Abstract
Background
Although approximately 25% of Brazilians have private health coverage (PHC), studies on the surveillance of chronic kidney disease (CKD) in this population are scarce. The objective of this study was to estimate the prevalence of CKD in individuals under two PHC regimes in Brazil, who total 8,335,724 beneficiaries.
Methods
Outpatient serum creatinine and proteinuria results of individuals from all five regions of Brazil, ≥ 18 years of age, and performed between 10/01/2021 and 10/31/2022, were analyzed through the own laboratory network database. People with serum creatinine measurements were evaluated for the prevalence and staging of CKD, and those with simultaneous measurements of serum creatinine and proteinuria were evaluated for the risk category of the disease. CKD was classified according to current guidelines and was defined as a glomerular filtration rate (GFR) < 60 ml/min/1.73 m² estimated by the 2021 CKD-EPI equation.
Results
The number of adults with serum creatinine results was 1,508,766 (age 44.0 [IQR, 33.9–56.8] years, 62.3% female). The estimated prevalence of CKD was 3.8% (2.6%, 0.8%, 0.2% and 0.2% in CKD stages 3a, 3b, 4 and 5, respectively), and it was higher in males than females (4.0% vs. 3.7%, p < 0.001, respectively) and in older age groups (0.2% among 18-29-year-olds, 0.5% among 30-44-year-olds, 2.0% among 45-59-year-olds, 9.4% among 60-74-year-olds, and 32.4% among ≥ 75-year-olds, p < 0.001) Adults with simultaneous results of creatinine and proteinuria were 64,178 (age 57.0 [IQR, 44.8–67.3] years, 58.1% female). After adjusting for age and gender, 70.1% were in the low-risk category of CKD, 20.0% were in the moderate-risk category, 5.8% were in the high-risk category, and 4.1% were in the very high-risk category.
Conclusion
The estimated prevalence of CKD was 3.8%, and approximately 10% of the participants were in the categories of high or very high-risk of the disease. While almost 20% of beneficiaries with PHC had serum creatinine data, fewer than 1% underwent tests for proteinuria. This study was one of the largest ever conducted in Brazil and the first one to use the 2021 CKD-EPI equation to estimate the prevalence of CKD.
Similar content being viewed by others
Background
Chronic kidney disease (CKD) is a major global public health problem, as a common condition that is silent in its early stages, preventable, neglected in many places and costly for all health systems [1]. In developed countries, more than 10% of adults have some degree of CKD, and most of this prevalence is increasing [2]. The complications of CKD can be avoided or mitigated with adequate care, and screening and early treatment are cost-effective in the population at risk [3, 4]. Nations with universal health insurance coverage have 5–7% of their budgets consumed by kidney replacement therapy, which is the final phase of care for CKD [5]. Nevertheless, CKD is not a subject of the prioritized programs to combat chronic noncommunicable diseases (NCDs) in many countries, including Brazil [6]. Between 2008 and 2023, the expenditures of the Brazilian Unified Health System (SUS) on outpatient kidney replacement therapy increased from approximately 1.7 to 4.1 billion Brazilian reais (nearly 340 to 820 million US dollars) [7].
Only in theory does Brazil have clinical guidelines for comprehensive care of patients with CKD and specific ministerial ordinance for the operation of health services relevant to this care [8, 9]. In fact, national studies have shown several inadequacies in the early identification of CKD by primary health care and in the population’s access to consultations with a nephrologist and to CKD diagnosis and follow-up tests [10, 11]. Despite these gaps that are highly present in the Brazilian scenario, this country is one of the few places in the world with universal coverage for dialysis and kidney transplantation [12, 13]. Among the public health actions relevant to the secondary prevention of CKD, epidemiological surveillance stands out, especially given the asymptomatic nature of the early stages of this disease and that many of the traditional nephroprotective medications are low-cost and covered by SUS [14,15,16].
Brazil is a country with a dual health care system in which the public health care system coexists with private health care. Approximately 25% of the Brazilian population has PHC [17]. However, detailed information on programs to combat NCD or care for complex patients in private health care is scarce [18]. The objective of this study was to estimate the prevalence of CKD in individuals with PHC in Brazil.
Methods
Study design and population
This was a retrospective, cross-sectional study based on records of laboratory tests performed between 10/01/2021 and 10/31/2022 in the own laboratory network of two private health companies in Brazil. Together, these companies are national in scope and have a medical assistance portfolio consisting of approximately 8,335,724 beneficiaries [19]. Outpatient serum creatinine and proteinuria tests of individuals from all five regions of Brazil were analyzed. This country has 26 states, in addition to the federal district, and is divided into five large regions (Fig. 1). The exclusion criteria were tests from patients under 18 years of age and those performed in hospital and emergency settings.
The study adhered to the Declaration of Helsinki and Resolution 466/2012 of the Brazilian National Health Council and was approved by the research ethics committee on 11/01/2022 under number 64260622.1.0000.8098. The free and informed consent form was waived because the study was observational, retrospective, noninterventional and large, making it impossible to communicate with all participants. The extraction of information from the database of the laboratories occurred between 12/01/2022 and 04/13/2023.
Data source, variables, and definitions
Demographic data of the participants (age, gender and collection site) and results of serum creatinine and urinary protein were obtained from laboratory records. In case of patients with two or more measurements of a given test, the lowest value available was used, to avoid overestimation of the prevalence and severity of CKD.
The estimated glomerular filtration rate (GFR) was calculated from serum creatinine, age, and gender using the 2021 CKD-EPI equation [20]. This equation was chosen because it is the most current and it does not require information on ethnicity, as race correction is no longer recommended and because the Brazilian population is highly mixed. CKD was defined as GFR < 60 ml/min/1.73 m² and was classified into stages 3a (45–59 ml/min/1.73 m²), 3b (30–44 ml/min/1.73 m²), 4 (15–29 ml/min/1.73 m²), and 5 (< 15 ml/min/1.73 m²) [21]. All the participating laboratories performed the serum creatinine tests with standardized methods.Proteinuria was assessed categorically. It was present in the case of any of the following: isolated urine albumin/creatinine ratio (ACR) > 30 mg/g, 24-hour albuminuria > 30 mg/24 h, or 24-hour proteinuria > 150 mg/24 h. The categories were mild (ACR < 30 mg/g, albuminuria < 30 mg/24 h, or proteinuria < 150 mg/24 h), moderate (ACR 30–300 mg/g, albuminuria 30–300 mg/24 h, or proteinuria 150–500 mg/24 h), and severe (ACR > 300 mg/g, albuminuria > 300 mg/24 h, or proteinuria > 500 mg/24 h) [21].
The representativeness of the sample in the regions of Brazil was calculated as the proportion between the number of adults who underwent the evaluated tests and the number of beneficiaries within each region. According to the historical series, the annual amount of serum creatinine tests performed is approximately 2,500,000, but the number of proteinuria measurements is less than 100,000.
Therefore, patients with serum creatinine measurements were evaluated for the prevalence of CKD and its stages, and those with simultaneous serum creatinine and proteinuria measurements were evaluated regarding the risk of CKD. According to the CKD heat map of KDIGO 2012 Clinical Practice Guideline (Kidney Disease Improving Global Outcomes), patients were considered to be at low risk when they had GFR ≥ 60 ml/min/1.73 m² and mild proteinuria. They were at moderate risk when they had GFR ≥ 60 ml/min/1.73 m² and moderate proteinuria or GFR 45–59 ml/min/1.73 m² and mild proteinuria. Patients were in the high-risk category for CKD when they had any of the following combinations: GFR ≥ 60 ml/min/1.73 m² and severe proteinuria, GFR 45–59 ml/min/1.73 m² and moderate proteinuria, or GFR 30–44 ml/min/1.73 m² and mild proteinuria. They were at very high-risk when they had GFR 45–59 ml/min/1.73 m² and severe proteinuria, GFR 30–44 ml/min/1.73 m² and moderate or severe proteinuria, or GFR < 30 ml/min/1.73 m² regardless of the level of proteinuria [21].
Data analysis
Initially, the distribution of participants by demographic variables (gender, age group, and region of Brazil) and laboratory results (GFR and proteinuria) was evaluated, and their respective 95% confidence intervals were calculated. The distribution of patients in the different GFR ranges was assessed according to gender, age, and region of Brazil. The intergroup distribution was assessed using the χ² test. The crude prevalence of CKD by region of Brazil was estimated as the proportion of the number of people with abnormal tests out of the total number of people who underwent that test. A risk map (or heat map) of CKD was drawn by crossing the GFR information and the proteinuria categories. Finally, the prevalence rates were adjusted for age and gender using the direct method, with the total study population as a reference. Statistical analyses were conducted using R version 4.2.1 software.
Results
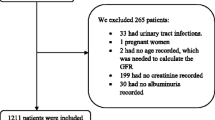
Between 1 October 2021 and 31 October 2022, 3,520,678 serum creatinine measurements were recorded. After excluding tests performed in hospitals or emergency rooms (1,137,104), tests performed in people under 18 years of age (211,200), and duplicate tests (663,608), 1,508,766 adults were included for the estimation of CKD prevalence and staging. Among them, 64,178 (4.3%) had results of both serum creatinine and proteinuria, so this was the number evaluated for the risk categories of CKD (Fig. 2).
The adults evaluated by serum creatinine had a median age of 44.0 (33.9–56.8) years, were predominantly female (62.3%), and were from the Southeast region (45.9%). The prevalence of CKD, estimated as the proportion of people with GFR < 60 ml/min/1.73 m², was 3.79% (2.58% with CKD in stage 3a, 0.81% in stage 3b, 0.24% in stage 4, and 0.16% in stage 5). Participants who had both serum creatinine and proteinuria results were 57.0 (44.8–67.3) years old, and 58.1% were female. Their distribution of proteinuria categories was 76.4% mild or absent, 18.1% moderate, and 5.6% severe (Table 1).
Patients with serum creatinine values made up 18.1% of the total beneficiaries of with PHC (20.2% in the North, 24.2% in the Northeast, 13.9% in the Midwest, 15.2% in the Southeast, and 19.6% in the South). Patients with both serum creatinine and proteinuria data were 0.8% of the beneficiaries (0.7% in the Northeast, 0.4% in the North, 1.7% in the South, 0.8% in the Southeast, and 0.6% in the Midwest) (Table 2).
The proportion of males with GFR < 60 ml/min/1.73 m² was higher than that of females (4.03% versus 3.65%, p < 0.001), and the low-GFR proportion increased with age (0.17% among 18-29-year-olds, 0.53% among 30-44-year-olds, 1.98% among 45-59-year-olds, 9.4% among 60-74-year-olds, and 32.4% among ≥ 75-year-olds, p < 0.001). The distribution of the total sample in the various GFR ranges (in ml/min/1.73 m²) was 67.47% at ≥ 90, 28.73% at 60–89, 2.58% at 45–59, 0.81% at 30–44, 0.24% at 15–29, and 0.16% at < 15 (Table 3; Fig. 3).
CKD, chronic kidney disease. Stage 3a, estimated glomerular filtration rate (GFR) 45–59 ml/min/1.73 m². Stage 3b, GFR 30–44 ml/min/1.73 m². Stage 4, GFR 15–29 ml/min/1.73 m². Stage 5, GFR < 15 ml/min/1.73 m².
The estimated crude prevalence of CKD was highest in the Southeast region (5.10%), followed by the Midwest (3.36%), South (3.33%), Northeast (2.59%), and North regions (2.03%). The age- and gender-adjusted prevalence of CKD was higher in the Midwest region (4.43%), followed by the Southeast (4.21%), South (3.77%), North (3.35%), and Northeast regions (3.02%) (Table 4).
The proportion of males with proteinuria was higher than that of females (26.08% versus 21.87%, p < 0.001). There was no progressive increase in the prevalence of proteinuria with age. The distribution of the total sample in levels of proteinuria was 76,37% at mild, 18.05% at moderate, and 5.58% at severe level (Table 5).
According to the CKD risk map, the crude prevalence of patients with low, moderate, high and very high-risk categories for the disease was 68.9%, 19.4%, 6.6% and 5.1%, respectively. After adjusting for age and gender, these prevalences were: 70.1%, 20.0%, 5.8% and 4.1%, respectively (Fig. 4).
CKD, chronic kidney disease. A, Gross distribution. B, Distribution adjusted for age and gender. GFR, estimated glomerular filtration rate. Mild proteinuria, albumin/creatinine ratio (ACR) < 30 mg/g or 24-hour albuminuria (24-hour ALB) < 30 mg or 24-hour proteinuria (24-hour PTU) < 150 mg. Moderate, ACR 30–300 mg/g or 24-hour ALB 30–300 mg or 24-hour PTU 150–500 mg. Severe, ACR > 300 mg/g or 24-hour ALB > 300 mg or 24-hour PTU > 500 mg.
Discussion
The present study showed that the prevalence of CKD in beneficiaries with PHC in Brazil was 3.8%, according to the GFR estimated by the 2021 CKD-EPI equation. After adjusting for age and gender, this prevalence was higher in the Midwest and Southeast and lower in the North and Northeast of Brazil. While 18.1% of the beneficiaries were tested for serum creatinine, only 0.8% underwent measurement of proteinuria. Among them, approximately 10% were at high or very high-risk categories of CKD.
In recent decades, several studies have estimated the prevalence of CKD (Table 6 S) [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44]. The great variability of results (0.8–32.5%) is due, among other factors, to the population profile (age, comorbidities), the data sources (telephone survey, disease codes, screening programs, population-based studies, laboratory databases), and the definitions of CKD used (reduced GFR with or without altered proteinuria).
The estimated prevalence of CKD of 3.8% found in the present study was higher than that found in studies based on telephone surveys (1.4%) [22, 41] and by registering disease codes (0.8%) [29]. This might have been due to the silent nature of the early stages of CKD, which leads to low awareness among the population about the disease and identification failures of it by health professionals [35]. This fact reinforces the need for screening for CKD in people at risk by measuring serum creatinine and proteinuria [8, 9, 21].
On the other hand, our prevalence of 3.8% was lower than the estimates of CKD prevalence from screening programs (8.9–32.5%), which generally include individuals with risk factors for the disease, such as hypertension, diabetes mellitus, and cardiovascular diseases [25, 26, 28, 33, 35, 36, 38, 39]. Another explanation for the lower prevalence of CKD found in this study might be the fact that we enrolled individuals with PHC, who might have a lower age and burden of comorbidities and better socioeconomic conditions, since they are mostly economically active people with a corporate-type PHC. Unfortunately, detailed information on the comorbidity profile of our population was not available.
When compared to studies based on disease code registration and screening programs, it is possible that population-based studies [342,37,40,42,43] and those based on laboratory databases [23, 24, 27, 29,30,31,32, 44] can include individuals with lower disease burdens. Even so, the prevalence of CKD found in this study (3.8%) was lower than that in previous studies of the same nature (5.6–12.4%). Possible explanations would be the lower mean age of the participants in our study and the use of the 2021 CKD-EPI equation rather than the 2009 equation. In fact, older age is an important risk factor for reduced GFR, and the 2021 CKD-EPI equation may overestimate the GFR by 3–5 ml/min/1.73 m² when compared to the 2009 CKD-EPI Eqs. [21, 45, 46]. In our population, when the 2009 CKD-EPI equation was applied, the prevalence of CKD was estimated at 5.1% (Table 7 S). In addition, the definition of CKD used in this study considered only reduced GFR, as a very small proportion of people in Brazil are routinely tested for proteinuria. This fact constitutes a serious flaw in the implementation of the line of care for CKD in our country, which has already been pointed out by previous national studies [10, 11]. Thus, participants with preserved GFR and present proteinuria were not counted as having CKD.
In our study, the estimated prevalence of CKD was slightly higher in males than in females. On this matter, the previous reports show discordant results. Women could have more CKD than men due to their smaller nephron mass and greater chance of early diagnosis, since in many cultures women are more conscientious about their health than men [23, 25, 28, 31,32,33, 37, 43,44,45, 47,48,49]. On the other hand, men might have a higher prevalence of CKD due to their higher frequency of hypertension and proteinuria [24, 26, 39].
The regional differences found after adjustment for age and gender could not be analysed in detail due to the unavailability of information on the patients’ morbidities. It might be that individuals from the North and Northeast regions of Brazil have a lower prevalence of CKD due to the lower prevalence of hypertension, diabetes, and obesity, as shown in a national telephone survey [50].
The result of 24% of patients with proteinuria and 10% of patients at high or very high-risk categories of CKD found in this cohort is higher than the estimative of previous studies [10, 35]. Possibly patients of our study with proteinuria test requests were sicker than the population with serum creatinine dosages. In fact, the crude prevalence of high or very high-risk categories of CKD was higher than the age- and gender adjusted prevalence.
Some limitations of this study should be acknowledged, such as the unavailability of information on the participants’ comorbidities, the impossibility of using two serum creatinine results in the same individuals to confirm the diagnosis of CKD, and the noninclusion of proteinuria measurement in the assessment of the prevalence of CKD. Nevertheless, the importance of this study lies in its size (one of the largest ever conducted in Brazil), in the national representativeness of individuals with PHC (approximately one-fifth of the beneficiaries were tested for serum creatinine), and because it is the first Brazilian study to use the 2021 CKD-EPI equation to estimate the prevalence of CKD.
Conclusions
In this Brazilian national study of individuals with PHC, we found a prevalence of CKD of 3.8%, a deficiency of proteinuria screening, and approximately 10% of participants with high or very high-risk for such disease. These results provide relevant information on various strata of the Brazilian population with PHC and serve as a basis for planning interventions aimed at early diagnosis and care of CKD.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 24-hour ALB:
-
24-hour albuminuria
- 24-hour PTU:
-
24-hour proteinuria
- ACR:
-
Urine albumin/creatinine ratio
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- GFR:
-
Glomerular filtration rate
- NCDs:
-
Noncommunicable diseases
- PHC:
-
Private health coverage
- SUS:
-
Brazilian Unified Health System
References
Borg R, Carlson N, Søndergaard J, Persson F. The growing challenge of chronic kidney disease: an overview of current knowledge. Int J Nephrol. 2023;2023:9609266. https://doi.org/10.1155/2023/9609266.
Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl (2011). 2022;12(1):7–11. https://doi.org/10.1016/j.kisu.2021.11.003.
Kakitapalli Y, Ampolu J, Madasu SD, Sai Kumar MLS. Detailed review of chronic kidney disease. Kidney Dis (Basel). 2020;6(2):85–91. https://doi.org/10.1159/000504622.
Liu HH, Zhao S. Savings Opportunity from Improved CKD Care Management. J Am Soc Nephrol. 2018;29(11):2612–5. https://doi.org/10.1681/ASN.2017121276.
Jha V, Al-Ghamdi SMG, Li G, Wu MS, Stafylas P, Retat L, Card-Gowers J, Barone S, Cabrera C, Garcia Sanchez JJ. Global Economic Burden Associated with chronic kidney disease: a pragmatic review of medical costs for the Inside CKD Research Programme. Adv Ther. 2023. https://doi.org/10.1007/s12325-023-02608-9.
Saúde Ministérioda. Brasil. Secretaria de Vigilância em Saúde, Departamento de Análise em Saúde e Vigilância de Doenças Não Transmissíveis. Plano de Ações Estratégicas para o Enfrentamento das Doenças Crônicas e Agravos não Transmissíveis no Brasil 2021–2030. Available on: http://bvsms.saude.gov.br/bvs/publicacoes/plano_enfrentamento_doencas_cronicas_agravos_2021_2030.pdf.
Ministério da Saúde. Brasil. DATASUS. Sistema de Informações Ambulatoriais do Sistema Único de Saúde (SIA/SUS). Available on: https://datasus.saude.gov.br/acesso-a-informacao/producao-ambulatorial-sia-sus/.
Saúde Ministérioda. Brasil. Secretaria de Atenção à Saúde. Departamento de Atenção Especializada e Temática. Diretrizes clínicas para o cuidado ao paciente com doença renal crônica – DRC no Sistema Único de Saúde. Available on: https://portalarquivos2.saude.gov.br/images/pdf/2014/marco/24/diretriz-cl--nica-drc-versao-final.pdf.
Ministério da Saúde, Brasil. Portaria nº 1675 de 2018. Critérios para a organização, funcionamento e financiamento do cuidado da pessoa com Doença Renal Crônica - DRC no âmbito do Sistema Único de Saúde. Available on: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2018/prt1675_08_06_2018.html.
Samaan F, Fernandes DE, Kirsztajn GM, Sesso RCC, Malik AM. Quality indicators for primary health care in chronic kidney disease in the public service of a city in the state of São Paulo, Brazil. Cad Saude Publica. 2022;38(2):e00090821. https://doi.org/10.1590/0102-311X00090821.
Samaan F, Gutierrez M, Kirsztajn GM, Sesso RC. Supply/demand ratio for medical consultations, diagnostic tests and chronic kidney disease monitoring in the Brazilian National Health System: a descriptive study, state of São Paulo, Brazil, 2019. Epidemiol Serv Saude. 2022;31(2):e20211050. https://doi.org/10.1590/S2237-96222022000200014.
Assis Buosi AP, Paturkar D, Dias ER, Estorninho MJ, Kolawole O, Ghooi R, Lutchman S. The rights of patients with chronic kidney disease in the World: Legal perspectives and challenges in Brazil, India, Portugal, South Africa, and Nigeria. Contrib Nephrol. 2021;199:322–38. https://doi.org/10.1159/000517722.
Silva GBD Junior, Oliveira JGR, Oliveira MRB, Vieira LJES, Dias ER. Global costs attributed to chronic kidney disease: a systematic review. Rev Assoc Med Bras (1992). 2018;64(12):1108–16. https://doi.org/10.1590/1806-9282.64.12.1108.
Burgos-Calderón R, Depine SÁ, Aroca-Martínez G. Population Kidney Health. A new paradigm for chronic kidney Disease Management. Int J Environ Res Public Health. 2021;18(13):6786. https://doi.org/10.3390/ijerph18136786.
Myers OB, Pankratz VS, Norris KC, Vassalotti JA, Unruh ML, Argyropoulos C. Surveillance of CKD epidemiology in the US - a joint analysis of NHANES and KEEP. Sci Rep. 2018;8(1):15900. https://doi.org/10.1038/s41598-018-34233-w.
Ministério da Saúde. Brasil. Secretaria de Ciência, Tecnologia, Inovação e Insumos Estratégicos em Saúde. Relação Nacional de Medicamentos Essenciais Rename 2022. Available on: http://bvsms.saude.gov.br/bvs/publicacoes/relacao_nacional_medicamentos_2022.pdf.
Ministério da Saúde. Brasil. Agência Nacional de Saúde Suplementar. Tabnet – Informações em saúde complementar: taxa de cobertura de planos de saúde. Available on: http://www.ans.gov.br/anstabnet/cgi-bin/dh?dados/ tabnet_tx.def.
Ministério da Saúde. Brasil. Agência Nacional de Saúde Suplementar. Programas de Promoção da Saúde e Prevenção de Riscos e Doenças. Available on: https://www.ans.gov.br/index.php?option=com_promoprev&view=consulta
Ministério da Saúde. Brasil. Agência Nacional de Saúde Suplementar. Tabnet – Informações em saúde complementar: Beneficiários por Operadora. Available on: https://www.ans.gov.br/anstabnet/cgi-bin/dh?dados/tabnet_cc.def7.
Inker LA, Eneanya ND, Coresh J, Tighiouart H, Wang D, Sang Y, et al. Chronic Kidney Disease Epidemiology Collaboration. New Creatinine- and cystatin C-Based equations to Estimate GFR without Race. N Engl J Med. 2021;385(19):1737–49. https://doi.org/10.1056/NEJMoa2102953.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1-150.global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013; 158(11):825 – 30. https://doi.org/10.7326/0003-4819-158-11-201306040-00007.
de Sousa LCM, Silva NR, Azeredo CM, Rinaldi AEM, da Silva LS. Health-related patterns and chronic kidney disease in the Brazilian population: National Health Survey, 2019. Front Public Health. 2023;11:1090196. https://doi.org/10.3389/fpubh.2023.1090196.
Samaan F, Damiani BB, Kirsztajn GM, Sesso R. A cross-sectional study on the prevalence and risk stratification of chronic kidney disease in Cardiological patients in São Paulo. Brazil Diagnostics (Basel). 2023;13(6):1146. https://doi.org/10.3390/diagnostics13061146.
Mazhar F, Sjölander A, Fu EL, Ärnlöv J, Levey AS, Coresh J, Carrero JJ. Estimating the prevalence of chronic kidney disease while accounting for nonrandom testing with inverse probability weighting. Kidney Int. 2023;103(2):416–20. https://doi.org/10.1016/j.kint.2022.10.027.
Feng T, Xu Y, Zheng J, Wang X, Li Y, Wang Y, Zhu B, Zhao L, Zhao H, Yu J. Prevalence of and risk factors for chronic kidney disease in ten metropolitan areas of China: a cross-sectional study using three kidney damage markers. Ren Fail. 2023;45(1):2170243. https://doi.org/10.1080/0886022X.2023.2170243.
Navise NH, Mokwatsi GG, Gafane-Matemane LF, Fabian J, Lammertyn L. Kidney dysfunction: prevalence and associated risk factors in a community-based study from the North West Province of South Africa. BMC Nephrol. 2023;24(1):23. https://doi.org/10.1186/s12882-023-03068-7.
Guedes M, Rosa BB, Rocha PT, Teixeira CM, Pecoits-Filho R. Braz J Nephrol (J Bras Nefrol). 2022;44(3 Suppl 1):90. Limitações nas práticas de triagem e estratificação de risco da doença renal crônica no brasil: uma análise de um banco de dados laboratorial nacional.
Gbaguidi GN, Houehanou CY, Amidou SA, Vigan J, Houinato DS, Lacroix P. Prevalence of abnormal kidney function in a rural population of Benin and associated risk factors. BMC Nephrol. 2021;22(1):116. https://doi.org/10.1186/s12882-021-02316-y.
Vestergaard SV, Christiansen CF, Thomsen RW, Birn H, Heide-Jørgensen U. Identification of patients with CKD in Medical databases: a comparison of different algorithms. Clin J Am Soc Nephrol. 2021;16(4):543–51. https://doi.org/10.2215/CJN.15691021.
Takeuchi M, Shinkawa K, Yanagita M, Kawakami K. Prevalence, recognition and management of chronic kidney disease in Japan: population-based estimate using a healthcare database with routine health checkup data. Clin Kidney J. 2021;14(10):2197–202. https://doi.org/10.1093/ckj/sfab016.
Jonsson AJ, Lund SH, Eriksen BO, Palsson R, Indridason OS. The prevalence of chronic kidney disease in Iceland according to KDIGO criteria and age-adapted estimated glomerular filtration rate thresholds. Kidney Int. 2020;98(5):1286–95. https://doi.org/10.1016/j.kint.2020.06.017.
Iwagami M, Tomlinson LA, Mansfield KE, Casula A, Caskey FJ, Aitken G, Fraser SDS, Roderick PJ, Nitsch D. Validity of estimated prevalence of decreased kidney function and renal replacement therapy from primary care electronic health records compared with national survey and registry data in the United Kingdom. Nephrol Dial Transplant. 2017; 1:32(suppl_2):ii142-ii150. https://doi.org/10.1093/ndt/gfw318.
Piccolli AP, Nascimento MM, Riella MC. Prevalence of chronic kidney disease in a population in southern Brazil (Pro-renal Study). Braz J Nephrol. 2017;39(4):384–90.
Benghanem Gharbi M, Elseviers M, Zamd M, Belghiti Alaoui A, Benahadi N, Trabelssi el H, Bayahia R, Ramdani B, De Broe ME. Chronic kidney disease, hypertension, diabetes, and obesity in the adult population of Morocco: how to avoid over- and under-diagnosis of CKD. Kidney Int. 2016;89(6):1363–71. https://doi.org/10.1016/j.kint.2016.02.019.
Ene-Iordache B, Perico N, Bikbov B, Carminati S, Remuzzi A, Perna A, Islam N, Bravo RF, Aleckovic-Halilovic M, Zou H, Zhang L, Gouda Z, Tchokhonelidze I, Abraham G, Mahdavi-Mazdeh M, Gallieni M, Codreanu I, Togtokh A, Sharma SK, Koirala P, Uprety S, Ulasi I, Remuzzi G. Chronic kidney disease and cardiovascular risk in six regions of the world (ISN-KDDC): a cross-sectional study. Lancet Glob Health. 2016;4(5):e307–19. https://doi.org/10.1016/S2214-109X(16)00071-1.
Galbraith LE, Ronksley PE, Barnieh LJ, Kappel J, Manns BJ, Samuel SM, Jun M, Weaver R, Valk N, Hemmelgarn BR. The see kidney disease targeted Screening Program for CKD. Clin J Am Soc Nephrol. 2016;11(6):964–72. https://doi.org/10.2215/CJN.11961115.
Ji E, Kim YS. Prevalence of chronic kidney disease defined by using CKD-EPI equation and albumin-to-creatinine ratio in the Korean adult population. Korean J Intern Med. 2016;31(6):1120–30. https://doi.org/10.3904/kjim.2015.193.
Barreto SM, Ladeira RM, Duncan BB, Schmidt MI, Lopes AA, Benseñor IM, Chor D, Griep RH, Vidigal PG, Ribeiro AL, Lotufo PA, Mill JG. Chronic kidney disease among adult participants of the ELSA-Brasil cohort: association with race and socioeconomic position. J Epidemiol Community Health. 2016;70(4):380–9. https://doi.org/10.1136/jech-2015-205834.
Pereira ERS, Pereira A, de Andrade C, de Naghettini GB, Pinto AV, Batista FKMS. Prevalência De doença renal crônica em adultos atendidos na Estratégia De Saúde Da Família. Braz J Nephrol. 2016;38(1):22–30. https://doi.org/10.5935/0101-2800.20160005.
Schaefer JCF, Pereira MS, Jesus CR, Schuelter-Trevisol F, Trevisol DJ. Estimativa Da função renal na população de 18 a 59 anos da cidade de Tubarão-SC: um estudo de base populacional. Braz J Nephrol. 2015;37(2):185–91.
de Moura L, Andrade SSC, de Malta A, Pereira DC, Passos CA. Prevalência De autorrelato de diagnóstico médico de doença renal crônica no Brasil: Pesquisa Nacional De Saúde, 2013. Rev bras Epidemiol. 2015;18:181–91. https://doi.org/10.1590/1980-5497201500060016.
Dutra MC, Uliano EJM, Machado DFG, de Martins P, Schuelter-Trevisol T, Trevisol F. Avaliação Da função renal em idosos: um estudo de base populacional. Braz J Nephrol. 2014;36(3):297–303. https://doi.org/10.5935/0101-2800.20140043.
Castro AF, Coresh J. CKD surveillance using laboratory data from the population-based National Health and Nutrition Examination Survey (NHANES). Am J Kidney Dis. 2009;53(3 Suppl 3):S46–55. https://doi.org/10.1053/j.ajkd.2008.07.054.
Bastos RMR, Bastos MG, Ribeiro LC, Bastos RV, Teixeira MTB. Prevalência Da doença renal crônica nos estágios 3, 4 e 5 em adultos. Revista Da Associação Médica Brasileira. 2009;55(1):40–4. https://doi.org/10.1590/S0104-42302009000100013.
Fu EL, Coresh J, Grams ME, Clase CM, Elinder CG, Paik J, Ramspek CL, Inker LA, Levey AS, Dekker FW, Carrero JJ. Removing race from the CKD-EPI equation and its impact on prognosis in a predominantly white European population. Nephrol Dial Transpl. 2023;38(1):119–28. https://doi.org/10.1093/ndt/gfac197.
Delgado C, Baweja M, Burrows NR, Crews DC, Eneanya ND, Gadegbeku CA, Inker LA, Mendu ML, Miller WG, Moxey-Mims MM, Roberts GV, St Peter WL, Warfield C, Powe NR. Reassessing the inclusion of race in diagnosing kidney diseases: an Interim Report from the NKF-ASN Task Force. Am J Kidney Dis. 2021;78(1):103–15. https://doi.org/10.1053/j.ajkd.2021.03.008.
Luyckx VA, Brenner BM. Low birth weight, nephron number, and kidney disease. Kidney Int Suppl. 2005;97S68–77. https://doi.org/10.1111/j.1523-1755.2005.09712.x.
Carrero JJ. Gender differences in chronic kidney disease: underpinnings and therapeutic implications. Kidney Blood Press Res. 2010;33(5):383–92. https://doi.org/10.1159/000320389.
Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens. 2009;27(5):963–75. https://doi.org/10.1097/hjh.0b013e3283282f65.
Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde e Ambiente. Departamento de Análise Epidemiológica e Vigilância de Doenças Não Transmissíveis. Vigitel Brasil 2023: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico: estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção para doenças crônicas nas capitais dos 26 estados brasileiros e no Distrito Federal em 2023. Available on: http://bvsms.saude.gov.br/bvs/publicacoes/vigitel_brasil_2023.pdf.
Acknowledgements
Not applicable.
Funding
This study was financed with the authors’ own resources.
Author information
Authors and Affiliations
Contributions
F.S. was responsible for conceptualizing the study, methodology, project administration, formal analysis and writing the original draft. R.C.S. was responsible for statistical analysis, formal analysis, validation, review and editing. AM. was responsible for data curation and validation. G.M.K. and R.S. were responsible for oversight and provided critical review of the draft. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the research ethics committee Invitare Pesquisa Clínica e Auditoria (https://www.invitare.com.br/site/). This committee authorized a waiver of consent due to the study being retrospective, non-interventionist, large in size and the impossibility of communicating with all participants (ethical presentation certificate number 64260622.1.0000.8098).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Samaan, F., Silveira, R.C., Mouro, A. et al. Laboratory-based surveillance of chronic kidney disease in people with private health coverage in Brazil. BMC Nephrol 25, 162 (2024). https://doi.org/10.1186/s12882-024-03597-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-024-03597-9