Abstract
Background and purpose
This study assessed the predictive factors for symptomatic intracranial hemorrhage (sICH) in patients with acute ischemic stroke (AIS) after receiving intravenous thrombolysis (IVT) within 6 h in northern China.
Methods
We retrospectively analyzed ischemic stroke patients who were treated with IVT between November 2016 and December 2018 in 19 hospitals in Shandong Province, China. Potential predictors of sICH were investigated using univariate and multivariate analyses.
Results
Of the 1293 enrolled patients (845 men, aged 62 ± 11 years), 33 (2.6%) developed sICH. The patients with sICH had increased coronary heart disease (36.4% vs. 13.7%, P = 0.001), more severe stroke (mean National Institutes of Health Stroke Scale [NIHSS] score on admission of 14 vs.7, P < 0.001), longer door-to-needle time [DNT] (66 min vs. 50 min, P < 0.001), higher blood glucose on admission, higher white blood cell counts (9000/mm3 vs. 7950/mm3, P = 0.004) and higher neutrophils ratios (73.4% vs. 67.2%, P = 0.006) et al. According to the results of multivariate analysis, the frequency of sICH was independently associated with the NIHSS score (OR = 3.38; 95%CI [1.50–7.63]; P = 0.003), DNT (OR = 4.52; 95%CI [1.69–12.12]; P = 0.003), and white blood cell count (OR = 3.59; 95%CI [1.50–8.61]; P = 0.004).
When these three predictive factors were aggregated, compared with participants without any factors, the multi-adjusted odds ratios (95% confidence intervals) of sICH for persons concurrently having one, two or three of these factors were 2.28 (0.25–20.74), 15.37 (1.96–120.90) and 29.05 (3.13–270.11), respectively (P for linear trend < 0.001), compared with participants without any factors.
Conclusion
NIHSS scores higher than 10 on admission, a DNT > 50 min, and a white blood cell count ≥9000/mm3 were independent risk factors for sICH in Chinese patients within 6 h after IVT for AIS.
Similar content being viewed by others
Introduction
Intravenous thrombolysis (IVT) treatment is an effective therapy for acute ischemic stroke (AIS), which includes providing recombinant tissue plasminogen activator (rt-PA) to patients within 4.5 h [1] and urokinase (UK) within 6 h in China [2]. However, symptomatic intracranial hemorrhage (sICH) is one of the most feared complications after thrombolytic therapy [3, 4], and is associated with neurological deterioration and poor outcome. Thus, identifying the predictors of sICH in patients receiving IVT is crucial.
SICH has been defined slightly differently among previous studies; the incidence rate of sICH varies between 2.0 and 7.2% worldwide [5,6,7,8], and the incidence of sICH in Asia is higher [9] or equivalent [8] to that in Western countries, according to mSITS-MOST (the modified version of Safe Implementation of Thrombolysis in Stroke-Monitoring Study) criteria. Different factors, such as a higher National Institutes of Health Stroke Scale (NIHSS) score, advanced age, elevated serum glucose levels and cardioembolism, have been suggested as predictors of sICH after IVT within 4.5 h of AIS in China (TIMS-China) study [5].
Given that UK is much cheaper and may have an apparent longer therapeutic time window than rt-PA, Chinese guidelines recommend UK for use within 6 h of the onset of AIS as an alternative to rt-PA [10]. However, to our knowledge, the incidence and predictors of sICH in the Chinese patients with AIS treated with rt-PA or UK within 6 h remain unclear, and it is worthwhile to explore the risk factors for sICH based on multicenter retrospective study data in northern China. In summary, identifying the risk factors for sICH has important practical significance for communicating with patients and their relatives and taking efficacious measures to prevent sICH.
Materials and methods
Study design
We retrospectively analyzed ischemic stroke patients who received IVT, including rt-PA and urokinase, within 6 h of stroke onset at 19 hospitals in Shandong Province, China, between November 2016 and December 2018. Inclusion and exclusion criteria for IVT were mainly adopted from the National Institute of Neurological Disorders and Stroke protocol and the protocol of the Chinese Guidelines for the Management of Stroke. Patients treated with endovascular treatment after IVT, patients with known tumors, inflammation, treatment administration > 6 h after symptom onset, no follow-up brain imaging after treatment administration and unavailable blood samples were excluded from this study. The selection of different thrombolytic doses and treatment strategies was completely determined by the institution or the treating physician and was not standardized. We assessed stroke severity by the baseline NIHSS score, and the presumed cause of ischemic stroke with the international Trial of ORG 10172 in Acute Stroke Treatment (TOAST) classification [11]. All TOAST classification assignments were further verified by an experienced senior neurologist (Jifeng Li).
Data on patient demographics, clinical characteristics and the use of thrombolysis medications were collected from patients’ charts by neurologists from the participating hospitals. Potential risk factors included age, sex, hypertension, diabetes mellitus, dyslipidemia, coronary heart disease, atrial fibrillation, door-to-needle time (DNT) (minutes), Onset-to-needle time (ONT) (minutes), NIHSS scores on admission, systolic blood pressure before thrombolysis, diastolic blood pressure before thrombolysis, smoking status, alcohol consumption, blood glucose on admission, antiplatelet treatment pre-IVT, anticoagulant treatment pre-IVT, serum white blood cell (WBC) count, neutrophil-WBC ratio (neutrophil ratio), platelet count, low-density lipoprotein cholesterol (LDL-C) level on admission, rt-PA dose (mg/kg body weight), urokinase dose (million units), and stroke subtype.
The study was approved by the Ethical Standards Committee on Human Experimentation at Shandong Provincial Hospital Affiliated to Shandong First Medical University. A signed consent form was obtained from all participants. The study was conducted in accordance with the principles for medical research involving human subjects expressed in the Declaration of Helsinki.
Outcome measures
The primary outcome was the incidence of symptomatic intracranial hemorrhage (sICH) between 0 and 36 h after IVT. SICH was based on parenchymal hemorrhage with deterioration using the National Institutes of Health Stroke Scale score of ≥4 points or death (the modified Safe Implementation of Thrombolysis in Stroke- Monitoring Study [mSITS-MOST]) [12].
1.3 Statistical analysis
For categorical variables, the chi-square (χ2) test or Fisher’s exact test was presented as percentages. For continuous variables, the t-test or the Mann–Whitney U-test was presented as the means ± SD or median (interquartile range). Variables with P < 0.05 in the univariate analysis were entered into the multivariate logistic regression analysis. Receiver operating characteristic curve analysis was performed for continuous variables with statistical significance in the logistic regression analysis to analyze the predictability of sICH. A multiple logistic regression model was used to estimate the odds ratios (ORs) and 95% confidence intervals (CIs) of sICH associated with individual risk factors and their load, which was assessed by counting the number of risk factors that were significantly related to an increased odds ratio of sICH (P < 0.05). We reported the results from two models: Model 1 was unadjusted, and Model 2 was adjusted for coronary heart disease, neutrophil ratio, and stroke subtype. A two-sided p value of < 0.05 was considered statistically significant. All analyses were performed with the SPSS 22.0 software.
Results
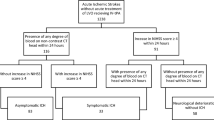
From November 2016 to December 2018, 1541 patients with AIS from 19 hospitals participated in this retrospective study. Among them, 22 patients who received IVT > 6 h after stroke onset were excluded, 56 patients who did not undergo follow-up brain CT after recanalization were excluded, and another 2 patients were excluded because of a lack of rt-PA dose record data. Furthermore, 168 patients who received endovascular treatment were also excluded. Thus, a total of 1293 patients with onset-to-needle time < 6 h met our study criteria. Among them, 33 (2.6%) experienced mSITS-MOST-defined sICH.
The demographic and baseline characteristics of the patients with sICH are summarized in Table 1. Compared with patients without sICH, sICH patients had more severe stroke (defined by higher NIHSS scores) on admission, longer DNT, increased history of coronary heart disease, higher blood glucose on admission, higher neutrophil ratio and white blood cell counts, higher rt-PA doses (0.9 mg/kg vs. 0.6 mg/kg or 50 mg/person), and increased rates of cardioembolism.
Fisher’s exact test: atrial fibrillation, coronary heart disease, diabetes mellitus, dyslipidemia, use of thrombolysis medications, dose of rt-PA, dose of urokinase, and stroke subtype.
We categorized the data into 2 categories based on the standard cut-points or previous studies. According to univariable analysis, the parameters selected for further multivariable analysis (P < 0.05) were: DNT > 50 min, prior coronary heart disease, baseline NIHSS scores > 10, neutrophil ratio prior to thrombolysis ≥71.2%, white blood cell count prior to thrombolysis ≥9000/mm3, and stroke subtype (Table 2).
Independent factors associated with sICH were analyzed using the multivariate logistic regression. The highest odds ratios were DNT >50 min (vs. ≤ 50) (OR, 4.52; 95% CI, 1.69–12.12; P = 0.003), the NIHSS scores on admission > 10 (vs. ≤ 10) (OR, 3.38; 95% CI, 1.50–7.63; P = 0.003), and white blood cell count ≥9000/mm3 (OR, 3.59; 95% CI, 1.50–8.61; P = 0.004) (Table 3).
When these three predictive factors were aggregated, the multi- adjusted OR (95% confidence interval) of having sICH was increased significantly with an increasing number of concurrent predictive factors (P for linear trend < 0.001) (Table 4).
Discussion
In this multicenter retrospective study, we observed that sICH occurred in 2.6% of patients by the mSITS-MOST definition in our research, which is comparable to incidence reported in the TIMS-China trial (2.0%) [5]. However, patients who received only intravenous rt-PA within 4.5 h of AIS onset were recruited for the TIMS-China trial. Furthermore, our report showed that higher NIHSS score, higher white blood cell count on admission, and delayed recanalization treatment were independently associated with sICH after IVT. Our study seems to be the first multicenter retrospective study conducted in northern China to investigate the predictors of sICH with AIS patients treated with rt-PA or UK within 6 h, which may better reflect real-world practices.
Compared with patients without sICH, sICH patients had higher blood glucose on admission in our research (mean 9.1 versus 8.3 mmol/L, P = 0.045) (Table 1). In addition, we found no statistical association between admission blood glucose and increasing the risk of sICH post IVT according to mSITS- MOST criteria (OR = 1.938; P = 0.124) (Table 2), a finding reported in prior studies [13, 14]. However, in previous studies [5, 15], elevated baseline glucose level was shown to be a risk factor for sICH in acute ischemic stroke patients treated with IV rt-PA, in which the sICH was diagnosed based on the European Cooperative Acute Stroke Study II (ECASS-II) definition. Certainly, the mechanism behind this phenomenon requires further research.
High white blood cell (WBC) counts are known to be involved in the inflammatory process of AIS [16]. A study by Tiainen et al. reported that higher WBC counts at admission were significantly associated with sICH in AIS patients treated with IVT [17], and similar findings were obtained in our research. In contrast, another study indicated that elevated WBC counts failed to independently predict sICH [18]. In our research, the best predictor of sICH was the WBC count in blood tests, and a value ≥9000/mm3 indicated a 3.6-fold increased risk for sICH. The different results of previous studies may have been caused by the different times of blood sampling due to the dynamic changes in WBC counts after stroke [19]. The mechanism behind the association between elevated WBC counts and sICH is not completely understood, which may be partly because AIS causes WBCs to migrate into the brain, where they can cause brain edema and injury by initiating inflammatory cascade reactions and releasing inflammatory cytokines [20].
Among the clinical risk factors, DNT and NIHSS scores were independently associated with sICH in our study, and these results are consistent with those of previous studies [5, 13]. The elapsed time from hospital admission to the thrombolytic bolus was defined as door-to-needle time (DNT). The benefit of IVT for patients with AIS is time-dependent. The clinical benefit from IVT declines rapidly (time is brain), and every minute counts [21]. In our report, DNT turned out to be the most reliable predictor of sICH among the other parameters assessed, which revealed that patients with a DNT > 50 min had a 4.5-times higher risk of developing sICH than those with a DNT ≤ 50 min, and the difference was statistically significant (P = 0.003) when adjusted for multivariate analysis.
The National Institutes of Health Stroke Scale (NIHSS) score is a tool used to objectively quantify stroke impairment of the stroke and is the most commonly used stroke outcome scale [22]. Higher NIHSS scores are generally associated with the more severe ischemic stroke, which is reflected by large areas of injured blood vessels that are prone to bleeding after IVT. In our research, a higher initial NIHSS score on admission increased the risk of sICH, which was similar to the findings of previous reports [23, 24]. We found that patients with NIHSS scores > 10 had a 3.4-times higher risk of sICH (using NIHSS scores ≤10 as reference). If a patient that had an acute stroke and receiving IVT has an NIHSS score > 10, the physician must be cautious and should check the patient’s white blood cell count. It is worth noting that the NIHSS-assessed stroke severity was milder in the current study than in previous studies, which may explain why the sICH incidence (2.6%) was lower than that in previous reports [6, 7].
A linear relationship showing that an increasing number of concurrent multiple risk factors is associated with an increased likelihood of having sICH was found. These findings suggest that increased monitoring is needed in order to reduce the risk of sICH after IVT for AIS patients in northern China.
Our study was conducted at multicenter hospitals, which including secondary hospitals and tertiary hospitals, and this is the greatest advantage of this study. Considering the research hospitals were located in rural and urban areas in northern China, care should be taken in comparing these results with those of previous studies because regional and racial characteristics may act as sources of bias.
This study has some limitations. First, as a retrospective study, the data may have generated system biases. Involved centers may have followed different protocols for IVT. Second,pretreatment Alberta Stroke Program Early CT Score (ASPECTS), hyperdense middle cerebral artery signs and other important parameters that may influence the risk of sICH, were not assessed in the present study. Third, the sample size was relatively small, and the obtained findings should be verified in future studies with larger samples.
Conclusions
We explored the independent predictive factors as for the risk of sICH within 6 h after IVT in northern China. Patients with the following 3 predictive factors should be closely monitored: an NIHSS score on admission higher than 10, a DNT > 50 min, and a white blood cell count ≥9000/mm3.
Availability of data and materials
All relevant data are within the manuscript. The dataset generated and analyzed in the current study is not publicly available due to privacy constraints relating to the ethical approval and informed consent signed by the participants. Data sharing was not stated in the informed consent signed by the participants.
References
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early Management of Patients with Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46–e110. https://doi.org/10.1161/str.0000000000000158.
Yuan Z, Wang B, Li F, Wang J, Zhi J, Luo E, et al. Intravenous thrombolysis guided by a telemedicine consultation system for acute ischaemic stroke patients in China: the protocol of a multicentre historically controlled study. BMJ Open. 2015;5(5):e006704. https://doi.org/10.1136/bmjopen-2014-006704.
Strbian D, Sairanen T, Meretoja A, Pitkäniemi J, Putaala J, Salonen O, et al. Patient outcomes from symptomatic intracerebral hemorrhage after stroke thrombolysis. Neurology. 2011;77(4):341–8. https://doi.org/10.1212/WNL.0b013e3182267b8c.
Lee RS, Ok YC, Lim JS, Lim BC, Cho KY, Lee MC. Outcome evaluation of intravenous infusion of urokinase for acute ischemic stroke. Chonnam Med J. 2012;48(1):52–6. https://doi.org/10.4068/cmj.2012.48.1.52.
Liu M, Pan Y, Zhou L, Wang Y. Predictors of post-thrombolysis symptomatic intracranial hemorrhage in Chinese patients with acute ischemic stroke. PLoS One. 2017;12(9):e0184646. https://doi.org/10.1371/journal.pone.0184646.
Yaghi S, Boehme AK, Dibu J, Leon Guerrero CR, Ali S, Martin-Schild S, et al. Treatment and outcome of thrombolysis-related hemorrhage: a multicenter retrospective study. JAMA Neurol. 2015;72(12):1451–7. https://doi.org/10.1001/jamaneurol.2015.2371.
Sung SF, Chen SC, Lin HJ, Chen YW, Tseng MC, Chen CH. Comparison of risk-scoring systems in predicting symptomatic intracerebral hemorrhage after intravenous thrombolysis. Stroke. 2013;44(6):1561–6. https://doi.org/10.1161/strokeaha.111.000651.
Xu X, Wang D, Wang F, Norton C, Liu X, Selim M. The risk of hemorrhagic transformation after thrombolysis for acute ischemic stroke in Chinese versus north Americans: a comparative study. J Stroke Cerebrovasc Dis. 2018;27(9):2381–7. https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.04.027.
Mehta RH, Cox M, Smith EE, Xian Y, Bhatt DL, Fonarow GC, et al. Race/ethnic differences in the risk of hemorrhagic complications among patients with ischemic stroke receiving thrombolytic therapy. Stroke. 2014;45(8):2263–9. https://doi.org/10.1161/strokeaha.114.005019.
Dong Q, Dong Y, Liu L, Xu A, Zhang Y, Zheng H, et al. The Chinese Stroke Association scientific statement: intravenous thrombolysis in acute ischaemic stroke. Stroke Vasc Neurol. 2017;2(3):147–59. https://doi.org/10.1136/svn-2017-000074.
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of org 10172 in acute stroke treatment. Stroke. 1993;24(1):35–41. https://doi.org/10.1161/01.str.24.1.35.
Wahlgren N, Ahmed N, Dávalos A, Ford GA, Grond M, Hacke W, et al. Thrombolysis with alteplase for acute ischaemic stroke in the safe implementation of thrombolysis in stroke-monitoring study (SITS-MOST): an observational study. Lancet. 2007;369(9558):275–82. https://doi.org/10.1016/s0140-6736(07)60149-4.
Lokeskrawee T, Muengtaweepongsa S, Patumanond J, Tiamkao S, Thamangraksat T, Phankhian P, et al. Prognostic parameters for symptomatic intracranial hemorrhage after intravenous thrombolysis in acute ischemic stroke in an Asian population. Curr Neurovasc Res. 2017;14(2):169–76. https://doi.org/10.2174/1567202614666170327163905.
Kamal H, Mehta BK, Ahmed MK, Kavak KS, Zha A, Lail NS, et al. Laboratory factors associated with symptomatic hemorrhagic conversion of acute stroke after systemic thrombolysis. J Neurol Sci. 2021;420:117265. https://doi.org/10.1016/j.jns.2020.117265.
Guo H, Xu W, Zhang X, Zhang S, Dai Z, Li S, et al. A Nomogram to predict symptomatic intracranial hemorrhage after intravenous thrombolysis in Chinese patients. Neuropsychiatr Dis Treat. 2021;17:2183–90. https://doi.org/10.2147/ndt.S320574.
Kim JY, Park J, Chang JY, Kim SH, Lee JE. Inflammation after ischemic stroke: the role of leukocytes and glial cells. Exp Neurobiol. 2016;25(5):241–51. https://doi.org/10.5607/en.2016.25.5.241.
Tiainen M, Meretoja A, Strbian D, Suvanto J, Curtze S, Lindsberg PJ, et al. Body temperature, blood infection parameters, and outcome of thrombolysis-treated ischemic stroke patients. Int J Stroke. 2013;8(8):632–8. https://doi.org/10.1111/ijs.12039.
Maestrini I, Strbian D, Gautier S, Haapaniemi E, Moulin S, Sairanen T, et al. Higher neutrophil counts before thrombolysis for cerebral ischemia predict worse outcomes. Neurology. 2015;85(16):1408–16. https://doi.org/10.1212/wnl.0000000000002029.
Emsley HC, Smith CJ, Gavin CM, Georgiou RF, Vail A, Barberan EM, et al. An early and sustained peripheral inflammatory response in acute ischaemic stroke: relationships with infection and atherosclerosis. J Neuroimmunol. 2003;139(1–2):93–101. https://doi.org/10.1016/s0165-5728(03)00134-6.
Ye L, Cai R, Yang M, Qian J, Hong Z. Reduction of the systemic inflammatory induced by acute cerebral infarction through ultra-early thrombolytic therapy. Exp Ther Med. 2015;10(4):1493–8. https://doi.org/10.3892/etm.2015.2672.
Kruyt ND, Nederkoorn PJ, Dennis M, Leys D, Ringleb PA, Rudd AG, et al. Door-to-needle time and the proportion of patients receiving intravenous thrombolysis in acute ischemic stroke: uniform interpretation and reporting. Stroke. 2013;44(11):3249–53. https://doi.org/10.1161/strokeaha.113.001885.
Kasner SE. Clinical interpretation and use of stroke scales. Lancet Neurol. 2006;5(7):603–12. https://doi.org/10.1016/s1474-4422(06)70495-1.
Weimar C, König IR, Kraywinkel K, Ziegler A, Diener HC. Age and National Institutes of Health stroke scale score within 6 hours after onset are accurate predictors of outcome after cerebral ischemia: development and external validation of prognostic models. Stroke. 2004;35(1):158–62. https://doi.org/10.1161/01.Str.0000106761.94985.8b.
Hao Y, Yang D, Wang H, Zi W, Zhang M, Geng Y, et al. Predictors for symptomatic intracranial hemorrhage after endovascular treatment of acute ischemic stroke. Stroke. 2017;48(5):1203–9. https://doi.org/10.1161/strokeaha.116.016368.
Acknowledgements
The authors wished to thank all the study participants, coordinators of the 19 participating hospitals.
Funding
This work was supported by the grants from Department of Science and Technology of Shandong Province (grants no. 2016GSF201068). Yuan Xue received grants from the Natural Science Foundation of Shandong Province (grant no. ZR2021MH010).
Author information
Authors and Affiliations
Contributions
Yuan Xue and Shan Li wrote the main manuscript text, Yuanyuan Xiang, Ziran Wang, Fengyun Wang, Yuanying Yu, Peng Yan and Xiaohui Liu collected data and followed up, Qinjian Sun prepared Tables 1, 2, 3 and 4, Yifeng Du collated data, Jifeng Li designed the project. All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Committee of the Shandong Provincial Hospital Affiliated to Shandong First Medical University approved the study protocol. Written informed consent was obtained from all participants, and the study was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xue, Y., Li, S., Xiang, Y. et al. Predictors for symptomatic intracranial hemorrhage after intravenous thrombolysis with acute ischemic stroke within 6 h in northern China: a multicenter, retrospective study. BMC Neurol 22, 6 (2022). https://doi.org/10.1186/s12883-021-02534-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-021-02534-9