Abstract
Introduction
Tuberculosis (TB), caused by Mycobacterium tuberculosis, remains a significant global health threat. It results in substantial mortality and may be underrecognized due to insufficient screening and diagnostic challenges. Furthermore, TB’s impact is closely linked to complex socioeconomic and healthcare factors. The COVID-19 pandemic has exacerbated these challenges due to similarities in clinical presentation and transmission dynamics with TB. Socioeconomic factors such as limited access to healthcare services, resource constraints, and social stigma further complicate TB management. Historically, TB faced increased burdens during natural disasters, wars, and pandemics. This study analyzes TB incidence changes, emphasizing the crucial need for timely diagnosis within the context of COVID-19 measures.
Method
This cross-sectional study, conducted at Shiraz’s TB referral center in Southern Iran, covered the period from January 1, 2018, to December 31, 2022. We analyzed patient data, including epidemiological and demographic factors, clinical and radiological features, and treatment outcomes. Data were compared between the pre-COVID-19 pandemic era and the COVID-19 pandemic era (from March 2020), using standard and regression analyses. A P-value of less than 0.05 was considered statistically significant.
Results
We analyzed 388 TB patients with a mean age of 48.38 ± 20.53 years, including 264 pulmonary cases (68.0%). The highest incidence of TB was recorded in 2019, representing 27.6% of the cases. During the COVID-19 era, logistic regression analysis identified significant associations with higher education levels (P = 0.032; OR = 1.380; 95% CI: 1.028–1.851), a decrease in symptoms such as sputum production (P = 0.004; OR = 0.342; 95% CI: 0.166–0.705) and chills (P = 0.036; OR = 0.282; 95% CI: 0.087–0.919), and an increase in symptoms of fatigue (P = 0.006; OR = 2.856; 95% CI: 1.358–6.005).
Conclusion
The COVID-19 pandemic has had a prolonged impact on TB cases in our country, resulting in a reduction in reported cases due to challenges in quarantine and screening. However, it has also led to a shift in TB patterns and a potential increase in latent TB cases and future mortality rates. Addressing the repercussions requires enhanced control strategies, prioritized service delivery, and secured funding for intensified case finding, expanded contact-tracing, community engagement, digital health tools, and uninterrupted access to medications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the ever-evolving landscape of global health challenges, Tuberculosis (TB) remains one of the most contagious and hazardous diseases, influenced by a complex array of interconnected factors [1]. This holds especially true in developing countries such as Iran, where the nature of the disease adds layers of complexity to its prevalence and patterns. TB’s reach extends beyond microbial dynamics, intertwining with socioeconomic, geopolitical, and healthcare realities unique to the region. Healthcare workers in low- and middle-income countries are particularly at risk of contracting tuberculosis, with several reports documenting a substantial burden and predominantly poor outcomes among these workers [2,3,4,5].
In 2015, the TB incidence rate in Iran was 16 per 100,000 people, decreasing to 14 per 100,000 in 2016 and 2017 [6,7,8]. The cost of treating a new smear-positive TB patient is approximately USD 1,409 [9]. A 2019 systematic review and meta-analysis found that healthcare workers in northern and western Iran had the highest prevalence of latent TB, which is asymptomatic and controlled by the immune system [10, 11]. Iran’s extensive borders with high TB-burden countries—such as Azerbaijan, Turkmenistan, Armenia, Pakistan, Afghanistan, and Iraq—combined with increased immigration and travel, complicate efforts to control TB [12,13,14,15,16,17].
For policymakers, clinicians, and the public health community, understanding the nature of TB is not merely an academic pursuit but a crucial imperative. As we delve into the intricate dance of variables shaping TB’s course in this endemic setting, it becomes clear that effective policies, informed clinical practices, and targeted public health interventions must continually adapt to keep pace with the shifting dynamics of this resilient infectious disease. In this context, the COVID-19 pandemic has undoubtedly been one of the most influential factors affecting TB management, incidence, and patterns. This influence extends from similarities in clinical and paraclinical features and transmission methods to social stigma and changes in healthcare adaptations such as social distancing, quarantines, and hospital policies [18].
Throughout history, TB has faced increased burdens due to disruptions from natural disasters, wars, and infectious pandemics. The Russian flu of 1889 and the Spanish influenza of 1918 increased TB-related mortality [19]. During both World Wars, TB was attributed to a quarter of the deaths [20]. The HIV pandemic in 1980 saw TB as an opportunistic infection leading to widespread mortality [21]. Additionally, outbreaks such as the 2001 Severe Acute Respiratory Syndrome (SARS) in Hong Kong, the 2013–2016 Ebola outbreak in West Africa, and the 2014 Middle East Respiratory Syndrome Coronavirus (MERS-CoV) in Saudi Arabia impacted TB programs, escalating disease burden and mortality in the affected regions in the following years [22,23,24].
he responses to TB and COVID-19 involve complex interactions across various levels of prevention, diagnosis, and treatment [25,26,27,28,29]. A modeling analysis from the STOP TB Partnership indicates that the COVID-19 pandemic is severely disrupting TB services, impacting prevention, detection, and treatment efforts [30]. This disruption is most noticeable in resource-limited settings but also affects wealthier regions [30]. As a result, future increases in TB incidence and mortality are expected, potentially jeopardizing progress and delaying the goals of the End TB Strategy [30]. The potential use of platforms like Xpert for TB diagnosis offers benefits, but during the COVID-19 emergency, there is a risk that existing diagnostic equipment may be redirected away from TB. Protective gear is essential for laboratory personnel handling viral samples [25, 26]. Cough is a key symptom for diagnosing TB, but its presence alongside other symptoms like fever complicates distinguishing TB from COVID-19 and other respiratory infections, especially in the absence of effective diagnostic tools [25]. Physical distancing measures may hinder active case finding and community-based TB and HIV management in high-burden areas, though they could help reduce TB transmission, as seen with influenza [27, 31, 32]. Additionally, both clinical and programmatic TB treatment approaches, including drug procurement, particularly for second-line drugs, may be adversely affected. The anticipated economic crisis post-COVID-19 may exacerbate poverty, social unrest, and malnutrition, further increasing TB incidence and mortality [33,34,35].
Tadolini et al. [25] reported the first cohort among 49 active TB and COVID-19 co-infection cases, in which 38.8% of patients, COVID-19 appeared during anti-TB treatment, potentially due to inadequate protection against SARS-CoV-2, which also impacted two healthcare workers. Diagnoses of TB and COVID-19 were made either simultaneously or within seven days in nine patients, complicating differential diagnosis; clinical assessments for COVID-19 might have facilitated the identification of pre-existing TB, although the role of COVID-19 in TB pathogenesis remains unclear. In 14 patients, COVID-19 was diagnosed before TB, highlighting the need for larger studies to explore if SARS-CoV-2 affects the progression of latent TB to active disease. Symptoms overlap may have led to earlier COVID-19 diagnosis, potentially revealing TB at an earlier stage. Additionally, seven patients with TB sequelae developed COVID-19, presenting higher mortality rates and multiple comorbidities, underscoring the need for further research into the impact of TB sequelae. The pandemic has also significantly impacted the healthcare system, particularly affecting hospital admissions and ICU capacity. Data on BCG vaccination are limited, with information available for only 30 patients, of whom 19 had been previously vaccinated; therefore, no definitive conclusions about its protective role can be drawn. Furthermore, there is currently no data available on drug–drug interactions.
Given the similarities in clinical presentations and transmission methods between COVID-19 and TB, it is crucial not to neglect timely TB diagnosis, especially in the context of the COVID-19 pandemic, which involves quarantine and self-isolation. The decline in routine care center visits and also misdiagnose of Coronavirus instead of TB may lead to under diagnose of actual TB prevalence rates and isolating rules and quarantine could aid in breaking the transmission chain of mycobacterium tuberculosis. Our previous research explored the potential impact of the COVID-19 pandemic on TB [18]. Based on our primary hypothesis and concerns, we analyzed changes in TB patterns and presentations before and after the COVID-19 era. We also aim to highlight how the COVID-19 pandemic and associated policies have affected TB patterns in our province. By examining these aspects, our research provides valuable insights into managing and preventing both TB and COVID-19, offering a nuanced understanding that will help address future public health challenges in infectious disease management.
Material and method
This cross-sectional study was conducted at the TB referral center in Shiraz, Southern Iran, from January 1, 2018, to December 31, 2022. Our center is the primary treatment facility for TB cases in the province. All patients diagnosed with TB, including those with concurrent HIV infection, are documented and followed up. Inclusion criteria included all patients with a confirmed diagnosis of TB, according to the WHO and national TB standard diagnostic guidelines [36], including pulmonary smear results or radiological/clinical features suggestive of TB, during the specified period. There were no age restrictions or specific exclusion criteria for this study.
Patient data were extracted from their records and included epidemiological and demographic factors, clinical and radiological features, and treatment outcomes Patient information was anonymized by removing identifying details, and each patient was assigned a unique number to ensure confidentiality.
Data were entered into SPSS version 26.0 for analysis. Normally distributed variables were reported as means with standard deviations (SD), non-normally distributed variables as medians with interquartile ranges (IQR), and categorical variables as percentages (%). The Chi-square test was used for evaluating categorical variables, while the independent t-test and analysis of variance (ANOVA) were used for continuous variables with normal distribution. The Mann-Whitney U test and Kruskal-Wallis test were used for continuous variables with non-normal distribution. Bonferroni correction was applied for pairwise comparisons in the ANOVA test for continuous variables. Data were compared between the pre-COVID-19 pandemic era and the COVID-19 pandemic era (from March 2020 to the end of the study). Logistic regression analysis was performed to assess associations between dependent variables and the factors evaluated in our study. 95% confidence intervals (95% CI) were calculated for all applicable estimates. Missing data were addressed using appropriate imputation techniques, and valid percentages/values were reported to ensure the robustness of the analysis. A P-value of less than 0.05 was considered statistically significant.
Results
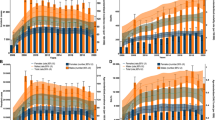
Our study covered the period from January 1, 2018, to December 31, 2022, encompassing five years. During this period, a total of 388 patients with a confirmed diagnosis of TB were included, with a mean age of 48.38 ± 20.53 years. Of these patients, 233 (60.2%) were male and 154 (39.8%) were female. As shown in Fig. 1, the highest number of TB cases occurred in 2019, with 107 cases (27.6%). This was followed by 2018 with 93 cases (24.0%), 2022 with 67 cases (17.3%), 2020 with 61 cases (15.7%), and 2021 with 60 cases (15.5%).
Among the 388 patients in our study, 264 (68.0%) had pulmonary TB, while 124 (32.0%) had extrapulmonary TB, with no cases of concurrent pulmonary and extrapulmonary involvement. For the purpose of our analysis, we focused on pulmonary TB cases and compared their characteristics over the years. Supplementary Table 1 presents a comparison of the epidemiological and clinical features of pulmonary tuberculosis in our study. The lowest number of pulmonary TB cases was observed in 2020, which coincides with the onset of the COVID-19 pandemic in Iran.
Based on the ANOVA test, there was no significant association between the years and the average age of TB patients. However, post-hoc tests revealed that patients in 2021 were significantly older than those in 2018 (P = 0.044) and 2019 (P = 0.030), with no significant difference compared to 2020 (P = 0.057) or 2022 (P = 0.302). There was a significant increase in the proportion of non-Iranian TB patients over the years (P = 0.03).
Significant changes were noted in symptom patterns over time. Notably, there was a relative decrease in hemoptysis and a relative increase in fatigue from 2018 to 2022. Variations were also observed in symptoms such as sputum production, weight loss, dyspnea, and chills. Additionally, significant changes were observed in the X-ray pattern of upper right lung involvement throughout the study period.
We further analyzed data by dividing the study period into pre-COVID-19 (before March 2020) and COVID-19 eras. Among the pulmonary and extrapulmonary TB cases, 216 (55.7%) were identified in the pre-COVID-19 era, while 172 (44.3%) occurred during the COVID-19 era. We compared pulmonary TB cases between these two periods, with results presented in Table 1.
As demonstrated in Table 1, following the COVID-19 pandemic, there was a significant increase in the number of non-Iranian TB cases. Additionally, there was a notable decrease in symptoms such as sputum production, chills, and hemoptysis, while symptoms including weight loss, dyspnea, and fatigue increased. The proportion of abnormal X-rays also rose from 77.9 to 88.2%, and the average treatment duration decreased.
We assessed the trends between the two time points based on the variables included in our study. Logistic regression analysis revealed significant associations with several factors: higher education levels (P = 0.032; OR = 1.380; 95% CI: 1.028–1.851), a decrease in symptoms such as sputum production (P = 0.004; OR = 0.342; 95% CI: 0.166–0.705) and chills (P = 0.036; OR = 0.282; 95% CI: 0.087–0.919), and an increase in symptoms of fatigue (P = 0.006; OR = 2.856; 95% CI: 1.358–6.005).
Discussion
TB is a complex health challenge influenced by diverse factors, exhibiting varied patterns. We previously discussed the potential effects of the COVID-19 pandemic and TB [18], and following our primary hypothesis and concern, we opted to compare the changes in TB pattern and presentations before and after the COVID-19 era, which as demonstrated, aligned with our primary concern that the COVID-19 pandemic caused slight changes in TB patterns.
The first notable change was the decrease in the number of cases during late 2019 and early 2020. Based on the WHO 2023 global tuberculosis report [1], a significant drop of 18% in the incidence of TB cases was observed in 2019 and 2020, following an increase in cases from 2017 to 2019, from 7.1 million to 5.8 million, with a partial recovery to 6.4 million in 2021, and 7.5 million in 2022. The rebound in TB cases in 2022, exceeded the pre-COVID level of 7.1 million cases in 2019, and was characterized as the highest number of newly diagnosed TB cases recorded in a single year. This represented the most significant annual total since the WHO initiated global TB monitoring in the mid-1990s [1]. This pattern corresponds with the pattern of TB cases in our report, with a peak in number of cases in 2019, followed by visible drop in 2020 (by 15.5%) and an increase towards 2022. We believe that this trend may be the result of delayed diagnosis following the COVID-19 pandemic, which covers a considerable backlog of people who developed TB in previous years. However, WHO reported a narrowing of the global gap between TB incidence and newly detected cases from 4 million in 2020 and 2021, to 3.1 million in 2022, which is relatively similar to the pre-pandemic period [1]. Anticipating a rise in TB cases in our province, healthcare workers and policymakers must prioritize effective treatment, early diagnosis, and comprehensive measures to address this emerging public health challenge.
Studies revealed an average 5% decrease in TB mortality rates between 2000 and 2018, in which TB maintained the highest death rate among single infectious pathogenic factors, even surpassing HIV. However, in 2022, this dynamic shifted as TB was surpassed by COVID-19 [1, 37]. As per WHO global reports, an observed decrement of 19% in TB mortality rates spanning the years 2015 to 2022 denotes a noteworthy trend. However, it is crucial to note that this decline, albeit commendable, remains insufficient in meeting the predetermined WHO End TB Strategy milestone of a 75% reduction by the year 2025 [1]. The mortality rate in our study was 7.6%, however the mortality rate did not significantly defer during our study period. However, an intriguing trend emerged when comparing specific years, revealing a decrease from 9.2% in 2019 to 5.1% in 2020 and 5.7% in 2021. This decline may be attributed to the misclassification of TB cases, where individuals, especially those who died before receiving medical care and investigations, who succumbed to TB or other pulmonary symptoms, were inaccurately labeled as COVID-19 cases. This misattribution potentially contributed to the observed reduction in recorded mortality rates. Early detection of TB, especially in multidrug-resistant tuberculosis, is vital [38]. Significance lies in the timely diagnosis, impacting both the individual’s disease prognosis and the potential transmission within the community, thereby influencing the reproductive rate of the TB epidemic [39, 40].
In high-burden areas, tuberculosis deaths could increase by up to 20% over 5 years due to the COVID-19 pandemic. Delays in timely diagnosis and treatment, resulting from prolonged COVID-19 interventions, may lead to a loss of life-years comparable to the direct impact of COVID-19 in regions with significant malaria and HIV/tuberculosis epidemics. Prioritizing critical prevention activities and healthcare services for HIV, tuberculosis, and malaria is vital to mitigate the overall impact of the COVID-19 pandemic [41]. It is evident that age and co-morbidities, such as HIV co-infection, poverty, diabetes, and malnutrition, are key factors influencing mortality in COVID-19, which these determinants also play a role in the mortality associated with TB [42]. Studies also indicate that TB and COVID-19 form a concerning combination, requiring urgent attention. TB should be recognized as a potential contributor to severe cases of COVID-19, and individuals with TB should be given priority in COVID-19 preventive measures, such as vaccination [43].
The emergence of the highly transmissible COVID-19 variants and severe vaccine access disparities—where less than 15% of people in low-income countries had received a dose by March 2022—led to additional COVID-19 waves in 2022 and beyond. Without a global vaccination effort, LMICs struggled to control the pandemic effectively [44]. As a result, the impact of COVID-19 on tuberculosis exceeded previous predictions, underscoring ongoing global neglect and making it unlikely that the End TB Strategy targets will be met by 2030 [45]. A study by Migliori et al. in 2020 reported that TB services across 43 centers in 19 countries experienced significant disruptions due to the COVID-19 pandemic [29]. The total number of TB cases dropped from 32,898 in 2019 to 16,396 in 2020, with a sharp decline beginning in March 2020, coinciding with lockdowns in many countries. This decline was observed globally, except in Australia, Singapore, and Virginia. Similarly, drug-resistant TB cases decreased from 4,717 in 2019 to 1,527 in 2020, starting in March, and TB-related hospital discharges also fell dramatically after an initial increase in early 2020. TB deaths decreased overall but rose in May 2020, possibly due to misattribution to COVID-19 or under-reporting. Newly diagnosed TB cases in outpatient clinics fell from 7,364 in 2019 to 5,703 in 2020, with a notable drop in March 2020. Despite fewer outpatient visits, telehealth usage surged in 2020, reflecting adaptations to pandemic-related challenges. Diagnoses of TB infection and the number of tests performed also declined. The study also evaluated the impact of COVID-19 on TB services across 19 countries in 2020, compared to 2019, found a significant decrease in both TB cases and drug-resistant TB diagnoses [29]. This decline is attributed to reduced access to care, lockdowns, and delayed reporting. While most countries, especially those with high TB burden, experienced these reductions, Australia and Virginia (USA) reported a modest increase in TB notifications due to enhanced surveillance [46,47,48]. Even in countries with low TB incidence, such as Italy, France, and Spain, TB cases declined. The drop in TB deaths in 2020 was accompanied by an increase in May and July, likely due to misattribution to COVID-19 and other issues like under-reporting. Telehealth services increased significantly in response to distancing measures [49]. The study highlights the severe disruptions in TB care caused by the pandemic and emphasizes the need to reallocate resources to prepare for a potential TB resurgence.
The reduction of TB in Iran has been significantly influenced by free treatment, heightened public awareness, improved hygiene practices, the establishment of new TB research centers, and enhanced access to faster and more accurate TB diagnostics [50]. TB healthcare services and centers in our province were still active during the COVID-19 pandemic, while this was not the case in many other countries where healthcare personnel engaged in TB management have been redeployed to address the COVID-19 emergency. Findings from 33 centers across 16 countries on five continents revealed a decline in attendance at tuberculosis centers during the initial four months of the 2020 pandemic compared to the same timeframe in 2019. Resource allocation was one of the most vital aspects of the pandemic to guarantee the uninterrupted provision of tuberculosis care throughout the ongoing pandemic [51]. Even brief interruptions can result in sustained rises in TB incidence and mortality. The WHO and specialized scientific publications anticipate a detrimental impact of the COVID-19 pandemic on the global TB epidemic [7, 52, 53]. This is attributed to increased strain on healthcare systems due to COVID-19, potentially weakening National TB programs [28]. Cilloni et al.‘s modeling analysis suggests that a 50% reduction in TB transmission during lockdowns, followed by a 3-month service suspension and 10-month recovery, may lead to an extra 1.19 million TB cases and 361,000 deaths in India over 5 years. Kenya could see 24,700 cases and 12,500 deaths, and Ukraine, 4,350 cases and 1,340 deaths. The buildup of undetected TB during lockdowns is a major concern. Rapid restoration of TB services and implementing targeted “catch-up” interventions post-lockdown are vital for preventing long-term increases in TB burden and mitigating negative consequences of disruptions [54].
Political commitment, strategic planning, community mobilization, and research and development are essential in combating both TB and COVID-19. Effective TB control relies on sustainable treatment programs, while addressing pandemics like COVID-19 requires robust emergency response capabilities. Prompt action to manage COVID-19 at early stages can enhance preparedness and resource allocation [55]. Efficient triage and isolation of cases help optimize healthcare resources, prevent system overload, and control epidemic spread [28]. Shortages of staff, protective equipment, tests, and drugs are longstanding issues in TB management, and these challenges have now extended to other programs and systems due to COVID-19. The pandemic is expected to impact lung health significantly, potentially leading to a rise in TB cases in the coming years. It has already caused delays in achieving the End-TB Strategy goals, necessitating increased focus and investment in TB control [56]. On the other hand, COVID-19 is transforming TB management by accelerating the adoption of digital innovations that ease the workload of healthcare workers [56]. The pandemic has also highlighted existing vulnerabilities in TB management, underscoring the need for innovation and digital solutions to address these issues and regain momentum in TB control efforts [56].
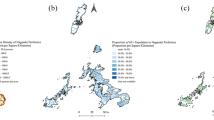
The surge in TB cases in Iran has been a subject of concern, and our research has revealed a noteworthy increase in non-Iranian TB patients throughout the years. Particularly, a substantial proportion of immigrants in Iran originate from Afghanistan, a country with a high incidence of TB, including neighboring Pakistan, which ranks among the nations with the highest TB cases globally. A spatio-temporal study in Pakistan identified northern and western regions as high-risk TB clusters, areas that share borders with eastern and southeastern Iran [57]. Previous research in Iran’s have shown that Afghan and Pakistani immigrants significantly contribute to TB incidence [58,59,60]. A study by Doosti et al. in Iran also reported that 12% of their TB cases were from Afghanistan [61]. Furthermore, previous studies have indicated that 97.1% of non-Iranian TB cases were among Afghan immigrants, with significant TB rates observed in Fars, Yazd, and Khorasan provinces due to Afghan immigration for treatment [62, 63]. This trend intensified during the COVID-19 pandemic, as more immigrants sought medical care at our provincial referral centers, driven by the availability of affordable medications and the lack of adequate healthcare in their home regions. The influx of individuals from these regions may contribute significantly to the rise in TB cases in Iran. Understanding and addressing the implications of immigration on TB transmission is crucial for developing targeted public health interventions to mitigate the impact of this infectious disease in the context of population movement. This insight underscores the importance of cross-border collaboration and comprehensive strategies to manage and prevent tuberculosis transmission, particularly among vulnerable immigrant populations.
Many factors may influence the trend and prevalence of TB cases, such as pulmonary TB has shown to be influenced by seasonality changes in previous studies, showing the highest incidence in late spring to early summer in Iran [64, 65]. A study from our province, Fars, also demonstrated a peak in incidence during warm seasons, specifically in May and June [66]. This was also in line with our findings, which as demonstrated in Fig. 1, a relatively increase in number of cases is observed during the warm seasons, especially May and June. One reason of this occurrence may be due to the compromised immune function resulting from insufficient vitamin D during colder seasons [67, 68]. Although in normal circumstances, the relatively elevated sun exposure during cold seasons in Fars province arises a question regarding whether vitamin D deficiency plays a role in the seasonal patterns observed in pulmonary tuberculosis, however, the enforced quarantine due to the COVID-19 pandemic may contribute to this theory.
Due to stringent physical-distancing measures, many avoided seeking medical care, fearing SARS-CoV-2 exposure in healthcare settings. Facilities noted fewer patients adhering to treatment schedules during lockdowns, posing risks for TB control and drug-resistant TB development [69]. Reallocating resources to control COVID-19 may have inadvertently affected TB diagnosis and treatment [52]. Overlapping respiratory symptoms between the two diseases, such as cough and difficulty breathing, could hinder TB diagnosis, as patients with respiratory symptoms are prioritized for COVID-19 screening. Yet, these overlapping symptoms might expedite access to imaging services, potentially revealing pre-existing TB during COVID-19 evaluation. In the context of clinical diagnosis, symptoms of TB and COVID-19 often overlap [70]. Additionally, COVID-19 can occur during TB treatment or reveal subclinical TB, a common scenario in TB-endemic regions [45]. In our assessment of clinical features, we observed a notable shift in symptoms reported by patients during the COVID-19 pandemic compared to the pre-COVID era. Specifically, there has been a significant decrease in patients presenting with symptoms such as sputum production and chills. Conversely, there has been an increase in cases characterized by fatigue, a symptom that is less specific and may have been underreported or overlooked. This change can be attributed to the heightened public awareness and extensive dissemination of information regarding COVID-19 symptoms, in which during the pandemic, patients with symptoms were more likely to seek medical attention due to the widespread concern about viral infections. As a result, cases of TB that presented with less characteristic symptoms, such as fatigue, or even asymptomatic have become more noticeable. This shift underscores the impact of the pandemic on the detection and diagnosis of TB, highlighting a tendency for atypical TB presentations to be identified more frequently as patients and healthcare providers adapted to the evolving clinical landscape.
Currently, in the post-pandemic period, Iran has eased stringent COVID-19 quarantine measures, moving towards more targeted interventions and preventive strategies. Our study serves multiple purposes: it underscores the immediate impact of COVID-19 on TB incidence and stresses the critical need for timely TB diagnosis amid pandemic-induced disruptions. Furthermore, we acknowledge the importance of addressing post-pandemic TB trends, particularly latent TB cases.
Conclusion
Our study demonstrates that the COVID-19 pandemic has had a prolonged impact on TB cases in our country. We observed a significant reduction in TB case numbers, attributed to decreased transmission during quarantine, challenges in screening, potential misdiagnosis, and fewer healthcare center visits. Given these trends, we anticipate an increase in TB mortality rates and latent TB cases in the coming years. To mitigate the effects of the pandemic on TB and protect the progress made over the past decade, it is essential to enhance TB control strategies. This includes prioritizing service delivery, securing funding for intensified case finding, expanding contact tracing, engaging communities to maintain awareness of TB symptoms and vaccination, leveraging digital health tools for remote TB management, and ensuring uninterrupted access to medications and diagnostics. Securing dedicated funding and mobilizing resources are crucial for addressing the challenges posed by the COVID-19 pandemic. Further research and cost-effectiveness assessments are needed to determine the most effective strategies for managing TB and other infectious diseases during emergency situations.
Data availability
All data regarding this study has been reported in the manuscript. Please contact the corresponding author if you are interested in any further information.
References
Global Tuberculosis Report. 2023 [https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2023]
Jarand J, Shean K, O’Donnell M, Loveday M, Kvasnovsky C, Van der Walt M, Adams S, Willcox P, O’Grady J, Zumla A, et al. Extensively drug-resistant tuberculosis (XDR-TB) among health care workers in South Africa. Tropical Med Int Health. 2010;15(10):1179–84.
Tudor C, Van der Walt M, Margot B, Dorman SE, Pan WK, Yenokyan G, Farley JE. Tuberculosis among health care workers in KwaZulu-Natal, South Africa: a retrospective cohort analysis. BMC Public Health. 2014;14(1):1–9.
O’Donnell MR, Jarand J, Loveday M, Padayatchi N, Zelnick J, Werner L, Naidoo K, Master I, Osburn G, Kvasnovsky C, et al. High incidence of Hospital admissions with Multidrug-resistant and extensively drug-resistant tuberculosis among South African Health Care workers. Ann Intern Med. 2010;153(8):516–22.
Joshi R, Reingold AL, Menzies D, Pai M. Tuberculosis among health-care workers in low- and middle-income countries: a systematic review. PLoS Med. 2006;3(12):e494.
Nasiri MJ, Dabiri H, Darban-Sarokhalil D, Rezadehbashi M, Zamani S. Prevalence of drug-resistant tuberculosis in Iran: systematic review and meta-analysis. Am J Infect Control. 2014;42(11):1212–8.
Organization WH. Global tuberculosis report 2013: World health organization; 2013.
Organization WH. Global hepatitis report 2017. World Health Organization; 2017.
Bay V, Tabarsi P, Rezapour A, Marzban S, Zarei E. Cost of Tuberculosis Treatment: evidence from Iran’s Health System. Osong Public Health Res Perspect. 2017;8(5):351–7.
YektaKooshali MH, Movahedzadeh F, Foumani AA, Sabati H, Jafari A. Is latent tuberculosis infection challenging in Iranian health care workers? A systematic review and meta-analysis. PLoS ONE. 2019;14(10):e0223335.
Proenca R, Mattos Souza F, Lisboa Bastos M, Caetano R, Braga JU, Faerstein E, Trajman A. Active and latent tuberculosis in refugees and asylum seekers: a systematic review and meta-analysis. BMC Public Health. 2020;20(1):838.
Basnyat B, Caws M, Udwadia Z. Tuberculosis in South Asia: a tide in the affairs of men. Multidiscip Respir Med. 2018;13:10.
Abbas J, Aman J, Nurunnabi M, Bano S. The Impact of Social Media on Learning Behavior for Sustainable Education: evidence of students from selected universities in Pakistan. Sustainability. 2019;11(6):1683.
Abbas J, Aqeel M, Abbas J, Shaher B, Sundas AJ, Zhang J. The moderating role of social support for marital adjustment, depression, anxiety, and stress: evidence from Pakistani working and nonworking women. J Affect Disord. 2019;244:231–8.
Karadakhy K, Othman N, Ibrahimm F, Saeed AA, Amin AAH. Tuberculosis in Sulaimaniyah, Iraqi Kurdistan: a detailed analysis of cases registered in Treatment centers. Tanaffos. 2016;15(4):197–204.
Farnia P, Mohammadi F, Masjedi MR, Varnerot A, Zarifi AZ, Tabatabee J, Douraghei M, Ghazisaeedi K, Mansorri D, Bahadori M, et al. Evaluation of tuberculosis transmission in Tehran: using RFLP and spoloigotyping methods. J Infect. 2004;49(2):94–101.
Asgharzadeh M, Shahbabian K, Samadi Kafil H, Rafi A. Use of DNA fingerprinting in identifying the source case of tubercolosis in East Azarbaijan province of Iran. J Med Sci. 2007;7(3):418–21.
Shahriarirad R, Fallahi MJ. TB and the COVID-19 pandemic: brothers in arms against lung health. Int J Tuberc Lung Dis. 2020;24(10):1126–7.
Zurcher K, Zwahlen M, Ballif M, Rieder HL, Egger M, Fenner L. Influenza pandemics and tuberculosis mortality in 1889 and 1918: analysis of historical data from Switzerland. PLoS ONE. 2016;11(10):e0162575.
Vynnycky E, Fine PE. Interpreting the decline in tuberculosis: the role of secular trends in effective contact. Int J Epidemiol. 1999;28(2):327–34.
Corbett EL, Watt CJ, Walker N, Maher D, Williams BG, Raviglione MC, Dye C. The growing burden of tuberculosis: global trends and interactions with the HIV epidemic. Arch Intern Med. 2003;163(9):1009–21.
Ichikawa M, Nakahara S, Wakai S, Hong-Jen C, Huang N. Lowered Tuberculosis notifications and deterred health care seeking during the SARS epidemic in Hong Kong/Chang and Huang respond. Am J Public Health. 2005;95(6):933.
Delamou A, Delvaux T, El Ayadi AM, Beavogui AH, Okumura J, Van Damme W, De Brouwere V. Public health impact of the 2014–2015 Ebola outbreak in West Africa: seizing opportunities for the future. BMJ Glob Health. 2017;2(2):e000202.
Alfaraj SH, Al-Tawfiq JA, Altuwaijri TA, Memish ZA. Middle East Respiratory Syndrome Coronavirus and Pulmonary Tuberculosis Coinfection: implications for infection control. Intervirology. 2017;60(1–2):53–5.
Tadolini M, Codecasa LR, Garcia-Garcia JM, Blanc FX, Borisov S, Alffenaar JW, Andrejak C, Bachez P, Bart PA, Belilovski E et al. Active tuberculosis, sequelae and COVID-19 co-infection: first cohort of 49 cases. Eur Respir J 2020, 56(1).
Motta I, Centis R, D’Ambrosio L, Garcia-Garcia JM, Goletti D, Gualano G, Lipani F, Palmieri F, Sanchez-Montalva A, Pontali E, et al. Tuberculosis, COVID-19 and migrants: preliminary analysis of deaths occurring in 69 patients from two cohorts. Pulmonology. 2020;26(4):233–40.
Organization WH. World Health Organization (WHO) information note tuberculosis and COVID-19. Geneva: World Health Organization; 2020.
Ong CWM, Migliori GB, Raviglione M, MacGregor-Skinner G, Sotgiu G, Alffenaar JW, Tiberi S, Adlhoch C, Alonzi T, Archuleta S et al. Epidemic and pandemic viral infections: impact on tuberculosis and the lung: a consensus by the World Association for Infectious Diseases and Immunological disorders (WAidid), Global Tuberculosis Network (GTN), and members of the European Society of Clinical Microbiology and Infectious Diseases Study Group for Mycobacterial Infections (ESGMYC). Eur Respir J 2020, 56(4).
Migliori GB, Thong PM, Alffenaar JW, Denholm J, Tadolini M, Alyaquobi F, Blanc FX, Buonsenso D, Cho JG, Codecasa LR et al. Gauging the impact of the COVID-19 pandemic on tuberculosis services: a global study. Eur Respir J 2021, 58(5).
Stop T. Partnership; Imperial College; Avenir Health; Johns Hopkins University; USAID. The potential impact of the Covid-19 response on tuberculosis in high-burden countries: a modelling analysis Geneva. Stop TB Partnership; 2020.
Soo RJJ, Chiew CJ, Ma S, Pung R, Lee V. Decreased influenza incidence under COVID-19 Control measures, Singapore. Emerg Infect Dis. 2020;26(8):1933–5.
Kuo SC, Shih SM, Chien LH, Hsiung CA. Collateral benefit of COVID-19 Control measures on Influenza Activity, Taiwan. Emerg Infect Dis. 2020;26(8):1928–30.
Saunders MJ, Evans CA. Fighting poverty to prevent tuberculosis. Lancet Infect Dis. 2016;16(4):395–6.
Carter DJ, Glaziou P, Lonnroth K, Siroka A, Floyd K, Weil D, Raviglione M, Houben R, Boccia D. The impact of social protection and poverty elimination on global tuberculosis incidence: a statistical modelling analysis of sustainable development goal 1. Lancet Glob Health. 2018;6(5):e514–22.
Migliori GB, Garcia-Basteiro AL. Predicting the effect of improved socioeconomic health determinants on the tuberculosis epidemic. Lancet Glob Health. 2018;6(5):e475–6.
Organization WH. WHO consolidated guidelines on tuberculosis. Module 3: diagnosis–rapid diagnostics for tuberculosis detection. World Health Organization; 2024.
Wang Y, Xu C, Ren J, Wu W, Zhao X, Chao L, Liang W, Yao S. Secular seasonality and Trend forecasting of tuberculosis incidence rate in China using the Advanced Error-Trend-Seasonal Framework. Infect Drug Resist. 2020;13:733–47.
Nardell E, Dharmadhikari A. Turning off the spigot: reducing drug-resistant tuberculosis transmission in resource-limited settings. Int J Tuberc Lung Dis. 2010;14(10):1233–43.
Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. JAMA. 1999;282(7):677–86.
Bjune G. Tuberculosis in the 21st century: an emerging pandemic? Norsk Epidemiologi 2005, 15(2).
Hogan AB, Jewell BL, Sherrard-Smith E, Vesga JF, Watson OJ, Whittaker C, Hamlet A, Smith JA, Winskill P, Verity R, et al. Potential impact of the COVID-19 pandemic on HIV, Tuberculosis, and malaria in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8(9):e1132–41.
Visca D, Ong CWM, Tiberi S, Centis R, D’Ambrosio L, Chen B, Mueller J, Mueller P, Duarte R, Dalcolmo M, et al. Tuberculosis and COVID-19 interaction: a review of biological, clinical and public health effects. Pulmonology. 2021;27(2):151–65.
Group TC-GS. Tuberculosis and COVID-19 co-infection: description of the global cohort. Eur Respir J. 2022;59(3):2102538.
Pai M, Olatunbosun-Alakija A. Vax the world. In., vol. 374: American Association for the Advancement of Science; 2021: 1031–1031.
Dheda K, Perumal T, Moultrie H, Perumal R, Esmail A, Scott AJ, Udwadia Z, Chang KC, Peter J, Pooran A, et al. The intersecting pandemics of tuberculosis and COVID-19: population-level and patient-level impact, clinical presentation, and corrective interventions. Lancet Respir Med. 2022;10(6):603–22.
Migliori GB, Tiberi S, Garcia-Basteiro AL, Duarte R. Tuberculosis and its future in the COVID-19 era: the Pulmonology series 2021. Pulmonology. 2021;27(2):94–6.
Akkerman O, Aleksa A, Alffenaar JW, Al-Marzouqi NH, Arias-Guillen M, Belilovski E, Bernal E, Boeree MJ, Borisov SE, Bruchfeld J, et al. Surveillance of adverse events in the treatment of drug-resistant tuberculosis: a global feasibility study. Int J Infect Dis. 2019;83:72–6.
McQuaid CF, Vassall A, Cohen T, Fiekert K, White RG. The impact of COVID-19 on TB: a review of the data. Int J Tuberc Lung Dis. 2021;25(6):436–46.
Organization WH. Programmatic innovations to address challenges in tuberculosis prevention and care during the COVID-19 pandemic. 2021.
Tavakoli A. Incidence and prevalence of tuberculosis in Iran and neighboring countries. Zahedan J Res Med Sci 2017, 19(7).
Migliori GB, Thong PM, Akkerman O, Alffenaar JW, Alvarez-Navascues F, Assao-Neino MM, Bernard PV, Biala JS, Blanc FX, Bogorodskaya EM, et al. Worldwide effects of Coronavirus Disease Pandemic on Tuberculosis services, January-April 2020. Emerg Infect Dis. 2020;26(11):2709–12.
Abdool Karim Q, Abdool Karim SS. COVID-19 affects HIV and Tuberculosis care. Science. 2020;369(6502):366–8.
Mandavilli A. The biggest monster’is spreading. And it’s not the coronavirus. New York Times 2020, 3.
Cilloni L, Fu H, Vesga JF, Dowdy D, Pretorius C, Ahmedov S, Nair SA, Mosneaga A, Masini E, Sahu S, et al. The potential impact of the COVID-19 pandemic on the tuberculosis epidemic a modelling analysis. EClinicalMedicine. 2020;28:100603.
Gomes C. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19). Brazilian J Implantology Health Sci 2020, 2(3).
Visca D, Tiberi S, Pontali E, Spanevello A, Migliori GB. Tuberculosis in the time of COVID-19: quality of life and digital innovation. Volume 56. Eur Respiratory Soc; 2020.
Ullah S, Daud H, Dass SC, Fanaee TH, Kausarian H, Khalil A. Space-time clustering characteristics of tuberculosis in Khyber Pakhtunkhwa Province, Pakistan, 2015–2019. Int J Environ Res Public Health. 2020;17(4):1413.
Moradi M, Arababadi MK, Hassanshahi G. Tuberculosis in the Afghan immigrant in Kerman province of Iran. 2008.
Tabrizi J, Rostami FF, Ahmadi S, Dolatabad SS. Socio-demographic factors affecting the prevalence of tuberculosis in Iran. 2014.
Azni SM, Mansourian AA, Nokandeh Z. Epidemiological study of tuberculosis in Damghan city (Iran) during 2003–2007. 2008.
Doosti A, Nasehi M, Moradi G, Roshani D, Sharafi S, Ghaderi E. The pattern of tuberculosis in Iran: A National Cross-sectional Study. Iran J Public Health. 2023;52(1):193–200.
Kiani B, Raouf Rahmati A, Bergquist R, Hashtarkhani S, Firouraghi N, Bagheri N, Moghaddas E, Mohammadi A. Spatio-temporal epidemiology of the tuberculosis incidence rate in Iran 2008 to 2018. BMC Public Health. 2021;21(1):1093.
MR Kadivar M, Ghaneh Shirazi R, Khavandegaran F, Karimi M. Epidemiology of tuberculosis among Afghan immigrants in Fars province, southern Islamic Republic of Iran. EMHJ-Eastern Mediterranean Health Journal, 13 (4), 758–764, 2007 2007.
Tabatabaee H, Hassan Zadeh J, Younes Nia F, Ali Akbarpoor M, Javanmard S, Honarvar B. Spatio-temporal pattern of tuberculosis in the regions supervised by Shiraz University of Medical Sciences 2006–2012. Iran J Public Health. 2015;44(9):1253–61.
Moosazadeh M, Khanjani N, Bahrampour A, Nasehi M. Does Tuberculosis have a seasonal pattern among migrant population entering Iran? Int J Health Policy Manag. 2014;2(4):181–5.
Fallahi MJ, Mirdamadi A, Moghadami M. Pulmonary tuberculosis seasonality survey in Fars Province, South of Iran. Shiraz E-Medical J. 2019;20(9):e86348.
Paynter S, Ware RS, Sly PD, Williams G, Weinstein P. Seasonal immune modulation in humans: observed patterns and potential environmental drivers. J Infect. 2015;70(1):1–10.
Koh GC, Hawthorne G, Turner AM, Kunst H, Dedicoat M. Tuberculosis incidence correlates with sunshine: an ecological 28-year time series study. PLoS ONE. 2013;8(3):e57752.
Dookie N, Padayatchi N, Naidoo K. Tuberculosis elimination in the era of Coronavirus Disease 2019 (COVID-19): a moving target. Clin Infect Dis. 2022;74(3):509–10.
Dheda K, Jaumdally S, Davids M, Chang J-W, Gina P, Pooran A, Makambwa E, Esmail A, Vardas E, Preiser W. Diagnosis of COVID-19: considerations, controversies and challenges in South Africa. Wits J Clin Med. 2020;2(Si1):3–10.
Acknowledgements
This study was the subject of the medical degree dissertation of Dr. Mohammad Nazemi.
Funding
No financial support was received for this report.
Author information
Authors and Affiliations
Contributions
M.J.F and R.S. designed the study. M.N. and A.Z. collected the data and drafted the manuscript. R.S. analyzed the data and drafted the manuscript. M.J.F revised the manuscript. All authors read and approving the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was approved by the Ethics Committee of Shiraz University of Medical Sciences and all experiments were performed in accordance with relevant guidelines and regulations. Based on the retrospective nature of the study, an informed consent waiver was approved by the Ethics committee of Shiraz University of Medical Sciences. Patients’ information was anonymized before analysis and confidentiality was assured by the researcher.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fallahi, M.J., Nazemi, M., Zeighami, A. et al. Changes in incidence and clinical features of tuberculosis with regard to the COVID-19 outbreak in Southern Iran. BMC Infect Dis 24, 1043 (2024). https://doi.org/10.1186/s12879-024-09947-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09947-0