinical interventions aiming at improving social participation among people with stroke.
Objective
To describe the patterns of intervention that have been applied to stroke survivors to improve social participation and to determine the preliminary effects of these patterns.
Methods
Eight online databases, including Cochrane Library, PubMed, Web of Science, Embase, Medline, CINAHL plus, PsycINFO, and Scoups were searched with predefined search terms from inception to September 22, 2022. References of included articles and previous reviews were also checked to identify additional studies. Two reviewers independently selected eligible studies and extracted data from the included articles.
Results
A total of 98 studies were included, of which only 25 studies considered social participation as primary outcome of clinical interventions. The patterns of intervention were various, consisting of exercise-based intervention, occupational therapy, self-management program, and complex intervention. Of the 25 studies, eight studies found a positive effect of relative clinical intervention on social participation for stroke survivors. Of note, the same modality of intervention such as exercise-based intervention and self-management program produced paradoxical conclusion on social participation.
Conclusion
Exercised-based intervention, occupational therapy, self-management program, and complex intervention were important intervention modalities for the improvement of social participation among stroke survivors. Even though the preliminary effectiveness on social participation seems to be potentially positive, further high-quality researches are still required to reach a consensus to achieve optimal social participation among stroke survivors.
Similar content being viewed by others
Introduction
Stroke has been a major global health concern, characterized by high morbidity, and a high rate of disability and recurrence [1]. With the increased population aging worldwide, the significance of stroke appears to increase in the future [2]. The main problem faced by stroke survivors is the long-term impact of disability on physical, psychological, and social function. Early-stage and continuous rehabilitation have been considered as a major buffer against unexpected changes resulting from stroke [3].
Social participation that refers to involvement in the life situation has been viewed as an ultimate outcome of successful rehabilitation according to the International Classification of Functioning, Disability, and Health (ICF) [4, 5]. Despite a strong willingness of stroke survivors to return to their previous lifestyle, their social participation was severely impaired [6]. Current evidence has found that there were tremendous difficulties for stroke survivors to re-engage in work, valued activities, and interpersonal interaction [7, 8]. Stroke survivors with a low level of social participation are at increased risk for adverse health outcome, including low mood, recurrent stroke, low quality of life, and even mortality [9]. As a result, the improvement of social participation among stroke survivors has been a primary focus of community rehabilitation [10].
Post-stroke social participation is a major public concern, which is associated with stroke-related physical dysfunction (including limb function, communication barriers, and cognition), emotion disorders (such as depression and isolation), and environment [11, 12]. There is an urgent demand for effective intervention program to continuously enhance social participation among stroke survivors. However, current rehabilitation studies frequently did not include social participation as a routine measurement outcome [13]. Some clinical trials merely included social participation as a secondary outcome rather than a primary outcome. In fact, current interventions mainly focus on the effectiveness on stroke survivors’ physical function rather than social participation itself [14, 15]. Of note, a good physical function was not always associated with satisfactory social participation among stroke survivors. A previous study pointed out that although stroke survivors showed very mild impairment and disability, their participation in daily activities and social role was substantially impacted [16].
Collectively, social participation among stroke survivors remains unsatisfactory, and the interventions aiming at improving social participation are not well-established. Thus, it is necessary to improve knowledge about clinical interventions for the improvement of social participation among stroke survivors. A scoping review that can outline key concepts, types of evidence, and gaps in research related to specific areas is an effective form of knowledge synthesis [17, 18]. Scoping review provides guidance for future research priorities by systematically searching, selecting, and integrating existing knowledge. Therefore, the aim of this scoping review is to (1) map the current evidence surrounding the interventions for improving social participation among stroke survivors and identify knowledge gaps in the researches, and (2) determine the preliminary effectiveness of the interventions on social participation among stroke survivors. This scoping review is expected to provide a basis for follow-up interventional studies.
Methods
This scoping review was conducted based on the methodology outlined by Arksey and O’ Malley and refined by Levac et al. and the PRISMA Extension for Scoping Reviews (PRISMA-ScR) [17, 18]. The methodology mainly involved six stages, (1) identifying the research questions; (2) searching related studies; (3) screening the studies; (4) charting the data; (5) collating, summarizing, and reporting the results; and (6) consultation with broader stakeholder, respectively. A scoping review methodology was selected because it can address more broad questions and identify the types of available evidence in a given field [19]. A scoping review also serves as a precursor to a systematic review [19]. This methodology assists to identify the gaps in current knowledge base to provide guide for further research in the field. The scoping review hasn’t been registered anywhere.
Search strategy
Eight online databases, including Cochrane Library, PubMed, Web of Science, Embase, Medline, CINAHL plus, PsycINFO, and Scoups were searched from database inception to September 22, 2022 to hit relevant studies concerning interventions to improve social participation among stroke survivors. The search terms were “stroke” and “participation”, and synonyms and Boolean operators were used in the search strategy. The specific search strategy was showed in Additional file (Supplement Table 1). There was no restriction on language published and study design. Additionally, a hand search was performed to select the references of included studies and previously published reviews.
Study selection
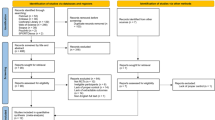
A total of 13,149 searched studies from the 8 databases were imported into Endnote X9 to exclude duplicates (Fig. 1). The inclusion criteria for studies in this scoping review were: (1) study participants who were stroke survivors and aged over 18 years; (2) experimental study; (3) outcome measures including social participation; and (4) social participation outcome evaluated using scales but not the qualitative description. The exclusion criteria were (1) participants with severe comorbidities such as malignant tumors and organ dysfunction; (2) animal experiments; and (3) unavailable full text. Additionally, study reviews were excluded, but their references were checked for presence in the search result. Two review authors independently screened titles, abstracts, and full-text articles based on inclusion and exclusion criteria after training, with a third review author available to moderate any disagreements. The review authors also contacted the investigators for additional data when required.
Quality appraisal
Cochrane risk of bias tool in the Cochrane Handbook (version 5.1.0) was used for the randomized controlled trials (RCTs) [44]. A total of seven indicators (random sequence generation, allocation concealment, blindness of participant and personnel, blindness of outcome assessment, incomplete outcome data, selective reporting, and other bias) was evaluated using “low risk”, “unclear risk”, or “high risk”. The criteria of the Australian Evidence-based Health Care Center for non-randomized controlled trials (non-RCTs) were used as well [45]. Each entry was assessed with “yes”, “no”, “unclear”, or “not applicable”. The quality appraisal was performed only for studies that considered social participation as primary outcome measure.
Data extraction
Data extraction was independently performed by two authors using Excel 2016 for tabulating the descriptive data from all included studies. The detailed information included author, year, country, participant characteristics (time from onset, and age), study design, sample size, study target, intervention, setting, training dosage, measurement point, the type of social participation outcome (primary or secondary), measurement tool of social participation, and results. Any disagreements between reviewers were resolved by consensus through team discussion.
Narrative synthesis
Narrative analyses were performed to summarize the study results. results. The analyses were guided by a three-step narrative synthesis framework: (1) develop a preliminary synthesis; (2) explore relationship between data; and (3) assess the robustness of the synthesis [46]. The first step was performed by identifying patterns using tabulation, grouping and thematic analysis. The second step was conducted by analyzing participant demographics, measurement of social participation, and intervention characteristics. Finally, the robustness of the synthesis was represented by methodological quality of included studies that considered social participation as primary outcome, the information required from included studies, and strength of conclusion that could be made. Additionally, frequencies and percentages were calculated to summarize the data if necessary.
Results
A total of 98 studies selected were included in the review. According to the primary outcome or secondary outcome of social participation, the data extracted were presented in two parts. The summary of 25 included studies where social participation was considered as primary outcome is shown in Tables 1 and 2. 73 studies where social participation was considered as secondary outcome were reported in Additional file (Supplementary Tables 2 and Table 3). All 98 published articles were distributed within a time frame of 20 years (2001–2022). Average two or three articles per year were published relevant to interventions to improve poststroke social participation from 2001 to 2012. However, since 2013, a substantial increase in the number of studies related to our scoping purpose. There were 72 studies published between 2013 and 2022, accounting for 73.5%. Of the 25 studies, four studies were from America, followed by Canada (N = 3), Sweden (N = 3), and the Netherland (N = 3). The majority of study designs were RCTs (76.0%), and the remaining studies were pre-post clinical trials. Of the 73 studies, 16 studies were from Canada (21.9%), 12 studies from America (16.4%), eight studies from Australia (11.0%), eight studies from China (11.0%), and seven studies from the UK (9.6%), respectively. The RCTs accounted for 68.5%. The other studies were single-group pre-post design and control studies (Supplementary Table 2).
Quality appraisal
The quality appraisal of studies considering social participation as primary outcome is represented in Additional file (Supplementary Tables 4 and Table 5). For RCTs, the leading risk was the blindness of participant and personnel. While many studies complied with the blindness of outcome assessment, the assessors might become aware of the allocation through patients’ responses during interviews, which may result in some bias. The randomization was generally performed. Allocation concealment in some studies was high risk or unclear risk due to lack of specific description. The overall study quality for RCTs was medium quality and above. For non-RCTs, the main risk was lack of control group and detailed description of the incomplete follow-up. The methodological quality for non-RCTs was acceptable.
Participants
Across the 25 articles, there were a total of 2091 participants. The average age or median age of the participants in most studies was over 60. There were only four articles with the mean age of the participants less than 50 [22, 25, 27, 37]. The period from onset to recruitment was various, which ranged from just 48 h after onset to several years following stroke. Three months and six months post-stroke were the frequently used time cutoff. With regards to the comorbidities, the participants in eight studies had physical impairments, including upper or limb function impairments, disability, and hemiparesis. Three articles reported post-stroke aphasia and two described cognitive impairments. The remaining studies had no clear description of the participants’ comorbidities. The results related to participants’ characteristics from 73 studies in which social participation was viewed as secondary outcome were similar with above description (Supplementary Table 2).
Participation measures
The included studies covered a variety of operational definitions, as presented in Table 1. The term “participation” and “social participation” were the most common. Of the enrolled studies, a total of 12 measurement tools were used to assess social participation. The participation subscale of the Stroke Impact Scale (SIS) was the most frequently used tool by 7 of 25 studies (28.0%). The second most common tool was the Reintegration to Normal Living Index (RNLI, 20.0%), followed by the Community Integration Questionnaire (CIQ, 16.0%) and Utrecht Scale for Evaluation of Rehabilitation-Participation (USER-P, 12.0%). Of the 25 studies, 10 studies measured outcome at three time points (baseline, post-intervention, and follow-up) and 9 studies at two time points (baseline and post-intervention). When it comes to the follow-up measure, 3 months after the intervention was the most frequently used. Of the 73 included studies, the most frequently used tool was the participation subscale of the Stroke Impact Scale (SIS) as well. The most frequent selection of follow-up duration was 3 months after the intervention, followed by 6 months, one year, and one month after the intervention (Supplementary Table 2).
Training dosage
The period of training varied from two days to six months. Specifically, 8 weeks (N = 4) and 12 weeks (N = 4) were the most frequently reported. The total sessions of the interventions varied from 2 sessions to 58 sessions, of which the top two sessions of intervention were 12 sessions (N = 3) and 10 sessions (N = 3). The session duration lasted from 10 min to 2.5 h, and the most frequent duration used was 30 min (N = 6), followed by 1 h (N = 2) and 2 h (N = 2). The session frequency ranged from twice a month to five times per week, and the most frequently reported session frequency was 2 to 3 times per week (N = 8). The different dosage for each study was presented detailly in Table 2. Of the 73 included studies, the most frequently used training period was 6–8 weeks. The top three sessions of intervention were 20 sessions (N = 10), 12 sessions (N = 7), and 36 sessions (N = 7), respectively. One-to-two-hour duration per session and 2 to 3 times per week were the most prevalent respectively (Supplementary Table 3).
Training protocol
Of the 25 studies, eight studies focused on physical exercise. Specifically, two studies were dedicated to identifying the effect of virtual reality program on assisting in the functional recovery [20, 27]. The participants needed to perform games that were conducted difficultly in the initial evaluation using the Canadian Occupational Performance Measure (COPM). The games trained participants’ motor skills, motor coordination, and cognitive skills. The other two studies demonstrated the effectiveness of treadmill and leg cycle ergometer as assisted exercise devices on lower-limb functions [41, 47]. The remaining four studies described different exercise methods, such as walk training, yoga training, and strength, balance, and motor coordination trainings supported by Physiotherapists [33,41–43,,]. Additionally, post-stroke aphasia and cognitive impairment is two potential factors to influence social participation. Two studies examined respectively whether grouping singing and supported conversation provided over Skype could improve stroke survivors’ social participation [21, 24]. One article investigated the effectiveness of computer-based cognitive flexibility training [31]. Generally, close to half of the studies considered physical exercise as a significant intervention modality to promote social participation.
In addition to exercise-based intervention, occupational therapy was another frequently reported intervention for seven times [25, 26, 28, 29, 32, 36, 42]. During the treatment process, occupational therapists made an initial evaluation to clarify the participants’ ability by using COPM and helped them set appropriate goals for activities. Thereafter, the participants and occupational therapists together identified specific strategies that would enable successful performance of the chosen activity. The strategies consisted of problem solving, implementing new ways of performing activities of daily living (ADL), home modification, motivational enhancement, and self-management strategies. Some studies encouraged family to participate in occupational therapy [29]. It is possible to use mobile phones to supervise participants to perform activities themselves during occupational therapists’ follow-up intervals [29].
Self-management programs which focus on teaching stroke survivors’ important skills to manage their functional and emotional conditions, such as setting goals, problem-solving, decision-making, and resource utilization are becoming more prevalent, given the positive effect of self-management programs in other chronic diseases, such as diabetes, asthma, and chronic obstructive pulmonary disease. Two studies evaluated the feasibility and effectiveness of self-management strategies for reinforcement of social participation after stroke [23, 34]. Moreover, there were five studies that considered social participation as secondary outcome exploring the effectiveness of self-management interventions on helping stroke survivors to engage in the society. However, the studies indicated that the effectiveness of self-management interventions was controversial among stroke survivors. It was believed that one of the mechanisms accountable for the enhancement of health behaviors by self-management was strengthening individuals’ self-efficacy to manage their condition.
Health education was as well used to improve social participation after stroke in two studies [37, 43]. The education topics were various, including emotional support, communication strategies, driving, working, active strategies for coping, sleep, yoga. Additionally, the Community Re-engagement Cue to Action Trigger Tool (CRCATT), a patient-mediated question prompt list, covering eight areas was used to cue and supervise stroke survivors for re-engagement in activities post-stroke [35]. It was perceived that CRCATT could assisted stroke patients to play a more self-directed role by asking relevant questions and anticipating their needs. Complex intervention was the last reported intervention method. Generally, complex intervention contained different contents, such as physical exercise, emotional support, and strategy acquisition [22, 33]. For example, a caregiver-mediated, home-based intervention possessed the following functions:, to improve stroke patients’ body functions and structural components, to enhance patients’ ability to perform daily activities within their living environments using compensatory training methods, and to assist the patients return to the society by the participation in outdoor leisure activities [33].
Of the 73 studies with social participation as secondary outcome, exercise-based intervention was still the most frequently described (N = 40; Supplementary Table 3). However, the content of exercise-based intervention varied more widely compared with studies with social participation as primary outcome, which embodied body parts, assisted devices, settings, patients’ course of disease. It is the best of our acknowledged that common dysfunction after stroke includes motor dysfunction, cognitive dysfunction, speech dysfunction, swallowing dysfunction, sensory dysfunction and so on. Thus, the target of exercise-based intervention was diverse. Besides, the physical exercise was inseparable from advanced medical devices. For example, robot-based exercise was more prevalent in during the rehabilitation process post stroke. The training settings were not limited to hospitals and rehabilitation facilities, but extended to communities and participant’s homes. Short message and mobile calls quickly became increasingly receptive to urge the patients’ continuous training within their own living environment. Additionally, some studies combine cognitive training and aerobic exercise together in order to enhance the effectiveness of physical recovery. Similarly, occupational therapy was of great concern in improving social participation (N = 10). Occupational therapists were confronted with a change in task-targeted activities from ADL into social activities, such as meeting friends. Self-management strategies acquisition seemed to be as important as physical recovery with reported for five times. Complex intervention that referred multidisciplinary cooperation and multidimensional support was becoming increasingly prevalent among with reported for seven times. In addition, some intervention programs such as information providing, calls, stroke navigation service, consultation supported by nurses, health education were as well investigated. One study examined the effectiveness of botulinum toxin injections (BoNT-A) on function and participation by improving stroke survivors’ physical activities.
Effectiveness of training on participation
Of the 25 articles treating social participation as a primary outcome, nine studies found positive results [22, 24, 25, 33, 37,38,39,40,41], while 14 studies did not show positive findings and two did not report the corresponding statistical analysis. The nine studies comprised of five RCTs and four single group pre-post study designs. The interventional protocol of the nine studies consisted of physical exercise (N = 4), supported conversation training for post-stroke aphasia (N = 1), occupational therapy (N = 1), health education (N = 1), and complex intervention (N = 2). Of the 73 studies with social participation as a secondary outcome, 26 studies had a positive result, and in these studies, the majority of intervention programs were physical exercise (N = 17). The rest studies focused on occupational therapy, self-management programs, complex intervention, health education, and invasive injection. Given the variety in included studies and difficulty in synthesis, the preliminary effectiveness of identified intervention modalities was evaluated by the number of studies that had a positive result. In summary, the preliminary effectiveness of intervention modalities for post-stroke social participation was potentially positive. Specifically, the exercise-based interventions and complex intervention seemed to be more promising than other interventions. But the effectiveness of exercise-based interventions on enhancing social participation among stroke survivors was paradoxical. The effect of self-management interventions and complex interventions needs to be further clarified given the controversial results in studies where social participation was primary outcome and secondary outcome.
Discussion
This scoping review was performed to map the literature regarding the implementation of interventions to improve social participation following stroke and to identify the preliminary effectiveness for stroke survivors. We identified 98 studies that explored interventions for improving social participation after stroke, typically using a RCT or pilot study design.
Our scoping review reveals several different patterns of intervention. Firstly, exercise-based intervention was frequently mentioned regardless of the outcome type of social participation. It is believed that physical recovery was an important approach to enhance patients’ abilities to participate in society [6], which is consistent with the ICF framework. A previous study found that exercised-based intervention might be effective in promoting post-stroke social participation [48]. A critical concern to existing evidence is that physical exercise is a broad concept and may be implemented in diverse ways, making it hard to figure out which exercise patterns are the most effective [49]. However, it’s notable that a comprehensive and personalized exercise-based intervention may be more beneficial to orient rehabilitation modality to patients’ goals due to the diverse physical dysfunction after stroke. Considering the long-term process of stroke rehabilitation, exercise-based intervention should be conducted persistently to promote the transformation of stroke patients’ participation from family to society.
Next, occupational therapy is another key intervention pattern. Its’s expected that occupational therapy may enhance social participation following stroke by the improvement of activity level according to ICF [50]. Occupational therapy was increasingly prevalent in view of the advantages of client-centered task training and being capable of being performed in the context of their living environment. Originally activities trained were home-based ADL that people carried out to maintain well-being [51]. Recently the range of activities is being extended to leisure activities and social activities. Occupational therapist directly helps stroke patients reintegrate into society by acquiring special strategies rather than learning ability of ADL [52]. To strength the effectiveness of occupational therapy, these strategies are quite important, such as motivational enhancement and problem-solving. Furthermore, caregivers should be included into the treatment team because they might play an essential role in both assisting stroke survivors in performing activities and acting as a therapist at the time of occupational therapist’ visit interval [29].
The next modality of intervention is self-management program. When the irreversible impairment caused by the stroke occurs, stroke survivors have to learn coping skills for re-obtain a better social participation. Self-management program is considered as a key way to address the gap because it is beneficial to empower clients and strengthen their beliefs in completing a specific task [53, 54]. Therefore, it is believed that self-management program is an indispensable way to compensate for missing physical function by enhancing strategies and skills to manage individual condition and achieve social participation. However, the effect of self-management programs needs to be further verified in the future.
Complex intervention is another significant intervention modality, which may provide multidimensional supports when stroke survivors encounter low self-efficacy, inappropriate coping style, inadequate family support, and inaccessibility of social services. The essence of a complex intervention is to target several factors important for influencing social participation. For example, Mayo et al. developed a community-based complex intervention according to the research priorities, including exercise-based programs, and project-based activities promoting learning, leisure, and social activities [55]. Generally, complex intervention was mainly applied in community and participants’ homes, aiming at fully utilizing the relevant resources. Health Education used to work as a separate intervention but now is incorporated into other intervention patterns, such as complex intervention. Stroke survivors’ knowledge may facilitate the management of their own life and social participation. Other intervention modalities were reported less frequently, but may be beneficial to improve social participation, such as CRCATT, a patient-mediated question prompt list [35]. Further studies are needed to examine the effectiveness of the novel intervention pattern.
With regards to the preliminary effectiveness, our findings support a potentially positive effect on improving social participation following stroke. Furthermore, it seems that exercise-based intervention has more benefits for stroke survivors compared with non-exercise-based intervention. Of note, controversial conclusion at the same intervention pattern is common. For example, virtual reality-based limb exercise, occupational therapy, and self-management program, and complex intervention produced both positive and negative results. It is not clear whether such a mix effect is induced by the intervention itself, the different dosage, or participants’ characteristics. Therefore, the real effectiveness of the different interventions remains to be explored.
Another critical question worth our profound meditation is that how to push these intervention patterns on stroke survivors so that they can obtain sustained benefits given the long-term process of stroke rehabilitation. Some studies demonstrated a positive short-term result (assessed at post-intervention time) but a negative long-term result (assessed at follow-up time, usually three months after the end of intervention), which revealed the intervention effect faded as the supports ended. On the one hand, it is appropriate to integrate the behavior change skills into the intervention to make active participation in society a habit [56]. On the other hand, it is necessary to make the supportive resources always accessible for stroke survivors. Mobile phone is expected to become an effective tool to continue to interact with stroke survivors and their caregivers and provide various supports so as to promote them to integrate into society.
The stroke patients included into this scoping review mainly covered middle-aged and elderly stroke survivors. To the best of our knowledge, age is the high risk of stroke, and people aged over 50 show susceptibility to stroke. In fact, stroke survivors tend to be younger recently and the loss of social participation seems to be more catastrophic for young people [57]. Thus, further research is needed to identify the characteristics of social participation in young stroke survivors and to explore intervention protocols targeted at them. Our findings regarding multiple measurement tools and operational definitions of social participation are consistent with previous literature [8]. The most frequently used measures in our study were the participation subscale of SIS (SIS-P), followed by RNLI and CIQ. These differences regarding social participation measurements are influenced by inconsistent conceptualization and may further affect the findings of included studies and the comparison of results. Representation of clear and consistent conceptualization and measurement have always been an issue in social participation research [58]. Moreover, with the development of subjective social participation, a notable concern is how to improve participation experiences and feelings among stroke survivors, given the quality of be socially participating is far more important than the amount to participate for people with disability [59]. The various training dosages may be another factor leading to inconsistent results of intervention protocols. For example, the self-management program with 18 two-hour, group-based sessions, twice per week for 8 weeks showed a positive effect on post-stroke social participation [60], while the self-management protocol with 12 weekly group sessions, each lasting 2.5 h demonstrated a negative result [61]. More intensive interventions may show a better interventional effect on social participation. Furthermore, our scoping review provides referenced training period (8 weeks), sessions (10–12 sessions), duration (30 min), and frequency (2 to 3 times per week) for better improving social participation. Additionally, the lack of heterogeneity of the countries and religion where the studies were performed could compromise adaptability and application of intervention modalities of social participation. Among the intervention protocols reviewed in this study, face-to-face interventions were dominated. In the future, the effects of smartphone-based tele-intervention can be further explored, with the advantage of achieving across-culture interaction [62].
Limitation and implication
There are a few limitations that should be acknowledged in the present scoping review. Firstly, despite every effort we have tried, three studies were excluded for unavailable full-text, which may have contributed to the incomplete synthesis of data. Secondly, we have made efforts to search eligible studies by checking references and contacting the investigators to reduce effect of incomplete data synthesis. Nevertheless, there were still some studies that mixed stroke survivors with other patients (e.g., traumatic brain injury, spinal injury, or impaired neurological conditions) being removed due to the failure to obtain the raw data of stroke survivors, which may also have an impact on the synthesis. Thirdly, there was a wide variation in the included studies, especially in the training programs, training dosages, and measurement tools of social participation, which may result in challenge in interpreting the results. While we have identified several intervention modalities, the preliminary effectiveness of current interventions on social participation among stroke survivors is hard to conclude in this scoping review. In the future, a meta-analysis may be carried out to determine the consistent discussion of some interventional protocols, such as self-management programs and occupational therapy. Finally, social participation was not widely used as a primary outcome, influencing the assessment and establishment of effective interventions. Our study distinguished the results in social participation as primary outcome and secondary outcome. More high-quality and large-sample researches are needed to identify the effectiveness of various interventions on post-stroke social participation that is viewed as a primary outcome. Additionally, the synthesis of data in our scoping review may provide some insight into participants, helpful measuring instruments, potential training protocol, and appropriate training dosage.
Conclusion
Exercised-based intervention, occupational therapy, self-management program, and complex intervention were important intervention modalities for improvement of social participation among stroke survivors. The preliminary effectiveness of identified intervention patterns was potentially positive. High-quality researches should be conducted to a consistent discussion targeted at achieving meaningful social participation after stroke.
Data Availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
References
Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart disease and stroke statistics–2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209.
Roth GA, Forouzanfar MH, Moran AE, Barber R, Nguyen G, Feigin VL, et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 2015;372:1333–41.
Winstein CJ, Stein J, Arena R, Bates B, Cherney LR, Cramer SC, et al. Guidelines for adult Stroke Rehabilitation and Recovery: a Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47:e98–e169.
Bergstrom A, Guidetti S, Tham K, Eriksson G. Association between satisfaction and participation in everyday occupations after stroke. Scand J Occup Ther. 2017;24(5):339–48.
Engel-Yeger B, Hamed-Daher S. Comparing participation in out of school activities between children with visual impairments, children with hearing impairments and typical peers. Res Dev Disabil. 2013;34(10):3124–32.
Zhou X, Du M, Weng Y, Zhou L. Hard return: the development and transformation process of social participation in stroke survivors; a qualitative study and initial theory. Clin Rehabil. 2020;34:824–36.
Urimubenshi G. Activity limitations and participation restrictions experienced by people with stroke in Musanze district in Rwanda. Afr Health Sci. 2015;15:917–24.
Engel-Yeger B, Tse T, Josman N, Baum C, Carey LM. Scoping Review: The Trajectory of Recovery of Participation Outcomes following Stroke. Behav Neurol. 2018; 2018: 5472018.
Zhang L, Sui M, Yan T, You L, Li K, Gao Y. A study in persons later after stroke of the relationships between social participation, environmental factors and depression. Clin Rehabil. 2017;31:394–402.
Winstein CJ, Stein J, Arena R, Bates B, Cherney LR, Cramer SC, et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47(6):e98–e169.
Ezekiel L, Collett J, Mayo NE, Pang L, Field L, Dawes H. Factors Associated with participation in life situations for adults with stroke: a systematic review. Arch Phys Med Rehabil. 2019;100:945–55.
Gustavsson M, Guidetti S, Eriksson G, von Koch L, Ytterberg C. Factors affecting outcome in participation one year after stroke: a secondary analysis of a randomized controlled trial. J Rehabil Med. 2019;51:160–6.
Bergstrom A, Guidetti S, Tham K, Eriksson G. Association between satisfaction and participation in everyday occupations after stroke. Scand J Occup Ther. 2017;24:339–48.
Tavares Aguiar L, Nadeau S, Rodrigues Britto R, Fuscaldi Teixeira-Salmel L, Caetano Martins J, Ribeiro Samora GA, et al. Effects of aerobic training on physical activity in people with stroke: a randomized controlled trial. NeuroRehabilitation. 2020;46(3):391–401.
Aprile I, Germanotta M, Cruciani A, Loreti S, Pecchioli C, Cecchi F, et al. Upper Limb Robotic Rehabilitation after Stroke: a Multicenter, Randomized Clinical Trial. J Neurol Phys Ther. 2020;44(1):3–14.
Rochette A, Desrosiers J, Bravo G, St-Cyr-Tribble D, Bourget A. Changes in participation after a mild stroke: quantitative and qualitative perspectives. Top Stroke Rehabil. 2007;14(3):59–68.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143.
de Rooij IJM, van de Port IGL, Punt M, Abbink-van Moorsel PJM, Kortsmit M, van Eijk RPA et al. Effect of virtual reality gait training on participation in survivors of Subacute Stroke: a Randomized Controlled Trial. Phys Ther. 2021;101(5).
Tarrant M, Carter M, Dean SG, Taylor R, Warren FC, Spencer A, et al. Singing for people with aphasia (SPA): results of a pilot feasibility randomised controlled trial of a group singing intervention investigating acceptability and feasibility. BMJ open. 2021;11(1):e040544.
Bin Zainal MN, Pei Wen PK, Sien NY, Kee KM, Chieh KJ, Asano M. Supporting people with stroke to return to work in Singapore: findings from a Pilot Vocational Rehabilitation Program. Am J Occup Ther. 2020;74(6):7406205040p1–p9.
Harel-Katz H, Adar T, Milman U, Carmeli E. Examining the feasibility and effectiveness of a culturally adapted participation-focused stroke self-management program in a day-rehabilitation setting: a randomized pilot study. Top Stroke Rehabil. 2020;27(8):577–89.
Cruice M, Woolf C, Caute A, Monnelly K, Wilson S, Marshall J. Preliminary outcomes from a pilot study of personalised online supported conversation for participation intervention for people with Aphasia. Aphasiology. 2020;1–25.
Chinchai P, Sirisatayawong P, Jindakum N. Community Integration and Quality of Life: stroke survivors as recipients of Rehabilitation by Village Health volunteers (VHVs) in Thailand. Occup Ther Health Care. 2020;34(3):277–90.
Hedman A, Eriksson G, von Koch L, Guidetti S. Five-year follow-up of a cluster-randomized controlled trial of a client-centred activities of daily living intervention for people with stroke. Clin Rehabil. 2019;33(2):262–76.
Aramaki AL, Sampaio RF, Cavalcanti A, Martins Silva e Dutra FC. Use of client-centered virtual reality in rehabilitation after stroke: a feasibility study. Arq Neuro-Psiquiat. 2019;77(9):622–31.
Stark S, Keglovits M, Somerville E, Hu Y-L, Conte J, Yan Y. Feasibility of a novel intervention to improve participation after stroke. Brit J Occup Ther. 2018;81(2):116–24.
Kamwesiga JT, Eriksson GM, Tham K, Fors U, Ndiwalana A, von Koch L, et al. A feasibility study of a mobile phone supported family-centred ADL intervention, F@ce (TM), after stroke in Uganda. Global Health. 2018;14(1):82.
Brouwer B, Bryant D, Garland SJ. Effectiveness of client-centered “Tune-Ups” on Community Reintegration, mobility, and Quality of Life after Stroke: a Randomized Controlled Trial. Arch Phys Med Rehab. 2018;99(7):1325–32.
van de Ven RM, Murre JMJ, Buitenweg JIV, Veltman DJ, Aaronson JA, Nijboer TCW, et al. The influence of computer-based cognitive flexibility training on subjective cognitive well-being after stroke: a multi-center randomized controlled trial. PLoS ONE. 2017;12(11):e0187582.
Kessler D, Egan M, Dubouloz C-J, McEwen S, Graham FP. Occupational Performance Coaching for Stroke Survivors: a pilot randomized controlled trial. Am J of Occup Ther. 2017;71(3):1–7.
Wang T-C, Tsai AC, Wang J-Y, Lin Y-T, Lin K-L, Chen JJ, et al. Caregiver-mediated intervention can improve physical functional recovery of patients with chronic stroke: a Randomized Controlled Trial. Neurorehab Neural Re. 2015;29(1):3–12.
Tielemans NS, Visser-Meily JMA, Schepers VPM, Passier PE, van de Port IGL, Vloothuis JDM, et al. Effectiveness of the Restore4stroke self-management intervention “Plan ahead!”: a Randomized Controlled Trial in Stroke Patients and Partners. J Rehabil Med. 2015;47(10):901–9.
McKellar J, Cheung D, Huijbregts M, Cameron J. The impact of a community re-engagement cue to action trigger tool on re-engaging in activities post-stroke: a mixed-methods study. Top Stroke Rehabil. 2015;22(2):134–43.
Guidetti S, Ranner M, Tham K, Andersson M, Ytterberg C, Von Koch L. A “Client-centred activities of Daily Living” intervention for persons with stroke: one-year Follow-Up of a Randomized Controlled Trial. J Rehabil Med. 2015;47(7):605–11.
Muller M, Toth-Cohen S, Mulcahey MJ. Development and evaluation of a hospital-based peer support group for younger individuals with stroke. Occup Ther Health Care. 2014;28(3):277–95.
Kim M, Cho K, Lee W. Community walking training program improves walking function and social participation in chronic stroke patients. Tohoku J Exp Med. 2014;234(4):281–6.
Marsden D, Quinn R, Pond N, Golledge R, Neilson C, White J, et al. A multidisciplinary group programme in rural settings for community-dwelling chronic stroke survivors and their carers: a pilot randomized controlled trial. Clin Rehabil. 2010;24(4):328–41.
Harrington R, Taylor G, Hollinghurst S, Reed M, Kay H, Wood VA. A community-based exercise and education scheme for stroke survivors: a randomized controlled trial and economic evaluation. Clin Rehabil. 2010;24(1):3–15.
Smith PS, Thompson M. Treadmill training post stroke: are there any secondary benefits? A pilot study. Clin Rehabil. 2008;22(10–11):997–1002.
Parker CJ, Gladman JRF, Drummond AER, Dewey ME, Lincoln NB, Barer D, et al. A multicentre randomized controlled trial of leisure therapy and conventional occupational therapy after stroke. Clin Rehabil. 2001;15(1):42–52.
Hinckley JJ, Packard MEW. Family education seminars and social functioning of adults with chronic aphasia. J Commun Disord. 2001;34(3):241–54.
Shuster JJ. Review: cochrane handbook for systematic reviews for interventions, Version 5.1.0. Res Syn Meth. 2011; 2: 126–130.
The Joanna Briggs Institute. Checklist for Quasi-Experimental Studies. 2020. https://jbi.global/sites/default/files/2020-08/Checklist_for_Quasi-Experimental_Appraisal_Tool.pdf.
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Narrative synthesis in systematic reviews: a product from the ESRC methods programme. ESRC Methods Program. 2006;1:1–69.
Katz-Leurer M, Carmeli E, Shochina M. The effect of early aerobic training on independence six months post stroke. Clin rehabil. 2003;17(7):735–41.
Obembe AO, Eng JJ. Rehabilitation interventions for improving social participation after stroke: a systematic review and meta-analysis. Neurorehabil Neural Repair. 2016;30(4):384–92.
Zhang Q, Schwade M, Smith Y, Wood R, Young L. Exercise-based interventions for post-stroke social participation: a systematic review and network meta-analysis. Int J Nurs Stud. 2020;111:103738.
Song C-S, Lee O-N, Woo H-S. Cognitive strategy on upper extremity function for stroke: a randomized controlled trials. Restor Neurol Neuros. 2019;37(1):61–70.
Legg LA, Lewis SR, Schofield-Robinson OJ, Drummond A, Langhorne P. Occupational therapy for adults with problems in activities of daily living after stroke. Cochrane Database Syst Rev. 2017;19(7):CD003585.
Escher AA, Amlani AM, Viani AM, Berger S. Occupational therapy in an Intensive Comprehensive Aphasia Program: performance and satisfaction outcomes. Am J Occup Ther. 2018;72(3):7203205110p1–p7.
Zhou X, Du MX, Hu Y. The effect of self-management programs on post-stroke social participation: a systematic review and meta-analysis. Clin Rehabil. 2022;36(9):1141–52.
Clark E, MacCrosain A, Ward NS, Jones F. The key features and role of peer support within group self-management interventions for stroke? A systematic review. Disabil Rehabil. 2020;42(3):307–16.
Mayo NE, Anderson S, Barclay R, Cameron JI, Desrosiers J, Eng JJ, et al. Getting on with the rest of your life following stroke: a randomized trial of a complex intervention aimed at enhancing life participation post stroke. Clin Rehabil. 2015;29(12):1198–211.
Tooley EM, Kolahi A. Motivating behavioral change. Med Clin North Am. 2022;106(4):627–39.
Pike C, Kritzinger A, Pillay B. Social participation in working-age adults with aphasia: an updated systematic review. Top Stroke Rehabil. 2017;24(8):627–39.
Tse T, Douglas J, Lentin P, Carey L. Measuring participation after stroke: a review of frequently used tools. Arch Phys Med Rehabil. 2013;94(1):177–92.
Fallahpour M, Jonsson H, Joghataei MT, Nasrabadi AN, Tham K. I am not living my life”: lived experience of participation in everyday occupations after stroke in Tehran. J Rehabil Med. 2013;45(6):528–34.
Huijbregts MPJ, Myers AM, Streiner D, Teasell R, Implementation. Process, and preliminary outcome evaluation of two community programs for persons with stroke and their Care Partners. Top Stroke Rehabil. 2008;15(5):503–20.
Amatya B, Lizama LEC, Elmalik A, Bastani A, Galea MP, Khan F. Multidimensional evaluation of changes in limb function following botulinum toxin injection in persons with stroke. NeuroRehabilitation. 2019;45(1):67–78.
Watson HA, Tribe RM, Shennan AH. The role of medical smartphone apps in clinical decision-support: a literature review. Artif Intell Med. 2019;100:101707.
Acknowledgements
We are grateful to Kaiqiang Sun for polishing the manuscript.
Funding
This work was supported by National Natural Science Foundation of China [82202816] and Fudan University Fosun Care and Scientific Research Fund [FNF202118].
Author information
Authors and Affiliations
Contributions
Xuan Zhou: Conceptualization, Methodology, Data Curation, Writing Original Draft, Writing - Review & Editing, Funding acquisition. Minxia Du: Conceptualization, Methodology, Data Curation. Xiaojie Dai: Conceptualization, Methodology. Shenghui Zhu: Visualization, Visualization. Lanshu Zhou: Supervision, Project administration, Data Curation, Writing - Review & Editing. Xuemei Li: Supervision, Project administration, Data Curation, Writing - Review & Editing. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
None.
Ethics approval and consent to participate
Not declared.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, X., Du, M., Dai, X. et al. Intervention patterns and preliminary effectiveness on Social Participation following stroke: a scoping review. BMC Neurol 23, 275 (2023). https://doi.org/10.1186/s12883-023-03250-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-023-03250-2