Abstract
Background
After a 920-day hiatus, COVID-19 resurged in the Tibet Autonomous Region of China in August 2022. This study compares the characteristics of COVID-19 between high-altitude residents and newcomers, as well as between newcomers and lowlanders.
Methods
This multi-center cohort study conducted at the Third People’s Hospital of Tibet Autonomous Region and Beijing University Shenzhen Hospital, included 520 high-altitude resident patients, 53 high-altitude newcomer patients, and 265 lowlander patients infected with the Omicron variant. Initially, we documented epidemiological, clinical, and treatment data across varying residency at admission. We compared the severity of COVID-19 and various laboratory indicators, including hemoglobin concentration and SpO2%, over a 14-day period from the date of the first positive nucleic acid test, as well as the differences in treatment methods and disease outcomes between highlanders and high-altitude newcomers. We also compared several characteristics of COVID-19 between high-altitude newcomers and lowlanders. Univariate analysis, multivariable logistic regression, and the generalized linear mixed model were utilized for the analysis.
Results
No fatalities were observed. The study found no significant differences in COVID-19 severity or in the physiological measures of hemoglobin concentration and SpO2% between high-altitude and lowland residents. Similarly, there were no statistically significant differences in the values or trends of hemoglobin and SpO2% between high-altitude residents and newcomers throughout the 14-day observation period. However, compared to age- and sex-matched lowlander patients (1:5 ratio), high-altitude newcomers exhibited higher heart rates, respiratory rates, and average hemoglobin concentrations, along with lower platelet counts. There were no significant differences in hospital stays between the two groups.
Conclusions
High-altitude residents and newcomer patients exhibit clinical similarities. However, the clinical characteristics of high-altitude newcomers and lowlander patients differ due to the impact of the high-altitude environment. These results highlight potential considerations for public health strategies in high-altitude regions such as Tibet.
Similar content being viewed by others
Introduction
The global impact of the COVID-19 pandemic over the past three years has been profound, yet its effects on plateau regions remain a topic of debate [1,2,3]. Previous research has shown contrasting results, suggesting that living in plateau environments could either decrease or increase the infection rate, severity, or mortality of respiratory diseases [3,4,5,6,7]. Studies investigating the adaptive and coping mechanisms of both high-altitude natives and newcomers are limited, with most of the existing research dating back several decades. Nevertheless, a study suggests natives living in high-altitude areas may exhibit lower susceptibility to common respiratory risks compared to newcomers [8]. Researchers have attributed this to lifelong adjustment to hypoxic conditions, which can increase lung volume, pulmonary diffusion capacity for oxygen, arterial oxygen saturation levels, and strengthen the antioxidant system [9, 10].Therefore, the prevalence of related diseases varies between high-altitude natives and newcomers, such as pulmonary hypertension-related high-altitude heart disease and other chronic mountain diseases [11].
On August 7, 2022, the Tibet Autonomous Region, China, experienced its first large-scale COVID-19 epidemic after a 920-day period free from the disease. The dominant strain of the virus was identified as the Omicron subvariant of COVID-19, BA.2.76, confirmed by the Chinese CDC. Approximately 45.6% of Tibet's territory lies above an altitude of 5,000 m, corresponding to an average barometric pressure of < 500 mmHg and an ambient partial pressure of oxygen (pO2) of 80 mmHg [12]. This low environmental pO2, known as hypobaric hypoxia, poses a notable physiological challenge, particularly for individuals infected with COVID-19, amplifying the severity of the condition.
Research indicates that cellular hypoxia leads to pathophysiological response to high-altitude environments. Typical responses to high altitude include hyperventilation, polycythemia, hypoxic pulmonary vasoconstriction, changes in oxygen affinity of hemoglobin, increases in oxidative enzymes, and increased concentration of capillaries in peripheral muscle [13]. Pulmonary diseases such as pulmonary hypertension and COPD are prevalent at high altitudes, significantly impair lung function [14, 15]. Therefore, Omicron-infected patients may face heightened risks of exacerbation. Moreover, the manifestation of severe COVID-19 infections might vary among distinct populations residing at higher altitudes. Variations in hypoxia tolerance between high-altitude residents and newcomers could potentially influence the severity of disease. Rashmi et.al [16] have found that genetic adaptations in individuals residing at high altitudes may enhance their ability to combat COVID-19 compared to newcomers. This assertion is supported by studies like Simbaña-Rivera et al. [17], which indicate better short-term survival rates among critically ill COVID-19 patients living at high altitudes. Furthermore, evidence from Stephens et al. [18] indicates a reduced infection and mortality rate within high-altitude populations.
In this cohort study, our objective was to delineate the clinical characteristics of COVID-19 among patients in the Tibet Autonomous Region, China, and to explore clinical variations between high-altitude residents and newcomers, as well as between high-altitude newcomers and the lowlanders.
Methods
Study design and participants
This multi-center cohort study enrolled 520 high-altitude resident patients and 53 high-altitude newcomer patients confirmed Omicron-infected patients admitted to the Third People’s Hospital of Tibet Autonomous Region, as well as 265 lowlander patients admitted to Beijing University Shenzhen Hospital. We collected the inpatient highlander and high-altitude newcomer cases data from electronic medical records (EMR) from Aug 7, 2022 to Sep 26, 2022. We collect the lowlander patient’s data from December 26, 2022, to February 15, 2023. Lowlander patients were matched to high-altitude newcomer cases at a 1:5 ratio based on age and gender. Only aged 18 years and above and non-pregnant were included. Those with incomplete records were excluded from the study. Patients were followed up until discharge. The Third People’s Hospital of Tibet Autonomous Region, designated as a COVID-19 treatment facility, is one of the tertiary hospitals in Lhasa, Tibet Autonomous Region, China, catering to the majority of severe cases in the region. Beijing University Shenzhen Hospital is also a tertiary hospital located in Shenzhen, Guangdong Province, China.
This study received ethics approval from the institutional ethics board of the Third People’s Hospital of Tibet Autonomous Region (Approval No. 2022003). Informed consent was obtained from all the participants. We reported the study in compliance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline [19]. (Supplemental file). All procedures of the study were carried out in accordance with relevant guidelines and regulations.
Definition of high-altitude residents, newcomers and lowlanders
High-altitude residents are defined as individuals whose families have resided at high altitudes for two or more generations, while newcomers are those whose families have lived at high altitudes for fewer than two generations. Lowlanders are individuals who resided in plain areas.
Data collection
Epidemiological, clinical, and treatment information were obtained with data collection forms from EMR. A team of trained physicians and statisticians reviewed the data. Demographics, comorbidities, laboratory examinations, chest computed tomographic (CT) scans, treatment and medication were documented upon admission. Laboratory test results obtained during the hospital stay were also recorded. Additionally, information regarding patient outcomes such as date of death (if applicable), length of hospitalization, and duration from the initial positive SARS-CoV-2 nucleic acid tests (NAT) to two consecutive negative NAT results was documented.
The severity of COVID-19 was categorized according to the Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia issued by the Chinese National Health Commission trial version 9 (https://www.gov.cn/zhengce/zhengceku/2022-03/15/5679257/files/49854a49c7004f4ea9e622f3f2c568d8.pdf). Four types of severity were defined: mild, moderate, severe, and critical. Demographic data, including high-altitude residential status, were self-reported by the patients. It is important to note that all COVID-19 vaccines referenced in this study were inactivated vaccines. Patients were classified based on severity and high-altitude residential status.
Laboratory examinations included serology, NAT, and routine blood examinations. Serology testing included COVID-19-specific IgG and IgM antibodies detection. Methods for NAT were described elsewhere [20]. Briefly, nasal or throat swab specimens were analyzed using the COVID-19 (ORF lab/N gene) nucleic acid detection kit (Hangzhou Dean Biological). Samples were considered positive if they exhibited a cycle threshold (Ct) < 35. Additionally, routine blood test, serum biochemical test, inflammation biomarker assessments, and coagulation examination were also conducted. Chest Computed Tomography (CT) scans were performed for all participants.
The CT diagnoses were conducted by experienced radiologists, characterized by the following features: COVID-19 infection cases typically displayed multifocal and diverse chest imaging manifestations, with a higher prevalence observed in the outer lung field and subpleural area. Lesions exhibited dynamic changes, presenting as nodular, patchy, or ground-glass opacities. After timely antiviral treatment, the lesions could have obvious absorption and fibrosis changes in a short timeframe. Pleural effusion and mediastinal and hilar enlarged lymph nodes were rare, while thickening of blood vessels within the lesions was more commonly observed.
Statistical analysis
The epidemiological, clinical, and treatment information of patients at admission were described. Univariate analyses were conducted for the comparison between the highlanders and the high-altitude newcomers, as well as the high-altitude newcomers and the lowlanders. Categorical variables are presented as frequencies and percentages, and the group comparisons were performed using Fisher’s exact test. Continuous variables with a normal distribution are reported as mean and standard deviation, and the means were compared using t test. Non-normally distributed continuous variables are presented as median and interquartile range (IQR) values, with the comparisons made using the Wilcoxon rank sum test.
Then, we tested the hypothesis that high-altitude residential status (whether individuals were high-altitude residents or newcomers) is independently associated with COVID-19 severity. Severity groups were categorized based on patient conditions: the severe group included those identified as severe and critical, while the non-severe group comprised patients with mild and moderate symptoms. We conducted a multivariable logistic regression analysis, adjusting for potential confounders such as age, sex, ethnicity, vaccination status, and variables demonstrating statistical differences between COVID-19 severity groups in univariate analysis.
Next, we investigated whether high-altitude residential status was associated with resting SpO2% using a multivariable linear regression model. Demographic variables and underlying comorbidities, which showed statistical differences in the univariate analysis, were included as covariates in the model. We visually assessed the normality assumption, and if it was not met, we conducted a data transformation accordingly.
Lastly, we compared hemoglobin concentration and SpO2% between high-altitude residents and newcomers over 14 days from the first date NAT positive. The overall difference and the trends were compared utilizing a generalized linear mixed model. The repeated measurements of hemoglobin concentration and SpO2% were treated as the outcome, with days since admission, high-altitude residential status, and their interaction terms included in the model. The overall trend of hemoglobin concentration and SpO2%, the overall difference between the residential status groups and the trend difference between the residential status groups were examined, correspondingly.
In this study, missing data was not imputed. All P values were two tailed, and a P value < 0.05 was considered statistically significant. All statistical analyses were performed using R software, version 4.1.3.
Results
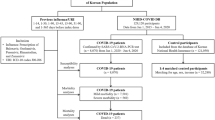
The inclusion and exclusion processes are illustrated in Fig. 1. In summary, the study cohort comprised 520 high-altitude residents, 53 high-altitude newcomers, and 265 lowland COVID-19 inpatients. (Figure S1). The median age and interquartile range (IQR) were 55.00 [40.00, 70.00] for high-altitude residents (51.92% male), 39.00 [33.00, 54.00] for high-altitude newcomers (49.06% male), and 41.00 [33.00, 54.00] for lowlanders (36.6% male). No death occurred during the study.
Table 1, Table S1 and Table S2 presents the baseline characteristics of the high-altitude residents and the newcomer patients. Comparing the high-altitude residents and the newcomers, univariable analysis demonstrated that high-altitude residents were older (median [IQR]: 55.00 [40.00, 70.00] vs. 39.00 [33.00, 54.00], P < 0.001), had lower heart rate (88.00 [80.00, 98.00] vs. 90.00 [84.75, 105.50], P = 0.019), lower monocyte count (0.35 [0.26, 0.47] vs. 0.42 [0.31, 0.58], P = 0.013), higher total carbon dioxide (17.40 [15.70, 19.20] vs.17.10 [15.20, 18.20], P = 0.043), higher D-dimer (0.48 [0.23, 1.10] vs. 0.27 [0.11, 0.67], P = 0.012), and a higher prevalence of hypertension (143 (27.88) vs. 5 (9.62), P = 0.007). (Tables 1 and 2). Although Table 2 shows that high-altitude residents were less likely to require oxygen therapy compared to newcomers, age-stratified analysis revealed no significant differences in the proportions of high-altitude residents and newcomers requiring oxygen therapy across different age groups (Table S3). Similarly, we conducted an age-stratified comparison of the hospital stays and days from the first positive NAT to two consecutive negative tests between high-altitude residents and newcomers, and found no significant differences between the two groups within each age category (Table S4 and S5).
Table 3 illustrates that, after adjusting for age, sex, ethnicity, smoking status, COVID-19 vaccination history, and comorbidities such as cardiovascular disease and chronic lung disease, we did not find sufficient evidence of an independent association between high-altitude residents and the newcomers with COVID-19 severity in the multivariable analysis.
Table S6 illustrates that, after adjusting for age, sex, ethnicity, smoking status, COVID-19 vaccination history, and comorbidities such as hypertension, diabetes, cardiovascular disease, chronic lung disease, chronic liver disease, chronic kidney disease, malignant tumors, immune deficiency, and hemodialysis, we did not find sufficient evidence of an independent association between high-altitude residential status and resting SpO2% among COVID-19 patients in the multivariable analysis.
Additionally, the hemoglobin concentration and SpO2% differences between high altitude residents and newcomers over 14-day period from the NAT positive date were explored. However, no statistically significant differences were observed in either the values or the trends over time. (Fig. 2).
Dynamic profile of hemoglobin concentration and SpO2% in COVID-19 patients. The bars represented in the figures indicated the standard error of the mean. A Difference on hemoglobin concentration trend between 493 high-altitude residents and 44 newcomers; B Difference on SpO2% trend between 497 high-altitude residents and 44 newcomers, over 14 days from the first date SARS-CoV-2 nucleic acid tests positive
Finally, we compared high-altitude newcomers and lowlanders. The lowlander data were matched to the high-altitude newcomer data based on age and gender, resulting in no significant differences in these demographics between the two groups. Lowlanders had a higher prevalence of hypertension and diabetes upon admission. High-altitude newcomers exhibited higher heart rates, respiratory rates, and average hemoglobin concentrations, as well as lower platelet counts. Additionally, high-altitude newcomers had a higher incidence of fever. (Table 4) In terms of treatment, a higher proportion of high-altitude newcomers received small molecule drugs (Paxlovid), monoclonal antibodies, thymosin, low molecular weight heparin, and prone position ventilation. (Table 5) There were no significant differences in hospital stays between high-altitude newcomers and lowlanders. (Table 4).
Discussion
This study is a large-scale cohort study focusing on hospitalized COVID-19 patients in the Tibet Autonomous Region, China. During the time the data was collected, no death occurred among the study population, which may be attributed to nationwide vaccination, early identification of severe cases, timely referral, and effective treatment. In this study, we did not observe any statistically significant differences between high-altitude residents and newcomers in hemoglobin concentration, SpO2%, or COVID-19 severity, nor in their trends over 14 days from the NAT date.
The lack of significant differences between high-altitude residents and newcomers in our study may be explained by the following factors: First, the definition of "newcomer" includes individuals who have lived at high altitudes for up to two generations, which might have been long enough for them to develop some level of acclimatization. The duration of stay for newcomers at high altitudes might have been sufficient for them to acclimatize. Both groups may share similar physiological adaptations to hypoxia, reducing potential variances in COVID-19 severity. These adaptations include increased red blood cell production and alterations in blood oxygen affinity, which could normalize hemoglobin and SpO2% levels across the two groups [21]. Future research should further investigate this issue by considering different definitions of "newcomer" based on varying lengths of time spent at high altitudes. In addition, although the high-altitude residents are predominantly Tibetan and the newcomers are mostly Han Chinese, the two groups are genetically close to each other. This similarity in genetic predispositions related to COVID-19 responses among both populations could thereby dilute any potential effects of altitude on the disease's severity. Whether the hypoxic adaptation genes, such as EPAS1 genes etc [22]., affects the COVID-19 severity, remains to be studied. Notably, despite similar disease severity, high-altitude residents exhibited significantly higher D-dimer levels, suggesting complex interactions between coagulation alterations and COVID-19 response, necessitating further investigation.
Our study also found that lowlanders had a higher prevalence of hypertension and diabetes upon admission, which may be due to the fact that all lowlanders were intensive care unit patients. High-altitude newcomers exhibited higher heart rates, respiratory rates, and average hemoglobin concentrations, as well as lower platelet counts, likely due to the hypoxic environment of high altitudes. The higher incidence of fever among high-altitude newcomers may be attributed to the different manifestations of the disease in various regions or the use of antipyretics. High-altitude newcomers received a higher proportion of treatments with small molecule drugs (Paxlovid), monoclonal antibodies, thymosin, low molecular weight heparin, and prone position ventilation compared to lowlanders, possibly due to the hypoxic environment requiring more aggressive treatment to achieve similar outcomes.
The current study has several limitations, which may also account for the negative findings observed. First, the sample size of the high-altitude newcomers was relatively small compared to high-altitude residents. Nonetheless, we computed the sample size and statistical power using the “pwr” function in R 4.0.3. With a significance level of 0.05 for a two-sided test, and sample sizes of 520 highlanders and 53 newcomers, the power is 0.93 when the effect size is moderate (0.5), as recommended by Cohen [23]. Additionally, for a power of 0.8, with 520 highlanders, only 34 newcomers are needed. Our study includes 53 newcomers, which meets the minimum sample size requirement. Second, given the observational nature of the study, it is unlikely to completely avoid residual confounding, potentially introducing bias when estimating associations. Third, demographic, clinical, treatment, and laboratory data were extracted from electronic medical records, resulting in missing data. To maintain the integrity of the samples, missing data were not imputed. Fourth, some measured parameters, such as heart rate, CO2, and Monocyte count, are subject to measurement error, as each sample was measured only once at each time point, which may lead to bias. Fifth, certain metrics such as arterial blood gas, lactate, chest ultrasound, and mechanical ventilation parameters were not collected during the study. In the current study, SpO2% was used to replace blood gas metrics even though previous study indicated SpO2% should be interpreted with caution in high-altitude settings, as hypocapnia significantly shifts the oxygen-hemoglobin dissociation curve and improves blood oxygen saturation [19]. This study also showed that SpO2%, as one determinant of need for intensive care resources, is notably lower in severe patients. Also, finger pulse oximetry was shown to be a valuable tool at high altitude [15]. Thus, SpO2% was used to make up for the lack of blood gas metrics. Lastly, when comparing high-altitude newcomers with lowlanders, the data for lowlanders in lowland hospitals were collected three months after the high-altitude data collection, and the data from the high-altitude and lowland areas were collected from two different provinces. This introduces uncertainty regarding potential strain variations or distinct latitudes and climates, making it difficult to rule out factors other than altitude that could introduce different COVID-19 characteristics. Additionally, we have tried our best, but we were unable to obtain all the clinical indicators in the lowlander data that were available in the high-altitude data. Therefore, we only compared the indicators that we could obtain.
Despite the aforementioned limitations, this study has several strengths. Firstly, to the best of our knowledge, this is the first large-scale high-altitude COVID-19 cohort study that compares differences between high-altitude residents and newcomers, as well as between high-altitude newcomers and lowlanders, a research question that has been rarely explored in prior studies. Secondly, it is noteworthy that during the COVID-19 pandemic, the ability of doctors to manage a large influx of patients and provide timely and effective treatment while simultaneously collecting such comprehensive data is commendable. Thirdly, the study uses rigorous statistical methods. The comparison between high-altitude residents and newcomers involves not only univariable analysis but also multivariable linear regression that accounts for confounding factors. In analyzing differences in the temporal trends of hemoglobin concentration and SpO2% between high-altitude residents and newcomers, the study employs generalized linear mixed models. The rigorous statistical approach enhances the credibility of the results.
This study contributes to a deeper understanding of COVID-19 in high-altitude regions and lays a foundation for future research on the adaptation to hypoxia among individuals residing at different altitudes.
Availability of data and materials
The data underlying this article will be shared at reasonable request to the corresponding author.
References
Hummel C, Knaul FM, Touchton M, Guachalla VXV, Nelson-Nunez J, Boulding C. Poverty, precarious work, and the COVID-19 pandemic: lessons from Bolivia. Lancet Glob Health. 2021;9:e579–81.
Ashktorab H, Pizuomo A, González NAF, Villagrana EDC, Herrera-Solís ME, Cardenas G, et al. A comprehensive analysis of COVID-19 impact in Latin America. Res Sq [Preprint]. 2021:rs.3.rs–141245. https://doi.org/10.21203/rs.3.rs-141245/v1.
Seclen SN, Nunez-Robles E, Yovera-Aldana M, Arias-Chumpitaz A. Incidence of COVID-19 infection and prevalence of diabetes, obesity and hypertension according to altitude in Peruvian population. Diabetes Res Clin Pract. 2020;169: 108463.
Arias-Reyes C, Zubieta-DeUrioste N, Poma-Machicao L, Aliaga-Raduan F, Carvajal-Rodriguez F, Dutschmann M, Schneider-Gasser EM, Zubieta-Calleja G, Soliz J. Does the pathogenesis of SARS-CoV-2 virus decrease at high-altitude? Respir Physiol Neurobiol. 2020;277: 103443.
Segovia-Juarez J, Castagnetto JM, Gonzales GF. High altitude reduces infection rate of COVID-19 but not case-fatality rate. Respir Physiol Neurobiol. 2020;281: 103494.
Burtscher M. Effects of living at higher altitudes on mortality: a narrative review. Aging Dis. 2014;5:274–80.
Luks AM, Swenson ER. Travel to high altitude with pre-existing lung disease. Eur Respir J. 2007;29:770–92.
Sinha S, Ray US, Tomar OS, Singh SN. Different adaptation patterns of antioxidant system in natives and sojourners at high altitude. Respir Physiol Neurobiol. 2009;167:255–60.
Torrance JD, Lenfant C, Cruz J, Marticorena E. Oxygen transport mechanisms in residents at high altitude. Respir Physiol. 1970;11:1–15.
Chiodi H. Respiratory adaptations to chronic high altitude hypoxia. J Appl Physiol. 1957;10:81–7.
Ge RL, Helun G. Current concept of chronic mountain sickness: pulmonary hypertension-related high-altitude heart disease. Wilderness Environ Med. 2001;12:190–4.
Petousi N, Croft QP, Cavalleri GL, Cheng HY, Formenti F, Ishida K, Lunn D, McCormack M, Shianna KV, Talbot NP, Ratcliffe PJ, Robbins PA. Tibetans living at sea level have a hyporesponsive hypoxia-inducible factor system and blunted physiological responses to hypoxia. J Appl Physiol. 1985;2014(116):893–904.
West JB. High-altitude medicine. Am J Respir Crit Care Med. 2012;186:1229–37.
Pasha MA, Newman JH. High-altitude disorders: pulmonary hypertension: pulmonary vascular disease: the global perspective. Chest. 2010;137:13S–19S.
Guo Y, Xing Z, Shan G, Janssens JP, Sun T, Chai D, Liu W, Wang Y, Ma Y, Tong Y, Huang Y, Cao Y, Wang C. Prevalence and Risk Factors for COPD at High Altitude: A Large Cross-Sectional Survey of Subjects Living Between 2100–4700 m Above Sea Level. Front Med (Lausanne). 2020;7: 581763.
Supriya R, Singh KP, Gao Y, Tao D, Cheour S, Dutheil F, et al. Mimicking gene-environment interaction of higher altitude dwellers by intermittent hypoxia training: COVID-19 preventive dtrategies. Biology (Basel). 2022;12(1):6.
Simbana-Rivera K, Jaramillo PRM, Silva JVV, Gomez-Barreno L, Campoverde ABV, Novillo Cevallos JF, Guanoquiza WEA, Guevara SLC, Castro LGI, Puerta NAM, Guayta Valladares AW, Lister A, Ortiz-Prado E. High-altitude is associated with better short-term survival in critically ill COVID-19 patients admitted to the ICU. PLoS ONE. 2022;17:e0262423.
Stephens KE, Chernyavskiy P, Bruns DR. Impact of altitude on COVID-19 infection and death in the United States: A modeling and observational study. PLoS ONE. 2021;16: e0245055.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet. 2020;395:497–506.
Luks AM, Hackett PH. Medical Conditions and High-Altitude Travel. N Engl J Med. 2022;386:364–73.
Yi X, Liang Y, Huerta-Sanchez E, Jin X, Cuo ZX, Pool JE, Xu X, Jiang H, Vinckenbosch N, Korneliussen TS, Zheng H, Liu T, He W, Li K, Luo R, Nie X, Wu H, Zhao M, Cao H, Zou J, Shan Y, Li S, Yang Q, Asan, Ni P, Tian G, Xu J, Liu X, Jiang T, Wu R, Zhou G, Tang M, Qin J, Wang T, Feng S, Li G, Huasang, Luosang J, Wang W, Chen F, Wang Y, Zheng X, Li Z, Bianba Z, Yang G, Wang X, Tang S, Gao G, Chen Y, Luo Z, Gusang L, Cao Z, Zhang Q, Ouyang W, Ren X, Liang H, Zheng H, Huang Y, Li J, Bolund L, Kristiansen K, Li Y, Zhang Y, Zhang X, Li R, Li S, Yang H, Nielsen R, Wang J and Wang J. Sequencing of 50 human exomes reveals adaptation to high altitude. Science. 2010;329:75–8.
Cohen J. The earth is round (p < .05): Rejoinder. American Psychologist. 1995;50:1103.
Acknowledgements
We would like to thank Prof. Jun Lv and Prof. Yuantao Hao in Peking University, School of Public health, for providing the valuable advice on this article. We would like to show our gratitude to the Clinical Research Academy, Peking University Shenzhen Hospital, for providing statistic support in this research.
Funding
YS was supported by National Natural Science Foundation of China (82204148), Shenzhen Science and Technology Innovation Commission Scientific Research Fund Project (JCYJ20220531094401003), Shenzhen's Sanming Project (SZSM201612061), and Scientific Research Foundation of Peking University Shenzhen Hospital (KYQD2022203). QZ was supported by Key Laboratory of Emergency and Trauma (Hainan Medical University), Ministry of Education Grant (KLET-202001). XJ was supported by National Natural Science Foundation of China (32000398); National Natural Science Foundation of China (31900487); Natural Science Foundation of Guangdong Province, China (2017A030306026); Guangdong-Hong Kong Joint Laboratory on Immunological and Genetic Kidney Diseases (2019B121205005); and Guangzhou Basic and Applied Basic Research Program (202201010189). The funders had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
Y. Shan and W. Wang had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. T. Pingcuo, X. Yan, X. Jin were responsible for study concept and design. Y. Shan, D. Liu, W. Wang, W. Chen, X. Wang, J. Zeng were responsible for acquisition of data. Y. Shan, W. Wang were responsible for analysis and interpretation of data. Y. Shan, W. Chen were responsible for drafting of the manuscript. Y. Shan, W. Wang were responsible for statistical analysis. Y. Shan, Q. Zhou and X. Jin were responsible for funding. T. Pingcuo, X. Yan, X. Jin, Y. Shan, Q. Zhai, Q. Luo, Y. Zhang, Z. Zhou, B. La, L. Thuen, Q. Li, G. Tian, X. Chen, Q. Ci, X. Zhu were responsible for administrative, technical, or material support. T. Pingcuo, X. Yan, X. Jin, Y. Shan and Q. Zhou were responsible for study supervision. J. Yan and Q. Zhai were responsible for critical revision of the manuscript for important intellectual content.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study obtained ethics approval from the institutional ethics board of the Third People’s Hospital of Tibet Autonomous Region (No. 2022003). Informed consent was obtained from all the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yan, X., Shan, Y., Luo, Q. et al. COVID-19 in the Tibet, China, the roof of the world: a comparative analysis of high-altitude residents and newcomers. BMC Infect Dis 24, 907 (2024). https://doi.org/10.1186/s12879-024-09831-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09831-x