Abstract
Background
This study aimed to investigate the risk predictors for early neurological deterioration (END) in isolated acute pontine infarction without any causative artery stenosis.
Methods
In this retrospective study, patients with isolated acute pontine infarction within 72 h of symptom onset were enrolled between October 2017 and December 2021. END was defined as an increase in the National Institutes of Health Stroke Scale (NIHSS) score ≥ 2 points within the first week postadmission. Patients were divided into the END and the non-END groups. Multiple logistic regression analysis was used to evaluate independent predictors of END in patients with isolated acute pontine infarction.
Results
A total of 153 patients were included in the final study (62 females; mean age, 67.27 ± 11.35 years), of whom 28.7% (47 of 153) experienced END. Multiple logistic regression analyses showed that infarct volume (adjusted odds ratio [aOR], 1.003; 95% CI, 1.001–1.005; P = 0.002) and basilar artery branch disease (aOR, 3.388; 95% CI, 1.102–10.417; P = 0.033) were associated with END. The combined ROC analysis of the infarct volume and basilar artery branch disease for predicting END showed that the sensitivity and specificity were 80.9% and 72.6%, respectively.
Conclusion
Basilar artery branch disease and infarct volume were associated with END in acute isolated pontine infarction and may be useful prognostic factors for neurological progression.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Early neurological deterioration (END) is relatively common in isolated acute pontine infarction (API), which is caused by small vessel disease or steno-occlusion of the orifice of a perforator at the parent artery. Based on previous studies, END in patients with isolated API has a high incidence of 25%–29% and is related to severe disability and poor outcomes [1,2,3]. However, the mechanism of END is currently unclear and may be related to hemodynamic factors, thrombus expansion, excitotoxicity and inflammation [4,5,6]
In previous studies [3, 7], END was reported to be related to the topographic location of the pontine infarction. However, another study showed that END was independent of the location and was not correlated with the size of the infarct [8]. Recently, the infarct size rather than topographic location of pontine infarction was suggested to be a possible predictor of END [9]. Similarly, these studies indicated that END was not related to severe stenosis of the basilar artery [3, 9, 10]. Therefore, the purpose of this study was to investigate the risk predictors for END in acute isolated pontine infarction without any causative artery stenosis.
Methods
This retrospective study was approved by the Medical and Health Research Ethics Committee of the Second People’s Hospital of Chengdu (Chengdu, China) and adhered to the Declaration of Helsinki. Because it was a retrospective study, informed consent was not needed, and all included patient information was anonymous.
Patient Selection
We retrospectively collected 153 patients with isolated API at Chengdu Second People's Hospital from October 2017 to December 2021. The inclusion criteria were as follows: (1) patients presenting within 72 h of onset; (2) diffusion-weighted imaging [DWI] within 48 h of admission showing isolated pontine infarction; and (3) patients with a modified Rankin scale (mRS) score ≤ 1 before admission. The exclusion criteria included (1) patients with pontine infarction with anterior circulation infarction or other vertebrobasilar infarction; (2) patients with vascular assessment (magnetic resonance angiography or computed tomography angiography) suggesting stenosis of the basilar artery (BA) (≥ 50%); (3) patients with cardiogenic embolism; (4) patients with severe cardiopulmonary, liver, or kidney insufficiency combined with malignant tumors; (5) patients with incomplete magnetic resonance imaging or poor imaging quality; and (6) patients with incomplete clinical data.
Data collection
Demographic features and conventional risk factors
Two clinicians reviewed the electronic medical record system at Chengdu Second People’s Hospital to collect information, and a data extraction form was designed to record the patient information. Basic information included age, sex, hypertension, diabetes, smoking, drinking, and history of stroke, and the clinical data included time from onset to arrival, blood pressure at admission, baseline blood glucose level, National Institutes of Health Stroke Scale (NIHSS) score at admission, presence of END, NIHSS score at discharge, infarct site, treatment and hospital days. The following risk factors were evaluated: 1) hypertension: repeated blood pressure readings of ≥ 140/90 mmHg, a history of previous hypertension or use of antihypertensive drugs; 2) diabetes: a history of diabetes or the use of diabetes medications, or more than two measurements of fasting plasma glucose levels > 7.0 mmol/L or a random plasma glucose level > 11.1 mmol/L; 3) smoking: ≥ 10 cigarettes per day; and 4) drinking: alcohol consumption > 2 U/d [11]. Baseline examinations included routine laboratory tests, such as creatinine, alanine aminotransferase (ALT), aspartate aminotransferase (AST), triglycerides, total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), brain MRI, and computed tomography angiography (CTA)/magnetic resonance angiography (MRA) of the head.
Brain mri protocol and analysis
MRI was performed within 48 h of admission using a Siemens 1.5 T/3.0 T MRI scanner (Siemens AG, Munich, Germany). We recorded the location of the pontine infarct lesion, the volume, the diameter and width of the largest slice, and the distance of the lesion from the midline of the pons. The pons was divided into 3 sections based on the rostrocaudal location of the lesion by diffusion-weighted imaging (DWI; upper, middle, or lower pons) [3, 7]. The upper pons is characterized by a relatively round shape with a small, round-shaped aqueduct (Fig. 1A); the middle pons is characterized by its square-shaped fourth ventricle, large middle cerebellar peduncles, and silhouettes of trigeminal nerves (Fig. 1B); and the lower pons is characterized by a shape similar to that of the middle pons but with images of facial/acoustic nerves and grooves rather than trigeminal nerves (Fig. 1C). If more than one adjacent lesion was involved, the primary affected lesion was considered for grouping purposes. The diameter and width of the largest slice of each infarction were measured on DWI scans. We chose the diameter multiplied by the width of the largest infarction slice multiplied by the number of infarct slices multiplied by the slice thickness and then divided by two as the infarct volume (Fig. 1D). MRI scans were obtained at a 5-mm slice thickness.
Stroke subtypes and END definition
This retrospective study included patients withy 2 types of stroke: (1) basilar artery branch disease (BABD) characterized by an infarct that reached or approached the pontine surface without BA stenosis [12,13,14] (Fig. 2A) and (2) small artery disease (SAD) indicated by a deeper infarct without involvement of the ventral surface in the absence of BA stenosis [15] (Fig. 2B). END was defined as an increase in the NIHSS score ≥ 2 points within the first week after admission [13, 16].
Statistical analysis
We used SPSS version 25.0 software (IBM Corp, Armonk, NY, USA) for statistical analysis. Continuous variables are expressed as the mean ± standard deviation (SD) or as the median and interquartile range (IQR). Differences between groups were compared using a t test or the rank-sum test. Categorical data are presented as frequencies (percentages), and the differences between groups were compared using the chi-squared test or Fisher’s exact test. Variables in univariate analyses (P < 0.10) were included in multivariate analysis. Receiver operating characteristic (ROC) analysis was used to assess the diagnostic value of our parameters for predicting END. Statistical significance was set at P < 0.05.
Results
Baseline characteristics
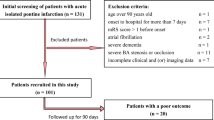
A total of 202 patients with acute pontine infarctions were admitted to our neurology department from October 2017 to December 2021; 41 patients met the exclusion criteria, and eight patients had missing information. Finally, 153 patients with acute isolated pontine infarctions were included in the final study (91 males and 62 females; mean age, 67.27 ± 11.35 years)(Fig. 3). END occurred in 28.7% (47 of 153) of them after admission. The NIHSS score at discharge (P < 0.001) and number of hospital days (P = 0.007) were significantly higher in the END group than in the non-END group (Table 1).
There were no significant differences in sex, age, hypertension, diabetes, drinking, smoking, baseline blood glucose level, history of ischemic stroke, blood pressure at admission, laboratory results, initial NIHSS score, or treatment after admission between the 2 groups (P > 0.05; Table 1).
Of the 153 patients, 86 patients (56.2%) had BABD, and 67 patients (43.8%) had SAD. The proportion of patients with END within one week after admission was 44.2% (38 of 86) in the BABD group and 13.4% (9 of 67) in the SVD group.
DWI indicated that upper pontine infarcts were significantly less common in the patients with END (4.3%, 2 of 47) than in the patients without END (24.5%, 26 of 106) (P = 0.003). Lower pontine infarcts were significantly more common with END than without END (63.8% vs. 42.5%, P = 0.015). Middle pontine infarctions were not significantly different between the two groups (P = 0.0659). Patients in the END group had a greater infarct diameter (P < 0.001) and width (P < 0.001) than those in the non-END group. The infarct volume was higher in patients with END than in patients without END (P < 0.001). There were no significant differences in the distance of the lesion from the midline of the pons in the two groups (p > 0.05) (Table 2).
When the factors associated with END in univariate analyses (P < 0.10) were entered into multivariate logistic regression analysis (adjusted for arrival time, HDL, creatinine, stroke subtype, topographic location, infarct volume, and the distance of the lesion from the midline of the pons), the results showed that infarct volume (aOR, 1.003; 95% CI, 1.001–1.005; P = 0.002) and BABD (aOR, 3.388; 95% CI, 1.102–10.417; P = 0.033) were associated with END (Table 3).
END symptoms mainly include alterations in facial movements (4.2%, 2 of 47), motor function (arm) (76.6%, 36 of 47), motor function (leg) (87.2%, 41of 47), sensations (2.1%,1of 47), and language ability (19.1%, 9 of 47) (Table 4).
The combined diagnostic value of the infarct volume and BABD was a sensitivity of 80.9%, a specificity of 72.6%, and an AUC of 0.774 (95% CI, 0.698–0.850, P < 0.05) (Fig. 4).
Discussion
In our study, markers predicting END in patients with acute isolated pontine infarction were evaluated, and infarct volume and subtype-BABD were found to be associated with END in API patients. Our study suggested that patients with BABD, especially those with a larger infarct volume, may be have higher risk of END.
Penetrating arterial infarction, particularly pontine infarction, tends to progress to END, in contrast to cerebral deep penetrating artery infarction [1, 17]. Our study showed that 28.7% of the patients with isolated pontine infarction experienced END after admission, consistent with previous research findings reporting an incidence of 27%–29% of END in patients with API [1, 18]. In 1989, Caplan initially proposed the concept of BAD and BA branch disease (BABD), which was defined as lesions extending to the ventral pontine surface in the blood supply region of the paramedian pontine artery with neither evidence of large arterial stenosis (> 50%) or occlusion nor evidence of cardiogenic embolism [19, 20]. A large retrospective study showed that BABD was the most common cause of API [15], accounting for 56.2% (86 of 153) of the patients with API included in our study, and Yamamoto et al. showed a relative frequency of approximately 40% [21]. In our study, END was significantly more frequent in patient with BABD than SAD (P < 0.0001), indicating that the BABD subtype was associated with END in patients with API, consistent with the study by Gokcal et al. [10]. However, Our study did not compare long-term outcomes between patients with BABD and SVD. Erro et al. [22] indicated that patients with BABD have a worse prognosis than patients with lacunar pontine infarctions.
Our data show that the deterioration of symptoms was related to the maximum infarct volume (P = 0.002). Recently, a retrospective study that included 407 patients with API by Haiyan Li et al. [9] also found that infarct size might be a predictor for neurological progression with isolated acute pontine infarction (aOR 4.580, P < 0.0001), which was different from our study in which the infarct size was represented by the maximal data of the ventrodorsal length multiplied by rostrocaudal thickness. However, Multiple logistic regression results showed that the OR of BABD was much higher than the OR of infarct volume in our study,So We speculated that subtype-BABD has a greater impact on the occurrence of END. Interestingly, another study [8] suggested that END was not related to the size of either infarct; however, its sample size was relatively small (n = 38), the expansion of ischemic lesions was not correlated with END, and the actual lesion size was not measured.
According to Huang et al. [7] and Oh et al. [3], lower pons lesions may be associated with a higher probability of progressive motor deficits in patients with isolated acute pontine infarction than those in the upper and middle pons. In our study, END was only numerically higher in patients with lower pontine infarction, but the difference in multiple logistic regression results was not statistically significant, which consistent with the conclusions reported by Gokcal et al. [10]. There were also studies reported by Li et al. [3] and Nakase et al. [8] showed that the deterioration of symptoms was not related to lower pons lesions (P > 0.05) [8]. In addition, our study quantitatively analyzed the relationship between the distance between the lesion and the midline of the pons and END, and the results exceeded our expectations and were negative, consistent with the findings reported by Oh et al. [3], who qualitatively divided the patients into groups with paramedian pontine infarcts and extended pontine infarcts according to the axial lesion location.
In analyzing the relationships between END and the infarct location and size in patients with API from an anatomical perspective, the corticospinal tracts exhibit a scattered distribution along the corticospinal fibers in the upper pons, located in the dorsolateral part of the pontine base at the level of the upper pons, and then converge into the anteromedial surface of the upper medulla to form compact bundles [23, 24]. Therefore, Huang et al. [7] and Oh et al. [3] proposed that the increased density of the corticospinal tracts in the lower pontine region, typically in the paramedian ventral area, results in greater damage to the corticospinal tracts. Infarcts in the lower pons lesions could damage more corticospinal tracts and are prone to END. Unfortunately, Our study only found that END was only numerically higher in patients with lower pontine infarction. The anatomic view also considers corticobulbar tracts in the upper areas of the pons to be more widespread than in the lower areas of the pons and they are located most medially [25]. Therefore, the infarct size might reflect the degree of damage to the conduction tract to the greatest extent. Patients with larger infarct volumes may have more damage to corticospinal tracts and corticobulbar tracts. Damage to the conduction tract is more serious in patients with END than in those without END. We hope that more high-quality studies will be designed to study the effects of the infarct site and infarct size on END in the future.
Previous BAD-related studies have shown that early intravenous thrombolysis does not prevent the occurrence of END [13, 26, 27]. Strategies to prevent the occurrence of END are currently an important topic. Several recent studies indicated that early intensive antiplatelet or anticoagulation therapy may reduce the risk of END and improve the clinical prognosis of patients [11, 28,29,30,31]. The study by Liu et al. with a small sample size (n = 17) showed that early administration of tirofiban after intravenous thrombolysis with urokinase reduced the incidence of END within 3 days from onset in patients with BAD (P = 0.004) [31]. Recently, our observational study showed that short-term application of dual antiplatelet therapy plus argatroban seemed safe and effective at preventing END in patients with BAD [11]. Whether this reinforced anti-embolization strategy is effective in patients with API at high risk of END needs to be confirmed.
This study has the following limitations. First, it was a single-center retrospective study with a modest sample size. Second, repeat MRI was not performed after deterioration to determine whether there was infarct volume expansion in END patients and to identify the cause of the neurological deterioration. Third, our study did not compare the long-term functional outcomes of the two groups of patients.
Conclusion
Our results indicate that the stroke subtype BABD and the larger infarct volume,which have more damage to conduction tract, are associated with END in patients with isolated API and may be useful prognostic factors for neurological progression.. Therefore, when treating patients with BABD, particularly patients with larger infarct volume, physicians must be aware of the risk of END.
Availability of data and materials
All original data can be obtained via email correspondence to 694,421,243@qq.com, and all charts in this study are presented in the article.
Abbreviations
- API:
-
Acute pontine infarction
- END:
-
Early neurological deterioration
- NIHSS:
-
National institutes of health stroke scale
- BABD:
-
Basilar artery branch disease
- ALT:
-
Aminotransferase
- AST:
-
Aspartate aminotransferase
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
- CTA:
-
Computed tomography angiography
- MRA:
-
Magnetic resonance angiography
- DWI:
-
Diffusion-weighted imaging
- SAD:
-
Small artery disease
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- ROC:
-
Receiver operating characteristic
References
Yamamoto Y, Ohara T, Hamanaka M, Hosomi A, Tamura A, Akiguchi I, Ozasa K. Predictive factors for progressive motor deficits in penetrating artery infarctions in two different arterial territories. J Neurol Sci. 2010;288(1–2):170–4.
Steinke W, Ley SC. Lacunar stroke is the major cause of progressive motor deficits. Stroke. 2002;33(6):1510–6.
Oh S, Bang OY, Chung CS, Lee KH, Chang WH, Kim GM. Topographic location of acute pontine infarction is associated with the development of progressive motor deficits. Stroke. 2012;43(3):708–13.
Serena J, Leira R, Castillo J, Pumar JM, Castellanos M, Dávalos A. Neurological deterioration in acute lacunar infarctions: the role of excitatory and inhibitory neurotransmitters. Stroke. 2001;32(5):1154–61.
Castellanos FX, Tannock R. Neuroscience of attention-deficit/hyperactivity disorder: the search for endophenotypes. Nat Rev Neurosci. 2002;3(8):617–28.
Terasawa Y, Iguchi Y, Kimura K, Kobayashi K, Aoki J, Matsumoto N, Shibazaki K, Inoue T, Kaji R. Neurological deterioration in small vessel disease may be associated with increase of infarct volume. J Neurol Sci. 2008;269(1–2):35–40.
Huang R, Zhang X, Chen W, Lin J, Chai Z, Yi X. Stroke Subtypes and Topographic Locations Associated with Neurological Deterioration in Acute Isolated Pontine Infarction. J Stroke Cerebrovasc Dis. 2016;25(1):206–13.
Nakase T, Sasaki M, Ikeda Y, Suzuki A. Progressing small vessel pontine infarction includes different etiologies. Ann Clin Transl Neurol. 2014;1(2):75–9.
Li H, Dai Y, Wu H, Luo L, Wei L, Zhou L, Lin Y, Wang Q, Lu Z. Predictors of Early Neurologic Deterioration in Acute Pontine Infarction. Stroke. 2020;51(2):637–40.
Gokcal E, Niftaliyev E, Baran G, Deniz C, Asil T. Progressive deficit in isolated pontine infarction: the association with etiological subtype, lesion topography and outcome. Acta Neurol Belg. 2017;117(3):649–54.
Xu J, Xu X, Wang H, He L, Liu Q, Du Y, Wang J. Dual Antiplatelet Therapy Plus Argatroban Prevents Early Neurological Deterioration in Branch Atherosclerosis Disease. Stroke. 2022;53(1):19–20.
Yamamoto Y, Ohara T, Hamanaka M, Hosomi A, Tamura A, Akiguchi I. Characteristics of intracranial branch atheromatous disease and its association with progressive motor deficits. J Neurol Sci. 2011;304(1–2):78–82.
Park MG, Oh EH, Kim BK, Park KP. Intravenous tissue plasminogen activator in acute branch atheromatous disease: Does it prevent early neurological deterioration? J Clin Neurosci. 2016;33:194–7.
Petrone L, Nannoni S, Del Bene A, Palumbo V, Inzitari D. Branch Atheromatous Disease: A Clinically Meaningful. Yet Unproven Concept Cerebrovasc Dis. 2016;41(1–2):87–95.
Kumral E, Bayulkem G, Evyapan D. Clinical spectrum of pontine infarction. Clinical-MRI correlations J Neurol. 2002;249(12):1659–70.
Jang SH, Park SW, Kwon DH, Park H, Sohn SI, Hong JH. The Length of an Infarcted Lesion Along the Perforating Artery Predicts Neurological Deterioration in Single Subcortical Infarction Without Any Relevant Artery Stenosis. Front Neurol. 2020;11: 553326.
Nakase T, Yoshioka S, Sasaki M, Suzuki A. Clinical evaluation of lacunar infarction and branch atheromatous disease. J Stroke Cerebrovasc Dis. 2013;22(4):406–12.
Kim JS, Cho KH, Kang DW, Kwon SU, Suh DC. Basilar artery atherosclerotic disease is related to subacute lesion volume increase in pontine base infarction. Acta Neurol Scand. 2009;120(2):88–93.
Men X, Li J, Zhang B, Zhang L, Li H, Lu Z. Homocysteine and C-reactive protein associated with progression and prognosis of intracranial branch atheromatous disease. PLoS ONE. 2013;8(9): e73030.
Nakase T, Yamamoto Y, Takagi M. Japan Branch Atheromatous Disease Registry Collaborators: The impact of diagnosing branch atheromatous disease for predicting prognosis. J Stroke Cerebrovasc Dis. 2015;24(10):2423–8.
Ohara T, Yamamoto Y, Tamura A, Ishii R, Murai T. The infarct location predicts progressive motor deficits in patients with acute lacunar infarction in the lenticulostriate artery territory. J Neurol Sci. 2010;293(1–2):87–91.
Erro ME, Gallego J, Herrera M, Bermejo B. Isolated pontine infarcts: etiopathogenic mechanisms. Eur J Neurol. 2005;12(12):984–8.
Yu C, Zhu C, Zhang Y, Chen H, Qin W, Wang M, Li K. A longitudinal diffusion tensor imaging study on Wallerian degeneration of corticospinal tract after motor pathway stroke. Neuroimage. 2009;47(2):451–8.
Li JB, Cheng RD, Zhou L, Wen WS, Zhu GY, Tian L, Ye XM. What drives progressive motor deficits in patients with acute pontine infarction? Neural Regen Res. 2015;10(3):501–4.
Kim JS, Lee JH, Im JH, Lee MC. Syndromes of pontine base infarction. A clinical-radiological correlation study Stroke. 1995;26(6):950–5.
Deguchi I, Hayashi T, Kato Y, Nagoya H, Ohe Y, Fukuoka T, Maruyama H, Horiuchi Y, Tanahashi N. Treatment outcomes of tissue plasminogen activator infusion for branch atheromatous disease. J Stroke Cerebrovasc Dis. 2013;22(7):e168-172.
Vynckier J, Maamari B, Grunder L, Goeldlin MB, Meinel TR, Kaesmacher J, Hakim A, Arnold M, Gralla J, Seiffge DJ, et al. Early Neurologic Deterioration in Lacunar Stroke: Clinical and Imaging Predictors and Association With Long-term Outcome. Neurology. 2021;10.1212
Kimura T, Tucker A, Sugimura T, Seki T, Fukuda S, Takeuchi S, Miyata S, Fujita T, Hashizume A, Izumi N, et al. Ultra-Early Combination Antiplatelet Therapy with Cilostazol for the Prevention of Branch Atheromatous Disease: A Multicenter Prospective Study. Cerebrovasc Dis Extra. 2016;6(3):84–95.
Berberich A, Schneider C, Reiff T, Gumbinger C, Ringleb PA. Dual Antiplatelet Therapy Improves Functional Outcome in Patients With Progressive Lacunar Strokes. Stroke. 2019;50(4):1007–9.
Wang PF, Sun ZR, Yu JC, Geng N, Liu LY, Zhu LN, Li J, Yuan HC, Zhao GC, Li ZG. Early argatroban and antiplatelet combination therapy in acute non-lacunar single subcortical infarct associated with mild intracranial atherosclerosis. BMC Neurol. 2021;21(1):440.
Liu B, Zhang H, Wang R, Qu H, Sun Y, Zhang W, Zhang S. Early administration of tirofiban after urokinase-mediated intravenous thrombolysis reduces early neurological deterioration in patients with branch atheromatous disease. J Int Med Res. 2020;48(5):300060520926298.
Acknowledgements
We sincerely thank all patients and medical staff who participated in this study for their contributions.
Funding
This work was funded by the Chengdu Science and Technology Bureau, which focuses on the research and development support plan (2019-YF09-00097-SN).
Author information
Authors and Affiliations
Contributions
Y-LL was involved in the entire process of the study, including designing the study, collecting data, analyzing the data, and drafting the original manuscript. H-MP participated in data collection, data analysis and form making, and Y-X participated in data management and statistical analysis. L-YH and J-W revised the manuscript. F-X designed the study and revised the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We obtained ethical approval for this study from the Medical and Health Research Ethics Committee of the Second People’s Hospital of Chengdu. Because it was a retrospective study, the Medical and Health Research Ethics Committee of the Second People’s Hospital of Chengdu waived the requirement for informed consent and information obtained from all included patients was anonymous.
Consent for publication
Not applicable.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, Y., Peng, H., Wang, J. et al. Risk factors for early neurological deterioration in acute isolated pontine infarction without any causative artery stenosis. BMC Neurol 22, 332 (2022). https://doi.org/10.1186/s12883-022-02861-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-022-02861-5