Abstract
Background
Modality transitions represent a period of significant change that can impact health related quality of life (HRQoL). We explored the HRQoL of adults transitioning to new or different dialysis modalities.
Methods
We recruited eligible adults (≥ 18) transitioning to dialysis from pre-dialysis or undertaking a dialysis modality change between July and September 2017. Nineteen participants (9 incident and 10 prevalent dialysis patients) completed the KDQOL-36 survey at time of transition and three months later. Fifteen participants undertook a semi-structured interview at three months. Qualitative data were thematically analyzed.
Results
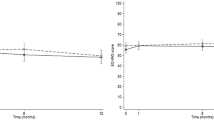
Four themes and five sub-themes were identified: adapting to new circumstances (tackling change, accepting change), adjusting together, trading off, and challenges of chronicity (the impact of dialysis, living with a complex disease, planning with uncertainty). From the first day of dialysis treatment to the third month on a new dialysis therapy, all five HRQoL domains from the KDQOL-36 (symptoms, effects, burden, overall PCS, and overall MCS) improved in our sample (i.e., those who remained on the modality).
Conclusions
Dialysis transitions negatively impact the HRQoL of people with kidney disease in various ways. Future work should focus on how to best support people during this time.
Similar content being viewed by others
Background
Globally, the number of people on dialysis is increasing, with North America having one of the highest rates [1]. Dialysis utilization not only uses a disproportionate amount of healthcare resources [2] but can be burdensome to people on dialysis. Despite people on dialysis reporting a lower health related quality of life (HRQoL) compared to the general population [3, 4], studies that have been conducted to explore HRQoL across dialysis modalities have not consistently shown a difference between modality types (e.g., hemodialysis, peritoneal dialysis, home hemodialysis) [5]. This may partially be explained by the dynamic changes to HRQoL throughout dialysis care trajectories [6], making it important to target times in care trajectories where HRQoL needs are high regardless of dialysis modality.
Dialysis transitions and changes in modality have been highlighted as a time where attention to the potential changes in HRQoL should be considered [7,8,9]. Transition periods in dialysis care pathways can be especially tumultuous [10]. People embark on a new way of life, challenging their coping mechanisms and making them re-evaluate their identities, their relationships with themselves, others, and with their disease and treatment [10]. Kidney failure transition periods are often triggered by declining health and medical necessity, and have been described as emotionally turbulent, “marked by periods of emotional upheaval and doubts about the future” [10, 11]. In addition to being times of mental and emotional stress, transition periods are also often periods of physical stress as people may be experiencing several symptoms related to uremia or inadequate dialysis. Morbidity and mortality have also been shown to increase during dialysis transitions, [12, 13] which may further impact HRQoL. Very few studies examine the changes in HRQoL in the transition period [3, 14, 15] and of these most compare the prospective changes in HRQoL from prior to dialysis initiation to 6 or 12 months later [3, 15].Unfortunately there is a paucity of literature on how HRQoL is impacted during the early dialysis transition, which is needed to better understand how kidney programs can support people during this time. We thus aimed to explore the HRQoL experiences of adults who were transitioning to a new dialysis modality.
Methods
Setting
This study was conducted in a large urban city in Western Canada that has seven adult dialysis sites that collectively serve approximately 680 patients on dialysis, with approximately 25 patients transitioning to dialysis every month. The three sites where patients primarily transition to dialysis were selected for recruitment and include an in-center hemodialysis (IHD) center, a home hemodialysis (HHD) clinic, and a peritoneal dialysis (PD) clinic.
Participants
Eligible adults attending an in-person appointment at the dialysis clinic during our study period (July 2017 to September 2017) were informed about the study by an intermediary. Interested individuals were approached by a member of the research team. Those who agreed to participate provided written informed consent and completed a baseline survey and demographic questionnaire. Participants were then contacted by telephone for later data collection phases. We included adults (≥ 18) who were undergoing a planned transition to dialysis or undertaking a modality change. As people undergoing temporary transitions may have different experiences, we excluded those who had an acute kidney injury and/or were expected to recover kidney function, and those who were undergoing a temporary modality change anticipated to last less than three months. We further excluded people who were not English speaking due to the lack of resources required to hire an interpreter and translate the study data.
Data collection
We leveraged the Kidney Disease Quality of Life-36 (KDQOL-36) to guide data collection. The KDQOL-36 is a validated tool for both pre-dialysis and dialysis patients that assess HRQoL in two generic domains [physical component summary score (PCS) and mental component summary score (MCS)] and three kidney disease-specific domains (“Symptoms/Problems”, “Burden of Kidney Disease”, and “Effects of Kidney Disease on Daily Life”) [16,17,18].
A male graduate student (CD), with one year of experience and training in qualitative research and no prior relationship with the participants, conducted semi-structured telephone interviews approximately three months after starting on their new modality. The interview guide was developed to collect qualitative data to complement the five domains of the KDQOL-36. The open-ended questions allowed patients to elaborate and provide context for how their modality transition impacted different aspects of their quality of life. (Supplementary File 1). Telephone based interviews were used as they are an effective way to increase participant comfort and allow participants to be more forthcoming with responses [19,20,21]. Participants who could not be contacted by telephone were approached at their next clinic visit. All participants were asked the same guiding questions, however, probing questions changed based on participant responses and queries derived from past interviews. All interviews were audio recorded, transcribed verbatim, and fieldnotes were taken. The transcripts were not returned to participants for approval.
To further explore HRQoL, participants completed an initial paper survey comprised of the KDQOL-36 survey domains within the first week of their modality transition and typically on their first day of IHD or their first day of home dialysis training (PD and HHD) and again three months later. The survey was most often filled out in private but if the patient requested it, a family member was present. Patients who were not coming to the clinic were mailed the surveys and asked to return them in a sealed envelope at their next clinic appointment.
Data analysis
We conducted an inductive thematic analysis to analyze the interview data [22, 23]. Interviews were transcribed verbatim. CD, DF, and JM then read the transcripts through several times to immerse in the data. An initial coding framework was generated through discussion and open coding of the dataset. Codes were refined, named, and defined through iterative rounds of discussion and further coding until distinct overarching themes were formed. The original transcripts were then re-reviewed to ensure the final themes were reflective of the data. The themes reflected the overarching HRQoL experiences during transitions; however, it was also noted that experiences were often shaped by modality specific nuances. These nuances were often experienced or emphasized differently across individuals, as such, it was not possible to synthesize common experiences. Examples from each modality were thus pulled from the data and highlighted descriptively based on HRQoL domains. No qualitative data software was used for data analysis.
Baseline characteristics were summarized with basic descriptive statistics. The KDQOL-36 surveys were scored using the scoring template provided by RAND corporation, which converts raw entry data to a score from 0 to 100 [16]. The additional domains from the KDQOL-SF were scored following instructions provided by RAND specific to these domains [16]. The mean and standard deviation were calculated for each of the KDQOL domains at baseline and at 3 months.
Results
Patient characteristics
Sixty-nine patients undertook modality changes during the recruitment period. Twenty-five were excluded based on pre-specified exclusion criteria. Of the 44 eligible patients, 30 consented to participate. Figure 1 shows the number of patients lost to follow-up. At three months, 19 patients (9 incident and 10 prevalent) remained in the study: 3 IHD, 9 PD, and 7 HHD. All 19 completed KDQOL surveys at baseline and 3 months. Four participants returned their surveys via mail but did not return our call to set up an interview. We attempted to contact these patients on three separate occasions, after which no further contact was made. Ultimately, fifteen participants were interviewed (range = 23 to 75 min). Table 1 shows the demographics of the 19 study participants. The mean age of the cohort was 50.9 +/- 16.9 years, with 73.7% male. Participants who were lost to follow up had similar characteristics. Dialysis vintage ranged from 0 months (incident patients) to one patient who had been on dialysis for over 7 years. All patients had hypertension and approximately one-quarter had diabetes. Other comorbidities were uncommon.
The transition experience
Four overarching themes and five sub-themes were identified during the qualitative analysis that reflected the modality transition experiences of patients. Themes included: (1) adapting to new circumstances, sub-themes 1a) tackling change 1b) accepting change; (2) adjusting together; (3) trading off; (4) challenges of chronicity, sub-themes 4a) the impact of dialysis; 4b) living with a complex disease; 4c) and planning with uncertainty. Exemplar quotations for each theme are provided in Table 2. Participants further described the various ways in which modality specific nuances impacted their HRQoL during their transition (exemplars in Fig. 2; Table 3). An increase in mean KDQOL-36 scores were observed from baseline to three months on therapy within each domain of the KDQOL-36 regardless of where the patient was transitioning from (i.e. incident or prevalent patients) (Table 4).
Theme 1: adapting to new circumstances
1a. Tackling Change. Dialysis care trajectories are not static processes, and often transitions did not go smoothly or as planned. Participants spoke of the ways in which they overcame both routine and unexpected changes and challenges in order to fit their new modality into their life. Some participants tackled change in active ways by advocating for unmet needs or adjusting the environment around them.
When I first got set up and everything, you walk into the room and I was like man, this reminds me of a hospital room. But now, it’s just contained to the bedroom. So it’s fine. [P6]
Others transitioned in a more passive way as the environment around them seemed outside of their control. This process was often cyclical where participants would “figure things out” yet often also be wary of what changes and challenges were to come.
1b. Accepting Change. Accepting change was discussed by participants in regard to the intricacies within both starting dialysis and the health changes that came with worsening complications of kidney disease. Though most participants learned to adjust to their new circumstance as their new treatment method was necessary, they experienced different degrees of acceptance at the time of interview.
I still haven’t adjusted to the night, because when the cycler changes and starts to drain like a vacuum, I just sort of wake up and I’m not quite sure why. But I am adjusting, and it’s getting a little better over time. [P29]
Some participants compared their situation to better times and spoke of what had been lost (e.g. physical functioning, ability to work). While others focussed on the positive ways in which their new modality improved their life (e.g. symptom improvement, treatment flexibility). The degree of acceptance was often influenced by individual contexts and views including their medical status, where they were transitioning from, their age, their work status, their interactions with other patients, and their future prospects (e.g. transplant).
Theme 2: adjusting together
My wife is sort of limited to falling asleep when I am finally set up and limited to waking up when I wake up as well. So, she’s also not getting the best sleep even when she is sleeping. [P1]
Participants spoke of the ways in which their kidney disease and transitioning to dialysis or a new modality impacted both their lives and the lives of those around them. Some participants spoke of this as a positive change, where they were feeling better and able to be more present, or their new modality was better suited to family dynamics. Other patients spoke of how they felt like a burden to friends and family and felt guilty about the impact their disease had on the people in their lives. Regardless, everyone was adjusting through this process together. Responsibilities also often needed to be adapted based on everyone’s needs, not just of those of the patient. At times there were conflicts in roles between what the patient felt they needed and could do, to what their support person felt they needed or should be doing.
Theme 3: trading off
… I’m feeling better compared to before. Other than actually having to go on dialysis at night. I am feeling better. [P6]
Most participants spoke of a give and take that occurred on dialysis and during modality transition. Having kidney disease was far from perfect and it was clear that there was no “best” dialysis treatment. As such, participants spoke of a trade off, giving up some things in favor of others. For example, one man spoke of how even though home dialysis was a lot of work to set up, it was better than driving to a facility three times per week. Ultimately, participants spoke of finding the modality that suited them best. This was a dynamic process, and as patients’ needs and circumstances changed, so did this “trade off” and subsequent modality fit. At times, the reason for modality switch was out of their control and patients could no longer stay on their intended therapy (i.e., PD membrane failure).
Theme 4: challenges of chronicity
4a. The Impact of Dialysis. Most participants expressed an improvement in some symptoms of kidney disease after their transition. However, the participants responded to their dialysis therapy differently and there were various other elements that impacted their HRQoL. The perceived impact of dialysis was important to understand in the context of how their dialysis modality met their expectations and what they were prepared for or were able to manage (e.g. financial impact of not working or time traveling to dialysis).
It ruins my social life, because, I had to wake up at 7:00 am to do [manual exchange of PD solution] and then 11:00 again and then three o’clock in the afternoon and then seven o’clock at night, so I don’t go nowhere… Even my groceries, I have to make it quick because I don’t want to be late for my exchange. [P11]
4b. Living with a Complex Disease(s). Patients were often not only living with kidney disease, which was already difficult enough, but frequently patients had additional comorbidities. This resulted in constant changing needs and symptoms that ebbed and flowed as their disease progressed. The impact was felt in all aspects of the patient’s life and appeared to vary based on what life stage the participant was at.
Since I got sick I cannot work anymore…with the kind of job I had, you have to be standing, running around, I cannot do that anymore. I easily get tired. [P11]
4c. Planning with Uncertainty. Living with kidney disease among other comorbidities led to feelings of uncertainty and often a lack of control. For some participants this was difficult, as it was hard to plan for the future when how they felt and where they were (e.g. dialysis modality, in hospital) could change quickly. However, many patients took things “day by day” and did not feel bound by the constraints felt by others. This enabled them to feel hopeful for the future and excited to plan for future events.
I still don’t feel that I have enough trust in my ability to commit to being able to do something…over today, but I’m not too sure what tomorrow will bring. [P5]
Discussion
We identified four primary themes that may help us understand the patient experience during their transition to a new dialysis modality: adapting to new circumstances, adjusting together, trading off, and challenges of chronicity. Overall, our findings illustrate that modality transitions represent a time of significant change that can be difficult for patients regardless of what modality they are transitioning to, or from and regardless of if it was an incident or prevalent transition. This reinforces the importance of creating integrated models of care that support people during transitions across the kidney disease trajectory [24].
We found that from the first day of dialysis treatment to the third month on a new dialysis therapy, all five HRQoL domains from the KDQOL-36 (symptoms, effects, burden, overall PCS, and overall MCS) improved in our sample (i.e., those who remained on the modality). Although we were underpowered to assess for statistical associations, we noticed that KDQOL-36 scores were similar across both incident and prevalent dialysis transitions, potentially indicating that dialysis transitions may negatively impact HRQoL regardless of where an individual is in their care trajectory. HRQoL scores are known to be lower in people on dialysis than the general public, as well as those who have received a kidney transplant, making HRQoL an important element in care for people on dialysis irrespective of dialysis modality choice or transition time period [25, 26]. However, the low HRQoL scores at the beginning of the transition period in our study demonstrate that the early transition period may be a particularly difficult time that would require supportive interventions.
Although our small sample size made it inappropriate to ascertain clinical meaning or statistical associations from the HRQoL scores in our study, the qualitative findings reveal the turmoil that may be present during dialysis transitions. Participants in our study spoke of how they had to tackle constant changes and challenges, adapt to their new roles and responsibilities, and adjust to the intricacies of each modality therapy, all while managing a complex illness. This was true across both incident and prevalent transitions. It is thus not surprising that other authors have reported that 44% of people initiating dialysis meet the criteria for depression [27]. A qualitative study of 36 people initiating hemodialysis identified three major constructs that patients describe during a transition period: “redefinition of self”, “quality of supports”, and “meanings of illness and treatment” [11]. In particular, the perceived quality of supports had a large impact on how people redefine themselves during transitions [11]. It is thus possible that providing adequate support during transition periods may positively impact HRQoL.
Interestingly, how patients described the transition period in our qualitative interviews differed, with some patients comparing their current situation to the last time they were feeling well on either a previous dialysis therapy, before they started dialysis, or even before they got sick with kidney disease, while others described the transition as the day of dialysis start. This was also true for when, and often if, their transition period ended. This creates further challenges as it makes it difficult to ascertain how long supportive interventions are required for, or when they are most effective at easing transition burden.
Individualized care is challenging in current dialysis facilities, where resources for patient-specific supports are often limited by time and budgetary constraints. Despite growing recognition that transition periods are times of immense difficulty for patients, relatively little is known about methods to ease physical and emotional strain during transitions. Clinicians often focus on medical complications during transition periods rather than psychological complications, and some experts have suggested psychosocial and spiritual factors should be attended to more by dialysis staff during transition states [10, 28]. Some authors have even suggested that transitional care units should be standard of care; in these units, patients would receive more individualized care for the initial weeks to months of dialysis, allowing a more intensive focus on their individual motivations and goals [29, 30].
Clinically, our findings highlight the importance of focusing on supporting patients during dialysis transitions, regardless of modality vintage. Viewing the transition experience from a more holistic lens may enable kidney programs to put common interventions in place across all phases of the care trajectory and ultimately better support patients across programs rather than in siloed care structures and dialysis units. Future research should aim to identify individual patient needs during transitions and to implement effective interventions to meet them. For interventions to be effective, a better understanding from patients and their families about the breadth and depth of the different meanings of and definitions attributed to transition periods are needed.
While our study yields important findings regarding the patient experience during transition periods, there are some important limitations. First, our recruitment period was short, yielding a small number of patients transitioning to and from a variety of dialysis vintages. This source of heterogeneity may have influenced our results. Statistical testing was not performed due to small sample size. However, despite our small sample size we achieved thematic saturation with our interviews. The fact that non-English speakers were excluded from our study is an important limitation, as it stands to reason that lacking the ability to fully communicate with care providers may have a profoundly negative impact on quality of life during the transition period. It is also possible that the true HRQoL scores during dialysis transitions are lower than what we found since many people who were approached to participate in our study refused as they were too overwhelmed by their circumstances. Participants who were lost to follow up also most often either died, or experienced peritoneal dialysis catheter malfunction sparking another modality change, both which may have further negatively impacted HRQoL. Although large difference in HRQoL were not noted between incident and prevalent dialysis starts, this would be an important avenue to explore in future work. Lastly, our sample was predominantly male, and sex and gender differences may impact transition experiences.
Conclusions
Modality transitions represent a time of significant change that can be difficult for patients regardless of what modality they are transitioning to, or from. Future research should focus on exploring this transition with larger sample sizes and in different contexts with a goal of seeking insight into how transitions can be improved.
Data Availability
We are not able to make our dataset publicly available due to the potential to identify participants in both the qualitative and quantitative data. Please contact the corresponding author should you wish to discuss this further.
Abbreviations
- HRQoL:
-
Health related quality of life
- IHD:
-
In-center hemodialysis
- HHD:
-
Home hemodialysis
- PD:
-
Peritoneal dialysis
- KDQOL-36:
-
The Kidney Disease Quality of Life-36 (KDQOL-36)
- PCS:
-
Physical component summary score
- MCS:
-
Mental component summary score
- MCID:
-
Minimal clinically important difference
References
Canadian Institute for Health Information. Annual statistics on organ replacement in Canada: Dialysis, transplantation and donation, 2009–2018. Ottawa, ON 2019.
Klarenbach SW, Tonelli M, Chui B, Manns BJ. Economic evaluation of dialysis therapies. Nat Rev Nephrol. 2014;10(11):644.
Broers NJH, Martens RJH, Canaud B, Cornelis T, Dejagere T, Diederen NMP, et al. Health-related quality of life in end-stage renal disease patients: the effects of starting dialysis in the first year after the transition period. Int Urol Nephrol. 2018;50(6):1131–42.
Mazairac AH, de Wit GA, Penne EL, van der Weerd NC, de Jong B, Grooteman MP, et al. Changes in quality of life over time—dutch haemodialysis patients and general population compared. Nephrol Dialysis Transplantation. 2011;26(6):1984–9.
CADTH. Dialysis modalities for the treatment of end-stage kidney disease: A health technology assessment. Ottawa, Ontario; 2017.
de Brito DCS, Machado EL, Reis IA, Moreira DP, Nébias THM, Cherchiglia ML. Modality transition on renal replacement therapy and quality of life of patients: a 10-year follow-up cohort study. Qual Life Res. 2019;28(6):1485–95.
Eneanya ND, Maddux DW, Reviriego-Mendoza MM, Larkin JW, Usvyat LA, Van Der Sande FM et al. Longitudinal patterns of health-related quality of life and dialysis modality: a national cohort study. BMC Nephrol. 2019;20(1).
Imbeault B, Nadeau-Fredette A-C. Optimization of Dialysis Modality Transitions for Improved Patient Care. Can J Kidney Health Disease. 2019;6:205435811988266.
Schaeffner E. Smoothing transition to dialysis to improve early outcomes after dialysis initiation among old and frail adults—a narrative review. Nephrol Dialysis Transplantation. 2022;37(12):2307–13.
Hutchinson TA. Transitions in the lives of patients with end stage renal disease: a cause of suffering and an opportunity for healing. Palliat Med. 2005;19(4):270–7.
Gregory DM, Way CY, Hutchinson TA, Barrett BJ, Parfrey PS. Patients’ perceptions of their experiences with ESRD and hemodialysis treatment. Qual Health Res. 1998;8(6):764–83.
Pulliam J, Li N-C, Maddux F, Hakim R, Finkelstein FO, Lacson E Jr. First-year outcomes of incident peritoneal dialysis patients in the United States. Am J Kidney Dis. 2014;64(5):761–9.
Lukowsky LR, Kheifets L, Arah OA, Nissenson AR, Kalantar-Zadeh K. Patterns and predictors of early mortality in incident hemodialysis patients: new insights. Am J Nephrol. 2012;35(6):548–58.
Moore C, Carter L-A, Mitra S, Skevington S, Wearden A. Quality of life improved for patients after starting dialysis but is impaired, initially, for their partners: a multi-centre, longitudinal study. BMC Nephrol. 2020;21(1).
Wu AW, Fink NE, Marsh-Manzi JV, Meyer KB, Finkelstein FO, Chapman MM, et al. Changes in quality of life during hemodialysis and peritoneal dialysis treatment: generic and disease specific measures. J Am Soc Nephrol. 2004;15(3):743–53.
RAND Corporation. Kidney Disease Quality of Life Instrument (KDQOL)2000. Available from: https://www.rand.org/health-care/surveys_tools/kdqol.html.
Breckenridge K, Bekker HL, Gibbons E, van der Veer SN, Abbott D, Briançon S, et al. How to routinely collect data on patient-reported outcome and experience measures in renal registries in Europe: an expert consensus meeting. Nephrol Dialysis Transplantation. 2015;30(10):1605–14.
Schatell D, Witten B. Measuring Dialysis Patients’ Health-Related Quality of Life with the KDQOL-36TM. KDQOL COMPLETE; 2012 April 16, 2018.
Musselwhite K, Cuff L, McGregor L, King KM. The telephone interview is an effective method of data collection in clinical nursing research: A discussion paper. Int J Nurs Stud. 2007;44(6):1064-70.
Smith EM. Telephone interviewing in healthcare research: a summary of the evidence. Nurse Res. 2005;12(3).
Sturges JE, Hanrahan KJ. Comparing telephone and face-to-face qualitative interviewing: a research note. Qualitative Res. 2004;4(1):107–18.
Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398–405.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77–101.
Chan C, Combes G, Davies S, Finkelstein F, Firanek C, Gomez R, et al. Transition between different renal replacement modalities: gaps in knowledge and care—the Integrated Research Initiative. Perit Dial Int. 2019;39(1):4–12.
Mapes DL, Lopes AA, Satayathum S, McCullough KP, Goodkin DA, Locatelli F, et al. Health-related quality of life as a predictor of mortality and hospitalization: the Dialysis Outcomes and practice patterns study (DOPPS). Kidney Int. 2003;64(1):339–49.
Posegger KR, Linhares MM, Mucci S, Romano TM, Gonzalez AM, Salzedas Netto AA, et al. The quality of life in type I diabetic patients with end-stage kidney disease before and after simultaneous pancreas‐kidney transplantation: a single‐center prospective study. Transpl Int. 2020;33(3):330–9.
Watnick S, Kirwin P, Mahnensmith R, Concato J. The prevalence and treatment of depression among patients starting dialysis. Am J Kidney Dis. 2003;41(1):105–10.
Covic A, Bammens B, Lobbedez T, Segall L, Heimbürger O, Van Biesen W, et al. Educating end-stage renal disease patients on dialysis modality selection. Nephrol Dialysis Transplantation Plus. 2010;3(3):225–33.
Morfín JA, Yang A, Wang E, Schiller B. Transitional dialysis care units: a new approach to increase home dialysis modality uptake and patient outcomes. Semin Dial. 2018;31(1):82–7.
Bowman B, Zheng S, Yang A, Schiller B, Morfín JA, Seek M, et al. Improving incident ESRD care via a transitional care unit. Am J Kidney Dis. 2018;72(2):278–83.
Acknowledgements
The authors are grateful to Georgina Freeman and Jacob Bailey at W21C Research and Innovation Centre who assisted with the initial qualitative data categorization and to Victoria Riehl-Tonn for her assistance with transcription.
Funding
Division of Nephrology, Cumming School of Medicine.
Author information
Authors and Affiliations
Contributions
Research idea and design JM, PR, MS, CD. Data analysis and interpretation JM, DF, CD, MS, PR; statistical analysis CD, DF, PR. Each author contributed important intellectual content during manuscript drafting and revisions.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Conjoint Health Research Ethics Board at the University of Calgary (ID#REB 17-1331). All methods were performed in accordance with the relevant guidelines and regulations. We received informed consent from all participants.
Consent for publication
Not applicable.
Competing interests
All authors have no conflicts to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dumaine, C.S., Fox, D.E., Ravani, P. et al. Health related quality of life during dialysis modality transitions: a qualitative study. BMC Nephrol 24, 282 (2023). https://doi.org/10.1186/s12882-023-03330-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-023-03330-y