Abstract
Background
This study aimed to develop and validate an AI (artificial intelligence)-aid method in myocardial perfusion imaging (MPI) to differentiate ischemia in coronary artery disease.
Methods
We retrospectively selected 599 patients who had received gated-MPI protocol. Images were acquired using hybrid SPECT-CT systems. A training set was used to train and develop the neural network and a validation set was used to test the predictive ability of the neural network. We used a learning technique named “YOLO” to carry out the training process. We compared the predictive accuracy of AI with that of physician interpreters (beginner, inexperienced, and experienced interpreters).
Results
Training performance showed that the accuracy ranged from 66.20% to 94.64%, the recall rate ranged from 76.96% to 98.76%, and the average precision ranged from 80.17% to 98.15%. In the ROC analysis of the validation set, the sensitivity range was 88.9 ~ 93.8%, the specificity range was 93.0 ~ 97.6%, and the AUC range was 94.1 ~ 96.1%. In the comparison between AI and different interpreters, AI outperformed the other interpreters (most P-value < 0.05).
Conclusion
The AI system of our study showed excellent predictive accuracy in the diagnosis of MPI protocols, and therefore might be potentially helpful to aid radiologists in clinical practice and develop more sophisticated models.
Similar content being viewed by others
Background
Coronary artery disease (CAD) is one of the leading causes of morbidity and mortality throughout the world [1]. According to the report released by the American Heart Association (AHA) in 2016, over 15.5 million people above 20 years of age suffer from CAD in the United States [2]. Currently, imaging methods regarding CAD diagnosis include electrocardiography [3], invasive coronary angiography (ICA) or non-invasive tomographic coronary angiography (CTCA) [4, 5], myocardial perfusion imaging (MPI) [6], ultrasonography [7], etc. All these methods have been proved to be effective. Among them, MPI with single-photon emission computer tomography (SPECT) is a well-established non-invasive test in terms of the evaluation of ischemia, scar, left ventricular volumes, and ejection fraction, by directly reflecting the tracer uptake of the heart [8]. With advances during the past few years, MPI has certainly evolved from a diagnostic test of high accuracy for the detection of CAD (reportedly with mean sensitivity and specificity of 90% and 75%, respectively) to an essential tool for risk stratification [9, 10].
Traditionally, the interpretation of medical imaging requires one’s sufficient knowledge in the medical-related domains [11], which needs decades of training. Clinically, this interpretation process can also be time-consuming. Simultaneously, patients have been demanding faster and more personalized care [12, 13]. The resultant shortage of physicians and the requirement for efficiency emerged thereafter. Inspiringly, artificial intelligence (AI, or machine learning) is poised to influence nearly every aspect of human life, especially in the medical field. These years, the combination of AI and medical imaging has been remaining as a hot topic and there is presently sufficient evidence demonstrating its practicability (e.g. AI with ultrasound, computed tomography, magnetic resonance imaging, or histopathology) [14,15,16,17]. However, the application of AI in nuclear medicine imaging and, in particular, MPI can be troublesome. Firstly, MPI images are multi-slices rather than planer images and the interpretation is mostly based on the information seen in multiple slices [18]. Secondly, the interpretation also relies on the agreement of images from various axes (i.e., short-axis, horizontal long-axis, vertical long-axis, and polar map) [19, 20]. These issues might hamper the establishment of an AI-aid diagnostic system in MPI. According to our limited knowledge, approaches to these problems are yet scarce, and we herein introduce an AI-aid method to detect ischemic abnormalities in MPI.
Materials and methods
Sample collection
We retrospectively selected 599 patients from the participating medical centers, and among them, 379 (63.27%) cases were males and 220 (36.73%) cases were females. All patients had received gated-MPI protocol using 99mTc-sestamibi. Images were acquired using four hybrid SPECT-CT systems including (Discovery NM/CT 670 CZT, GE Healthcare; Discovery NM 530c, GE Healthcare; Symbia T16, Siemens Corp.). Acquisition parameters were as follows:
-
1)
Discovery NM/CT 670 CZT: 64 × 64 matrix size; 1.3 zoom; 30 secs per view (30 views in total); 140 keV ± 10% main energy window; 120 kVp CT tube voltage; 20 mA tube current; 1.25 mm slice thickness.
-
2)
Discovery NM 530c: 64 × 64 matrix size; no zoom; 30 secs per frame (48 frames in total); 140 keV ± 10% main energy window; without CT acquisition.
-
3)
Symbia T16: 64 × 64 matrix size; 1.45 zoom; 16 secs per view (32 views in total); 140 keV ± 10% main energy window; without CT acquisition.
Reconstruction parameters were as follows:
-
All images were reconstructed using FBP algorithm with Butterworth filter (critical frequency: 0.45 ~ 0.50). The correction methods used in the reconstruction process included CT-based AC (Discovery NM/CT 670 CZT), and dual-energy-window technique-based SC.
-
Individuals’ MPI images were pulled out for preparation. The mean diagnostic age was 59.14-year-old with a standard deviation of ± 11.61. All patients had or were suspected to have CAD-related presentations prior to the SPECT scan. MPI images consisted of three conventional axes: short-axis (SA, 13,267 slices), horizontal long-axis (HLA, 11,465 slices), and vertical long-axis (VLA, 11,676 slices). Patients were divided into two subsets including a training set and a validation set. By doing so, firstly, images of all patients were indexed in sequence and therefore 13,267 slices of SA, 11,465 slices of HLA, and 11,676 slices of VLA were totally indexed. Secondly, with these index numbers, we then separated these images randomly before training using Python software (version 3.7.3). The training set was then used to train and develop the following neural network accounting for 70% (each axis), and the validation set was used to test the predictive ability of the neural network accounting for 30% (each axis).
Machine learning network selection
Machine learning strategies can be generally split into either unsupervised or supervised learning. The main scope of unsupervised learning is to discover underlying structure or relationships among variables in a dataset, whereas supervised learning normally requires the classification of one or more categories or outcomes [21]. Due to the particularity of medical images which often requires the evaluation of multiple categories, in this study, we selected the supervised learning method-regional deep learning technique, an ROI (region of interest)-based conventional neural network named YOLO (you only look once, version 3), [22] to complete the training. The YOLO algorithm was composed of four main stages: preprocessing of the tagged images, feature extraction utilizing deep convolutional networks (training), lesion detection with confidence (calculating), and finally lesion classification using fully connected neural networks (FC-NNs, output) [23]. Machine learning network was implemented using Python software.
Tagging method for CAD-suspected lesions
Images were tagged in accordance with the standardized myocardial segmentation and nomenclature for tomographic imaging of heart proposed by the ATA in 2002 [24]. Therefore, a total of 17 tags (from the basal to the apical) were applied in the tagging process (Fig. 1). If a lesion was identified to exist in the apex wall, we delineate that area with a tag “17” in all three axes (i.e. SA, HLA, and VLA). Accordingly, if a lesion was detected in the non-apical segment like the mid inferior wall, we give that area a tag “10” both in SA and VLA. In the input process of training, images of three axes were sent to the model separately and therefore a total of three sub-models were trained and then incorporated into one model. When detecting ischemia, these sub-models will give three independent results based on the ischemic area. A program named “labelme” under the Anaconda environment was used in this tagging step.
Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. a short-axis; b horizontal long-axis; c vertical long-axis; 1, basal anterior; 2, basal anteroseptal; 3, basal inferoseptal; 4, basal inferior; 5, basal inferolateral; 6, basal anterolateral; 7, mid anterior; 8, mid anteroseptal; 9, mid inferoseptal; 10, mid inferior; 11, mid inferolateral; 12, mid anterolateral; 13, apical anterior; 14, apical septal; 15, apical inferior; 16, apical lateral; 17, apex
Statistical analysis
The age distribution of patients was tested using the Kolmogorov–Smirnov method. The lesion distribution of the 17 segments among SA, HLA, and VLA was tested using the Chi-square test. A P-value < 0.05 was considered to be statistically significant.
Validation of the neural network
To test the training performance of the neural network, we calculated the average precision and recall rate. Additionally, in order to test its general clinical accuracy, ROC analysis was applied using the validation set. The gold standard was set as the diagnostic report made by an agreement of two experienced interpreters with at least 30 years of high-volume medical-related background (expert). We also randomly selected 100 slices (random validation set) of each axis and compared the statistical differences of sensitivity, specificity among AI, beginner (with 1 week of training, intern), inexperienced interpreter (with 5 years of medical-related background, resident physician), and experienced interpreter, by using McNemar’s test [25]. To test the consistency between AI and the gold standard, a consistency check was also performed by calculating Cohen’s Kappa coefficients. Lastly, to evaluate the diagnostic speed of AI, we performed a time consumption analysis between AI and experienced interpreters based on 60 patients selected from the validation set. We compared the distribution and statistical differences in terms of time consumption between them. All statistics were derived by using SPSS 23.0 (IBM, USA) and a P-value < 0.05 was considered to be statistically significant.
Results
Patient and lesion distribution
Overall, there was a normal distribution in both the male group and female group (all P-value > 0.05). Also, the diagnostic age of females was older than that of males (distribution peak at around 65-year-old for the female group and around 55-year-old for the male group). As shown in Table 1 and Fig. 2, SA accounted for the majority of lesions among all three axes (24,539 for SA vs. 3,978 for HLA vs. 9,479 for VLA). Additionally, for each axis, statistically significant differences were derived among different segments (all P-value < 0.001). Among different segments, segment 4 (inferior) accounted for the majority in SA (22.20%), segment 17 (apical) accounted for the majority in HLA (49.52%), and segment 4 accounted for the majority in VLA (22.73%) (Table 1 and Fig. 2). In comparison, segment 6 (anterolateral) accounted for the minority in SA (11.79%), segment 14 (septal) accounted for the minority in HLA (24.46%), and segment 1 accounted for the minority in VLA (6.08%) (Table 1 and Fig. 2).
Lesion distribution among three axes. SA, Short axis; HLA, Horizontal long axis; VLA, Vertical long axis; 1, Anterior for SA (Basal anterior for VLA); 2, Anteroseptal; 3, Interseptal; 4, Inferior for SA (Basal inferior for VLA); 5, Inferolateral; 6, Anterolateral; 7, Mid anterior; 10, Mid inferior; 13, Apical anterior, 14, Septal; 15, Apical inferior; 16, Lateral; 17, Apical
Metrics of accuracy, recall, and precision in the training set
In SA, accuracy ranged from 74.37% to 84.73%, recall rate ranged from 94.04% to 98.76%, and average accuracy ranged from 90.04% to 98.15% (Table 2). The accuracy, recall rate, and average precision of segment 4 were larger than those of other segments (84.73%, 98.76%, and 98.15%, respectively).
In HLA, the range of accuracy was 66.20% ~ 79.32%, the range of recall rate was 88.50% ~ 92.77%, and the range of average accuracy was 81.90% ~ 90.34% (Table 3). Among segments 14, 17, and 16, segment 17 had the largest accuracy (79.32%), recall rate (92.77%), and average precision (90.34%), whereas segment 14 had the smallest numbers (66.20% for accuracy, 88.50% for recall rate, and 81.90% for average precision).
In VLA, the range of accuracy was 88.02% ~ 94.64%, the range of recall rate was 76.96% ~ 91.8%, and the range of average accuracy was 80.17% ~ 93.37 (Table 4). The greatest accuracy was found in segment 17 (94.64%), whereas the greatest recall rate and average precision were found in segment 1 (91.80% and 93.37%, respectively). In addition, the smallest accuracy was found in segment 15(87.91%) and the smallest recall rate and average precision were found in segment 13 (76.96% and 80.17%, respectively).
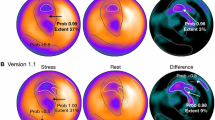
Validation of the neural network
Figure 3 was an example predicted by AI and segments of all lesions were identified accurately. In ROC analysis of the validation set, sensitivity, specificity, and AUC of SA were 93.8%, 97.6%, and 94.1%, respectively (Fig. 4a). The sensitivity, specificity, and AUC of HLA were 88.9%, 93.0%, and 94.3%, respectively (Fig. 4b). The sensitivity, specificity, and AUC of VLA were 91.7%, 96.8%, and 96.1%, respectively (Fig. 4c).
As demonstrated in Fig. 5, when comparing both sensitivity and specificity with those of AI, all interpreters showed statistically significant differences in the random validation set (all P-value < 0.05). Table 5 showed the comparison of sensitivity among AI, beginner, inexperienced, and experienced interpreters in the random validation set. The beginner had the largest sensitivity in the SA (99.15%, 95% CI: 97.33 ~ 99.78%), HLA (98.35%, 95% CI: 94.87 ~ 99.57%), and VLA (98.30%, 95% CI: 96.14 ~ 99.31%). However, there was no statistically significant difference between the beginner and AI in SA. The sensitivity of the experienced interpreter was larger than that of AI in HLA and there was a statistically significant difference (P-value < 0.001), but lower than those of AI in both SA and VLA (P-value of SA < 0.05, P-value of VLA > 0.05). In comparison, the inexperienced interpreter had the lowest sensitivity among all interpreters in both SA and VLA and there were statistically significant differences when comparing with AI (P-value < 0.001). However, in terms of the HLA axis, it had the same sensitivity as the experienced interpreter.
As shown in Table 6, the beginner had the smallest specificities in all three axes (4.17% in SA, 8.57% in HLA, 1.66% in VLA), and there were statistically significant differences compared with AI (all P-value < 0.001). Conversely, AI had the largest specificities in SA (98.61%, 95% CI: 91.46 ~ 99.93%), HLA (94.29%, 95% CI: 85.27 ~ 98.15%), and VLA (97.24%, 95% CI: 93.33 ~ 98.98%).Although the inexperienced interpreter and the experienced interpreter had the same specificity in SA, it could be noticed that the specificities of the experienced interpreter were larger than those of the inexperienced interpreter in HLA and VLA. Additionally, the specificities of both the inexperienced and experienced interpreters had statistically significant differences (all P-value < 0.05).
Consistency check showed that AI had the best agreement with the gold standard in all three axes (Cohen’s Kappa coefficients: 0.943 for SA, 0.754 for HLA, and 0.905 for VLA, all P-value < 0.001, Table 7). Likewise, the beginner had the smallest agreement with the gold standard (Cohen’s Kappa coefficients: 0.052 for SA, 0.095 for HLA, and 0.013 for VLA; P-value of SA and HLA < 0.05, P-value of VLA > 0.05). Cohen’s Kappa coefficients of the experienced interpreter were smaller than those of AI but larger than those of the inexperienced interpreter (0.712 vs. 0.447 for SA, 0.804 vs. 0.662 for HLA, and 0.827 vs. 0.630 for VLA, all P-value < 0.001).
In the time consumption analysis of the selected dataset, it took AI 1673.23 s in SA, 1698.41 s in HLA, and 1715.08 s in VLA to generate diagnoses, whereas it took the experienced interpreter 2348.67 s in SA, 2162.89 s in HLA, and 2352.98 s in VLA to give final prognoses. Also, the average time consumption of AI per axis was much less compared with that of the experienced interpreter (Supplementary Table 1). Figure 6 shows that AI completed the detective process mostly between 20 and 40 s in three axes. However, those numbers ranged largely from 20 to 60 s for the experienced interpreter.
Discussion
Due to the shortage of large-scale publicly available datasets containing SPECT images for the detection of CAD, the application of deep learning has not been thoroughly explored. This study described a clinical application of an AI-aid system with explainable predictions tested in a large, multicenter population with gated-MPI protocols. This system demonstrated significantly high predictive accuracy and clinical availability in all three axes.
Among all cardiovascular diseases, CAD is a major cause of morbidity and mortality among adults worldwide and brings a heavy burden for the patients and their families [26]. In our cohort, more male patients received gated-MPI protocols (63.27% males vs. 36.73% females). This might be explained by the hypothesis that women often present with atypical symptoms and therefore continue to delay seeking treatment [27]. On the whole, the diagnostic age of CAD in females was larger than that of males (distribution peak at around 65-year-old for females and around 55-year-old for males). The increased number of elderly female patients might need targeted care.
The 17-segment model of the left ventricle, as an optimally weighted approach for the visual interpretation of regional left ventricular abnormalities, has been widely used since it was proposed. In terms of the correspondence between left ventricular 17 myocardial segments and coronary arteries, segments 1, 2, 7, 8, 13, 14, and 17 are assigned to the left anterior descending coronary artery distribution. Segments 3, 4, 9, 10, and 15 are assigned to the right coronary artery when it is dominant. Segments 5, 6, 11, 12, and 16 generally are assigned to the left circumflex artery [28]. Based on the research of Juillière, Y., et al., the most common segments of ischemia could be segment 1(anterior), segment 4 (inferior), and segment 17 (apical) [29]. Our study also revealed a similar distribution (15.52% for segment 1, 20.01% for segment 4, 9.07% for segment 17). The higher abnormality ratio of segment 4 in our study might be explained by the higher involvement ratio of stenosis in the right coronary artery, compared with those of the left anterior descending coronary artery or the left circumflex artery. Likewise, in a clinical trial of 215 patients conducted by Nordlund, D., et al., 39%of patients had left anterior descending artery occlusion, 49% had right coronary artery occlusion, and 12% had left circumflex artery occlusion [30]. This was also consistent with the distribution of our analysis.
In SA, the training accuracy, recall rate, as well as average precision of segment 4 were larger than those of other segments (84.73%, 98.76%, and 98.15%, respectively, Table 2). In HLA, segment 17 had the largest accuracy (79.32%), recall rate (92.77%), and average precision (90.34%), compared with other segments (Table 3). Similarly, the greatest accuracy was found in segment 17 (94.64%) and the greatest recall rate and average precision were found in segment 1 of VLA (91.80% and 93.37%, respectively, Table 4). The higher accuracy seen in these segments might be contributed from the relatively larger number of lesions among these segments in the training set (segment 4 accounted for 22.20% in SA, segment 17 accounted for 49.52% in HLA, and 15.56% in VLA, Table 1). This indicated that a large number of lesions is essential for AI to extract enough features and subsequently increase the training accuracy of algorithm architecture. Some researchers also concluded that datasets with adequate sample size are one of the dominant factors in developing and training effective computer-aided diagnosis algorithms [31, 32].
Apostolopoulos, I.D., et al. [33] proposed a method for automatic classification of polar maps based on a neural network named VGG16. The proposed model achieved a sensitivity of about 75.00% and a specificity of about 73.43%. Arsanjani, R., et al. [34] introduced a Support Vector Machine (SVM) algorithm in their study to predict the detection of ≥ 70% coronary artery lesions and their research yielded both relatively good sensitivity (84%) and specificity (88%) during validation. Betancur, J., et al. [35] developed an automatically predictive model to identify obstructive heart disease using deep learning and also achieved a good accuracy (AUC: 0.76 ~ 0.80). However, these studies did not incorporate different axes of the heart from MPI images as targeted training.
The results of our work highlight the capabilities of deep learning for classification tasks of nuclear medicine imaging. On the validation set, sensitivity, specificity, as well as AUC of all axes were all above 90% except for the sensitivity of HLA. On the random validation set, AI outperformed the beginner, the inexperienced interpreter, as well as the experienced interpreter, since it achieved both relatively larger sensitivities and specificities in all three axes (most P-value < 0.05, Tables 5 and 6). In terms of the comparison with the experienced interpreter, the proposed AI-aid system yielded a relatively equivalent performance of sensitivity. On the whole, the beginner had the largest sensitivities in all three axes (98.30 ~ 99.15%, Table 5). However, specificities in these axes were extremely low (1.66 ~ 8.57%). This suggested that the beginner could identify most of the ischemic lesions, but it resulted from the price of a large amount of false-positive lesions. Clinically, this situation must be avoided. However, even with a short period of training, this situation was not observed with AI, and therefore, this again confirmed the fact that AI, if with a proper design, has the intrinsically efficient learning capability in the classification of medical imaging. It could also be noticed that AI also had the best agreement in all axes (Cohen’s Kappa coefficients: 0.943 for SA, 0.754 for HLA, and 0.905 for VLA). These results suggest that the YOLO network, though an endeavor in our study, can be used as a promising approach in nuclear medicine. Several studies also confirmed the availability of it in medical imaging, since it offers an excellent tradeoff between accuracy and efficiency [22, 36, 37].
There were three limitations to our study. First, since this was a retrospective study, acquisition parameters of different SPECT systems in different institutions had already been fixed to obtain good performance and could be adjusted to the exact same settings before model training. This might hamper the accuracy of the model to some extent but improve its robustness simultaneously. However, to minimize the impact of the input data, we did use same reconstruction parameters to reconstruct these SPECT images. Second, the gold standard was set as the diagnostic report made by an agreement of two experienced interpreters because of the dilemma that not every patient received coronary angiography during hospitalization on the one hand, and more MPI images were preferred to be used in the AI training process on the other hand. Third, due to the relatively limited number of lesions in the HLA, both sensitivity and specificity were inevitably lower than other axes in terms of the random validation set. Lower accuracy in some of the segments seen in this study might be partially be addressed by using a larger cohort in the next stage of our study. Last, the extent of ischemia was not included in our training because too many tags require much more samples in the training set. To achieve good accuracy in terms of both segment and extent of ischemia, further larger datasets will surely be required.
Conclusion
The AI system of our study showed excellent predictive accuracy, agreement, clinical availability, and efficiency in a large, multicenter population with gated-MPI protocols and therefore, might be potentially helpful to aid radiologists in clinical practice and develop more sophisticated models.
Availability of data and materials
All datasets and materials used and/or analyzed during the current study are available from the corresponding authors on any reasonable request.
Abbreviations
- AI:
-
Artificial intelligence
- MPI:
-
Myocardial perfusion imaging
- CAD:
-
Coronary artery disease
- AHA:
-
American heart association
- ICA:
-
Invasive coronary angiography
- SPECT:
-
Single-photon emission computer tomography
- SA:
-
Short-axis
- HLA:
-
Horizontal long-axis
- VLA:
-
Vertical long-axis
- ROI:
-
Region of interest
- YOLO:
-
You only look once
- SVM:
-
Support vector machine
References
Malakar AK, Choudhury D, Halder B, Paul P, Uddin A, Chakraborty S. A review on coronary artery disease, its risk factors, and therapeutics. J Cell Physiol. 2019;234(10):16812–23.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38-360.
Sonecha TN, Delis KT. Prevalence and distribution of coronary disease in claudicants using 12-lead precordial stress electrocardiography. Eur J Vasc Endovasc Surg. 2003;25(6):519–26.
Williams MC, Hunter A, Shah A, Assi V, Lewis S, Mangion K, et al. Symptoms and quality of life in patients with suspected angina undergoing CT coronary angiography: a randomised controlled trial. Heart (British Cardiac Society). 2017;103(13):995–1001.
Van Mieghem CA, Thury A, Meijboom WB, Cademartiri F, Mollet NR, Weustink AC, et al. Detection and characterization of coronary bifurcation lesions with 64-slice computed tomography coronary angiography. Eur Heart J. 2007;28(16):1968–76.
Patel KK, Al Badarin F, Chan PS, Spertus JA, Courter S, Kennedy KF, et al. Randomized Comparison of Clinical Effectiveness of Pharmacologic SPECT and PET MPI in Symptomatic CAD Patients. JACC Cardiovasc Imaging. 2019;12(9):1821–31.
Irie Y, Katakami N, Kaneto H, Nishio M, Kasami R, Sakamoto K, et al. The utility of carotid ultrasonography in identifying severe coronary artery disease in asymptomatic type 2 diabetic patients without history of coronary artery disease. Diabetes Care. 2013;36(5):1327–34.
Nudi F, Iskandrian AE, Schillaci O, Peruzzi M, Frati G, Biondi-Zoccai G. Diagnostic accuracy of myocardial perfusion imaging with CZT technology: systemic review and meta-analysis of comparison with invasive coronary angiography. JACC Cardiovasc Imaging. 2017;10(7):787–94.
Loong CY, Anagnostopoulos C. Diagnosis of coronary artery disease by radionuclide myocardial perfusion imaging. Heart (British Cardiac Society). 2004;90 Suppl 5(Suppl 5):2–9.
Underwood SR, Shaw LJ, Anagnostopoulos C, Cerqueira M, Ell PJ, Flint J, et al. Myocardial perfusion scintigraphy and cost effectiveness of diagnosis and management of coronary heart disease. Heart (British Cardiac Society). 2004;90 Suppl 5(Suppl 5):v34-6.
Shameer K, Badgeley MA, Miotto R, Glicksberg BS, Morgan JW, Dudley JT. Translational bioinformatics in the era of real-time biomedical, health care and wellness data streams. Brief Bioinform. 2017;18(1):105–24.
Steinhubl SR, Topol EJ. Moving from digitalization to digitization in cardiovascular care: why is it important, and what could it mean for patients and providers? J Am Coll Cardiol. 2015;66(13):1489–96.
Boeldt DL, Wineinger NE, Waalen J, Gollamudi S, Grossberg A, Steinhubl SR, et al. How consumers and physicians view new medical technology: comparative survey. J Med Internet Res. 2015;17(9): e215.
Akkus Z, Cai J, Boonrod A, Zeinoddini A, Weston AD, Philbrick KA, et al. A survey of deep-learning applications in ultrasound: artificial intelligence-powered ultrasound for improving clinical workflow. J Am Coll Radiol. 2019;16(9 Pt B):1318–28.
Winkel DJ, Heye T, Weikert TJ, Boll DT, Stieltjes B. Evaluation of an ai-based detection software for acute findings in abdominal computed tomography scans: toward an automated work list prioritization of routine CT examinations. Invest Radiol. 2019;54(1):55–9.
Sheth D, Giger ML. Artificial intelligence in the interpretation of breast cancer on MRI. J Magn Reson Imaging. 2020;51(5):1310–24.
Colling R, Pitman H, Oien K, Rajpoot N, Macklin P, Snead D, et al. Artificial intelligence in digital pathology: a roadmap to routine use in clinical practice. J Pathol. 2019;249(2):143–50.
Kirişli HA, Gupta V, Shahzad R, Al Younis I, Dharampal A, Geuns RJ, et al. Additional diagnostic value of integrated analysis of cardiac CTA and SPECT MPI using the SMARTVis system in patients with suspected coronary artery disease. J Nucl Med. 2014;55(1):50–7.
Mahmood S, Gunning M, Bomanji JB, Gupta NK, Costa DC, Jarritt PH, et al. Combined rest thallium-201/stress technetium-99m-tetrofosmin SPECT: feasibility and diagnostic accuracy of a 90-minute protocol. J Nucl Med. 1995;36(6):932–5.
Zoccarato O, Marcassa C, Lizio D, Leva L, Lucignani G, Savi A, et al. Differences in polar-map patterns using the novel technologies for myocardial perfusion imaging. J Nucl Cardiol. 2017;24(5):1626–36.
Johnson KW, Torres Soto J, Glicksberg BS, Shameer K, Miotto R, Ali M, et al. Artificial Intelligence in Cardiology. J Am Coll Cardiol. 2018;71(23):2668–79.
Yan Y, Conze PH, Lamard M, Quellec G, Cochener B, Coatrieux G. Towards improved breast mass detection using dual-view mammogram matching. Med Image Anal. 2021;71:102083.
Al-Masni MA, Al-Antari MA, Park JM, Gi G, Kim TY, Rivera P, et al. Simultaneous detection and classification of breast masses in digital mammograms via a deep learning YOLO-based CAD system. Comput Methods Programs Biomed. 2018;157:85–94.
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105(4):539–42.
Hawass NE. Comparing the sensitivities and specificities of two diagnostic procedures performed on the same group of patients. Br J Radiol. 1997;70(832):360–6.
Luo F, Das A, Chen J, Wu P, Li X, Fang Z. Metformin in patients with and without diabetes: a paradigm shift in cardiovascular disease management. Cardiovasc Diabetol. 2019;18(1):54.
Parvand M, Rayner-Hartley E, Sedlak T. Recent developments in sex-related differences in presentation, prognosis, and management of coronary artery disease. Can J Cardiol. 2018;34(4):390–9.
Pereztol-Valdés O, Candell-Riera J, Santana-Boado C, Angel J, Aguadé-Bruix S, Castell-Conesa J, et al. Correspondence between left ventricular 17 myocardial segments and coronary arteries. Eur Heart J. 2005;26(24):2637–43.
Juillière Y, Marie PY, Danchin N, Gillet C, Paille F, Karcher G, et al. Radionuclide assessment of regional differences in left ventricular wall motion and myocardial perfusion in idiopathic dilated cardiomyopathy. Eur Heart J. 1993;14(9):1163–9.
Nordlund D, Heiberg E, Carlsson M, Fründ ET, Hoffmann P, Koul S, et al. Extent of myocardium at risk for left anterior descending artery, right coronary artery, and left circumflex artery occlusion depicted by contrast-enhanced steady state free precession and T2-weighted short tau inversion recovery magnetic resonance imaging. Circ Cardiovasc Imaging. 2016;9(7):e004376.
Morozov SP, Gombolevskiy VA, Elizarov AB, Gusev MA, Novik VP, Prokudaylo SB, et al. A simplified cluster model and a tool adapted for collaborative labeling of lung cancer CT scans. Comput Methods Programs Biomed. 2021;206: 106111.
Kohli MD, Summers RM, Geis JR. Medical Image Data and Datasets in the Era of Machine Learning-Whitepaper from the 2016 C-MIMI Meeting Dataset Session. J Digit Imaging. 2017;30(4):392–9.
Apostolopoulos ID, Papathanasiou ND, Spyridonidis T, Apostolopoulos DJ. Automatic characterization of myocardial perfusion imaging polar maps employing deep learning and data augmentation. Hell J Nucl Med. 2020;23(2):125–32.
Arsanjani R, Xu Y, Dey D, Fish M, Dorbala S, Hayes S, et al. Improved accuracy of myocardial perfusion SPECT for the detection of coronary artery disease using a support vector machine algorithm. J Nucl Med. 2013;54(4):549–55.
Betancur J, Commandeur F, Motlagh M, Sharir T, Einstein AJ, Bokhari S, et al. Deep learning for prediction of obstructive disease from fast myocardial perfusion SPECT: a multicenter study. JACC Cardiovasc Imaging. 2018;11(11):1654–63.
Al-Antari MA, Han SM, Kim TS. Evaluation of deep learning detection and classification towards computer-aided diagnosis of breast lesions in digital X-ray mammograms. Comput Methods Programs Biomed. 2020;196:105584.
Loey M, Manogaran G, Taha MHN, Khalifa NEM. Fighting against COVID-19: a novel deep learning model based on YOLO-v2 with ResNet-50 for medical face mask detection. Sustain Cities Soc. 2021;65:102600.
Acknowledgements
The authors thank Dr. Shen Wang, who had always been a source of encouragement and inspiration.
Funding
This research was funded by the National Natural Science Foundation of China grants (#81571709 and #81971650), the Key Project of Tianjin Science and Technology Committee Foundation grant (#16JCZDJC34300), and the Tianjin Medical University General Hospital youth incubation Foundation (ZYYFY2016032). The funding bodies played no role in the design of the study and collection, analysis, interpretation of data, and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
This is a multicenter study, all authors played an important role in this research. Specific contributions are listed as follows: RZ and PW conceived the idea for this study. RZ and PW designed the study. YB, YF, JL, Xu. L, JS, YH, Xi. L, XW, MS, and JZ retrieved the raw data, reconstructed the original MPI images, cropped, resized, and formatted all these images for the next stage of data analysis. HW, CS, and WL developed and modified the diagnostic network. MW, Sh. W, YS, XZ, Se. W, LX, and WW provided significant help in the interpretation process as well as in the tagging process of data. WZ and ZM evaluated the methods and derived results. QJ, JT, NL, WZ, and ZM obtained the funding and contributed significantly to the original study design and subsequent modification during the implementation of this study. RZ analyzed the data and wrote the first draft. All authors reviewed the analyses and drafts of this manuscript and approved its final version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The studies involving human participants were reviewed and approved by the Institutional Review Board and Ethics Committee of Tianjin Medical University General Hospital (ethical approval number: IRB2022-004–01). The patients/participants provided their written informed consent to participate in this study. We confirm that all methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Table 1. Timeconsumption (seconds) of AI and experienced interpreter.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, R., Wang, P., Bian, Y. et al. Establishment and validation of an AI-aid method in the diagnosis of myocardial perfusion imaging. BMC Med Imaging 23, 84 (2023). https://doi.org/10.1186/s12880-023-01037-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12880-023-01037-y