Abstract
Background
Pneumonia is related to poor prognosis in acute ischemic stroke (AIS), and its risk might be higher in atrial fibrillation (AF) related AIS with elevated plasma D-dimer. The aim of our study was to investigate the prognostic value of D-dimer for predicting clinical outcome of AF-related AIS with pneumonia.
Method
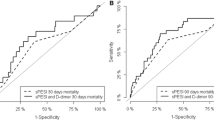
AF-related AIS patients with pneumonia were prospectively enrolled. Receiver operating characteristic (ROC) curve was used to determine the optimal D-dimer point for 3-month mortality and death/severe disability. The associations between the D-dimer and 3-month mortality and death/severe disability were assessed by multivariable logistic regression analysis.
Results
A total of 415 patients were enrolled in this study. ROC curve analysis showed that the optimal cut point of D-dimer for 3-month death/severe disability and mortality were D-dimer≥2.35 mg/l and D-dimer≥3.35 mg/l, respectively. Multivariable logistic regression analysis showed that D-dimer≥2.35 mg/l [adjusted odds ratio (aOR) 5.99, 95% confidence interval (CI): 3.04–11.83, P<0.001], higher NIHISS score (aOR:1.53, 95% CI: 1.38–1.69, P<0.001) and larger infarct volume (aOR 1.01, 95% CI: 1.01–1.02, P<0.001) were associated with increased risk of 3-month death/severe disability), and anticoagulant was associated with decreased risk of death/severe disability (aOR:0.21, 95% CI: 0.09–0.47, P<0.001). Higher NIHISS score (aOR:1.64, 95% CI: 1.38–1.94, P<0.001), older age (aOR 1.08, 95% CI: 1.02–1.14, P = 0.007), D-dimer≥3.35 mg/l (OR 8.49, 95% CI: 4.13–17.84,P<0.001), larger infarct volume (aOR 1.02, 95% CI: 1.00–1.03, P = 0.014), and higher CRUB-65 score (aOR 6.43, 95% CI: 3.10–13.34, P<0.001) were associated with increased risk of 3-month mortality.
Conclusions
AF-related AIS patients with concurrent high D-dimer and pneumonia increased risk of 3-month mortality and death/severe disability, plasma D-dimer may have predictive value in outcome after AF-related AIS with pneumonia.
Similar content being viewed by others
Background
Atrial fibrillation (AF) is the most common arrhythmia, which associated with increased risk of mortality and disability after stroke. The large infarcts characteristically associated with AF reflect the larger size of stasis thrombi that form in the low shear environment of the left atrium [1, 2]. 30-day mortality of AF-related stroke was more than 24%, another 35% patients had severe disability [3,4,5].
D-dimer is a protein produced by the degradation of cross-linked fibrin by factor XIII. It is used as a screening tool for venous thromboembolism, but its role in other pathologies has not been fully elucidated [6]. AF leads to decreased flow in the left atrial appendage and the atrium, which combine with platelet activation and endothelial dysfunction, increase coagulation activity and lead to stroke. Studies had showed that patients with AF could increase D-dimer levels [7,8,9], and higher D-dimer levels could increase risk of future cerebrovascular and cardiovascular events [10,11,12], increased D-dimer levels had been reported to be proportional to the severity of stroke. In addition, pneumonia leads to fibrin deposition in the alveoli and interstitial lungs, inducing activation of the intravascular and extravascular coagulation systems [13]. D-dimer may reflect the effect of infection on coagulation. Some studies had reported that elevated D-dimer levels in pneumonia patients might indicate hypercoagulability and increase the risk of thrombosis [14,15,16]. Pneumonia is the most common complication of AIS, which could lead to poor clinical outcomes and increase mortality, previous study had showed a significant correlation between D-dimer levels and pneumonia severity, and higher D-dimer levels in patients with pneumonia could identify individuals at increased risk for in-hospital death [17]. Studies had showed that elevated D-Dimer was associated with major complications during hospitalization in patients with pneumonia [18, 19].
The predictive value of D-dimer in clinical outcome among AF-related AIS with pneumonia has not been elucidated. Therefore, in the present study, we investigated the prognostic value of D-dimer for predicting clinical outcome of AF-related AIS with pneumonia.
Methods
Study population
This study was a multicenter prospective study conducted in three medical centers: Nanchong Central Hospital of the Second Clinical Medical School, North Sichuan Medical College, the Chengdu second people’s hospital, and affiliated Hospital of North Sichuan Medical College. Patients with AF-related AIS were admitted within 7 days to the stroke ward between July 2015 and March 2019. AIS is defined as sudden loss of neurological function with symptoms lasting for more than 24 h. Brain CT scan was normal or acute ischemic changes, diffusion-weighted imaging showed acute ischemic changes. TOAST classification was used for determining stroke subtype. AF-relate stroke was confirmed by an experienced neurologist who blinded to the study. The severity of stroke was assessed using the National Institutes of Health Stroke Scale (NIHSS) [20].
Pneumonia was diagnosed based on clinical history and symptoms (cough, fever, purulent secretions), and laboratory parameters of respiratory tract infection, and was confirmed by chest CT.
Only patients who met all the following criteria were included in the study: 1. First new-onset AF-related AIS within 7 days. 2. AIS was consistent with clinical manifestations. 3. Patients had pneumonia within 7 days after stroke. 4. Patients have electrocardiogram-confirmed AF within the prior 6 months. All patients received standard treatment, including anticoagulant treatment or antiplatelet treatment, lipid-lowering treatment, and rehabilitation. Exclusion criteria: 1. Cerebral hemorrhage; 2. Renal failure (glomerular filtration rate < 30 ml/min.1.73m2); 3. Active malignancies; 4. Aortic dissection.5. Presence of thrombus in the left atrium/appendage.
Data collection
Plasma D-dimer levels were measured with an enzyme-linked fluorescent immunoassay method (Lituo Biotechnology Co. Ltd., Hunan, China) in all patients on admission. Other laboratory data on admission [white blood cells, hemoglobin, liver function, kidney function, LDL-cholesterol, serum glucose, glycated hemoglobin, brain natriuretic peptide, and procalcitonin (PCT)] were performed. Body temperature was checked at least three times a day. In case of suspect clinical infection, chest CT, PCT, blood and sputum cultivations were rechecked. The severity of pneumonia was assessed using CRUB-65 score within 48 h after pneumonia. The CURB-65 index uses five core clinical features: new onset confusion, urea > 7 mmol/l, respiratory rate 30 breaths/min, systolic blood pressure [21]. Infarct volume was manually calculated by radiologist using hand tracing method in terms of brain CT.
All patients were followed up for 3 months. Clinical outcome was defined as 3-month mortality (include the in-hospital mortality) and death/ severe disability (scores 3–5 on the modified Rankin Scale [mRS]) after AF related AIS, good outcome was defined as mRS ≤ 2 [22].
Statistical analysis
All patients were divided death/severe disability and good outcome groups, and then, patients were classified into death and survivor groups. To identify differences between subgroups, the Pearson χ2 test was used for categorical variables. Distributions of continuous variables were determined by the Kolmogorov–Smirnov test, while Mann–Whitney two sample test was applied in case of non-normal distributions. Receiver operating characteristic (ROC) curve analysis was used to evaluate sensitivity, specificity and to determine the optimal cut point of D-dimer for 3-month mortality and death/ severe disability. We then performed logistic regressions analyses to determine the association between D-dimer and 3-month mortality and death/ severe disability. Results were expressed as adjusted odds ratios (aOR) with the corresponding 95% confidence interval (CI). SPSS 22.0 statistical software was used for data analyses. P < 0.05 was used as a significance level.
Results
Patient characteristics
415 AF-related AIS patients with pneumonia were included in the study, 211 patients were female (52.45%) and 184 patients were male (47.55%), with an average age of 67.62 ± 9.84 years old (ranging from 40 to 93 years old), median NIHSS score was 11(7–14), medians international standard ratio (INR) was 1.36(1.09–1.95). 19.76% (82) patients were treated with anticoagulation, medians D-dimer value was 1.9 mg/l (1.2–3.0 mg/l). There were 123(29.64%) cases of diabetes, 265(63.86%) cases of hypertension, 278 (66.99%) cases of hyperlipidemia, 126(30.36%) cases of smoking and 147(35.42%) cases of drinking. During 3 months of follow-up, 50 (12.05%)patients had died (17 patients had died during hospitalization), 178 (42.89%) patients had severe disability (Table 1).
Factors related to death/severe disability
228 (228/415,54.94%) patients had death/severe disability after 3 months of follow-up. The patients with death/severe disability had older age (68.68 ± 9.63 vs 66.32 ± 9.97,P = 0.005), higher NIHSS score [13(10–16) vs 7(5–11), P<0.001], higher D-dimer levels [2.50(1.60–3.88) vs 1.30(0.80–2.00), P<0.001], larger infarct volume [81(50–127) vs 51(29–76), P<0.001], and higher CRUB-65 score [2(1–3) vs 2(1–2), P = 0.005], lower percentage of anticoagulant (9.21% vs 32.62%, P<0.001) than those who good outcome (Table 1).
ROC curve showed that D-dimer predict death/ severe disability with AUC of 0.78 (95%CI 0.73 to 0.82). The optimal cut point off D-dimer for death/ severe disability was D-dimer≥2.35 mg/l. Using D-dimer ≥2.35 mg/l to predict death/severe disability, the sensitivity was 55.70%, the specificity was 83.96%, positive predictive value was 80.89%; and negative predictive value was 60.85%.
In the multivariate logistic regression model, after adjusting for all the confounding factors (Model 1), higher NIHISS score, higher D-dimer value and larger infarction volume were associated with increased risk of 3-month death/severe disability (aOR:1.50, 95% CI: 1.36–1.67, P<0.001; aOR 2.29, 95% CI: 1.70–3.08, P<0.001; aOR 1.01, 95% CI: 1.01–1.02, P<0.001;respectively),and anticoagulant was associated with decreased risk of 3-month death/severe disability (aOR:0.22, 95% CI: 0.10–0.49, P<0.001); when D-dimer≥2.35 mg/l was entered into multivariate logistic regression (Model 2), higher NIHISS score, D-dimer≥2.35 mg/l and larger infarction volume were associated with increased risk of 3-month death/severe disability (aOR:1.53, 95% CI: 1.38–1.69, P<0.001; aOR 5.99, 95% CI: 3.04–11.83, P<0.001; aOR 1.01, 95% CI: 1.01–1.02, P<0.001respectively) (Table 2),and anticoagulant was associated with decreased risk of death/severe disability (aOR:0.21, 95% CI: 0.09–0.47, P<0.001) (Table 2), the CURB-65 score was not associated with the risk of death/severe disability(P ≥ 0.05).
Factors related to death
After 3 months of follow-up, 50 (98/387,25.32%) patients died. The patients who died had older age (71.49 ± 10.27 vs 67.09 ± 9.68, P = 0.005), higher NIHSS score[18(14–20) vs 10(7–13), P < 0.001], higher D-dimer levels [3.85(1.98–4.65) vs 1.80(1.10–2.70),P < 0.001], larger infarct volume [118(68–135) vs 61(34–102), P<0.001], and higher CRUB-65 score [3(2–3) vs 2(1–2), P < 0.001] than those who stayed alive(Table 3).
17 patients died during hospitalization, the patients who died during hospitalization had higher NIHSS score[19(13–21) vs 10(7–14), P < 0.001], higher D-dimer levels [3.40(1.90–4.40) vs 1.85(1.18–2.93),P = 0.002],and higher CRUB-65 score [3 (2–3) vs 2(1–2),P < 0.001] than those non- in-hospital death group.
ROC curve showed high accuracy for D-dimer predict 3-month mortality with AUC of 0.76(95%CI 0.69 to 0.84). The optimal cut point of D-dimer for 3-month mortality was D-dimer≥3.35 mg/l. Using a cutoff point of D-dimer≥3.35 mg/l to predict 3-month mortality, the specificity was 84.93%, positive predictive value was 35.29%; and negative predictive value was 93.94%.
In the multivariate logistic regression model, after adjusting for all the confounding factors (Model 1), higher NIHISS score, higher age, higher D-dimer value, larger infarct volume, and higher CURB-65 score were independently associated with increased risk of 3-month mortality (aOR:1.58, 95% CI: 1.35–1.86, P<0.001; aOR 1.07, 95% CI: 1.01–1.13, P = 0.016; aOR 170, 95% CI: 1.27–2.28, P < 0.001; aOR 1.01, 95% CI: 1.00–1.03, P = 0.020; aOR 6.36, 95% CI: 3.19–12.71, P < 0.001,respectively); when D-dimer≥3.35 mg/l was entered into multivariate logistic regression (Model 2), higher NIHISS score, higher age, D-dimer≥3.35 mg/l, larger infarct volume, and higher CURB-65 score were independently associated with increased risk of 3-month mortality (aOR:1.64, 95% CI: 1. .38–1.94, P<0.001; aOR 1.08, 95% CI: 1.02–1.14, P = 0.007; aOR 8.49, 95% CI: 4.13–17.84, P < 0.001; aOR 1.02, 95% CI: 1.00–1.03, P = 0.014; aOR 6.43, 95% CI: 3.10–13.34, P < 0.001, respectively) (Table 4).
In the multivariate logistic regression model, after adjusting for all the confounding factors, higher NIHSS and higher CURB-65 were independently associated with increased risk of in-hospital mortality (aOR 1.55, 95% CI: 1.27–1.90, P < 0.001; aOR 3.73, 95% CI: 1.53–9.11, P < 0.001, respectively);
Discussion
AF is the most prevalent sustained cardiac rhythm disorder seen in clinical practice. AF is linked to a 5-fold increased risk of cerebrovascular events, and approximately 20% of strokes are related to AF.AF-related strokes impart worse prognosis than those occurring in the absence of AF. The 30-day mortality of AF-related stroke was 24%, another 35% of patients were unable to live independently [2, 4]. In this study, we found that the 3-month mortality was 12.05%, the remaining 365 survivors, severe disability rates were 48.76% (178/365). The mortality and disability rate in this study were lower than those reported in previous studies, which may be due to most of the patients from the level of first-class comprehensive hospital, medical conditions are relatively good. We identified risk factors associated with outcome in AF-related stroke patients with pneumonia, the results showed that the patients with death/severe disability had older age, higher NIHSS score, higher D-dimer levels, larger infarct volume than those with good outcome.
D-dimer is a specific cross-linked fibrin degradation product, it is a sensitive biomarker for indicating coagulation and fibrinolytic activation, which remains stable over time in the absence of any adverse events [23]. D-dimer levels are commonly used to screen for pulmonary embolism and aortic dissection [6, 8]. Previous studies had showed that the level of D-dimer increased after AIS, which might be related to stroke subtype and stroke volume, and significantly increased in cardiogenic embolic ischemic stroke [24, 25]. In recent years, some studies had showed that D-dimer levels could be a valuable and independent short-term prognostic marker for acute stroke [26]. In AF-related AIS patients with pneumonia, the prognostic value of D-dimer levels remains unclear. In our study, we found D-dimer level was significantly elevated (2.24 ± 1.54 mg/l), we have obtained the correlation between D-dimer levels and outcome, the optimal cut point off D-dimer for 3-month death/severe disability and mortality was D-dimer≥2.35 mg/l and ≥ 3.35 mg/l, respectively, after adjusting for fully confounders, we found a significant association of D-dimer≥2.35 mg/l and D-dimer≥3.35 mg/l with increased risks of 3-month death/severe disability and mortality after AF-related AIS with pneumonia. From our results, we could confirm that D-dimer was a valuable prognostic marker of functional outcome and death among AF-related AIS with pneumonia.
The mechanism of the relationship between D-dimer levels and the prognosis of AF-related AIS patients with pneumonia remains unclear. D-dimer levels may reflect ongoing thrombus formation within cerebral vessels or may be a marker of systemic hypercoagulability [27]. The mechanism of high D-dimer levels affected the prognosis of ischemic stroke might be the activation of inflammation through D-dimer. D-dimer can activate monocytes to secrete pro-inflammatory cytokines such as interleukin-6 (IL-6) [28], which play an important role in endothelial dysfunction, atherosclerosis and promotion of hypercoagulability [29, 30]. Elevated D-dimer levels may reflect ongoing cerebrovascular thrombosis by inducing the inflammatory process and may also be a marker of systemic hypercoagulation leading to poor prognosis in patients with acute ischemic stroke [31]. In addition, studies had showed that compared with patients with lacunar stroke or without arterial occlusion, patients with left ventricular venous thrombosis had a higher increased D-dimer levels at the early stage of the disease. Therefore, high D-dimer levels might be a sensitive indicator of poor prognosis, especially in patients with left ventricular venous thrombosis [32]. In addition, Atrial fibrillation is a rapid and uncoordinated atrial activity that results in ineffective atrial contraction, causing blood turbulence in the left atrium and systemically. In fact, compared with laminar or pulsating flowing [33], the loss of shear stress in turbulent conditions is associated with decreased expression of endothelial nitric oxide synthase (eNOS), in addition, patients with atrial fibrillation have a higher degree of systemic inflammation. According to this hypothesis, circulating inflammatory mediators such as TNF-α and IL-18, which are closely associated with endothelial dysfunction and cardiovascular disease [33,34,35], may induce vascular injury, aggravate the burden of atherosclerosis, and lead to higher cardiovascular morbidity and mortality, as seen in AF subjects [36]. Atrial fibrillation may lead to vascular endothelial dysfunction, on the other hand immunosuppression [37], inhalation of oral secretions, or dysphagia after stroke could increase the risk of pulmonary infection. When patients are in the pulmonary infection state, fibrin deposition in the alveolar compartment enhances the inflammatory response, increases blood flow and vascular permeability, increases neutrophils recruitment and inflammatory mediator production [38]. The synergistic effect of activated inflammation and activated coagulation may lead to adverse outcomes [39]. Thus, D-dimer may represent the biological activation of inflammatory, hemostatic, and fibrinolytic systems.
In our this study, the cut-off value of D-dimer used for predicting death/severe disability was D ≥ 2.35 mg/l, the sensitivity was 55.70%, the specificity was 83.96%, positive predictive value was 80.89%; and negative predictive value was 60.85%. Using a cut-off point of D-dimer≥3.35 mg/l for predicting 3-month mortality, the sensitivity was 60.0%, the specificity was 84.93%, positive predictive value was 35.29%; and negative predictive value was 93.94%. As shown above, poor sensitivity was observed when D-dimer≥3.35 mg/l used for predicting death.
Some limitations of this study are worth considering. First, in this study, we relied on a single baseline D-dimer levels, so we were unable to investigate the association between dynamic changes D-dimer levels and clinical outcomes among AF-related AIS with infection. D-dimer levels should be measured repeatedly for longitudinal analysis, which may provide additional information about development and its prognostic impact. Second, we did not collect the patients’ MRS at discharge, the functional status of the patients at discharge may also affect mortality. Third, left atrial appendage (LAA) is an important source of thrombi in patients with AF, but we lack data of left atrial. Fourth, due to contraindications, some patients were treated with platelet aggregation instead of anticoagulant after stroke, and we did not further analyze these patients, which might have an impact on the study results. The strength of our study was that it was related to the large number of patients, moreover, it was a multicenter clinical prospective observational study with robust and of high clinical relevance results.
Conclusion
In conclusion, our study showed a positive correlation between increased D-dimer level and unfavorable outcome after AF-related AIS with infection. Our findings substantiated the importance of an early diagnosis of elevated D-dimer in AF-related stroke survivors with infection given the elevated risk of unfavorable outcome. D-dimer levels may have potential predictive value in risk stratification of ischemic stroke.
Availability of data and materials
Data used in this study may be available by request to corresponding author via email: 2399548051@qq.com
Abbreviations
- AF:
-
Atrial fibrillation
- AIS:
-
Acute ischemic stroke
- ROC:
-
Receiver operating characteristic
- aOR:
-
adjusted odds ratio
- NIHSS:
-
National Institutes of Health Stroke Scale
- TOAST:
-
Trial of Org 10,172 in Acute Stroke Treatment
- mRS:
-
modified Rankin Scale
- PCT:
-
Procalcitonin
- IQR:
-
Interquartile range
References
Hathcock JJ. Flow effects on coagulation and thrombosis. Arterioscler Thromb Vasc Biol. 2006;26(8):1729–37. https://doi.org/10.1161/01.ATV.0000229658.76797.30.
Li X, Sim MMS, Wood JP. Recent insights into the regulation of coagulation and thrombosis. Arterioscler Thromb Vasc Biol. 2020;40(5):e119–25. https://doi.org/10.1161/ATVBAHA.120.312674.
Alkhouli M, Alqahtani F, Aljohani S, Alvi M, Holmes DR. Burden of atrial fibrillation-associated ischemic stroke in the United States. JACC Clin Electrophysiol. 2018;4(5):618–25. https://doi.org/10.1016/j.jacep.2018.02.021.
Hylek EM, Go AS, Chang Y, Jensvold NG, Henault LE, Selby JV, et al. Effect of intensity of Oral anticoagulation on stroke severity and mortality in atrial fibrillation. N Engl J Med. 2003;349(11):1019–26. https://doi.org/10.1056/NEJMoa022913.
Ko D, Thigpen JL, Otis JA, Forster K, Henault L, Quinn E, et al. Influence of statin therapy at time of stroke onset on functional outcome among patients with atrial fibrillation. Int J Cardiol. 2017;15(227):808–12. https://doi.org/10.1016/j.ijcard.2016.10.055.
Bounameaux H, Cirafici P, de Moerloose P, Schneider PA, Slosman D, Reber G, et al. Measurement of Ddimer in plasma as diagnostic aid in suspected pulmonary embolism. Lancet. 1991;337(8735):196–200. https://doi.org/10.1016/0140-6736(91)92158-x.
Weymann A, Sabashnikov A, Ali-Hasan-Al-Saegh S. Cardiac Surgery and Cardiology-Group Imcsc-Group IMP. Predictive role of coagulation, fibrinolytic, and endothelial markers in patients with atrial fibrillation, stroke, and thromboembolism: a meta-analysis, metaregression, and systematic review. Med Sci Monit Basic Res. 2017;23:97–140. https://doi.org/10.12659/MSMBR.902558.
Sadanaga T, Mitamura H, Fukuda K, Ogawa S. D-dimer levels positively correlate with B-type natriuretic peptide levels in patients with atrial fibrillation. Int J Cardiol. 2012;158(1):110–1111. https://doi.org/10.1016/j.ijcard.2012.04.079.
Thulin Å, Lindbäck J, Granger CB, Wallentin L, Lind L, Siegbahn A. Extracellular vesicles in atrial fibrillation and stroke. Thromb Res. 2020;193:180–9. https://doi.org/10.1016/j.thromres.2020.07.029.
Hamatani Y, Nagai T, Nakai M, Nishimura K, Honda Y, Nakano H, et al. Anzai T; NaDEF investigators. Elevated plasma D-dimer level is associated with short-term risk of ischemic stroke in patients with acute heart failure. Stroke. 2018;49(7):1737–40. https://doi.org/10.1161/STROKEAHA.118.021899.
Albertsen IE, Rasmussen LH, Overvad TF, Graungaard T, Larsen TB, Lip GY. Risk of stroke or systemic embolism in atrial fibrillation patients treated with warfarin: a systematic review and meta-analysis. Stroke. 2013;44(5):1329–36. https://doi.org/10.1161/STROKEAHA.113.000883.
Ding WY, Gupta D, Lip GYH. Atrial fibrillation and the prothrombotic state: revisiting Virchow's triad in 2020. Heart. 2020;16: heartjnl-2020-316977. https://doi.org/10.1136/heartjnl-2020-316977.
G€unther A, Mosavi P, Heinemann S, Ruppert C, Muth H, Markart P, et al. Alveolar fibrin formation caused by enhanced procoagulant and depressed fibrinolytic capacities in severe pneumonia. Comparison with the acute respiratory distress syndrome. Am J Respir Crit Care Med. 2000;161(2 Pt 1):454–62. https://doi.org/10.1164/ajrccm.161.2.9712038.
Guo SC, Xu CW, Liu YQ, Wang JF, Zheng ZW. Changes in plasma levels of thrombomodulin and D-dimer in children with different types of mycoplasma pneumoniae pneumonia. Zhongguo Dang Dai Er Ke Za Zhi. 2013;15(8):619–22.
Inoue Arita Y, Akutsu K, Yamamoto T, Kawanaka H, Kitamura M, Murata H, et al. A fever in acute aortic dissection is caused by endogenous mediators that influence the extrinsic coagulation pathway and do not elevate Procalcitonin. Intern Med. 2016;55(14):1845–52. https://doi.org/10.2169/internalmedicine.55.5924.
Snijders D, Schoorl M, Schoorl M, Bartels PC, van der Werf TS, Boersma WG. D-dimer levels in assessing severity and clinical outcome in patients with community acquired pneumonia. A secondary analysis of a randomised clinical trial. Eur J Intern Med. 2012;23(5):436–41. https://doi.org/10.1016/j.ejim.2011.10.019.
Querol-Ribelles JM, Tenias JM, Grau E, Querol-Borras JM, Climent JL, Gomez E, et al. Plasma d-dimer levels correlate with outcomes in patients with community-acquired pneumonia. Chest. 2004;126(4):1087–92. https://doi.org/10.1378/chest.126.4.1087.
Chalmers JD, Singanayagam A, Scally C, Hill AT. Admission D-dimer can identify low-risk patients with community-acquired pneumonia. Ann Emerg Med. 2009;53(5):633–8. https://doi.org/10.1016/j.annemergmed.2008.12.022.
Snijders D, Schoorl M, Bartels PC, van der Werf TS, Boersma WG. D-dimer levels in assessing severity and clinical outcome in patients with community-acquired pneumonia. A secondary analysis of a randomised clinical trial. Eur J Intern Med. 2012;23(5):436–41. https://doi.org/10.1016/j.ejim.2011.10.019.
Anderson A, Klein J, White B, Bourgeois M, Leonard A, Pacino A, et al. Training and certifying users of the National Institutes of Health stroke scale. Stroke. 2020;51(3):990–3. https://doi.org/10.1161/STROKEAHA.119.027234.
Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58(5):377–82. https://doi.org/10.1136/thorax.58.5.377.
Quinn TJ, Dawson J, Walters MR, Lees KR. Functional outcome measures in contemporary stroke trials. Int J Stroke. 2009;4(3):200–5. https://doi.org/10.1111/j.1747-4949.2009.00271.x.
Tripodi A. D-dimer testing in laboratory practice. Clin Chem. 2011;57(9):1256–62. https://doi.org/10.1373/clinchem.2011.166249.
Koch HJ, Horn M, Bogdahn U, Ickenstein GW. The relationship between plasma D-dimer concentrations and acute ischemic stroke subtypes. J Stroke Cerebrovasc Dis. 2005;14(2):75–9. https://doi.org/10.1016/j.jstrokecerebrovasdis.2004.12.002.
Park YW, Koh EJ, Choi HY. Correlation between serum D-dimer level and volume in acute ischemic stroke. J Korean Neurosurg Soc. 2011;50(2):89–94. https://doi.org/10.3340/jkns.2011.50.2.89.
Yang XY, Gao S, Ding J, Chen Y, Zhou XS, Wang JE. Plasma D-dimer predicts short-term poor outcome after acute ischemic stroke. PLoS One. 2014;9(2):e89756. https://doi.org/10.1371/journal.pone.0089756.
Yuan W, Shi ZH. The relationship between plasma D-dimer levels and outcome of Chinese acute ischemic stroke patients in different stroke subtypes. J Neural Transm. 2014;121(4):409–13. https://doi.org/10.1007/s00702-013-1113-y.
Robson SC, Shephard EG, Kirsch RE. Fibrin degradation product D-dimer induces the synthesis and release of biologically active IL-1β, IL-6 and plasminogen activator inhibitors from monocytes in vitro. Br J Haematol. 1994;86(2):322–6. https://doi.org/10.1111/j.1365-2141.1994.tb04733.x.
Pwelsh MB, Langhorne P, Rumley A, Lowe GD, Stott DJ. Associations of inflammatory and haemostatic biomarkers with poor outcome in acute ischaemic stroke. Cerebrovasc Dis. 2009;27(3):247–53. https://doi.org/10.1159/000196823.
Barber M, Langhorne P, Rumley A, Lowe GD, Stott DJ. Hemostatic function and progressing ischemic stroke: D-dimer predicts early clinical progression. Stroke. 2004;35(6):1421–5. https://doi.org/10.1161/01.STR.0000126890.63512.41.
Skoloudík D, Bar M, Sanák D, Bardon P, Roubec M, Langová K, et al. D-dimers increase in acute ischemic stroke patients with the large artery occlusion, but do not depend on the time of artery recanalization. J Thromb Thrombolysis. 2010;29(4):477–82. https://doi.org/10.1007/s11239-009-0372-9.
Topper JN, Cai J, Falb D, Gimbrone MA Jr. Identification of vascular endothelial genes differentially responsive to fluid mechanical stimuli: cyclooxygenase-2, manganese superoxide dismutase, and endothelial cell nitric oxide synthase are selectively up-regulated by steady laminar shear stress. Proc Natl Acad Sci USA. 1996;93:10417–22. https://doi.org/10.1073/pnas.93.19.10417 PMID:8816815.
Zhang H, Park Y, Wu J, Chen X, Lee S, Yang J, et al. Role of TNF-alpha in vascular dysfunction. Clin Sci (Lond). 2009;116(3):219–30. https://doi.org/10.1042/CS20080196 PMID:19118493.
Elhage R. Hans-Gustaf Ljunggren, and Göran K. Hansson. Proatherogenic role of interleukin-18: effects on inflammation and action on vascular cells. Cardiovasc Res. 2012;96(2):176–80. https://doi.org/10.1093/cvr/cvs220.
Sokolic J, Tokmadzic VS, Knezevic D, Medved I, Vukelic Damjani N, Balen S, et al. Endothelial dysfunction mediated by interleukin-18 in patients with ischemic heart disease undergoing coronary artery bypass grafting surgery. Med Hypotheses. 2017;104:20–4. https://doi.org/10.1016/j.mehy.2017.05.009 PMID:28673582.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. and ESC Scientific Document Group. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37:2893–962. https://doi.org/10.1093/eurheartj/ehw210 PMID:27567408.
Chamorro Á, Meisel A, Planas AM, Urra X, van de Beek D, Veltkamp R. The immunology of acute stroke. Nat Rev Neurol. 2012;8(7):401–10. https://doi.org/10.1038/nrneurol.2012.98.
Abraham E. Coagulation abnormalities in acute lung injury and sepsis. Am J Respir Cell Mol Biol. 2000;22(4):401–4. https://doi.org/10.1165/ajrcmb.22.4.f184.
Csala M, Léránt I, Bánhegyi G, Kardon T, Puskás F, Mucha I, et al. Prostaglandin-independent stimulation ofinterleukin-6 production by fibrinogen degradation product D in perfusedmurine liver. Scand J Immunol. 1998;48(3):269–71. [PMID:9743211]. https://doi.org/10.1046/j.1365-3083.1998.00395.x.
Acknowledgments
We thank all patients and their families for generously consenting to use of human tissues in this research.
Funding
The study was supported by the youth innovation subject in medical research of Sichuan province (Q16004), which is not involved in the database management (collection, analysis, interpretation of data) and has no access to patient information. The funding body did not participate in designing the study or writing the manuscript. The study protocol has undergone peer-review process by the funding body.
Author information
Authors and Affiliations
Contributions
YX was responsible for the concept and design of the study, data collection and analysis and the first draft of the paper and further manuscript. LTL, QZL and MY were responsible for concept and design of the study, the data collection and interpretation. LPP was responsible for the data analysis. ZY was responsible for overseeing the concept and design of the study, the data analysis and interpretation. All authors read and approved the final manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We obtained ethical approval for this study from the Medical and Health Research Ethics Committee in Nanchong Central Hospital of the Second Clinical Medical School, North Sichuan Medical College, Second people’s Hospital of Chengdu, Affiliated Hospital of North Sichuan Medical College. The current study was carried out according to the Declaration of Helsinki. If the patient has consciousness disorder or aphasia, the decision cannot be made by themselves, the consent form can be signed by the patient’s legal proxies. Prior to enrollment, all patients or their legal proxies will be given detailed information about the aims, scope, and possible consequences of the trial by a physician. Written informed consent was obtained from all study participants or their legal proxies.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, X., Lu, T., Qu, Z. et al. Plasma D-dimer level is associated with clinical outcomes in patients with atrial fibrillation related acute ischemic stroke after pneumonia. BMC Neurol 21, 137 (2021). https://doi.org/10.1186/s12883-021-02168-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-021-02168-x