Abstract
Background
Even though the disease has spread throughout the world, with millions killed, global COVID-19 vaccination coverage remains low, particularly in developing countries. However, epidemiological data is lacking in the area. Hence, this study aimed to assess COVID-19 uptake, willingness for vaccination, and associated factors.
Method
A hospital-based cross-sectional study was conducted from May 1 to June 30, 2022, among patients attending chronic follow-up clinics in the two comprehensive specialized hospitals in Bahir Dar. The total sample size was 423. Participants were selected by a systematic random sampling technique. Data was gathered using a pre-tested questionnaire and analyzed using SPSS version 23. A descriptive analysis was performed. A binary logistic regression analysis was done to assess the association between variables. Variables with a p-value < 0.05 in the multi-variable logistic regression with a 95% confidence interval were considered statistically significant.
Results
The analysis included 400 out of 423 participants, representing a 95% response rate. The COVID-19 vaccination uptake was 46.8%, while the acceptance was 60.5%. About 56% and 68% of the respondents had good knowledge and a favorable attitude, respectively. Elderly people were 2.7 times more likely to be vaccinated. Similarly, urban residents were 3.94 times more vaccinated. The probability of being vaccinated among respondents with good knowledge and favorable attitudes was 70% and 79%, respectively. The willingness for vaccination increased among those individuals with favorable attitudes (AOR: 1.82). Urban people were less likely to accept vaccination (AOR: 0.46). Some participants misunderstood that vaccination may aggravate their disease condition.
Conclusion
The overall COVID-19 vaccine uptake and acceptance for vaccination were low compared to what was estimated by the WHO. Age, residence, knowledge, and attitude were associated with COVID-19 vaccine uptake and acceptance of vaccination. Besides, there was a high level of rumor about the status of the vaccine and risk factors. Hence, special emphasis is warranted to deliver centrally trusted information. Moreover, further nationwide studies are warranted in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The pandemic coronavirus was named coronavirus disease 2019 (COVID-19) by the WHO and began at the beginning of December 2019 near Wuhan City, Hubei Province, China [1]. It is an acute respiratory disease syndrome caused by the coronavirus-2 (SARS-CoV-2) that can spread rapidly with the increased emergence of new strains [2]. Despite the implementation of preventive measures, the burden of the pandemic is not significantly reduced [3].
The COVID-19 pandemic, caused by SARS-CoV-2, has resulted in over 774,771,942 confirmed cases and 7,035,337 deaths globally [4]. Africa is also heavenly affected by the pandemic, where more than 9,576,309 confirmed cases and 175,500 deaths were reported. COVID-19 also significantly affected Ethiopia, with 501,157 confirmed cases and 7,574 deaths [4, 5].
Although COVID-19 can infect all individuals, not all people are equally affected by the virus, develop the disease, and die [6]. Chronic follow-up patients, especially when they are unvaccinated, were more likely to progress to severe conditions and death [7,8,9,10,11]. A study conducted in the USA reported that more than 99% of deaths and 94.4% of hospital admissions related to COVID-19 occurred among unvaccinated high-risk individuals [9, 12].
In Ethiopia, one recent study indicated that the COVID-19 pandemic causes 72% of poor medication adherence, commonly linked to the impacts on their follow-up visits, availability of medications, and increased prices [13]. According to a recent study conducted in 2024 in Bahir Dar city, a total of 72 (17.4%) participants reported at least one side effect following the COVID-19 vaccination. The prevalence was higher in participants with chronic follow-up patients who had a history of regular medication use [14].
Community-level vaccine coverage of 65 to 80+% (average 70%) is required to protect the community from COVID-19 infection, which also depends on its coverage and public willingness for vaccination [15]. However, global COVID-19 vaccine coverage is inequitable and lagging, especially in developing countries [16]. In Australia, 81.5% had received at least one dose of the COVID-19 vaccine [17]. Similarly, in India, among cancer patients, 80% of COVID-19 vaccinations were reported [18]. In contrast, as of June 2022, only two countries in the African Region (the Seychelles and Mauritius) have achieved the 70% target [19].
On December 31, 2023, approximately 860 million doses of the COVID-19 vaccine had been delivered to countries in the African Region, and 646 million doses had been administered. Cumulatively, 38% of the African Region’s population had received ≥ 1 dose, 32% had completed a primary series, and 21% had received ≥ 1 booster dose. The total population coverage with ≥ 1 dose ranged by country from 0.3 to 89% [20]. Meanwhile, in Malawi (22%) [21], among DM patients in Sudan (31%) [22] had received at least one dose of the COVID-19 vaccine. According to the data reported on July 6, 2022, the vaccination coverage in Ethiopia reached 38.4% [23].
Availability and accessibility of a safe vaccine do not necessarily guarantee to mitigate the pandemic unless vaccine recipients are willing to utilize the vaccine [24, 25]. This might be due to public attitude and perception [26, 27]. According to different studies, the willingness for COVID-19 vaccination was (80–90%) in China, Brazil, and South Africa, and (50–60%) in Russia, Poland, and France [28, 29]. A study conducted in China reported that acceptance was 79.08% [30]. Similarly, acceptance was reported at 36.2% among DM patients in Saudi Arabia [31], and 70.1% in Uganda [32].
Although the impact of COVID-19 among chronic follow up patients is significant, research on COVID-19 vaccine uptake and willingness among chronic follow-up patients in Bahir Dar is lacking. Few studies were conducted in Ethiopia. However, they were conducted either among health care workers within the first month of the first vaccine announcement in the country where the quality and safety issues were the greatest issues or in different areas of the country [33,34,35,36]. Moreover, we tried to include the vaccine uptake and associated factors. Acceptance of new and available vaccines varied based on differences in sociodemographic, economic, political, and personal factors [33, 37, 38]. Addressing these barriers is crucial to attain maximum vaccine coverage and eradicate this pandemic [39]. Therefore, this study aimed to assess COVID-19 vaccine uptake, willingness for vaccination, and associated factors among patients attending chronic follow-up in the comprehensive specialized hospitals of Bahir Dar, Ethiopia, from May 1 to June 30, 2022.
Methods and materials
Study, design and period
A health facility-based cross-sectional study design was conducted from May 1 to June 30, 2022, in the two comprehensive specialized hospitals (Felege Hiwot Comprehensive Specialized Hospital (FHCSH) and Tibebe-Ghion Comprehensive Specialized Hospital (TGCSH)) found in Bahir Dar, Ethiopia. Bahir Dar is the capital city of the Amhara National Regional State, located about 570 km northwest of Addis Ababa, Ethiopia. The FHCSH is the largest comprehensive specialized hospital in the Amhara National Regional State, whereas the TGCSH is a teaching hospital affiliated with Bahir Dar University College of Medicine and Health Sciences. Each hospital serves about 700 patients per month, referred from various health facilities in Bahir Dar city administration and adjacent zones, who attend chronic follow-up clinics (including those with CHF, hypertension, DM, and other conditions).
Source population and study population
The source population was patients with chronic diseases, including chronic liver disease, hypertension, diabetes mellitus, cardiovascular disease, chronic kidney disease, chronic obstructive pulmonary disease, asthma, and attending follow-up in the two comprehensive specialized hospitals. On the other hand, the study population consisted of patients who had chronic care appointments and follow-up during the data collection period, selected by the sampling technique and based on the inclusion criteria.
Inclusion and exclusion criteria
All patients with chronic diseases who were volunteers to participate were included in the study. Patients with chronic diseases under the age of 18 and those patients who were unable to respond due to severe illness were excluded from the study.
Operational definitions
Uptake: The percentage of people who received a COVID-19 vaccine, assessed by asking respondents if they had taken a vaccine (“Yes” or “No”) and reasons for not being vaccinated.
Willingness for Vaccination: The intention to receive available COVID-19 vaccines, assessed by asking respondents if they would take a vaccine if available (“Yes” or “No”). Reasons for refusal were assessed if the answer was “No.”
Chronic Disease Condition: Individuals with any medical illness, irrespective of the duration of follow-up.
Knowledge: Assessed using ten items about COVID-19 and its vaccine. Correct answers received one-point, incorrect answers received zero, and “I don’t know” responses were given negative one point. A score of 70% or above was considered good knowledge.
Attitude: Assessed using ten items. Agreement received one point, neutral zero points, and disagreement negative received one point. A score of 70% or higher was considered a positive attitude.
Sample size determination
A single population proportion formula was used to calculate the sample size (n = Z α/22*P (1-P)/d2). Assumptions: Confidence level: 95%, Critical value (Z): 1.96, Precision (d): 0.05, Proportion for uptake (P): 0.05, Proportion for willingness (P): 0.59 [35].
Calculations:
Vaccine uptake: n = (1.96) ² * 0.5 (1-0.5) / (0.05) ² = 384.
Willingness: n = (1.96) ² * 0.59(1-0.59) / (0.05) ² = 372.
Final sample size: Using the larger sample size (384) and adding a 10% non-response rate, the total sample size was 423.
Sampling technique
A systematic random sampling technique was used. The sampling frame included 1392 patients attending chronic follow-up, using the average monthly case flow of the previous year as a baseline. The sampling fraction (K) was calculated as 1392/423 = 3.29, rounded to 3. Patients were selected every 3rd interval from those actively involved participants during the data collection period. The first participant was chosen by lottery from the first three patients, and subsequent participants were selected systematically.
Data collection tool and procedure
The primary data source was obtained through a direct face-to-face interview. The data were collected using a pretested questionnaire adapted from the previous relevant literature [5, 8, 37, 42, 54]. The questionnaire consisted of different sections that covered socio-demographic characteristics, questions related to vaccine uptake and willingness for vaccination, knowledge, attitude, and chronic disease conditions. Reasons related to previous un-vaccination and COVID-19 vaccine refusal were also included in the questionnaire. The data was collected by two nurses in each hospital under the supervision of one MSc holder.
Data quality assurance
Training was given to data collectors and supervisors. Trained nurses who know the treatment centers were recruited. The questionnaire was translated to the local language, Amharic, and then back to the English version to assure its consistency during data recording and analysis. A pretest was also conducted on 5% of the sample size at Debre Tabor Comprehensive Specialized Hospital, and adjustments were made to the tool as necessary. The reliability of the questionnaire was also assessed. The principal investigator and supervisors were actively involved in supervising and monitoring the data collection. The completed questionnaire was checked daily for completeness and consistency. Selection bias might be expected during the data collection. To minimize this, we employed a prospective study design and provided training for data collectors recruited outside of the health facility of our interest.
Data processing and analysis
During the data collection, the questionnaire was checked for its completeness. Unrecorded values or responses were manually cleaned up. Data was entered into the epi-data software version 4.6 and exported to SPSS version 23 for analysis. Descriptive analysis was done first to find the frequencies and percentages. Binary logistic regression analysis was done using the crude odds ratio (COR), and multi-variable logistic regression with an adjusted odds ratio (AOR) at the 95% CI was performed to assess the association between dependent and independent variables. The p-values < 0.25 and < 0.05 were taken as cut-off values to test the level of statistical significance of the association for the bi-variable and multivariable logistic regression analyses, respectively.
Results
Socio-demographic characteristics
A total of 400 patients (95% response rate) participated in this study. The mean age was 53.5 years (SD = 17.3). Most participants were from FHCSH (52.5%), female (56.5%), and unable to read and write (51.3%). The majority were married (74.3%), Orthodox Christians (81.3%), and of Amhara ethnicity (99.2%). The most common occupation was farming (41.5%), and the most common diagnoses were hypertension (26.2%), followed by diabetes mellitus (18.2%) (Table 1).
Participants knowledge about COVID-19
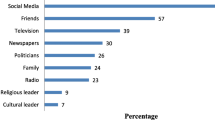
More than half (55.7%; 95% CI: 50.7–60.7%) had good knowledge of COVID-19 and its vaccine. The majority (84.5%) had information regarding the disease and its vaccine. Of those who had information, most (42.3%) considered television and radio as trusted sources of information. Most (67.5%) and 73.75% knew the transmission and the symptoms associated with COVID-19, respectively. The majority (75%) knew that going to crowded public places is a risk, while 66.25% knew that wearing a mask is necessary even after vaccination. Furthermore, 65.2% and 78% knew that chronic patients were among the priority groups for the vaccine and understood its availability for COVID-19, respectively (Table 2).
Participants attitudes toward COVID-19 and its vaccines
Most respondents (68%; 95% CI: 63.2–72.5%) had a favorable attitude towards COVID-19 and its vaccine. Specifically, 72.8% felt susceptible to COVID-19, 79% believed the vaccine was essential, and 76.5% agreed that it should be given to all. Additionally, 61.25% believed vaccines provide long-term immunity, 62.5% believed vaccines prevent complications, and the majority did not believe the vaccine contradicted their religion (73.7%) or culture (80.2%) (Table 3).
Coronavirus disease-19 vaccine uptake and associated factors
Nearly half, 46.8% (95%CI: 41.8–51.8%), had taken at least one dose of the COVID-19 vaccine. Specifically, 30% had been fully vaccinated, while 16.8% had been partially vaccinated or had been informed to have another dose. According to the multi-variable logistic regression analysis, the odds of COVID-19 vaccine uptake were 2.7 (95% CI: 1.17–6.2) among the older groups (age > 64 years) and 3.94 (95% CI: 1.64–9.5) for those living in the urban area. Besides, those with good knowledge and a favorable attitude toward COVID-19 and its vaccine had 2.3 (95% CI: 1.18–4.5) and 3.8 (95% CI: 1.8–7.9) increased odds for vaccine uptake (Table 4).
Respondents who had not taken the COVID-19 vaccine before (n = 213) were assessed for their concerns. Based on this, the majority (19.7%) worried that the vaccine might aggravate their current disease condition and treatment, which was followed by those who were against the COVID-19 vaccine, (13.6%) (Fig. 2).
Willingness for the COVID-19 vaccination and associated factors
Of the total (n = 280) participants assessed for willingness for COVID-19 vaccination, the majority (60.5%; 95%CI: 54.5–66.3%) were willing to accept the vaccine if available. According to the multi-variable binary logistic regression analysis, participants who had a favorable attitude were more likely to accept the vaccine, with an AOR of 1.82 (95% CI: 1.03–3.21). The probability of accepting the vaccine among the urban population was lower (31.5%) with an AOR of 0.46 (95%CI: 0.22–0.92) (Table 5).
Out of 110 respondents who were assessed for their reason for vaccine refusal, most (35.7%) were due to their threat that the vaccine may aggravate their current disease condition or affect their treatment, which was followed by those who needed to apply non-vaccine preventable mechanisms (15.2%) (Fig. 3).
Discussion
The present study found that 46.8% had taken at least one dose of the COVID-19 vaccine, 30% had been fully vaccinated, and 16.8% had been partially vaccinated. This implies that the vaccination was lower than what was expected by the WHO to achieve 70% vaccine coverage in the community [12, 15]. Hence, more than 50%, once exposed to COVID-19, might be vulnerable to increased COVID-19-associated morbidity, hospitalization, and mortality [9, 40].
Our finding was higher than a previous study conducted among cancer patients in India [18], a study done among NCD patients in Malawi by 2022 [21], and among DM patients in Sudan [22]. The discrepancy may be due to a difference in the period of data collection and the sociodemographic patterns of the study groups, as discussed below. For example, the study conducted in India only considered a specific group (only cancer patients aged ≥ 45 years), which might have affected the outcome. The data was also collected at the beginning of 2021, when the quality and safety of the vaccine were not assured and the awareness of the people was lower than reported elsewhere [41, 42].
Our finding also showed that the vaccine uptake in rural areas was lower (20.24%) than in the urban population (79.76%). This is in agreement with a study in Bangladesh [43]. This could be attributed to the vaccine’s inaccessibility in rural areas. It may also be due to rural people’s lack of awareness and religious or cultural beliefs about the virus and its vaccine. In support of this, a global survey conducted in 90 countries showed that Christianity was negatively related to the COVID-19 vaccination [44].
The odds of COVID-19 vaccine uptake were 2.7 among the older age groups (age > 64 years) as compared to the adult age groups (18–64 years). Participants living in the urban area were also more likely to be vaccinated than those living in the rural area, with an AOR of 3.94. Similarly, respondents with good knowledge and favorable attitudes towards COVID-19 and/or its vaccine were more likely to take it, with an AOR of 2.3 and 3.6, respectively. This implies that older people are more highly threatened by the disease than the adult groups, as the burden and severity have been considered high in the older age groups since the emergency of the pandemic [45, 46].
Due to increased accessibility and awareness in the first pandemic era, urban residents may have taken the COVID-19 vaccine more often. The same is true for the participant’s knowledge and attitude. Participants who did not take the COVID-19 vaccine were also assessed for their reasons or concerns for why they did not take the COVID-19 vaccine. The majority, 45 (19.7%) of the respondents, worried that the vaccine might aggravate their current disease condition or treatment, which was followed by those who were totally against the COVID-19 vaccine (13.6%). This indicated that, although the people had information, they either lacked awareness or were misinformed. Our finding is in agreement with a previous study showing the negative impact of misinformation and/or a rumor on the acceptance of the COVID-19 vaccine [47,48,49,50].
In the present study, 60.5% were willing to accept the vaccine if it was available. This implies that although people have information, either they do not understand or have been misinformed about the effectiveness of the vaccine or its safety [35]. Availability and accessibility of a safe COVID-19 vaccine do not necessarily guarantee to mitigate the COVID-19 pandemic unless vaccine recipients are willing to utilize the vaccine [24, 25]. The willingness to vaccinate can be affected by multiple beliefs and misconceptions among different population classes [35]. Our finding is in agreement with the previous study conducted in DCSH (59.4%) [35], and GCSH (63.8%) [51]. Our finding was also in agreement with the systematic review and meta-analysis studies conducted in Africa [52, 53] and around the world [54].
The willingness to accept the vaccine in our finding was higher than the study conducted among DM patients in Saudi Arabia, 36.2% [31], a study conducted among patients with NCD in rural areas of Malawi, 24% [21] and among patients with chronic disease in Guji Zone, Ethiopia, 39.5% [36]. The disagreement might be due to the difference in the period during which the studies were conducted. The perception regarding the quality and safety issues of the vaccine was misleading and in question during the first season of the pandemic, as reported in the previous studies [48, 49]. In contrast, our finding was lower than a study conducted among elderly and chronic patients in China, 79.08% [30]. The difference may be due to China’s high disease burden during the period when the pandemic first existed. It could also be due to China’s mandatory vaccinations. This finding was also lower than the study done in Uganda (70.1%) [32]. The source of this variation might be due to the study period where the burden of the pandemic was high in these areas, for example in China, initiating the people to accept the vaccine. It might also be due to the sociodemographic difference.
The probability of willingness for COVID-19 vaccination was higher among individuals with favorable attitudes. The implication is that the attitude or perception of the population matters more than the knowledge to accept new vaccines. This was in agreement with the previous study conducted in DCSH and Guji Zone, Ethiopia [35, 36].
In the present study, vaccine acceptance was higher among participants living in rural areas. In agreement with our finding, a study in China showed that urban participants had a higher COVID-19 vaccine hesitancy (9.39%) than their rural counterparts (4.26%) [55]. A study in Bangladesh also showed that the majority (84.3%) of the rural population responded to accepting the COVID-19 vaccine [56]. The increase in refusals for the COVID-19 vaccine in the urban population might be by chance and need further investigation. However, it could also be due to misinformation (“rumor”) delivered in the urban population by different social media about the vaccine’s status as reported elsewhere [48, 50, 55, 57, 58]. In support of this, a global survey reported that people’s perceptions toward COVID-19 vaccine acceptance have fluctuated with the information flow on various social media [59].
Strength and limitation
This was the first study conducted to assess both COVID-19 vaccine uptake and willingness for vaccination among patients attending chronic follow-up who are one of the first WHO priority groups for COVID-19 vaccination. Besides, this study used probability sampling techniques, in which the results could be generalized to the population of chronic follow-up patients in the study settings. Despite this, during our data collection, HIV patients on ART follow-up and those cancer patients were attending a different clinic and were not included. This may underestimate the outcome and limit its generalizability. Causal relationships between the dependent and independent variables could not be established due to the use of a cross-sectional design. Furthermore, an interviewer bias might be expected. However, this had been managed through effective monitoring by the assigned supervisors in each of the hospitals. Hence, these limitations need to be considered when interpreting these findings.
Conclusions
The overall COVID-19 vaccine uptake and willingness for vaccination were low compared with what was estimated by the WHO. Respondents’ age, residence, knowledge, and attitude towards the COVID-19 vaccine were all significantly associated with COVID-19 vaccine uptake. On the other hand, residence, and attitude towards COVID-19 and its vaccine were associated with willingness for vaccination. There was also a high level of misinformation or a rumor about the status of the vaccine and misunderstandings about the effect of the new vaccine on their underlining conditions. This could be an obstacle to the progress made in vaccine distribution and pandemic control.
Hence, special emphasis is warranted for individuals with chronic diseases through health education or information campaigns from trusted sources (health care workers, policymakers, and the media) on the safety of the current vaccine and its interaction with their underlining conditions. This is important to tackle the rumor, reduce its burden, and avoid the long-term impact of the pandemic on these high-risk groups. Moreover, future nationwide longitudinal and surveillance studies are warranted to monitor the public attitude, acceptance, and uptake of COVID-19 vaccination with the progress of vaccine improvement and the national vaccination program in terms of access, distribution, and coverage.
Data availability
The datasets supporting the conclusions of this article are included within the article. Materials relevant to this study can be obtained from the corresponding author (DT) for further inquiry.
Abbreviations
- AOR:
-
Adjusted odd ratio
- ART:
-
Anti-Retroviral Therapy
- COR:
-
Crude odd ratio
- CHF:
-
Chronic heart failure
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- COVID-19:
-
Coronavirus Disease 2019
- DM:
-
Diabetes mellitus
- FHCSH:
-
Felege Hiwot Comprehensive Specialized Hospital
- GCSH:
-
Gondar Comprehensive Specialized Hospital
- HCW:
-
Health care worker
- ICU:
-
Intensive Care Unit
- MOH:
-
Ministry of Health
- NCD:
-
Non-communicable disease
- SPSS:
-
Statistical Packages for socials Sciences
- SARS:
-
COV-2 Severe Acute Respiratory Syndrome COV2
- TGCSH:
-
Tibebe-Ghion Comprehensive Specialized Hospital
- USA:
-
United States of America
- WHO:
-
World Health Organization
References
Bartsch SM, O’Shea KJ, Ferguson MC, Bottazzi ME, Wedlock PT, Strych U, et al. Vaccine efficacy needed for a COVID-19 coronavirus vaccine to prevent or stop an epidemic as the sole intervention. Am J Prev Med. 2020;59(4):493–503.
Gebru AA, Birhanu T, Wendimu E, Ayalew AF, Mulat S, Abasimel HZ, et al. Global burden of COVID-19: situational analyis and review. Hum Antib. 2021;29(2):139–48.
Tran VD, Pak TV, Gribkova EI, Galkina GA, Loskutova EE, Dorofeeva VV et al. Determinants of COVID-19 vaccine acceptance in a high infection-rate country: a cross-sectional study in Russia. Pharm Pract (Granada). 2021;19(1).
WHO M. WHO coronavirus (COVID-19) dashboard. World Health Organization; 2021.
Gashaw DG, Alemu ZA, Constanzo F, Belay FT, Tadesse YW, Muñoz C, et al. COVID-19 patient satisfaction and associated factors in telemedicine and hybrid system. Front Public Health. 2024;12:1384078.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–9.
Xia Y, Li Q, Li W, Shen H. Elevated mortality of chronic diseases during COVID-19 pandemic: a cause for concern? Therapeutic Adv Chronic Disease. 2020;11:2040622320961590.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. 2020.
Control CfD. Prevention. Trends in Number of COVID-19 cases and deaths in the US reported to CDC, by State/Territory. Accessed March. 2021;16.
Chen Y, Gong X, Wang L, Guo J. Effects of hypertension, diabetes and coronary heart disease on COVID-19 diseases severity: a systematic review and meta-analysis. MedRxiv. 2020.
Peng P, Y, Meng, K, Guan, H, Leng, L, Zhu, R, Wang, B, et al. Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV. Zhonghua Xin xue guan bing za zhi. 2020;48(6):450–5.
Organization WH. WHO SAGE roadmap for prioritizing uses of COVID-19 vaccines: an approach to optimize the global impact of COVID-19 vaccines. Based on public health goals, global and national equity, and vaccine access and coverage scenarios, first issued 20 October 2020, updated: 13 November 2020, updated: 16 July 2021, latest update: 21 January 2022. World Health Organization; 2022.
Shimels T, Asrat Kassu R, Bogale G, Bekele M, Getnet M, Getachew A, et al. Magnitude and associated factors of poor medication adherence among diabetic and hypertensive patients visiting public health facilities in Ethiopia during the COVID-19 pandemic. PLoS ONE. 2021;16(4):e0249222.
Siraj EA, Yayehrad AT, Yilma Z, Getahun T, Melaku MS, Bizuneh GK, et al. Post COVID-19 vaccination side effects and associated factors among vaccinated clients in Bahir Dar City, Ethiopia. SAGE Open Nurs. 2023;9:23779608231172358.
Doshi P. Covid-19: Do many people have pre-existing immunity? Bmj. 2020;370.
Lucero-Prisno DE III, Ogunkola IO, Imo UF, Adebisi YA. Who will pay for the COVID-19 vaccines for Africa? Am J Trop Med Hyg. 2021;104(3):794.
Day D, Grech L, Nguyen M, Bain N, Kwok A, Harris S, et al. Serious Underlying Medical conditions and COVID-19 vaccine hesitancy: a large cross-sectional analysis from Australia. Vaccines. 2022;10(6):851.
Noronha V, Abraham G, Bondili SK, Rajpurohit A, Menon RP, Gattani S, et al. COVID-19 vaccine uptake and vaccine hesitancy in Indian patients with cancer: a questionnaire-based survey. Cancer Res Stat Treat. 2021;4(2):211.
Organization WH. Monthly Bulletin-COVID-19 vaccination in the African Region: Issue No. 04. 2022.
Doshi RH. COVID-19 Vaccination Coverage—World Health Organization African Region, 2021–2023. MMWR Morbidity and Mortality Weekly Report. 2024;73.
Aron MB, Connolly E, Vrkljan K, Zaniku HR, Nyirongo R, Mailosi B, et al. Attitudes toward COVID-19 vaccines among patients with Complex Non-communicable Disease and their caregivers in Rural Malawi. Vaccines. 2022;10(5):792.
Omar SM, Khalil R, Adam I, Al-Wutayd O. The concern of COVID-19 Vaccine Safety is behind its low uptake among patients with diabetes Mellitus in Sudan. Vaccines. 2022;10(4):527.
WHO. COVID-19 weekly epidemiological update, edition 99, 6 July 2022. 2022.
Hajure M, Tariku M, Bekele F, Abdu Z, Dule A, Mohammedhussein M, et al. Attitude towards COVID-19 vaccination among Healthcare workers: a systematic review. Infect Drug Resist. 2021;14:3883.
Harrison EA, Wu JW. Vaccine confidence in the time of COVID-19. Eur J Epidemiol. 2020;35(4):325–30.
Lin C, Tu P, Beitsch LM. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines. 2021;9(1):16.
Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, et al. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines. 2020;8(3):482.
Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–8.
Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, van Exel J, et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Springer; 2020.
Wang J, Yuan B, Lu X, Liu X, Li L, Geng S, et al. Willingness to accept COVID-19 vaccine among the elderly and the chronic disease population in China. Hum Vaccines Immunotherapeutics. 2021;17(12):4873–88.
Aldossari KK, Alharbi MB, Alkahtani SM, Alrowaily TZ, Alshaikhi AM, Twair AA. COVID-19 vaccine hesitancy among patients with diabetes in Saudi Arabia. Diabetes Metabolic Syndrome: Clin Res Reviews. 2021;15(5):102271.
Bongomin F, Olum R, Andia-Biraro I, Nakwagala FN, Hassan KH, Nassozi DR, et al. COVID-19 vaccine acceptance among high-risk populations in Uganda. Therapeutic Adv Infect Disease. 2021;8:20499361211024376.
Aemro A, Amare NS, Shetie B, Chekol B, Wassie M. Determinants of COVID-19 vaccine hesitancy among Health Care workers in Amhara region referral hospitals, Northwest Ethiopia: a cross-sectional study. Epidemiol Infect. 2021:1–23.
Zewude B, Belachew A. Intention to receive the Second Round of COVID-19 Vaccine among Healthcare workers in Eastern Ethiopia. Infect Drug Resist. 2021;14:3071.
Berihun G, Walle Z, Berhanu L, Teshome D. Acceptance of COVID-19 Vaccine and Determinant Factors Among Patients with Chronic Disease Visiting Dessie Comprehensive Specialized Hospital, Northeastern Ethiopia. Patient preference & adherence. 2021:1795 – 805.
Daba C, Asefa L, Lemma H, Atamo A, Kebede E, Gebrehiwot M. Why does COVID-19 Vaccine Acceptance rate remain low among patients with chronic diseases? Evidences from Public hospitals of Ethiopia. Patient Prefer Adherence. 2022;16:1371.
Zhang F, Karamagi H, Nsenga N, Nanyunja M, Karinja M, Amanfo S et al. Predictors of COVID-19 Epidemics in Countries of the World Health Organisation African Region. 2021.
Tran VD, Pak TV, Gribkova EI, Galkina GA, Loskutova EE. Determinants of COVID-19 vaccine acceptance in a high infection-rate country: a cross-sectional study in Russia.
Joshi A, Kaur M, Kaur R, Grover A, Nash D, El-Mohandes A. Predictors of COVID-19 vaccine acceptance, intention, and hesitancy: a scoping review. Front Public Health. 2021;9.
Havers FP, Pham H, Taylor CA, Whitaker M, Patel K, Anglin O et al. COVID-19-associated hospitalizations among vaccinated and unvaccinated adults ≥ 18 years–COVID-NET, 13 states, January 1–July 24, 2021. MedRxiv. 2021.
Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021;194:245–51.
Wang C, Han B, Zhao T, Liu H, Liu B, Chen L, et al. Vaccination willingness, vaccine hesitancy, and estimated coverage at the first round of COVID-19 vaccination in China: a national cross-sectional study. Vaccine. 2021;39(21):2833–42.
Mistry SK, Ali AM, Yadav UN, Huda MN, Parray AA, Mahumud RA, et al. COVID-19 vaccination coverage is extremely low among older population in Bangladesh: findings from a cross-sectional study. Hum Vaccines Immunotherapeutics. 2022;18(1):2030624.
Trepanowski R, Drążkowski D. Cross-national comparison of religion as a predictor of COVID-19 vaccination rates. J Relig Health. 2022;61(3):2198–211.
Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, Imai N et al. Estimates of the severity of COVID-19 disease. MedRxiv. 2020:2020.03. 09.20033357.
Tisminetzky M, Delude C, Hebert T, Carr C, Goldberg RJ, Gurwitz JH. Age, multiple chronic conditions, and COVID-19: a literature review. Journals Gerontology: Ser A. 2022;77(4):872–8.
Loomba S, De Figueiredo A, Piatek SJ, De Graaf K, Larson HJ. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat Hum Behav. 2021;5(3):337–48.
Islam MS, Kamal A-HM, Kabir A, Southern DL, Khan SH, Hasan SM, et al. COVID-19 vaccine rumors and conspiracy theories: the need for cognitive inoculation against misinformation to improve vaccine adherence. PLoS ONE. 2021;16(5):e0251605.
Sharevski F, Huff A, Jachim P, Pieroni E. (Mis) perceptions and engagement on Twitter: COVID-19 vaccine rumors on efficacy and mass immunization effort. Int J Inform Manage Data Insights. 2022;2(1):100059.
Lee SK, Sun J, Jang S, Connelly S. Misinformation of COVID-19 vaccines and vaccine hesitancy. Sci Rep. 2022;12(1):13681.
Mekonnen CK, Demissie NG, Beko ZW, Ferede YM, Abate HK. Intent to get vaccinated against COVID-19 pandemic and its associated factors among adults with a chronic medical condition. Int J Afr Nurs Sci. 2022;16:100401.
Azanaw J, Endalew M, Zenbaba D, Abera E, Chattu VK. COVID-19 vaccine acceptance and associated factors in 13 African countries: a systematic review and meta-analysis. Front Public Health. 2023;10:1001423.
Wake AD. The acceptance rate toward COVID-19 vaccine in Africa: a systematic review and meta-analysis. Global Pediatr Health. 2021;8:2333794X211048738.
Kazeminia M, Afshar ZM, Rajati M, Saeedi A, Rajati F. Evaluation of the acceptance rate of COVID-19 vaccine and its associated factors: a systematic review and meta-analysis. J Prev. 2022;43(4):421–67.
Wu J, Shen Z, Li Q, Tarimo CS, Wang M, Gu J, et al. How urban versus rural residency relates to COVID-19 vaccine hesitancy: a large-scale national Chinese study. Soc Sci Med. 2023;320:115695.
Roy DN, Huda MN, Azam MS. Factors influencing COVID-19 vaccine acceptance and hesitancy among rural community in Bangladesh: a cross-sectional survey based study. Hum Vaccines Immunotherapeutics. 2022;18(5):2064685.
Joshi A, Surapaneni KM, Kaur M, Bhatt A, Nash D, El-Mohandes A. A cross sectional study to examine factors influencing COVID-19 vaccine acceptance, hesitancy and refusal in urban and rural settings in Tamil Nadu, India. PLoS ONE. 2022;17(6):e0269299.
Olanipekun T, Abe T, Effoe V, Westney G, Snyder R. Changes in COVID-19 vaccine acceptance rate among recovered critically ill patients: a 12-month follow-up study. Vaccine. 2021;39(48):7074–81.
Marzo RR, Shrestha R, Sapkota B, Acharya S, Shrestha N, Pokharel M, et al. Perception towards vaccine effectiveness in controlling COVID-19 spread in rural and urban communities: a global survey. Front Public Health. 2022;10:958668.
Acknowledgements
AcknowledgmentThe authors would like to gratitude Bahir Dar University, College of Medicine and Health Sciences, Department of Adult Health Nursing for letting me conduct this research. We also advance our profound thanks to Felegehiwot Comprehensive Specialized Hospital and Tibebe Ghion Comprehensive Specialized Hospital managers for allowing us to conduct and facilitate the data collection, especially those staff working in the chronic follow-up clinic. The data collectors and the study participants were also acknowledged.
Funding
The authors declare that no external funds or grants were received for this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: MK, DT, HB, GDData curation: Mulu Kebede.Formal data analysis: MK and DT Methodology: MK, DT, HB, GD, AA, MEResources: MK, DT, HB, GDInvistigation: MK, DT, HB, GDSoftware: MK, DT, AA, ME Supervision: HB, GD Visualization and validation: = DT, HB, GD, AA, MEWriting the original draft: MKRevised the manuscript and approval for publication: All the authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institutional review board of Bahir Dar University, College of Medicine and Health Sciences and received a protocol number of 423/2022. The data collection was performed according to the guidelines and regulations of the Declaration of Helsinki. A permission letter was obtained from the ethical review board and provided to each of the selected comprehensive specialized hospitals. During the data collection period, the aim of the study was explained. Written informed consent was obtained from the study participants. Moreover, for illiterate participants, the consent paper was read to them, and thumb signs were obtained. There was no invasive procedure or experiment performed to conduct this study, and there was no significant risk to the study participants. That is, the data was collected by using a questionnaire. Participants were encouraged to feel free and guaranteed that their responses would be kept private. The participants who were willing to sign the informed consent were interviewed. The confidentiality of the information was assured by the coding system, which was used only for study purposes.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tegegne, D., Kebede, M., Biresaw, H. et al. Coronavirus disease-19 vaccine uptake, willingness for vaccination, and associated Factors among chronic follow patients attending in the two comprehensive specialized hospitals of Bahir Dar, Ethiopia. BMC Infect Dis 24, 976 (2024). https://doi.org/10.1186/s12879-024-09882-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09882-0