Abstract
Background
Acinetobacter baumannii is a health threat due to its antibiotic resistance. Herein, antibiotic susceptibility and its association with the Toxin-antitoxin (TA) system genes in A. baumannii clinical isolates from Iran were investigated. Next, we prepared meropenem-loaded chitosan nanoparticles (MP-CS) and investigated their antibacterial effects against meropenem-susceptible bacterial isolates.
Methods
Out of 240 clinical specimens, 60 A. baumannii isolates were assessed. Antibiotic resistance of the isolates against conventional antibiotics was determined alongside investigating the presence of three TA system genes (mazEF, relBE, and higBA). Chitosan nanoparticles were characterized in terms of size, zeta potential, encapsulation efficiency, and meropenem release activity. Their antibacterial effects were assessed using the well diffusion method, minimum inhibitory concentration (MIC), and colony-forming unit (CFU) counting. Their cytotoxic effects and biocompatibility index were determined via the MTT, LDH, and ROS formation assays.
Results
Ampicillin, ceftazidime, and colistin were the least effective, and amikacin and tobramycin were the most effective antibiotics. Out of the 60 isolates, 10 (16.7%), 5 (8.3%), and 45 (75%) were multidrug-resistant (MDR), extensively drug-resistant (XDR), and pandrug-resistant (PDR), respectively. TA system genes had no significant effect on antibiotic resistance. MP-CS nanoparticles demonstrated an average size of 191.5 and zeta potential of 27.3 mV alongside a maximum encapsulation efficiency of 88.32% and release rate of 69.57%. MP-CS nanoparticles mediated similar antibacterial effects, as compared with free meropenem, against the A. baumannii isolates with significantly lower levels of meropenem. MP-CS nanoparticles remarkably prevented A549 and NCI-H292 cell infection by the A. baumannii isolates alongside demonstrating a favorable biocompatibility index.
Conclusion
Antibiotic-loaded nanoparticles should be further designed and investigated to increase their antibacterial effect against A. baumannii and assess their safety and applicability in vivo settings.
Similar content being viewed by others
Introduction
Acinetobacter baumannii is an important nosocomial pathogen that causes various infections including pneumonia, meningitis, sepsis, wound infection, urinary tract infections (UTI), and ventilator-associated pneumonia (VAP). In the case of A. baumannii, increased antibiotic resistance and stability under harsh environmental conditions are considered to be associated with pathogenesis [1, 2]. Recently, the emergence of antibiotic resistance in A. baumannii has become a major health concern [2, 3].
Toxin-antitoxin (TA) systems are small genetic elements present on plasmids or chromosomes of various prokaryotes. In bacteria, TA systems consist of two sets of genes; one set is responsible for coding a “toxin” and the other one is responsible for the expression of a corresponding “antitoxin” [4]. TA systems function as a mechanism to immediately respond to environmental stress including antibiotics and host immune responses [5, 6]. The toxin produced in this system is stable, while the antitoxin is unstable; hence, susceptible to proteolytic degradation [4]. When the antitoxin is degraded, the produced toxin kills the bacteria [7, 8]. Although the TA systems have been reported to be associated with bacterial resistance to agents such as antibiotics, the exact underlying mechanism by which this resistance is conferred has not yet been elucidated [9, 10]. Moreover, A. baumannii is equipped with various TA systems existing on plasmids and/or bacterial chromosomes. These systems belong to the type II TA systems. Among the TA systems found in A. baumannii, three genes, namely mazEF, relBE, and higBA, are the most investigated and important ones that belong to the type II TA system [5, 7, 11,12,13,14]. Previous investigations have studied the relationship between these genes and antibiotic resistance and have asserted that further investigations are necessary. For instance, Coskun and colleagues reported that Pseudomonas aeruginosa and Staphylococcus isolates sensitive to gentamicin, ciprofloxacin, levofloxacin, clindamycin, phosphomycine, nitrofurantoin, fusidic acid, cefoxitin expressed relatively higher levels of the mazEF gene compared with those of the resistant isolates [11]. Based on the findings of a more recent report by Coşkun and colleagues, P. aeruginosa isolates sensitive to imipenem and meropenem expressed significantly higher levels of the relBE gene while isolates sensitive to amikacin significantly expressed higher levels of the higBA gene [13]. Regarding A. baumannii, Ghafourian and colleagues reported that the mazEF gene was expressed by 85 clinical isolates and that this TA system-related expression should be further investigated as an antibacterial therapeutic strategy [7]. However, unlike P. aeruginosa and Staphylococcus, it has not yet been elucidated if there is a correlation between the expression of the mazEF, relBE, and higBA genes and the resistance of A. baumannii isolates to common antibiotics, which was our aim in the current study.
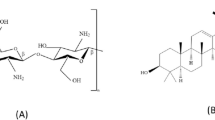
Chitosan (CS) is a natural cationic polysaccharide with amino groups. This property gives chitosan biological activity at low pH levels allowing it to interact with negatively charged molecules including proteins, polysaccharides, and phospholipids found in bacterial cells [15,16,17]. The high biological activity and biocompatibility of chitosan render it a strong candidate as an antibacterial substitute for conventional therapies [15,16,17]. Various studies have demonstrated the applicability of chitosan nanoparticles for antibacterial purposes. For instance, Fu and colleagues have also demonstrated that chitosan-modified polymyxin B-loaded liposomes have significantly higher antibacterial effects against biofilm-forming A. baumannii as compared with polymyxin B alone [18]. Other researchers have also demonstrated that chitosan could be introduced as a potent inhibitor of multidrug-resistant (MDR) A. baumannii [15, 19]. Alongside chitosan, other nanoparticles have also been investigated for their antibacterial effects. For instance, Tiwari and colleagues developed polyvinylpyrrolidone-capped silver nanoparticles and demonstrated that they can be a potent alternative for carbapenem in combating carbapenem-resistant A. baumannii [20].
Based on the increasing importance of MDR A. baumannii in causing various infections, in this study, the prevalence of the type II TA system-related genes mazEF, relBE, and higBA was investigated in the clinical isolates of A. baumannii from patients hospitalized in Iran. In addition, the antibiotic susceptibility patterns of these isolates against various conventional antibiotics were also determined. Next, we evaluated the antibacterial effects of meropenem-loaded chitosan/sodium tripolyphosphate (TPP) nanoparticles (hereafter referred to as MP-CS nanoparticles) on a number of these clinical isolates.
Materials and methods
Sample collection
In the present study, specimens were collected from patients admitted to different wards of Dey Hospital in Tehran, Iran, from January to December 2020. The clinical specimens were obtained from patients who had been hospitalized for at least three consecutive days, and following the confirmation of A. baumannii infection, the bacterial isolates were given to us by the hospital’s Infectious Disease Laboratory for the rest of the experiments. All protocols and experiments carried out in this study were in accordance with the guidelines of the Ethical Committee of the Islamic Azad University of Kazerun, Kazerun Branch, Kazerun, Iran as well as approved by the mentioned committee (approval ID: IR.IAU.KAU.REC.1399.105).
Bacterial isolation and characterization
For A. baumannii isolation, clinical specimens were separately cultured on MacConkey agar (Merck KGaA, Darmstadt, Germany) and blood agar media (Merck KGaA, Darmstadt, Germany) containing 5% sheep blood (Tamad Kala, Tehran, Iran) and incubated at 37 °C for 24 h. After the incubation, the culture plates were examined using Gram staining as A. baumannii are Gram-negative and they appear as short, almost round, rod-shaped Gram-negative bacterium [21]. The suspected colonies were selected for further examination which included culturing on differential culture media such as Triple Sugar Iron (TSI) agar (Merck KGaA, Darmstadt, Germany), Oxidative Fermentative (O-F) media (Merck KGaA, Darmstadt, Germany), and Sulfide Indole Motility (SIM) media (Merck KGaA, Darmstadt, Germany). Moreover, the evaluation of catalase and oxidase activity of the suspected colonies was used for further confirmation. Furthermore, determination of Acinetobacter species was carried out using the carbohydrate fermentation test [22]. The isolated bacteria were stored at -70 °C in Tryptic Soy Broth (TSB; Merck KGaA, Darmstadt, Germany) containing 30% glycerol until further use.
Antibiotic susceptibility
Disk diffusion
The susceptibility of the A. baumannii isolates to antibiotics including ampicillin-sulbactam (10/10 µg), cefotaxime (30 µg), minocycline (30 µg), ceftriaxone (30 µg), ceftazidime (30 µg), meropenem (10 µg), ticarcillin-clavulanate (75/10 µg), gentamicin (10 µg), ciprofloxacin (5 µg), trimethoprim-sulfamethoxazole (1.25/23.75 µg), cefepime (30 µg), piperacillin (100 µg), amikacin (30 µg), and tobramycin (10 µg) was determined using the Kirby-Bauer disk diffusion method (DDM) on Mueller-Hinton agar (Merck KGaA, Darmstadt, Germany) according to the Clinical and Laboratory Standards Institute (CLSI) guidelines [23]. A. baumannii (ATCC19606) was utilized as a control during antibiotic susceptibility tests [24].
Minimum inhibitory concentration (MIC)
The MIC values were determined using the broth microdilution method and the clinical isolates were designated as susceptible, intermediate, or resistant according to the standards of the CLSI [23]. Briefly, ampicillin-sulbactam (MIC values of ≤ 8/4, 16/8, and ≥ 32/16 µg/mL were designated as susceptible, intermediate, and resistant, respectively), cefotaxime (MIC values of ≤ 8, 16–32, and ≥ 64 µg/mL were designated as susceptible, intermediate, and resistant, respectively), ceftriaxone (MIC values of ≤ 8, 16–32, and ≥ 64 µg/mL were designated as susceptible, intermediate, and resistant, respectively), ceftazidime (MIC values of ≤ 8, 16, and ≥ 32 µg/mL were designated as susceptible, intermediate, and resistant, respectively), meropenem (MIC values of ≤ 2, 4, and ≥ 8 µg/mL were designated as susceptible, intermediate, and resistant, respectively), ticarcillin-clavulanate (MIC values of ≤ 16/2, 32/2–64/2, and ≥ 128/2 µg/mL were designated as susceptible, intermediate, and resistant, respectively), gentamicin (MIC values of ≤ 4, 8, and ≥ 16 µg/mL were designated as susceptible, intermediate, and resistant, respectively), ciprofloxacin (MIC values of ≤ 1, 2, and ≥ 4 µg/mL were designated as susceptible, intermediate, and resistant, respectively), trimethoprim/sulfamethoxazole (MIC values of ≤ 2/38 and ≥ 4/76 µg/mL were designated as susceptible and resistant, respectively), cefepime (MIC values of ≤ 8, 16, and ≥ 32 µg/mL were designated as susceptible, intermediate, and resistant, respectively), piperacillin (MIC values of ≤ 16, 32–64, and ≥ 128 µg/mL were designated as susceptible, intermediate, and resistant, respectively), amikacin (MIC values of ≤ 16, 32, and ≥ 64 µg/mL were designated as susceptible, intermediate, and resistant, respectively), tobramycin (MIC values of ≤ 4, 8, and ≥ 16 µg/mL were designated as susceptible, intermediate, and resistant, respectively), minocycline (MIC values of ≤ 4, 8, and ≥ 16 µg/mL were designated as susceptible, intermediate, and resistant, respectively), and colistin (MIC values of ≤ 2 and ≥ 4 µg/mL were designated as intermediate and resistant, respectively) were the investigated antibiotics.
Determination of the MDR, extensively drug-resistant (XDR), and pandrug-resistant (PDR) isolates
The MDR, XDR, and PDR status of the A. baumannii isolates were defined according to a previous report by Magiorakos and colleagues [25]. According to the report, “MDR was defined as acquired non-susceptibility to at least one agent in three or more antimicrobial categories”, while “XDR was defined as non-susceptibility to at least one agent in all but two or fewer antimicrobial categories (i.e. bacterial isolates remain susceptible to only one or two categories)” and “PDR was defined as non-susceptibility to all agents in all antimicrobial categories” [25].
DNA extraction and PCR-assisted confirmation of the TA system genes
The bacterial isolates were cultured in TSB media overnight. DNA extraction was carried out on the fresh overnight cultures of the bacterial isolates using a commercial DNA extraction kit (CinnaGen, Tehran, Iran) according to the manufacturer’s instructions. The extracted DNA was used as the template for conventional PCR assay for determining the presence of mazEF, relBE, and higBA genes. The primers used for the PCR assay were previously designed by Maghraby et al. (Table 1) [26]. For each round of PCR, 3 µg of the template DNA, 2.5 µL of 10X PCR buffer, 0.5 µL of 10 mM dNTPs, 0.75 µL of 50 mM MgCl2, 0.25 µL of 5 U/µL of Taq DNA polymerase, and 25 pmol of each primer (forward and reverse) were mixed and brought to a final volume of 25 µL using sterile DNase/RNase-free double-distilled water (DDW). The PCR amplification assay was carried out with the following thermal conditions: an initial denaturation step at 94 °C for 1 min, followed by 30 cycles consisting of a denaturation step at 94 °C for 1 min, an annealing step at 54 °C for 1 min, and an extension step at 72 °C for 1.5 min, all of which were followed by a final extension step at 72 °C for 10 min. The amplicons were assessed by electrophoresis on 1.5% agarose gel containing 0.5 µg/mL ethidium bromide.
Nanoparticle preparation
In this experiment, the ionic gelation method was used for the preparation of the nanoparticles, as previously described by Elnaggar et al. [27]. In detail, 1 g of chitosan (Sigma Aldrich, United States) was dissolved in 200 mL of acetic acid solution (2%) and was stirred for 30 min at room temperature. Next, 0.2% w/v sodium tripolyphosphate (TPP) solution (prepared using deionized water) was added to the chitosan solution under stirring in a drop-wise manner. The resultant thick emulsion of the prepared chitosan/TPP nanoparticles was allowed to sediment which was followed by ultracentrifugation (Beckman, California, US) at 25,000 rpm for 30 min to purify the nanoparticles. The precipitate of the purified nanoparticles was stored at 4 ˚C until further use.
For the preparation of the meropenem-loaded chitosan/TPP nanoparticles, a 0.015% w/v chitosan solution was prepared using 2% v/v acetic acid. Next, 0.006% w/v sodium TPP solution was prepared using deionized water, and different concentrations of meropenem (with final concentrations of 0.5, 1, and 1.85 µg) were added to it under continuous stirring [28]. The resultant sodium TPP/meropenem solution was added to the chitosan solution under stirring for 30 min in a drop-wise manner. The resultant thick emulsion of the prepared meropenem-loaded chitosan/TPP nanoparticles was allowed to sediment and was centrifuged at 25,000 rpm for 30 min to purify the nanoparticles. The precipitate of the purified nanoparticles was stored at 4 ˚C until further use.
Characterization of nanoparticles
Particle size, polydispersity index (PDI), and ζ potential
The particle size, PDI, and ζ potential of the prepared nanoparticles were determined by the dynamic light scattering technique using a particle analyzer. Of note, the nanoparticle-containing samples were appropriately diluted with double distilled water before the measurements, and all of the measurements were performed in triplicate.
Encapsulation efficiency
A previously described method was used to evaluate the encapsulation efficiency of the prepared nanoparticles [29, 30]. First, the nanoparticles were diluted with phosphate-buffered saline (PBS; 1:10 v/v). Next, the samples were centrifuged at 15,000 rpm at 4 ˚C for 15 min. The absorption of the resultant supernatant was measured by a UV-visible spectrophotometer instrument (UV-1800, Shimadzu, Japan) at the wavelength of 260 nm to measure the unentrapped drug. Of note, methanol was used as the blank. Finally, the encapsulation efficiency of the prepared nanoparticles was calculated using the following formula:
In vitro drug release
The release rate of meropenem from the prepared meropenem-loaded chitosan/TPP nanoparticles was measured using the membrane diffusion method as previously described [30]. The absorbance of each of the samples was measured at least three times at the wavelength of 298 nm to calculate the concentration of meropenem [31].
Antibacterial effects of the nanoparticles
The in vitro antibacterial effects of the prepared nanoparticles were assessed using the well diffusion method as previously described [32, 33]. The Mueller Hinton agar plates were prepared. Following the solidification of the prepared plates, colonies of A. baumannii isolates were selected from overnight culture plates and inoculated on Mueller Hinton agar plates. Next, wells were punched out using a 0.7 cm cork borer. 100 µL of each nanoparticle sample, or meropenem (at the final concentration of 10 µg as per the CLSI guidelines), were separately pipetted into different wells [23]. Finally, the plates were incubated at 37 °C for 12 h. After this, the radius of the clear bacterial inhibition zone around each of the wells was carefully measured. Furthermore, the MIC values against the bacterial isolates were evaluated using the microdilution method to further determine the antibacterial effects of the prepared nanoparticles. Of note, in both well diffusion and microdilution tests, meropenem and double-distilled water were used as the positive and negative control, respectively.
Cell culture
The A549 cell line (which is a human alveolar basal epithelial cell line) and the NCI-H292 cell line (which is a mucoepidermoid pulmonary carcinoma cell line) were obtained from the Iranian Biological Resource Center (IBRC; Tehran, Iran) and American Type Culture Collection (ATCC, United States), respectively. These two cell lines were selected as they have been previously used as cell models for A. baumannii infection [34,35,36,37,38]. The A549 cells were cultured in high glucose Dulbecco’s Modified Eagle Medium (DMEM; Gibco, United States) which was supplemented with 10% (v/v) heat-inactivated fetal bovine serum (FBS; Gibco, California, United States). Moreover, the NCI-H292 cells were cultured in RPMI-1640 (Gibco, United States) supplemented with 10% FBS. Additionally, the culture media was supplemented with amphotericin B (2.5 µg/mL), vancomycin (50 µg/mL), gentamicin (50 µg/mL), and 1% 4-(2-hydroxyethyl)piperazine-1-ethane-sulfonic acid (HEPES). All of the cell cultures were incubated in an incubator at 37 ˚C with 5% CO2 in a humidified condition.
Cell line and bacterial culture preparation for infection
A549 and NCI-H292 cells in the growth phase were washed twice using PBS. Next, the cells were detached using a 0.05% trypsin-ethylenediaminetetraacetic acid (EDTA) solution and were centrifuged at 1500 rpm for 5 minutes. The resultant cell pellet was resuspended in room temperature DMEM (supplemented with 10% v/v FBS but without antibiotics) to obtain a cell concentration of 2 × 105 cells/mL. At the same time, the bacterial isolates were grown in 100 mL of LB broth at 37 ˚C (with 200 rpm agitation) until an optical density of 0.6 at the wavelength of 600 nm was obtained. The colony-forming unit (CFU) of the bacterial isolates was calculated before the infection experiment. Of note, A. baumannii ATCC 19,606 was used as the reference bacteria. Moreover, from the clinical isolates susceptible to meropenem, two isolates were selected for the further steps of the investigations.
Cell infection
A549 and NCI-H292 cells were cultured until reaching a contamination-free confluency rate of more than 90%. Next, the cells were washed twice with PBS, and 1 mL of fresh room temperature DMEM (supplemented with 10% v/v FBS but without antibiotics) was added to each well (6-well cell culture plates). The bacterial isolates were added to the cell-containing wells with a multiplicity of infection (MOI) of 3:1 indicating 1.2 × 107 bacteria CFUs:0.4 × 107 A549 cells. The plates were incubated at 37 ˚C containing 5% CO2 for 24 h.
CFU counting
The population of the bacterial isolates after infection was classified into four categories which include [1] before coinfection [2], remaining non-interacting during coinfection [3], interacting or adhered bacteria on the surface of A549 or NCI-H292 cells, and [4] bacteria internalized into the cells. Of note, there were four different methods used for the calculation of CFU of the bacteria of each of these four categories. Briefly, for the CFU calculation of bacteria remaining non-interacting during coinfection, the suspension culture in DMEM media which contained the free bacteria was used while for the CFU calculation of interacting or adhered bacteria on the surface of the cells, the cell culture media were gently first aspirated and the cells were detached and centrifuged. Next, the cell pellet was resuspended again and a sample of the solution was used for CFU calculation. Ultimately, for the CFU calculation of bacteria internalized into the cells, samples were taken after the homogenization of the cells. Of note, CFU calculation was performed according to a method previously reported by Tiwari and colleagues [20].
Cytotoxic effect of the nanoparticles on A549 and NCI-H292 cells
The in vitro cytotoxicity of the MP-CS nanoparticles on the A549 and NCI-H292 cell lines was investigated using the MTT assay (MTT Assay Kit; Abcam, Cambridge, UK) and LDH assay (LDH Assay Kit; Abcam, Cambridge, UK) as per the manufacturer’s instructions. Briefly, the effects of the different concentrations of the nanoparticles on the viability of the A549 and NCI-H292 cells were investigated to determine the IC50 and the non-toxic dose of the MP-CS nanoparticles. Of note, the cells were seeded in 96-well cell culture plates for 24 h for both of the assays.
Evaluation of reactive oxygen species (ROS) formation
The cells were seeded in the wells of an ELISA plate and after adhering to the bottom of the wells, a proportion of the culture medium was replaced with 50 µL of the 0.5% nitroblue tetrazolium (NBT) solution. The plate was incubated for 1.5 h and then the supernatant was carefully discarded. Next, the wells were supplied with 200 µL absolute methanol for cell fixation and then washed twice with PBS. The wells were left to dry at room temperature, after which the cells were exposed to 150 µL KOH (2 M) for cell membrane disruption. In the following, 150 µL dimethyl sulfoxide (DMSO; Sigma-Aldrich, United States) was added to each well for the dissolution of the formazan crystals. Ultimately, the absorbance of each well was measured at 620 nm.
Statistical analysis
The data pertaining to the association between the risk factors were analyzed by Chi-square with a confidence level of 95% using the IBM SPSS statistics software (version 27; IBM, United States). Moreover, one-way ANOVA and Student’s t-test were used for statistical analysis between the experimental groups as performed using the GraphPad Prism software (version 10.1.0; GraphPad Software, San Diego, California, United States). A p-value < 0.05 was considered statistically significant.
Results
Demographic data
A total number of 240 clinical specimens (of which 88, 53, 45, 33, and 21 specimens were derived from the blood, urine, sputum, respiratory secretions, and skin wounds of the patients, respectively) were collected from 60 patients; out of which, a total number of 60 A. baumannii isolates were selected randomly in a way that no more than one isolate was selected from each patient. Out of the selected A. baumannii isolates, 24 belonged to female patients (40%) and 36 belonged to male patients (60%).
Among them, the most bacterial isolates were derived from trachea (31; 51.7%), throat (6; 10%), sputum (5; 8.3%), urinary catheterization (5; 8.3%), axillary (3; 5%), abdominal wound (2; 3.3%), chest wound (2; 3.3%), inguinal (2; 3.3%), central venous port (1; 1.7%), nose (1; 1.7%), nasogastric tube (1; 1.7%), and sternum (1; 1.7%). Among the causes of hospitalization (Table 2), respiratory issues (17; 28.3), heart surgery (6; 10%), heart issues (6; 10%), abdominal surgery (6; 10%), cancer (6; 10%), and stroke (5; 8.3%) were the most frequent causes of hospitalization of the patients infected with A. baumannii.
Antibiotic resistance patterns
According to the results (Tables 3 and 4), ampicillin-sulbactam (60; 100%), colistin (60; 100%), ceftazidime (60; 100%), cefotaxime (59; 98.3%), ceftriaxone (59; 98.3%), piperacillin (59; 98.3%), ticarcillin-clavulanate (59; 98.3%), minocycline (59; 98.3%), gentamicin (58; 96.7%), cefepime (58; 96.7%), meropenem (58; 96.7%), and ciprofloxacin (58; 96.7%) were among the used antibiotics to which most of the A. baumannii isolates showed resistance. Moreover, amikacin (51; 85%) and tobramycin (51; 85%) were the tested antibiotics against which the lowest rates of resistance were observed. In this study, out of the 60 bacterial isolates, 59 isolates (98.34%) were resistant to more than eight of the tested antibiotics and only 1 isolate (1.66%) demonstrated susceptibility to seven of the tested antibiotics.
Determination of the MDR, XDR, and PDR isolates
Our findings demonstrated that out of the 60 clinical isolates, 10 (16.7%), 5 (8.3%%), and 45 (75%) were MDR, XDR, and PDR, respectively. Further analyses indicated no significant relationship between the age of the patients, the sex of the patients, the hospitalization ward, and the isolation site with the MDR, XDR, and PDR status of the bacterial isolates (p = 0.666, p = 0.361, p = 0.606, p = 0.208, respectively). However, the only significant relationship between the antibiotic resistance status of the bacterial isolates was found with the hospitalization cause of the patients from whom the isolates were derived (p = 0.025).
Distribution of the TA system genes
In the present study, the prevalence of the mazEF, relBE, and higBA genes in 60 A. baumannii clinical isolates was investigated. According to the results, mazEF, relBE, and higBA were present in 24 (40%), 32 (53.3%), and 35 (58.3%) of the bacterial isolates, respectively. Moreover, 6 (10%) clinical isolates were negative for all of the investigated genes, meaning that 54 (90%) of the clinical isolates contained at least one of the studied genes.
Further analyses indicated that there is no significant relationship between the presence of the mazEF, relBE and higBA genes in the clinical isolates with their resistance to the investigated antibiotic agents (Table 5). Moreover, it was demonstrated that the presence or absence of the mazEF, relBE, and higBA genes had no significant effect on the MDR, XDR, or PDR status of the clinical isolates (Table 6).
It was also discovered that the sex of the patients from whom the A. baumannii isolates were collected had no significant effects on the presence or the absence of the mazEF, relBE, and higBA genes in the bacterial isolates (p = 0.747, p = 0.139, and p = 0.109, respectively). In reference to the age of the patients from whom the clinical isolates were collected and the presence or the absence of the mazEF, relBE, and higBA genes, no significant relationship was found according to the results (p = 0.555, p = 0.894, and p = 0.390, respectively). Additionally, the sources from which the A. baumannii isolates were derived had no significant effect on the presence or the absence of the mazEF, relBE, and higBA genes in the bacterial isolates (p = 0.198, p = 0.437, and p = 0.741, respectively). Moreover, it was also revealed that there is no significant relationship between the patients’ hospitalization ward and the presence or the absence of the mazEF, relBE, and higBA genes in the clinical isolates (p = 0.504, p = 0.615, and p = 0.384, respectively). Ultimately, it was elucidated that the cause of hospitalization had no significant correlation with the presence or the absence of the mazEF, relBE, and higBA genes (p = 0.487, p = 0.552, and p = 0.381, respectively).
Nanoparticle characterization
DLS results demonstrated that the CS nanoparticles had a mean size of 180.1 ± 7.2 nm with a PI of 0.35 while the MP-CS nanoparticles demonstrated an average size of 191.5 ± 5.3 nm with a PI of 0.32. Moreover, the zeta potential of the CS and MP-CS nanoparticles were 24.8 and 27.3 mV, respectively.
Encapsulation efficiency
Herein, we investigated the encapsulation efficiency of the prepared nanoparticles using three different concentrations of meropenem (0.5, 1, and 1.85 µg). According to our results (Fig. 1a), the nanoparticles demonstrated an encapsulation efficiency of 59.42 ± 3.43% at the concentration of 0.5 µg, which was significantly lower than the concentrations of 1 and 1.85 µg with the encapsulation efficiencies of 81.44 ± 5.23 and 88.32 ± 6.46%, respectively (p < 0.01 for both comparisons). Of note, the concentrations of 1 and 1.85 µg meropenem did not show any significant difference in their encapsulation efficiency rates. Therefore, the concentration of 1.85 µg was selected for the rest of the experiment.
In vitro drug release
Our meropenem-loaded nanoparticles demonstrated an in vitro release rate of around 69% after 8 h (Fig. 1b). A burst release pattern was observed during the first two hours as the nanoparticles had release rates of 7.435 ± 2.534, 10.243 ± 1.795, 19.812 ± 2.353, 29.44 ± 4.364, and 43 ± 3.694% at 15 min, 30 min, 60 min, 90 min, and 2 h, respectively. After this, the release pattern of the nanoparticles shifted toward a more gradual behavior, exhibiting release rates of 50.439 ± 4.543, 55.145 ± 3.598, 61.345 ± 4.342, and 69.574 ± 3.534% at 3 h, 4 h, 6 h, and 8 h, respectively.
Antibacterial effects of the nanoparticles
In regard to the in vitro antibacterial activity of the nanoparticles, a well diffusion assay was conducted. In regard to the A. baumannii (ATCC19606) strain (Fig. 2a), meropenem, the CS nanoparticles, and the MP-CS nanoparticles demonstrated the lowest to highest inhibition zones, respectively. Moreover, the inhibition zones caused by the loaded and unloaded nanoparticles were both significantly higher than those of free meropenem (p < 0.05 and p < 0.001, respectively). Furthermore, the MP-CS nanoparticles caused inhibition zones significantly greater than those of the CS nanoparticles (p < 0.01). In regard to clinical isolate #1 (Fig. 2b), meropenem, the CS nanoparticles, and the MP-CS nanoparticles demonstrated the lowest to highest inhibition zones, respectively. However, the CS nanoparticles did not cause inhibition zones significantly different from those caused by free meropenem. On the other hand, the inhibition zone caused by the MP-CS nanoparticles was significantly greater than those of the free meropenem and the CS nanoparticles (p < 0.01 and p < 0.05, respectively). In regard to clinical isolate #2 (Fig. 2c), the greatest inhibition zone was caused by the MP-CS nanoparticles followed by the CS nanoparticles and free meropenem. The antibacterial effects of the MP-CS nanoparticles were significantly higher than those caused by free meropenem and the CS nanoparticles (p < 0.0001 for both comparisons). Moreover, the CS nanoparticles also caused inhibition zones significantly greater than those mediated by free meropenem (p < 0.01).
Assessment of the antibacterial effects of the MP-CS nanoparticles. The antibacterial effects of meropenem, the CS nanoparticles, and the MP-CS nanoparticles on A. baumannii (ATCC19606) strain (a), A. baumannii strain #1 (b), and A. baumannii strain #2 (c) assessed via the well diffusion method. The minimum inhibitory concentrations of the CS nanoparticles and MP-CS nanoparticles on A. baumannii (ATCC19606) strain (d), A. baumannii strain #1 (e), and A. baumannii strain #2 (f). The minimum inhibitory concentrations of meropenem and meropenem encapsulated in the MP-CS nanoparticles (at their corresponding minimum inhibitory concentrations) on A. baumannii (ATCC19606) strain (g), A. baumannii strain #1 (h), and A. baumannii strain #2 (i). NPs, nanoparticles. Data are expressed as mean ± standard deviation. All experiments were performed in triplicate (n = 3). *, **, ***, ****, and ns represent p < 0.05, p < 0.01, p < 0.001, p < 0.0001, and p > 0.05, respectively
In regard to MIC, the MP-CS nanoparticles demonstrated significantly lower MIC values against the A. baumannii (ATCC19606) strain, A. baumannii strain #1, and A. baumannii strain #2 in comparison with their unloaded counterparts (103 vs. 162, 161 vs. 265, and 202 vs. 310 µg/mL, respectively; p < 0.001, p < 0.001, p < 0.01, respectively) (Fig. 2d, e, and f, respectively). A comparison between the concentrations of the meropenem encapsulated in the MP-CS nanoparticles (calculated at the corresponding MIC concentrations of the MP-CS nanoparticles) with the concentration of free meropenem demonstrated that a significantly lower concentration of the antibiotic was required to reach the MIC value against the A. baumannii (ATCC19606) strain, A. baumannii strain #1, and A. baumannii strain #2 (0.0558 vs. 1.49, 0.0873 vs. 1.6, and 0.1096 vs. 1.85 µg/mL, respectively; p < 0.001, p < 0.001, p < 0.01, respectively) (Fig. 2g, h, and i, respectively).
CFU counting
The results of the CFU counting experiment, at different stages of A. baumannii infection in the presence and absence of the MP-CS nanoparticles have been summarized in Table 7. The CFU count of the bacteria internalized into A549 and NCI-H292 cells was around 14–26% when the cells were co-cultured with the A. baumannii strains. However, this count remarkably dropped to around 1–4% when the cells were treated with MP-CS nanoparticles during the co-infection step. Moreover, the CFU count of bacteria interacting or adhering on the surface of A549 or NCI-H292 cells dropped from around 30–37% to 2-3.5% while the cells were under the MP-CS nanoparticle treatment. Moreover, the CFU count of bacteria remaining non-interacting during coinfection was around 93–96% when the cells were treated with the MP-CS nanoparticles during the co-infection step.
Cytotoxic effects of the nanoparticles on A549 and NCI-H292 cells
The cytotoxic effects of the MP-CS nanoparticles on the viability of A549 and NCI-H292 cells were assessed via the MTT and LDH assays. The results of the MTT assay demonstrated that the concentrations at which the nanoparticles exhibited antibacterial activity had no negative effect on the viability of A549 and NCI-H292 cells (Fig. 3a and b). Of note, the IC50 values for the MP-CS nanoparticles were calculated as 726.9 µg/mL (R2 = 0.9748) against the A549 cells and 643.1 µg/mL (R2 = 0.9709) against the NCI-H292 cells, which were around four-fold higher than the concentration at which the nanoparticles showed antibacterial activity (meaning MIC). In regard to the results of the MTT assay, the concentrations of 100, 200, and 300 µg/mL of the MP-CS nanoparticle did not significantly reduce the viability of A549 and NCI-H292 cells in comparison with those of the control groups. However, at the concentration of 400 µg/mL, the cell viability rates of both A549 and NCI-H292 cells declined to around 86.04 and 84.5%, respectively, which were significantly lower in comparison with those of the corresponding control groups (p < 0.0001).
Assessment of the effect of MP-CS nanoparticles on the viability of A549 and NCI-H292 cells via the MTT (a and b, respectively) and LDH assays (c and d, respectively). Data are expressed as mean ± standard deviation. NPs, nanoparticles. All experiments were performed in triplicate (n = 3). *, ****, and ns represent p < 0.05, p < 0.0001, and p > 0.05, respectively
In contrast with the MTT assay results, which determine the number of living cells, the LDH assay measures the number of dead cells. Briefly, LDH is released into the cell culture medium upon cell membrane disruption and cell death which could be correlated to cell death rate. For the simplification of the comparison between the results of the MTT assay and LDH assay, we expressed the results of the LDH assay as the percentage of the living cells. According to our findings (Fig. 3c and d), the MP-CS nanoparticles at the concentrations of 100 and 200 µg/mL did not significantly reduce the viability of A549 and NCI-H292 cells in comparison with those of the corresponding control groups. However, a significant reduction in the viability of A549 and NCI-H292 cells was observed at the concentrations of 300 and 400 µg/mL in comparison with those of the corresponding control groups (p < 0.05 and p < 0.0001, respectively).
Evaluation of ROS formation
Our results demonstrated that the infection of A549 and NCI-H292 cells with A. baumannii significantly increased the level of formed ROS in comparison with those of the uninfected cell groups (p < 0.0001 for both cell lines) (Fig. 4). However, treatment of the infected cells with the MP-CS nanoparticles significantly lowered the ROS level in comparison with those of the corresponding infected cells (p < 0.0001 for both cell lines). Moreover, it was also demonstrated that the levels of ROS following the treatment of the infected A549 and NCI-H292 cells with the MP-CS nanoparticles were comparable to those of the uninfected (control) corresponding cells (p > 0.05 for both comparisons), demonstrating no negative effects on the viability of the infected cells as a result of the MP-CS nanoparticle treatment.
Discussion
In this study, out of 240 clinical specimens, 60 (25%) isolates were identified as A. baumannii. Such infection frequency was consistent with that of a study by Babapour and colleagues in which 24% of the bacterial isolates collected from patients in three hospitals in Tehran, Iran were identified as A. baumannii [39]. A comparison between the results of this study with those of other similar studies in other countries demonstrates that the infection frequency of this bacterium in clinical isolates collected in Iran is higher than those of the other countries [40, 41]. The reason for this higher A. baumannii infection rate in Iranian hospitalized patients can be a subject of further investigation.
According to our results, the highest rate of A. baumannii isolates was collected from the trachea specimens (31 isolates; 51.7%), which is consistent with the findings reported in a study by Alkasaby and colleagues [42]. Furthermore, as reported by Maghraby et al., the majority of A. baumannii isolates were related to chest infection specimens [26]. However, Al Mobarak et al. reported some contradicting results in this regard as they reported that A. baumannii isolates were mainly isolated from wounds, respiratory secretions, urine, and blood [43]. Such differences can be elucidated and justified by studying a larger number of specimens, the underlying medical conditions that led to the hospitalization of the patients, and the general hospitalization conditions.
Based on our results, all of the 60 A. baumannii isolates (100%) were resistant to ampicillin, ceftazidime, and colistin; therefore, these antibiotics were designated the most infective ones. On the other hand, as 9 isolates (15%) demonstrated susceptibility to amikacin and tobramycin, these two antibiotics were regarded as the most effective antibiotics in this study. However, since a high rate of resistance to antibiotics by the bacterial isolates was observed in this investigation, these findings are consistent with the findings of previous studies which reported that most A. baumannii strains isolated in Iran were resistant to first-line antibiotics, including aminoglycosides, fluoroquinolones, and carbapenems [44,45,46].
The widespread resistance of A. baumannii to different groups of antimicrobial agents has been previously reported by various studies conducted in Iran. For instance, in a study by Fazeli et al. in which 121 isolates of A. baumannii were isolated from different hospitals in Isfahan, Iran, the investigators reported that these bacterial strains were highly resistant to common antibiotics including cefotaxime (100%), ceftriaxone (100%), meropenem (100%), ciprofloxacin (100%), aztreonam (100%), cefepime (99.2%), trimethoprim-sulfamethoxazole (99.2%), tetracycline (92.6%), amikacin (87.6%), tobramycin (86.8%), and ampicillin-sulbactam (33.9%) [47]. Moreover, Karimi et al. reported that among 60 A. baumannii isolates obtained from Hazrat-e-Rasoul Hospital in Tehran, 93.3% were resistant to ceftazidime and 91.6% were resistant to amikacin, which is consistent with our results. Also, they reported that 3.3% of their bacterial isolates were resistant to colistin making it the most effective antibiotic [48].
In the current study, 10 (16.7%), 5 (8.3%), and 45 (75%), of the clinical isolates were MDR, XDR, and PDR, respectively. Our results were rather different from those conducted and reported by other researchers in Iran [44, 49,50,51]. For instance, in a study by Fazeli et al., it was reported that 62.8% of the A. baumannii isolates were considered XDR [47]. It is worth mentioning that as the findings of the present study and similar studies conducted in Iran indicate, antibiotic resistance and the emergence of MDR strains of A. baumannii are rapidly increasing and this topic requires meticulous molecular and clinical attention [44, 49,50,51]. Furthermore, novel prevention and treatment strategies against A. baumannii infections are urgently warranted.
The prevalence of the TA system genes in the A. baumannii isolates was also investigated in this study. The mazEF, relBE, and higBA genes were present in 24 (40%), 32 (53.33%), and 35 (58.3%) bacterial isolates, respectively. In addition, 6 isolates (10%) were negative for the three investigated genes. To our knowledge, only a few studies have investigated the prevalence and functionality of the TA system genes in bacterial isolates. According to a similar study on 27 A. baumannii isolates, 62.9% had the mazEF gene, 81.5% had the relBE gene, and 29.6% had the higBA gene [26]. As reported by Ghafourian et al., the chromosomal DNA of all of the A. baumannii isolates (100%) were positive for mazEF, and that relBE was found in the chromosomal DNA of only 88.2% of the bacterial isolates whereas higBA was the least prevalent gene (4.7%) in the bacterial isolates [7]. In contrast, as performing PCR on the plasmid DNA of the bacterial isolates did not result in the amplification of any of the mentioned TA system genes, it was concluded that maintenance of the TA systems is through chromosomal genes in A. baumannii [7].
Previous studies have also investigated the TA systems in other bacterial species as well. For instance, Savari et al. found that both the relBE and higBA genes are present in all of the isolates of P. aeruginosa investigated [52]. In another study conducted by Hemati et al., the relBE gene was present in all of the P. aeruginosa isolates investigated [53]. According to Moritz and colleagues, the TA system genes were also prevalent in vancomycin-resistant enterococci, with mazEF and relBE being present in 100 and 44% of the bacterial isolates, respectively [14].
Regarding the characterization of the nanoparticles, other researchers have also used the same technique for the preparation of CS nanoparticles and have reported results consistent with our findings. For instance, Mahboubi Kancha et al. have reported an average size of around 170–200 nm for CS nanoparticles [54, 55]. The zeta potentials of our nanoparticles are also similar to those reported by Mahboubi Kancha et al. as these researchers have reported a zeta potential of around 25–30 mV for their CS nanoparticles [54, 55].
Other researchers have also reported encapsulation efficiency rates of around 75–80% for CS nanoparticles loaded with different drugs other than meropenem [54, 55]. These values are consistent with the findings of our experiments. CS nanoparticles have also been used for the delivery of other antibiotics such as colistin and imipenem. According to an investigation by Elnaggar and colleagues, entrapment efficiency of around 75% for CS nanoparticles loaded colistin has been reported [56]. In a 2023 report, Mufti and colleagues reported an encapsulation efficiency of around 87% for the encapsulation of imipenem into CS nanoparticles [57]. Such findings accentuate the capacity of CS nanoparticles for the encapsulation of antibiotics.
Similar sustained drug release patterns from CS nanoparticles have been reported by other researchers. According to a recent investigation, a drug release rate of around 60% from CS nanoparticles loaded with a particular snake’s venom has been reported [54], which is slightly lower than our reported release rate. According to another investigation, the release rate of berberine from loaded CS nanoparticles has been reported to be around 77% [55]. Based on the findings of Elnaggar et al., around 27% release of colistin from CS nanoparticles after 2 h has been documented which is similar to our findings (which was 43 ± 3.694) [56].
Researchers investigating nanoparticles for the delivery of antibiotics have also reported that such nanoparticles could mediate antibacterial effects themselves. According to Mufti and colleagues, it was demonstrated that CS nanoparticles loaded with imipenem could mediate antibacterial effects in vitro and that the loading of these nanoparticles enhanced their antibacterial impact against A. baumannii [57]. Other types of nanoparticles have also been developed and evaluated for the delivery of antibiotics against antibiotic-resistant bacterial strains. For instance, in a report by Shaaban and colleagues, it was demonstrated imipenem/cilastatin-loaded poly Ɛ-caprolactone nano-formulations improved the antibacterial activity of imipenem against imipenem-resistant clinical isolates of Klebsiella pneumoniae and P. aeruginosa in comparison with free imipenem or cilastatin [58]. In 2023, Gui and colleagues also reported that pH-responsive imipenem-loaded nanocarriers demonstrated synergistic antibacterial effects against A. baumannii [59]. These findings are consistent with our results and highlight the applicability of nanoparticles for the delivery of antibiotics against various bacterial pathogens.
CS nanoparticles’ outstanding qualities such as their biocompatibility and low cytotoxic effects have attracted a lot of attention in the field of biomedical research [60,61,62]. For instance, Friedman et al. have reported that not only CS nanoparticles do not trigger immunological responses but they also demonstrated anti-inflammatory activity as these nanoparticles prevented the production of inflammatory cytokines induced by Propionibacterium acnes in human monocytes and keratinocytes [63]. Because of this property, CS nanoparticles can be used in tissue engineering, targeted drug delivery, and other therapeutic interventions [60, 62, 64]. Herein, we demonstrated that CS nanoparticles can be loaded with meropenem to mediate antibacterial effects at concentrations that do not mediate significant cytotoxic effects against A549 and NCI-H292 cells. Our findings are consistent with other similar studies. For instance, researchers have reported that CS nanoparticles cross-linked with either TPP or hydroxypropyl methylcellulose phthalate (HPMCP) do not cause significant cytotoxicity on the viability of mesenchymal stem cells [55].
Conclusion
Due to the high antibiotic resistance rate, there is an urgent need for effective surveillance to control A. baumannii in Iran. Management of treatment, such as assessing the sensitivity of the bacterial strains to certain antibiotics before the treatment of the patients to find the most suitable antibiotic(s), and patient hospitalization until the resolution of the infection can be considered as possible solutions to prevent further spread of the resistant bacterial strains. Herein, we demonstrated that there is no significant correlation between the presence of the mazEF, relBE, and higBA genes and the resistance of the A. baumannii clinical isolates to the investigated antibiotics or their MDR, XDR, or PDR status. Moreover, we reported that CS nanoparticles encapsulated with meropenem can mediate antibacterial effects against meropenem-susceptible clinical isolates of A. baumannii derived from patients hospitalized in Iran. Such antibacterial effects were mediated in a synergistic fashion as unloaded CS nanoparticles also demonstrated antibacterial effects; therefore, the encapsulation of meropenem into the CS nanoparticles resulted in potent antibacterial effects with significantly lower concentrations of meropenem. Since meropenem is an antibiotic to which a proportion of antibiotic-resistant A. baumannii clinical isolates are susceptible, improving the antibacterial effects of this antibiotic can be leveraged to fight A. baumannii infections that are susceptible to meropenem and are resistant to other antibiotics. These nano-delivery systems are hoped and believed to provide new a direction for combating drug-resistant bacterial infections.
Data availability
All data generated or analysed during this study are included in this published article.
Abbreviations
- UTI:
-
Urinary tract infections
- VAP:
-
Ventilator-associated pneumonia
- TA:
-
Toxin-antitoxin
- CS:
-
Chitosan
- MDR:
-
Multidrug-resistant
- TPP:
-
Sodium tripolyphosphate
- MP-CS:
-
Meropenem-loaded chitosan/sodium tripolyphosphate nanoparticles
- TSI:
-
Triple Sugar Iron
- O-F:
-
Oxidative Fermentative
- SIM:
-
Sulfide Indole Motility
- TSB:
-
Tryptic Soy Broth
- DDM:
-
Disk diffusion method
- CLSI:
-
Clinical and Laboratory Standards Institute
- MIC:
-
Minimum inhibitory concentration
- XDR:
-
Extensively drug-resistant
- PDR:
-
Pandrug-resistant
- DDW:
-
Double-distilled water
- TPP:
-
Tripolyphosphate
- PDI:
-
Polydispersity index
- PBS:
-
Phosphate-buffered saline
- IBRC:
-
Iranian Biological Resource Center
- ATCC:
-
American Type Culture Collection
- DMEM:
-
Dulbecco’s Modified Eagle Medium
- FBS:
-
fetal bovine serum
- HEPES:
-
4-(2-hydroxyethyl)piperazine-1-ethane-sulfonic acid
- EDTA:
-
ethylenediaminetetraacetic acid
- CFU:
-
Colony-forming unit
- NBT:
-
Nitroblue tetrazolium
- DMSO:
-
Dimethyl sulfoxide
- HPMCP:
-
Hydroxypropyl methylcellulose phthalate
References
Houang ET, Chu YW, Leung CM, Chu KY, Berlau J, Ng KC, et al. Epidemiology and infection control implications of Acinetobacter spp. in Hong Kong. J Clin Microbiol. 2001;39(1):228–34.
Michalopoulos A, Falagas ME. Treatment of Acinetobacter infections. Expert Opin Pharmacother. 2010;11(5):779–88.
Ellis D, Cohen B, Liu J, Larson E. Risk factors for hospital-acquired antimicrobial-resistant infection caused by Acinetobacter baumannii. Antimicrob Resist Infect Control. 2015;4:40.
Qiu J, Zhai Y, Wei M, Zheng C, Jiao X. Toxin-antitoxin systems: classification, biological roles, and applications. Microbiol Res. 2022;264:127159.
Jurenaite M, Markuckas A, Suziedeliene E. Identification and characterization of type II toxin-antitoxin systems in the opportunistic pathogen Acinetobacter baumannii. J Bacteriol. 2013;195(14):3165–72.
Makarova KS, Wolf YI, Koonin EV. Comprehensive comparative-genomic analysis of type 2 toxin-antitoxin systems and related mobile stress response systems in prokaryotes. Biol Direct. 2009;4:19.
Ghafourian S, Good L, Sekawi Z, Hamat RA, Soheili S, Sadeghifard N, et al. The mazEF toxin-antitoxin system as a novel antibacterial target in Acinetobacter baumannii. Mem Inst Oswaldo Cruz. 2014;109(4):502–5.
Ghafourian S, Raftari M, Sadeghifard N, Sekawi Z. Toxin-antitoxin systems: classification, Biological function and application in Biotechnology. Curr Issues Mol Biol. 2014;16:9–14.
Gerdes K, Maisonneuve E. Bacterial persistence and toxin-antitoxin loci. Annu Rev Microbiol. 2012;66:103–23.
Kolodkin-Gal I, Verdiger R, Shlosberg-Fedida A, Engelberg-Kulka H. A differential effect of E. Coli toxin-antitoxin systems on cell death in liquid media and biofilm formation. PLoS ONE. 2009;4(8):e6785.
Coskun USS, Cicek AC, Kilinc C, Guckan R, Dagcioglu Y, Demir O, et al. Effect of mazEF, higBA and relBE toxin-antitoxin systems on antibiotic resistance in Pseudomonas aeruginosa and Staphylococcus isolates. Malawi Med J. 2018;30(2):67–72.
Williams JJ, Halvorsen EM, Dwyer EM, DiFazio RM, Hergenrother PJ. Toxin-antitoxin (TA) systems are prevalent and transcribed in clinical isolates of Pseudomonas aeruginosa and methicillin-resistant Staphylococcus aureus. FEMS Microbiol Lett. 2011;322(1):41–50.
Coşkun U, Dagcioglu Y. Evaluation of toxin-antitoxin genes, antibiotic resistance, and virulence genes in Pseudomonas aeruginosa isolates. Rev Assoc Med Bras (1992). 2023;69(1):51–5.
Moritz EM, Hergenrother PJ. Toxin-antitoxin systems are ubiquitous and plasmid-encoded in Vancomycin-resistant enterococci. Proc Natl Acad Sci U S A. 2007;104:311–6.
Costa EM, Silva S, Vicente S, Veiga M, Tavaria F, Pintado MM. Chitosan as an effective inhibitor of multidrug resistant Acinetobacter baumannii. Carbohydr Polym. 2017;178:347–51.
Abd El-Hack ME, El-Saadony MT, Shafi ME, Zabermawi NM, Arif M, Batiha GE, et al. Antimicrobial and antioxidant properties of chitosan and its derivatives and their applications: a review. Int J Biol Macromol. 2020;164:2726–44.
Raafat D, Sahl HG. Chitosan and its antimicrobial potential–a critical literature survey. Microb Biotechnol. 2009;2(2):186–201.
Fu YY, Zhang L, Yang Y, Liu CW, He YN, Li P, et al. Synergistic antibacterial effect of ultrasound microbubbles combined with chitosan-modified polymyxin B-loaded liposomes on biofilm-producing Acinetobacter baumannii. Int J Nanomed. 2019;14:1805–15.
Hassan A, Ikram A, Raza A, Saeed S, Zafar Paracha R, Younas Z, et al. Therapeutic potential of Novel Mastoparan-Chitosan nanoconstructs against clinical MDR Acinetobacter baumannii: in silico, in vitro and in vivo studies. Int J Nanomed. 2021;16:3755–73.
Tiwari V, Tiwari M, Solanki V. Polyvinylpyrrolidone-capped silver nanoparticle inhibits infection of Carbapenem-resistant strain of Acinetobacter baumannii in the Human Pulmonary epithelial cell. Front Immunol. 2017;8:973.
Bazzi AM, Al-Tawfiq JA, Rabaan AA. Misinterpretation of Gram Stain from the stationary growth phase of positive blood cultures for Brucella and Acinetobacter species. Open Microbiol J. 2017;11:126–31.
Héritier C, Poirel L, Fournier PE, Claverie JM, Raoult D, Nordmann P. Characterization of the naturally occurring oxacillinase of Acinetobacter baumannii. Antimicrob Agents Chemother. 2005;49(10):4174–9.
Lewis IIJS. Performance standard for antimicrobial disk susceptibility testing. CLSI document M100 33rd Edition. Clinical and Laboratory Standards Institute (CLSI); 2022.
Goudarzi H, Douraghi M, Ghalavand Z, Goudarzi M. Assessment of antibiotic resistance pattern in Acinetobacter Bumannii carrying Bla oxA type genes isolated from hospitalized patients. Novelty Biomed. 2013;1(2):54–61.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–81.
El Maghraby HM, Mohammed HA. Detection of toxin-antitoxin system in Acinetobacter baumannii isolated from patients at Zagazig University Hospitals. Egypt J Med Microbiol. 2018;27(4):81–6.
Elnaggar YSR, Etman SM, Abdelmonsif DA, Abdallah OY. Intranasal Piperine-Loaded Chitosan nanoparticles as Brain-targeted therapy in Alzheimer’s Disease: optimization, Biological Efficacy, and potential toxicity. J Pharm Sci. 2015;104(10):3544–56.
Liu YH, Kuo SC, Yao BY, Fang ZS, Lee YT, Chang YC, et al. Colistin nanoparticle assembly by coacervate complexation with polyanionic peptides for treating drug-resistant gram-negative bacteria. Acta Biomater. 2018;82:133–42.
El-Refaie WM, Elnaggar YS, El-Massik MA, Abdallah OY. Novel curcumin-loaded gel-core hyaluosomes with promising burn-wound healing potential: development, in-vitro appraisal and in-vivo studies. Int J Pharm. 2015;486(1–2):88–98.
Elnaggar YS, Talaat SM, Bahey-El-Din M, Abdallah OY. Novel lecithin-integrated liquid crystalline nanogels for enhanced cutaneous targeting of terconazole: development, in vitro and in vivo studies. Int J Nanomed. 2016;11:5531–47.
Elragehy NA, Abdel-Moety EM, Hassan NY, Rezk MR. Stability-indicating determination of meropenem in presence of its degradation product. Talanta. 2008;77(1):28–36.
Charannya S, Duraivel D, Padminee K, Poorni S, Nishanthine C, Srinivasan MR. Comparative Evaluation of Antimicrobial Efficacy of Silver Nanoparticles and 2% chlorhexidine gluconate when used alone and in combination assessed using Agar Diffusion Method: an in vitro study. Contemp Clin Dent. 2018;9(Suppl 2):S204–9.
Magaldi S, Mata-Essayag S, Hartung de Capriles C, Perez C, Colella MT, Olaizola C, et al. Well diffusion for antifungal susceptibility testing. Int J Infect Dis. 2004;8(1):39–45.
Wintachai P, Surachat K, Chaimaha G, Septama AW, Smith DR. Isolation and characterization of a Phapecoctavirus Infecting Multidrug-Resistant Acinetobacter baumannii in A549 alveolar epithelial cells. Viruses. 2022;14(11):2561.
Smani Y, Domínguez-Herrera J, Pachón J. Rifampin protects human lung epithelial cells against cytotoxicity Induced by Clinical Multi and Pandrug-resistant Acinetobacter baumannii. J Infect Dis. 2011;203(8):1110–9.
Barati H, Fekrirad Z, Jalali Nadoushan M, Rasooli I. Anti-OmpA antibodies as potential inhibitors of Acinetobacter baumannii biofilm formation, adherence to, and proliferation in A549 human alveolar epithelial cells. Microb Pathog. 2024;186:106473.
Gaddy JA, Arivett BA, McConnell MJ, López-Rojas R, Pachón J, Actis LA. Role of acinetobactin-mediated Iron Acquisition functions in the Interaction of Acinetobacter baumannii strain ATCC 19606T with human lung epithelial cells, Galleria mellonella caterpillars, and mice. Infect Immun. 2012;80(3):1015–24.
Chen C-L, Dudek A, Liang Y-H, Janapatla RP, Lee H-Y, Hsu L, et al. d-mannose-sensitive pilus of Acinetobacter baumannii is linked to biofilm formation and adherence onto respiratory tract epithelial cells. J Microbiol Immunol Infect. 2022;55(1):69–79.
Babapour E, Haddadi A, Mirnejad R, Angaji S-A, Amirmozafari N. Biofilm formation in clinical isolates of nosocomial Acinetobacter baumannii and its relationship with multidrug resistance. Asian Pac J Trop Biomed. 2016;6(6):528–33.
Asif M, Alvi IA, Rehman SU. Insight into Acinetobacter baumannii: pathogenesis, global resistance, mechanisms of resistance, treatment options, and alternative modalities. Infect Drug Resist. 2018;11:1249–60.
Haque M, Sartelli M, McKimm J, Abu Bakar M. Health care-associated infections - an overview. Infect Drug Resist. 2018;11:2321–33.
Alkasaby NM, El Sayed Zaki M. Molecular study of Acinetobacter baumannii isolates for Metallo-β-Lactamases and extended-Spectrum-β-Lactamases genes in Intensive Care Unit, Mansoura University Hospital, Egypt. Int J Microbiol. 2017;2017:3925868.
Al Mobarak MF, Matbuli RM, Meir H, Al Gehani N, El Toukhy AAM, Al Qureshey KF, et al. Antimicrobial resistance patterns among Acinetobacter Baumannii isolated from King Abdulaziz Hospital, Jeddah, Saudi Arabia: four-year Surveillance Study (2010–2013). Egypt J Med Microbiol. 2014;38(3276):1–8.
Feizabadi MM, Fathollahzadeh B, Taherikalani M, Rasoolinejad M, Sadeghifard N, Aligholi M, et al. Antimicrobial susceptibility patterns and distribution of blaOXA genes among Acinetobacter Spp. Isolated from patients at Tehran hospitals. Jpn J Infect Dis. 2008;61(4):274–8.
Shoja S, Moosavian M, Peymani A, Tabatabaiefar MA, Rostami S, Ebrahimi N. Genotyping of carbapenem resistant Acinetobacter baumannii isolated from tracheal tube discharge of hospitalized patients in intensive care units, Ahvaz, Iran. Iran J Microbiol. 2013;5(4):315–22.
Karbasizade V, Heidari L, Jafari R. Detection of oxa-type carbapenemase genes in Acinetobacter baumannii isolates from nosocomial infections in Isfahan hospitals, Iran. J Med Bacteriol. 2015:31–6.
Fazeli H, Taraghian A, Kamali R, Poursina F, Nasr Esfahani B, Moghim S. Molecular Identification and Antimicrobial Resistance Profile of < em > Acinetobacter baumannii isolated from nosocomial infections of a Teaching Hospital in Isfahan, Iran. Avicenna J Clin Microbiol Infect. 2014;1(3):21489.
Karimi F, Amini K, javadi G. A phenotypic and genotypic study of Colistin Arn Resistance Regulator gene classes in Acinetobacter Baumannii isolated from clinical cases using Multiplex PCR. J Microb Biology. 2020;9(34):13–21.
Taherikalani M, Fatolahzadeh B, Emaneini M, Soroush S, Feizabadi MM. Distribution of different carbapenem resistant clones of Acinetobacter baumannii in Tehran hospitals. New Microbiol. 2009;32:265–71.
Sohrabi N, Farajnia S, Akhi MT, Nahaei MR, Naghili B, Peymani A, et al. Prevalence of OXA-type β-lactamases among Acinetobacter baumannii isolates from Northwest of Iran. Microb Drug Resist. 2012;18(4):385–9.
Karmostaji A, Peerayeh SN, Salmanian AH. Distribution of OXA-type class D β-lactamase genes among nosocomial multi drug resistant Acinetobacter baumannii isolated in Tehran hospitals. Jundishapur J Microbiol. 2013;6(5).
Savari M, Rostami S, Ekrami A, Bahador A. Characterization of toxin-antitoxin (TA) systems in Pseudomonas aeruginosa Clinical isolates in Iran. Jundishapur J Microbiol. 2016;9(1):e26627.
Hemati S, Azizi-Jalilian F, Pakzad I, Taherikalani M, Maleki A, Karimi S, et al. The correlation between the presence of quorum sensing, toxin-antitoxin system genes and MIC values with ability of biofilm formation in clinical isolates of Pseudomonas aeruginosa. Iran J Microbiol. 2014;6(3):133–9.
Mahboubi Kancha M, Mehrabi M, Bitaraf FS, Vahedi H, Alizadeh M, Bernkop-Schnürch A, Preparation. Characterization, and Anticancer Activity Assessment of Chitosan/TPP nanoparticles loaded with Echis carinatus Venom. Anticancer Agents Med Chem. 2024.
Mahboubi Kancha M, Alizadeh M, Mehrabi M. Comparison of the protective effects of CS/TPP and CS/HPMCP nanoparticles containing berberine in ethanol-induced hepatotoxicity in rat. BMC Complement Med Ther. 2024;24(1):39.
Elnaggar YS, Elwakil BH, Elshewemi SS, El-Naggar MY, Bekhit AA, Olama ZA. Novel Siwa propolis and colistin-integrated chitosan nanoparticles: elaboration; in vitro and in vivo appraisal. Nanomed (Lond). 2020.
Mufti IU, Gondal A, Kiyani KM, Mufti SM, Shahid R, Ihsan A, et al. Microstructural, physico-chemical, antibacterial and antibiofilm efficacy of imipenem loaded chitosan nano-carrier systems to eradicate multidrug resistant Acinetobacter baumannii. Mater Today Commun. 2023;35:105874.
Shaaban MI, Shaker MA, Mady FM. Imipenem/cilastatin encapsulated polymeric nanoparticles for destroying carbapenem-resistant bacterial isolates. J Nanobiotechnol. 2017;15(1):29.
Gui S, Li X, Feng M, Liu H, Huang L, Niu X. A fresh pH-responsive imipenem-loaded nanocarrier against Acinetobacter baumannii with a synergetic effect. Front Bioeng Biotechnol. 2023;11:1166790.
Safarzadeh Kozani P, Safarzadeh Kozani P, Malik MT. AS1411-functionalized delivery nanosystems for targeted cancer therapy. Explor Med. 2021;2:146–66.
Harugade A, Sherje AP, Pethe A, Chitosan. A review on properties, biological activities and recent progress in biomedical applications. Reactive Funct Polym. 2023;191:105634.
Safarzadeh Kozani P, Safarzadeh Kozani P, Hamidi M, Valentine Okoro O, Eskandani M, Jaymand M. Polysaccharide-based hydrogels: properties, advantages, challenges, and optimization methods for applications in regenerative medicine. Int J Polym Mater. 2022;71(17):1319–33.
Friedman AJ, Phan J, Schairer DO, Champer J, Qin M, Pirouz A, et al. Antimicrobial and anti-inflammatory activity of Chitosan–Alginate nanoparticles: a targeted therapy for cutaneous pathogens. J Invest Dermatology. 2013;133(5):1231–9.
Kim Y, Zharkinbekov Z, Raziyeva K, Tabyldiyeva L, Berikova K, Zhumagul D, et al. Chitosan-based biomaterials for tissue regeneration. Pharmaceutics. 2023;15(3):807.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
Marziyeh Sadat Amini: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualization, Writing - original draft. Majid Baseri Salehi: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Software, Supervision, Validation. Nima Bahador: Formal analysis, Methodology. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures were approved by and performed in accordance with the ethical standards of the Ethical Committee of the Islamic Azad University, Kazeroun Branch, Kazeroun, Iran and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Moreover, all experiments have been approved by the Ethical Committee of the Islamic Azad University, Kazerun Branch, Kazerun, Iran (approval ID: IR.IAU.KAU.REC.1399.105).
Consent for publication
Not applicable.
Informed consent
Informed consent was obtained from all individual participants (or their next of kin) involved in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Amini, M.S., Baseri Salehi, M. & Bahador, N. Evaluating the antibacterial effect of meropenem-loaded chitosan/sodium tripolyphosphate (TPP) nanoparticles on Acinetobacter baumannii isolated from hospitalized patients. BMC Infect Dis 24, 631 (2024). https://doi.org/10.1186/s12879-024-09522-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09522-7