Abstract
Purpose
To evaluate the intracavity left ventricular (LV) blood flow kinetic energy (KE) parameters using four-dimensional (4D) flow cardiovascular magnetic resonance (CMR) in patients with acute myocardial infarction (AMI).
Methods
Thirty AMI patients and twenty controls were examined via CMR, which included cine imaging, late gadolinium enhancement (LGE) and global heart 4D flow imaging. The KE parameters were indexed to LV end-diastolic volume (EDV) to obtain average, systolic and diastolic KE as well as the proportion of LV in-plane KE (%). These parameters were compared between the AMI patients and controls and between the two subgroups.
Results
Analysis of the LV blood flow KE parameters at different levels of the LV cavity and in different segments of the same level showed that the basal level had the highest blood flow KE while the apical level had the lowest in the control group. There were no significant differences in diastolic KE, systolic in-plane KE and diastolic in-plane KE between the anterior wall and posterior wall (p > 0.05), only the systolic KE had a significant difference between them (p < 0.05). Compared with those in the control group, the average (10.7 ± 3.3 µJ/mL vs. 14.7 ± 3.6 µJ/mL, p < 0.001), systolic (14.6 ± 5.1 µJ/mL vs. 18.9 ± 3.9 µJ/mL, p = 0.003) and diastolic KE (7.9 ± 2.5 µJ/mL vs. 10.6 ± 3.8 µJ/mL, p = 0.018) were significantly lower in the AMI group. The average KE in the infarct segment was lower than that in the noninfarct segment in the AMI group (49.5 ± 18.7 µJ/mL vs. 126.3 ± 50.7 µJ/mL, p < 0.001), while the proportion of systolic in-plane KE increased significantly (61.8%±11.5 vs. 42.9%±14.4, p = 0.001).
Conclusion
The 4D Flow MRI technique can be used to quantitatively evaluate LV regional hemodynamic parameters. There were differences in the KE parameters of LV blood flow at different levels and in different segments of the same level in healthy people. In AMI patients, the average KE of the infarct segment decreased, while the proportion of systolic in-plane KE significantly increased.
Similar content being viewed by others
Introduction
After acute myocardial infarction (AMI), the myocardial systolic function of the infarct segment is weakened or lost, and left ventricular (LV) contraction becomes asymmetrical. Asymmetric contraction causes the LV wall to experience uneven blood tension, resulting in complex hemodynamic changes that may lead to adverse remodelling and subsequent left heart failure [1,2,3]. The effect of AMI on LV hemodynamic has been confirmed, and the quantification of LV hemodynamic is highly valuable for determining the prognosis of patients with myocardial infarction [4,5,6].
Kinetic energy (KE) represents the energy that blood possess due to its motion and could represent an important hemodynamic parameter to evaluate [7]. The KE of blood flow includes both in-plane and through-plane components. In-plane KE is the sum of all KE values in the horizontal direction of the short axis from the base to the apex of the LV. In contrast, through-plane KE refers to the component of blood flow perpendicular to the short axis of the heart.
Compared with traditional cardiac MRI, 4D Flow MRI can evaluate the blood flow state more comprehensively, so as to help us fully understand the development of the disease. At present, some studies have applied 4D Flow KE parameters to patients with AMI, and found that the in-plane KE of left ventricle increased in the group with decreased ejection fraction [8, 9]. However, a pathological increase in in-plane KE may exert heterogeneous hemodynamic force on the LV wall, which leads to further expansion of the endocardium and increased endothelial dysfunction, and may even be related to the occurrence of complications after myocardial infarction. At present, there are few studies on the kinetic energy of regional blood flow based on 4D Flow MRI. The aim of this study was to analyze the changes in KE parameters of regional blood flow in the cardiac cavity of MI patients and to determine the importance of KE in hemodynamic changes of patients with AMI.
Materials and methods
Study population
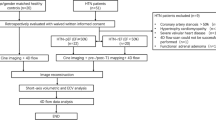
Thirty patients with AMI and twenty age-/sex-matched healthy controls from Cangzhou Central Hospital were retrospectively evaluated between February 2022 and August 2023. The regional ethics committee approved this study (approval number: 2023-222-02), and the requirement for written informed consent was waived.
The inclusion criteria for patients were as follows: a clinical diagnosis of AMI [10]; percutaneous coronary intervention (PCI) performed within 12 h after the onset of chest pain; CMR imaging completed within one week after treatment; and no contraindications for cardiac MRI. The exclusion criteria for patients were as follows: a previous history of vascular reconstruction surgery (coronary artery bypass grafting or PCI); known cardiomyopathy or valvular heart disease; hemodynamic instability lasting more than 24 h after PCI; poor-quality CMR images; or incomplete imaging data [3].
CMR examination
All control subjects and patients were scanned in a 3.0T scanner (MR750, GE Healthcare, Signa Discovery) with a 16-channel phased array coil. All the subjects were trained to hold their breath at the end of expiration, and ECG gating and respiratory gating were monitored.
CMR protocol and image acquisition
The CMR protocol was as follows:
-
1.
The following cines were defined using the survey images: horizontal long-axis, 2-chamber, 4-chamber and the LV volume contiguous short-axis stack.
-
2.
All cines were acquired with a balanced steady-state free precession (bSSFP) procedure. The typical parameters for the bSSFP sequence were as follows: flip angle (FA) 60°, echo time (TE) 1.89 milliseconds, repetition time (TR) 3.74 milliseconds, field of view (FOV) 320–420 mm depending on patient size, slice thickness 8 mm, and 25 phases per cardiac cycle.
-
3.
LGE imaging was performed 15 min after gadolinium-based contrast agent injection in AMI patients only. LGE imaging was performed with a phase sensitive myocardial delayed enhancement (PSMDE) spoiled gradient recalled echo (FSPGR) sequence. The PSMDE sequence details are as follows: TE/TR, 2.46/5.3 msec; FA, 25°.
-
4.
For global heart 4D flow, the field of view (FOV) was planned in the transaxial plane to ensure that the global heart was within the FOV. 4D flow data were acquired with PC VIPR, a 3D radially undersampled, three-directional velocity-encoding technique [11]. Scan parameters captured by 4D Flow MRI as defined in the latest version of the 4D Flow MRI Consensus Statement for 2023 [12]: TE, 2.0 ms; TR, 5.3 ms; FA, 7°; VENC, 150 cm/sec; spatial resolution, 2.5mm3; temporal resolution,30ms.
Image analysis
A GE AW4.7 postprocessing workstation was used to measure cardiac function parameters. The indices of left ventricular volume and cardiac function, including the left ventricular end diastolic volume index (LVEDVi), left ventricular end systolic volume index (LVESVi) and left ventricular ejection fraction (LVEF), which were corrected by body surface area, were obtained.
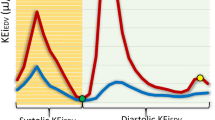
The parameters of KE were analysed using MASS (version 2021-EXP, Medis Medical Imaging). All the images were outlined by a radiologist with 7 years of experience in CMR diagnosis, using automatic tracking technology combined with manual adjustment to outline the endocardium and epicardium of the left ventricle at end diastole and end systole, and were confirmed or adjusted by a radiologist with more than 10 years of experience. The calculation formula for KE was KE = 1/2 ρblood × Vvoxel× v2, where ρblood represents the density of blood (1.06 g/cm3), Vvoxel represents the voxel volume, and v represents the velocity. For each phase, the total KE within the LV was obtained by summing the KE of each voxel, and then the time-resolved KE curve was obtained by summing the KE values of each voxel in the whole cardiac cycle to derive physiologically relevant parameters. In-plane KE was obtained by summing all KE in the short-axis planes from basal to apical LV and is expressed as a percentage of the total LV KE. All KE parameters were indexed to the LVEDV, and the units were µJ/mL (KEiEDV) [13].
An example of left ventricular short-axis KE mapping and CMR in the AMI group, and the arrows refers to the infarction area in the LGE images of AMI patients in the anterior wall. The parameters of the AMI group are as follows: LVEF = 48.9%±13.0, systolic KEiEDV=14.6 ± 5.1µJ/ml, In-plane KE = 32.0%±11.4. LGE: delayed enhancement
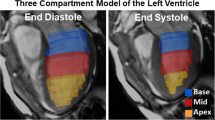
Segmentation method for calculating the regional KE of the LV cavity
MASS automatically quantified the blood flow KE parameters in 16 segments of the heart in all subjects according to American Heart Association standards. In this study, the subjects’ ventricles were divided in equal thirds into base, mid-ventricle and apex, and each level was divided into 4 segments (anterior wall, posterior wall, septal wall and lateral wall). The differences in regional blood flow KE at different levels and in different segments of the same level of the heart cavity in the healthy control group were used as the reference for the AMI group. In the AMI group, the segment with the largest area of myocardial infarction was defined as the infarct segment, and the contralateral myocardium was defined as the noninfarct segment.
Statistical analysis
All analyses were performed using SPSS® Statistics (Version 26.0, International Business Machines). The Shapiro-wilk test was used to evaluate the normal distribution of the data. The normally distributed data are expressed as the mean ± standard deviation (SD), and two-independent sample t tests were used. Categorical data are presented as numbers and proportions and Chi-square test were used. The comparison of different levels and different segments in the control group was performed by one-way ANOVA, and the difference in regional blood flow KE in the AMI group was compared by paired t test or Wilcoxon signed rank sum test. A two-tailed p value of less than 0.05 was considered to indicate statistical significance.
Results
Patient demographic characteristics
There were no significant differences in heart rate (67.1 ± 15.7 beats/min vs. 73.0 ± 8.8 beats/min, P = 0.057) between the AMI patients and the control group. Healthy controls and the AMI group were matched for age (54 ± 9 years vs. 58 ± 9 years, P = 0.133). The CMR volume parameters of the AMI patients were significantly greater than those of the control group, while the LVEF was significantly lower (48.9%±13.0 vs. 67.1%±9.4) (Table 1).
KE parameter results
Total KE of LV blood flow for the two groups
The average LV KEiEDV and systolic and diastolic KE in AMI patients were significantly lower than those in the control group (10.7 ± 3 µJ/ml vs. 14.7 ± 3 µJ/ml, P < 0.01; 14.6 ± 5.1 µJ/ml vs. 18.9 ± 3.9 µJ/ml, P = 0.003; and 7.9 ± 2.5 µJ/ml vs. 10.6 ± 3.8 µJ/ml, P = 0.003, respectively). No significant difference was found in the in-plane KE proportion between the AMI patients and the control group (32.0%±11.4 vs. 30.9%±12.2, P = 0.742) (Table 2; Figs. 1 and 2).
Blood flow KE at different levels in the control group
As shown in Table 3, blood flow KE parameters were different at different levels in the same patient. The average, systolic and diastolic KE in the basal segment (6.7 ± 1.8 µJ/ml, 8.5 ± 2.7 µJ/ml, and 5.4 ± 2.1 µJ/ml, respectively) were significantly greater than those in the middle segment (4.9 ± 2.1 µJ/ml, 5.9 ± 2.6 µJ/ml, and 4.5 ± 2.2 µJ/ml, respectively) and apical segment (1.7 ± 0.6 µJ/ml, 2.0 ± 0.7 µJ/ml, and 1.6 ± 0.6 µJ/ml, respectively), and the values in the apical segment were the lowest (all p < 0.05).
Blood flow KE in different segments in the control group
Comparisons of LV blood flow KE parameters in different segments at the same level in the control group were shown in Table 4; Fig. 3. The systolic KE and systolic in-plane KE were significantly different, while the diastolic KE and diastolic in-plane KE were not significantly different. According to pairwise comparisons of the anterior wall, posterior wall, septal wall and lateral wall, the systolic blood flow KE in the anterior wall and septal wall was significantly greater than that in the contralateral myocardial segment (all P < 0.05). The systolic in-plane KE was not significantly different between the anterior and posterior walls but was significantly different between the septal and lateral walls.
Bar charts of LV flow KEiEDV parameters at different segments of the LV cavity in controls (bars = mean ± sd; error bars = inter-quartile range). Abbreviations are the same as those in Table 4
Regional blood flow KE in the AMI group
In the AMI group, there were 2 cases of anterior wall infarction, 20 cases of posterior wall infarction (14 cases in the basal segment and 6 cases in the middle segment), 5 cases of septal wall infarction, and 3 cases of lateral wall infarction. Because the sample size of patients with anterior and middle posterior wall infarctions was small, this study analysed only the difference of blood flow KE in patients with posterior basal myocardial infarction. As shown in Table 5, the systolic and diastolic KE in the infarct segment were significantly lower than those in the noninfarct segment (49.5 ± 18.7 µJ/ml vs. 126.3 ± 50.7 µJ/ml, P < 0.001; 25.7 ± 9.1 µJ/ml vs. 44.5 ± 21.4 µJ/ml, P = 0.005). However, the proportion of systolic in-plane KE in the infarct segment was greater than that in the noninfarct segment (61.8% ± 11.5 vs. 42.9% ± 12.1, P = 0.001). There was no significant difference in the proportion of diastolic in-plane KE between the infarct and noninfarct segments (53.6% ± 19.0 vs. 43.2% ± 14.4, P = 0.203).
Discussion
Total KE of LV blood flow in the control and AMI groups
The KEiEDV parameter of LV blood flow was decreased in patients with AMI, which was consistent with the results of Pankaj et al. [1] and Kanski et al. [14]. After MI, the regional contractility of the myocardium was reduced, which reduces the regional pressure on the blood in the cavity and the pressure gradient between the LV and the aorta, thus reducing the total thrust of systolic blood flow, which ultimately manifests as a decrease in systolic KE. Another finding of the study by Pankaj Garg also supports this view: the LV stroke volume was related to the KEiEDV only at the end of systole in the infarction group but not in the control group. In addition, Riva’s study also found that the KE of patients in the AMI group was significantly reduced [15].
Blood flow KE at different levels in the control group
Several studies have reported the application of MRI in detecting LV blood flow KE in healthy individuals. However, the current studies on blood flow KE parameters in healthy people have focused mainly on evaluating flow in the global heart chamber, while few studies have evaluated the KE parameters of different segments. In our study of 20 healthy subjects, the KE values at different levels were different: the basal segment had the largest values, while the apex had the smallest values, which may be related to the proximity of the base flow to the left ventricular outflow tract (LVOT). The jet through the aortic valve improved the KE of the basal segment flow. Previous studies have shown that the blood in the LV contains different components during the cardiac cycle; the residual volume refers to the volume that stays at the apex for more than one cardiac cycle, and the KE of the residual volume is small. Corrado’s research also revealed that the volume through the apex was significantly reduced [16].
Blood flow KE in different segments of the control group
In this study, analysis of the blood flow KE in different segments at the same level in the control group showed no statistically significant differences in the diastolic KE, systolic in-plane KE or diastolic in-plane KE between the anterior and posterior walls of the heart cavity. The difference in blood flow KE between the septal and lateral walls was statistically significant only for diastolic KE and diastolic in-plane KE. Therefore, we preliminarily concluded that the blood flow KE parameters between the anterior and posterior walls were similar. To compare the regional blood flow in the myocardial infarction group, we focused on analysing the anterior and posterior wall blood flow.
LV blood flow has a complex motion and hemodynamic characteristics [17,18,19,20]. The statistically significant difference in systolic KE between the anterior and posterior walls in the control group may be related to the presence of an asymmetric vortex in the heart cavity during systole. Goya studied the characteristics of the LV systolic vortex in healthy dogs and reported that the systolic vortex in the posterior basal region had larger vorticity than in the anterior region, this phenomenon can provide reference value for the statistically significant difference in systolic KE between anterior and posterior wall cardiac blood flow in healthy control group [21].
Regional blood flow KE in the AMI group
The blood flow KE in the infarct segment was lower than that in the noninfarct segment in AMI patients, and the proportion of in-plane KE was increased, which was consistent with Pankaj’s findings [1]. In addition, Arkaet al. [3] reported that patients with adverse ventricular remodelling had increased in-plane KE. The increase in the in-plane KE may be related to pathological blood flow. After MI, LV function was damaged, and the cardiac cavity begins to expand. However, progressive LV impairment and dilatation also cause increased sphericity, which in turn changes flow conditions inside the cavity to a ‘meta-stable’ state with a large, swirling vortex that encompasses the majority of the LV [2]. This vortex flow includes transverse thrusts, which increase the proportion of in-plane KE. In addition, our study revealed that there was no significant difference in diastolic in-plane KE between infarct and noninfarct segments. This finding is consistent with the findings of Arka, which may also be related to changes in diastolic blood flow. Suwa et al. [22] reported that patients with impaired LV function had a greater diastolic vortex than did those with normal LV function.
The purpose of this study is to analyse the changes in KE parameters of regional blood flow in the cardiac cavity of MI patients and to determine whether in-plane KE is highly important in blood flow near the cardiac cavity of the regionally infarcted myocardium. A pathological increase in in-plane KE may exert heterogeneous hemodynamic force on the LV wall, which leads to further expansion of the endocardium and increased endothelial dysfunction [23,24,25,26]. This pathological process may be related to the formation of ventricular aneurysms. Ventricular aneurysm [27]is a common complication of AMI. After infarction, necrotic myocardial cells are gradually replaced by fibrous scar tissue, and the infarcted myocardium becomes thinner and bulges outwards, possibly leading to abnormal movement during contraction. To date, there is a lack of research on the relationship between hemodynamic parameters and ventricular aneurysm formation in MI patients. Prospective studies are needed in the future, which may provide hemodynamic insights into the pathophysiology of remodelling after myocardial infarction.
Study limitations
First, this was a single-centre study with a small sample size. Second, the infarct sites of patients with AMI included in this study were not exactly in the same segment, so the KE between adjacent segments may have an impact. Therefore, the sample size should be expanded for further study to comprehensively evaluate cardiac hemodynamic changes in AMI patients.
Conclusions
This study provides a methodological reference for the regional analysis of LV flow parameters via 4D Flow MRI. Differences in the KE parameters at different levels and in different segments of the same level in the LV cavity were found in healthy people. In AMI patients, the average KE in the infarct segment decreased, while the proportion of in-plane KE increased. This was a preliminary study analysing regional LV blood flow KE, and further exploration is needed to determine whether regional LV blood flow KE has predictive value for AMI.
Data availability
All data generated or analysed during this study are included in this published article.
References
Pankaj G, Crandon S, Swoboda PP, et al. Left ventricular blood flow kinetic energy after myocardial infarction - insights from 4D flow cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2018;20:61.
Pedrizzetti G, Canna GL, Alfieri O, Tonti G. The vortex–an early predictor of cardiovascular outcome? Nat Rev Cardiol. 2014;11:545–53.
Arka D, Kelly C, Ben-Arzi H, Geest RJVD, Plein S, Dall’Armellina E. Acute intra-cavity 4D flow cardiovascular magnetic resonance predicts long-term adverse remodelling following ST-elevation myocardial infarction. J Cardiovasc Magn Reson. 2022;24:64.
Yamamoto K, Nishimura RA, Chaliki HP, Appleton CP, Holmes DRJ, Redfield MM. Determination of left ventricular filling pressure by doppler echocardiography in patients with coronary artery disease: critical role of left ventricular systolic function. J Am Coll Cardiol. 1997;30:1819–26.
Nucifora G, Delgado V, Bertini M, Marsan NA, Veire NRVD, Arnold CTN, Siebelink HM, Schalij MJ, Holman ER, Sengupta PP, Bax JJ. Left ventricular muscle and fluid mechanics in acute myocardial infarction. Am J Cardiol. 2010;106:1404–09.
Møller JE, Whalley GA, Dini FL, Doughty RN, Gamble GD, Klein AL, Quintana M, Yu CM. Independent prognostic importance of a restrictive left ventricular filling pattern after myocardial infarction: an individual patient meta-analysis: Meta-Analysis Research Group in Echocardiography acute myocardial infarction. Circulation. 2008;117:2591–8.
Qin JJ, Indja B, Gholipour A, Gök M, Grieve SM. Evaluation of left ventricular function using four-dimensional flow cardiovascular magnetic resonance: a systematic review. J Cardiovasc Dev Dis. 2022;9:304.
Garg P, Crandon S, Swoboda PP et al. Left ventricular blood flow kinetic energy after myocardial infarction - insights from 4D flow cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2018;20.
Garg P, van der Geest RJ, Swoboda PP, et al. Left ventricular thrombus formation in myocardial infarction is associated with altered left ventricular blood flow energetics. Eur Heart J - Cardiovasc Imaging. 2019;20:108–17.
Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012;60:1581–98.
Corrado PA, Macdonald JA, François CJ, Aggarwal NR, Weinsaft JW, Wieben O. Reduced regional flow in the left ventricle after anterior acute myocardial infarction: a case control study using 4D flow MRI. BMC Med Imaging. 2019;19:101.
Bissell MM, Raimondi F, Ait Ali L et al. 4D Flow cardiovascular magnetic resonance consensus statement: 2023 update. J Cardiovasc Magn Reson. 2023;25.
Peng K, Zhang X, Hua T, Wan L, Xiao F, Zhang X, Liu Y, Xu Y, Tang H, Wang S, Tang G. Evaluation of left ventricular blood flow kinetic energy in patients with hypertension by four-dimensional flow cardiovascular magnetic resonance imaging: a preliminary study. Eur Radiol. 2023;33:4676–87.
Kanski M, Arvidsson PM, Töger J, Borgquist R, Heiberg E, Carlsson M, Arheden H. Left ventricular fluid kinetic energy time curves in heart failure from cardiovascular magnetic resonance 4D flow data. J Cardiovasc Magn Reson. 2015;17:111.
Riva A, Sturla F, Pica S, et al. Comparison of Four-Dimensional Magnetic Resonance Imaging Analysis of Left Ventricular Fluid Dynamics and Energetics in ischemic and restrictive cardiomyopathies. J Magn Reson Imaging. 2022;56:1157–70.
Corrado PA, Macdonald JA, François CJ, Aggarwal NR, Weinsaft JW, Wieben O. Reduced regional flow in the left ventricle after anterior acute myocardial infarction: a case control study using 4D flow MRI. BMC Med Imaging. 2019;19.
Bertini M, Nucifora G, Marsan NA, Delgado V, Bommel RJV, Boriani G, Biffi M, Holman ER, Wall EEVD, Schalij MJ, Bax JJ. Left ventricular rotational mechanics in acute myocardial infarction and in chronic (ischemic and nonischemic) heart failure patients. Am J Cardiol. 2009;103:1506–12.
Burns AT, Gerche AL, Prior DL, Macisaac AI. Left ventricular untwisting is an important determinant of early diastolic function. JACC Cardiovasc Imaging. 2009;2:709–16.
Sengupta PP, Khandheria BK, Narula J. Twist and untwist mechanics of the left ventricle. Heart Fail Clin. 2008;4:315–24.
Mele D, Smarrazzo V, Pedrizzetti G, Capasso F, Pepe M, Severino S, Luisi GA, Maglione M, Ferrari R. Intracardiac flow analysis: techniques and potential clinical applications. J Am Soc Echocardiogr. 2019;32:319–32.
Goya S, Wada T, Shimada K, Hirao D, Tanaka R. The relationship between systolic vector flow mapping parameters and left ventricular cardiac function in healthy dogs. Heart Vessels. 2018;33:549–60.
Suwa K, Saitoh T, Takehara Y, et al. Intra-left ventricular flow dynamics in patients with preserved and impaired left ventricular function: analysis with 3D cine phase contrast MRI (4D-Flow). J Magn Reson Imaging. 2016;44:1493–503.
Eriksson J, Zajac J, Alehagen U, Bolger AF, Ebbers T, Carlhäll CJ. Left ventricular hemodynamic forces as a marker of mechanical dyssynchrony in heart failure patients with left bundle branch block. Sci Rep. 2017;7:2971.
Eriksson J, Bolger AF, Ebbers T, Carlhäll CJ. Assessment of left ventricular hemodynamic forces in healthy subjects and patients with dilated cardiomyopathy using 4D flow MRI. Physiol Rep. 2016;4:e12685.
Arvidsson PM, Töger J, Carlsson M, Steding-Ehrenborg K, Pedrizzetti G, Heiberg E, Arheden H. Left and right ventricular hemodynamic forces in healthy volunteers and elite athletes assessed with 4D flow magnetic resonance imaging. Am J Physiol Heart Circ Physiol. 2017;312:H314–28.
Pedrizzetti G, Arvidsson PM, Töger J, Borgquist R, Domenichini F, Arheden H, Heiberg E. On estimating intraventricular hemodynamic forces from endocardial dynamics: a comparative study with 4D flow MRI. J Biomech. 2017;60:203–10.
Subramanian K, Mahdi R, Singh H, Sood A, Mittal BR. Perfusion defect with characteristic anterior wall indentation on myocardial perfusion imaging caused by a large left ventricular aneurysm. J Nucl Cardiol. 2023;30:2809–12.
Acknowledgements
Not applicable.
Funding
This study was supported by the Medical Science Research Project of Hebei Province in China in 2024 (Approval number: 20241752), and chaired by Fenghai Liu.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Xiqing Niu, Yutong Dun, Guoce Li, Houning Zhang, Bin Zhang, Zhibin Pan, Hao Bian, Liqing Kang. The first draft of the manuscript was written by Xiqing Niu and all authors commented on previous versions of the manuscript. The manuscript was reviewed by Fenghai Liu. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was a retrospective study and was approved by the Cangzhou Central Hospital Medical Ethics Committee and exempted from informed consent.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of the images in Figure(s) 1 and 2.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Niu, X., Dun, Y., Li, G. et al. Evaluation of left ventricular blood flow kinetic energy in patients with acute myocardial infarction by 4D Flow MRI: a preliminary study. BMC Med Imaging 24, 131 (2024). https://doi.org/10.1186/s12880-024-01310-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12880-024-01310-8