Abstract
Background
Multidrug-resistant tuberculosis (MDR-TB) is a global health threat associated with high morbidity and mortality rates. Diagnosis and treatment delays are associated with poor treatment outcomes in patients with MDR-TB. However, the risk factors associated with these delays are not robustly investigated, particularly in high TB burden countries such as China. Therefore, this study aimed to measure the length of diagnosis and treatment delays and identify their risk factors among patients with MDR-TB in Hunan province.
Methods
A retrospective cohort study was conducted using MDR-TB data from Hunan province between 2013 and 2018. The main outcomes of the study were diagnosis and treatment delay, defined as more than 14 days from the date of symptom to diagnosis confirmation (i.e., diagnosis delay) and from diagnosis to treatment commencement (i.e., treatment delay). A multivariable logistic regression model was fitted, and an adjusted odds ratio (AOR) with a 95% confidence interval (CI) was used to identify factors associated with diagnosis and treatment delay.
Results
In total, 1,248 MDR-TB patients were included in this study. The median length of diagnosis delays was 27 days, and treatment delays were one day. The proportion of MDR-TB patients who experienced diagnosis and treatment delay was 62.82% (95% CI: 60.09–65.46) and 30.77% (95% CI: 28.27–33.39), respectively. The odds of experiencing MDR-TB diagnosis delay among patients coming through referral and tracing was reduced by 41% (AOR = 0.59, 95% CI: 0.45–0.76) relative to patients identified through consultations due to symptoms. The odds of experiencing diagnosis delay among ≥ 65 years were 65% (AOR = 0.35, 0.14–0.91) lower than under-15 children. The odds of developing treatment delay among foreign nationalities and people from other provinces were double (AOR = 2.00, 95% CI: 1.31–3.06) compared to the local populations. Similarly, the odds of experiencing treatment delay among severely ill patients were nearly 2.5 times higher (AOR = 2.49, 95% CI: 1.41–4.42) compared to patients who were not severely ill. On the other hand, previously treated TB cases had nearly 40% (AOR = 0.59, 95% CI: 0.42–0.85) lower odds of developing treatment delay compared with new MDR-TB cases. Similarly, other ethnic minority groups had nearly 40% (AOR = 0.57, 95% CI: 0.34–0.96) lower odds of experiencing treatment delay than the Han majority.
Conclusions
Many MDR-TB patients experience long diagnosis and treatment delays in Hunan province. Strengthening active case detection can significantly reduce diagnosis delays among MDR-TB patients. Moreover, giving attention to patients who are new to MDR-TB treatment, are severely ill, or are from areas outside Hunan province will potentially reduce the burden of treatment delay among MDR-TB patients.
Similar content being viewed by others
Background
Antimicrobial drug resistance is a human-made threat that results from either inadequate treatment, sub-optimal adherence to treatment regimens, or the persistence of resistant strains because of diagnosis or treatment delay [1]. Multidrug-resistant tuberculosis (MDR-TB), defined as tuberculosis (TB) resistant to at least isoniazid and rifampicin [2], is a major threat to global health [3]. MDR-TB is more difficult to diagnose and treat than drug-susceptible tuberculosis (DS-TB) and is associated with higher treatment costs, longer treatment durations, and poorer treatment outcomes [2]. Globally, nearly half a million people developed MDR-TB in 2021, with only 32% of these patients receiving treatment [2].
China has the second-highest MDR-TB burden, accounting for 14% of the global burden share [4]. China aims to achieve the World Health Organization (WHO) 2021 report END-TB strategy targets to reduce TB incidence by 90%, reduce TB mortality by 95%, and eliminate catastrophic costs in TB-affected households by 2035 [5]. China has implemented phenotypic and molecular diagnosis tests, including Gene-Xpert MTB/RIF, to minimize diagnosis delay, which may help achieve these targets. Moreover, China’s health system adopted the Directly Observed Treatment Short course approach to improve MDR-TB treatment success rates [6], but its implementation is poor [7].
Early diagnosis and initiation of MDR-TB treatment are crucial for achieving the global END-TB strategy targets by reducing MDR-TB infection and improving favourable treatment outcomes [8]. Delays in diagnosis and treatment of MDR-TB are associated with increased risk of morbidity [9], mortality, and community transmission, as well as increased treatment costs [10]. Recently, the introduction of the Gene-Xpert MTB/RIF Assay has improved the early detection of TB, MDR-, and extensively drug-resistant (XDR)-TB.
Studies among patients with DS-TB have reported that sociodemographic, behavioural, and clinical factors, including attitudes, knowledge, occupation, and educational status of patients, the presence of diabetes mellitus, and access to TB treatment centres, affect timely diagnosis and commencement of TB treatment [11]. However, the risk factors associated with diagnosis and treatment delays in patients with MDR-TB are yet to be robustly investigated, including in high-burden countries such as China. Understanding the factors that influence diagnosis and treatment delays will assist clinicians in identifying patients at higher risk of diagnosis and treatment delay, increasing the chance of timely diagnosis and treatment and good MDR-TB treatment outcomes, and reducing the chance of onward transmission. Therefore, this study aimed to evaluate diagnosis and treatment delays and risk factors for these delays among MDR-TB patients in Hunan province, China.
Methods
Study area
A retrospective cohort study was conducted in Hunan province, China. Hunan is one of the 34 provincial regions in China. It has an estimated total area of 211,800 square kilometres’ (81,800 square miles) and has just over 66 million inhabitants as of 2020. According to the census conducted in 2022, Hunan province has 41 ethnic groups. Of these, 89.79% identified as Han, and the remaining 10.21% as one of the minority groups, including Tujia, Miao, Dong, Yao, Bai, Hui, Zhuang, Uyghurs, and so on [12]. The proportion of TB cases that are MDR-TB in Hunan province ranges from 10.6% to 25.2%, which is significantly higher than the national average of 1.8% [13]. Hunan Chest Hospital is the only chest hospital in Changsha (the province’s capital) that provides diagnosis and treatment services for patients with MDR and Extensively Drug-resistant (XDR)-TB. The hospital commenced MDR- and XDR-TB care in 2011 and serves as a referral hospital for presumptive DR-TB patients.
Data sources and variables
The study population was all MDR-TB and XDR-TB patients enrolled at Hunan Chest Hospital between 2013 and 2018. Data were obtained from an internet-based TB management system administered by the TB Control Institute of Hunan province. All pulmonary or extrapulmonary MDR- and XDR-TB patients enrolled during the study period were included. The data contained demographic variables (age, gender, year of diagnosis, occupational status, residence, ethnicity, patient source, and detainee status) and clinical factors (initial date of symptoms, date of diagnosis, date of treatment commencement, registration type, diagnosis type, diagnosis institution type, and treatment delay).
Definition of variables
Multidrug-resistant tuberculosis (MDR-TB) is defined as a TB patient who is resistant to at least isoniazid and rifampicin. Extensively drug-resistant (XDR)-TB is defined as a TB patient resistant to isoniazid, rifampicin, fluoroquinolones, and either bedaquiline or linezolid (or both) [14]. We defined a total interval as the entire time required from the onset of symptoms to the start of MDR-TB treatment, which was divided into diagnosis and treatment intervals [15]. Diagnosis interval was defined as the time from the onset of symptoms to the date of MDR-TB confirmation [11]. Treatment delay was defined as the time from MDR-TB confirmation to commencement of MDR-TB treatment [16]. Severely ill was defined as a patient with severe comorbidities, having persistent coughing with breathlessness and weakness with extreme weight loss. Hunan ethnic classification recognizes 55 minority groups, including the Han majority.
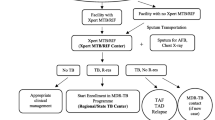
MDR- TB diagnosis in Hunan province
Hunan Chest Hospital follows WHO-recommended methods for the diagnosis and treatment of MDR-TB. Clinical assessments based on symptoms, microscopic sputum examinations, radiological examinations, and molecular techniques such as Line Probe Assay and Gene Xpert are commonly used to diagnose MDR-TB in the province.
There are 131 counties in Hunan province, and only 32 counties can provide comprehensive diagnosis services, including culture. In Hunan Chest Hospital, drug susceptibility testing (DST) is mainly carried out to diagnose MDR-TB. As a result, sputum specimens from all culture-positive TB patients from all parts of the province are referred to the Hunan Chest Hospital for DST. In the hospital, phenotypic DST based on solid and liquid culture techniques and molecular methods using line probe assays and Xpert® MTB/RIF are performed. The Hunan Chest Hospital performs DST for rifampicin, isoniazid, ethambutol, streptomycin, kanamycin, and ofloxacin. Solid and liquid cultures are used to follow up on patients’ progress and treatment outcomes.
Data analysis
Data in an Excel spreadsheet was translated from Mandarin to English and exported to Stata version 17 software for analysis. Descriptive statistics were conducted and presented as frequencies (percentages) for categorical variables and medians with interquartile ranges (IQR) for continuous variables. The outcome variables (diagnosis and treatment intervals) were calculated in days and categorized as delayed and non-delayed. The number of days between the onset of symptoms and diagnosis confirmation and between diagnosis and commencement of MDR-TB treatment were calculated. A 14-day cut-off point was used to dichotomize diagnosis and treatment delay to be consistent with a previous study (https://www.health.nsw.gov.au/Infectious/controlguideline/Pages/tuberculosis.aspx).
We used chi-square tests to assess associations between outcome and explanatory variables. A univariable logistic regression model was first fitted, and variables with a p-value of < 0.2 were entered into a multivariable logistic regression model. An adjusted odds ratio (DST) with a 95% CI was used to determine the statistical significance and strength of associations between risk factors and delays in diagnosis and treatment initiation. As there is no cut-off point to classify delay, sensitivity analysis was conducted using a median value to determine the threshold for delay. We also run two separate analyses based on the type of treatment category (new versus retreatment). A sensitivity analysis was also conducted using a negative binomial regression model, whereby the outcomes were taken as counts. Hosmer–Lemeshow’s goodness of fit test was used to assess model fitness. As the mean and the variance were not equal, the negative binomial model was used over the Poisson regression model for the count data analysis. An adjustive relative risk (ARR) with a corresponding 95% CI was used to declare statistical significance.
Results
In this study, 1,248 MDR-TB patients were included. The mean age of respondents was 43 years, with an SD of 12 years. The majority were male (73.9%), farmers (79.3%), Han ethnicity (92.0%), and new treatment patients (83.1%) (Table 1).
Median time to diagnosis and treatment interval among multidrug-resistant tuberculosis patients
Overall, the median diagnosis interval among MDR-TB patients was 27 days (IQR 7–66 days), and the median treatment interval was one day (IQR 0–24 days) (Table 2). The overall prevalence of diagnosis delay among MDR-TB patients was 62.8% (95% CI: 60.1–65.4), and 30.8% (95% CI: 28.3–33.4) of MDR-TB patients experienced treatment delay. The diagnosis and treatment delay distribution are summarized in Supplementary files, Figs. S1 and S2.
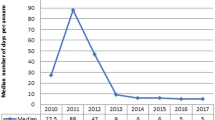
The trend in diagnosis and treatment delay among MDR-TB patients
Diagnosis delay among MDR-TB patients increased yearly but not linearly. On the other hand, the treatment delay increased over 2013 and 2015. Then, the trend was steady from 2015 to 2016 and showed a slight reduction between 2016 and 2017. The trend of treatment delay increased alarmingly over a period of 2017 and 2018 (Fig. 1).
Factors affecting diagnosis delay among patients treated for MDR-TB
The odds of experiencing MDR-TB diagnosis delay among patients who came through referral and tracing was 41% lower (AOR = 0.61, 95% CI: 0.47–0.80) relative to patients identified through consultations due to symptoms. Compared to patients younger than 15 years, patients aged ≥ 65 years had 65% lower odds of experiencing diagnosis delay (AOR = 0.35, 95% CI: 0.14–0.91) (Table 3).
In sensitivity analysis (i.e., using the median 27 days as a cut-off point instead of 14 days), age, occupation of respondents, and patient source of diagnosis were statistically significant factors associated with treatment delay, suggesting the results are sensitive to the selection of the threshold defining a delay. The odds of experiencing diagnosis delay among elderly MDR-TB patients (≥ 65 years) was 60% lower (AOR = 0.40, 0.17–0.94) than among children under 15 years old. The odds of developing diagnosis delay among MDR-TB patients identified through referral and tracing was 25% lower (AOR = 0.75, 0.59–0.96) compared with MDR-TB patients who came to seek consultations due to having had symptoms (Supplementary file Table S1).
No significant variables were identified in the sensitivity analysis that stratified MDR-TB patients as new or previously treated (Supplementary file Table S2).
Supplementary file Table S3 shows the negative binomial regression assessment of factors affecting diagnosis delay among MDR-TB patients. The finding showed that gender, diagnosis institution type, age, and treatment category were significantly associated with diagnosis delay.
Factors affecting treatment delay among patients treated for MDR-TB
Current residence, treatment category, ethnicity, and severity of illness were associated with treatment delay. The odds of developing treatment delay among foreign nationalities and people from other provinces were almost double (AOR = 1.99, 95% CI: 1.30–3.04) compared to the local populations. The odds of experiencing treatment delay among severely ill patients were 2.58 times higher (AOR = 2.58, 95% CI: 1.46–4.58) than patients who were not severely ill. Previously treated TB cases had 41% lower odds (AOR = 0.59, 95% CI: 0.42–0.85) of treatment delay than new MDR-TB cases. Similarly, other ethnic minority groups had 67% lower odds (AOR = 0.55, 95% CI: 0.33–0.93) of experiencing treatment delay than the Han majority (Table 4).
A sensitivity analysis was conducted using different thresholds defining a delay, and sensitivity to this threshold was identified. A sensitivity analysis using the third quartile (24 days) showed that only two variables (ethnicity and patient source) remained significant; the odds of experiencing treatment delay among ethnic minority MDR-TB patients were 62% lower (AOR = 0.38, 95% CI: 0.19–0.74) compared to the Han majority. The odds of experiencing treatment delay among patients identified through referral and tracing was 7.39 (4.75–11.49) times higher than patients who came to seek consultations (Supplementary file Table S4).
In a sensitivity analysis based on treatment category (new vs re-treatment), other occupations had 38% higher odds (AOR = 1.38, 95% CI: 1.01–1.90) of experiencing treatment delay than farmers (Supplementary file Table S5).
Findings from the negative binomial model showed that patient source was significantly associated with the risk of treatment delay (Supplementary file Table S6).
Discussion
This study evaluated risk factors of diagnosis and treatment delay among MDR-TB patients in Hunan province. About 2/3 and 1/3 MDR-TB patients experienced diagnosis and treatment delays, respectively, using a 14-day threshold to define a delay. The median diagnosis and treatment intervals among MDR-TB patients were 27 and one day, respectively. Elderly patients (≥ 65 years) and patients identified through tracing and referral had lower odds of diagnosis delay than their counterparts. Patients with Han ethnicity, previous TB treatment history, residence outside Hunan province, and who were severely ill had a significantly higher probability of experiencing MDR-TB treatment delay.
Diagnosis and treatment interval for MDR-TB
The median diagnosis interval found in this study was longer than the nine days reported in Myanmar [17] and five days in Bangladesh [18]. The difference could result from using different diagnosis modalities and algorithms to diagnose MDR-TB. On the other hand, the interval was shorter than previously reported in China, with a median diagnosis of 84 days [19]. The difference could be because of the introduction of Gene-Expert, which reduced laboratory result turnaround time in diagnosing MDR-TB patients [20]. Previous studies also showed that using GeneXpert had significantly reduced treatment delay among DR-TB patients [21, 22]. The study also revealed that 2/3 of MDR-TB patients developed diagnosis delays. However, our finding was higher than the WHO recommendations that every patient should have an early diagnosis of TB, including universal Drug Susceptibility Testing (DST) [2]. The WHO recommends that all DR-TB patients need to commence their treatment as soon as possible to prevent unnecessary side effects, complications, and poor treatment outcomes.
The trend of treatment delay increased alarmingly over a period of 2017 and 2018. A possible justification could be the high case burden of MDR-TB in Hunan province between 2017 and 2018, and patients may be obliged to wait longer to commence their treatment. Moreover, study subjects’ variation in terms of MDR-TB signs and symptoms and poor health-seeking behaviour may contribute to the difference. Also, previous studies suggested that the initiation of MDR-TB treatment mainly depends on baseline laboratory investigations and PMDT panel team decisions on DST test results and availability of treatment options [23, 24]. So, the alarming treatment delay in 2017/2018 could be due to the lack of treatment options. However, further research is needed to point out possible factors contributing to the high burden of treatment delay in 2017 and 2018.
Many MDR-TB patients experienced treatment delays in Hunan province, and it is highly recommended that the initiation of prompt MDR-TB treatment following confirmatory diagnosis is prioritized to achieve the END-TB strategy targets. Early diagnosis and treatment of TB is particularly important to minimize community transmission of the disease, reduce side effects, and improve disease progression treatment outcomes and quality of life of the patients. It can also help minimize the patients’ catastrophic costs [25].
There are few studies previously conducted in China to determine MDR-TB diagnosis and treatment delay. Our study is the first to investigate MDR-TB diagnosis and treatment delays, focusing on Hunan Province (one of the provinces with high MDR-TB burden in China). Our study has incorporated important variables such as ethnic minority and residence that have been missed in the previous studies. The first study conducted in Taizhou, Zhejiang Province, showed that the overall diagnosis and treatment delay was not illustrated. Instead, it primarily determines factors associated with waiting time for DST, pre-attrition, time of waiting for treatment, and treatment outcomes and associated factors. Moreover, it did not report the overall diagnosis delay and associated risk factors. On the other hand, a study conducted in China to determined diagnosis and treatment delay among MDR-TB patients lacked socio-demographic variables such as ethnicity and residence [26]. However, in our study, ethnic minorities and residents outside Hunan Province were identified as risk factors for diagnosis and treatment delay. This will add a piece of literature to the existing knowledge. Moreover, none of the studies conducted a sensitivity analysis, which is valuable for better decision-making and more reliable predictions and highlights areas for improvement. As there is no cut-off point to decide diagnosis and treatment delay, applying a sensitivity analysis to show the result at different points is significant.
Risk factors of MDR-TB diagnosis delay
Previous studies suggested that elderly patients often struggle to access diagnosis and treatment centres and usually rely on their families to visit health facilities [27]. However, our findings showed that patients ≥ 65 years of age had lower odds of diagnosis delay than patients aged < 15 years. A possible explanation could be that MDR-TB diagnosis in children is impacted by different diagnostic approaches; for example, children may be treated for other respiratory tract infections before diagnosis testing is undertaken, resulting in delayed MDR-TB diagnosis. A previous study revealed that the diagnosis of MDR-TB is bacteriological, and children need a systematic diagnosis approach that leads to a longer time to diagnosis of MDR-TB [28]. Moreover, a lack of awareness that children develop MDR-TB, a perceived inability to diagnose active MDR-TB without TST and CXR, and no international guidance on preventive therapy against MDR-TB could contribute to MDR-TB diagnosis delay in children aged < 15 years [29]. Therefore, improving diagnosis protocols in children could minimize diagnosis delay among MDR-TB patients.
In this study, patients identified through tracing and referral had a lower diagnosis delay than patients identified through symptomatic consultations. Moreover, tracing MDR-TB patients might have a significant contribution to MDR-TB patients visiting the health facility timely due to possible consultation, which is a basic component of support and overcoming major barriers that lead to not disclosing the disease due to the high nature of MDR-TB stigmatization. Also, referral reduces waiting times for primary care and minimizes double investigation as they can rely on their pre-referral work-up. The shorter delay among tracing and referral sub-groups may also be caused by the bias of symptom onset time.
Moreover, our findings agree with previous studies carried out on DS-TB patients. For instance, age and active case findings [30] were significantly associated with diagnosis delay among DS-TB patients. Moreover, other sociodemographic variables (educational status, knowledge of MDR-TB, and personal beliefs and attitudes) [31], using traditional medicines and healers, and limited health service access due to geographical location [32] were significantly associated with diagnosis delay among DS-TB patients.
Risk factors of MDR-TB treatment delay
Regarding treatment delay, Han ethnicity, patients with previous TB treatment history, residence other than Hunan province, and becoming severely ill were significantly associated with MDR-TB treatment delay. This study found that ethnic minority groups in Hunan province had lower odds of experiencing treatment delay than the Han majority. This could be due to improving educational attainment among ethnic minorities, which is highly prioritized in China [33]. This finding is consistent with a study conducted by Gilmour et al. among DS-TB patients in Hunan province; ethnic minority groups had lower odds of experiencing treatment delay than the Han majority. A systematic review and meta-analysis conducted among DS-TB patients in Ethiopia showed that lower educational level was significantly associated with poor health-seeking behaviour [34]. However, further research is recommended to illuminate why the Han majority groups are at higher odds of experiencing treatment delay than ethnic minority groups.
In this study, previously treated MDR-TB cases had lower odds of experiencing MDR-TB treatment delay. This might be because previously treated cases were more knowledgeable about what to do and aware of the severity of the disease and the risk of developing a resistant form of TB, and they already had relationships with clinicians that expedited their care; they were also less likely to experience diagnosis delay than new MDR-TB patients [34, 35].
Patients from locations other than Hunan province had an increased likelihood of experiencing treatment delay. In China, the hukou system, a household registration system, permits a permanent resident for a single address issued by the government of China to each family member given at birth or by employment in formal sectors [36]. The hukou system allows each family member access to essential public services, education, health services, social benefits, and job recruitment by the governmental or private sectors [37]. As a result, patients from Hunan province will have better access to health care and are less likely to experience treatment delays than patients from outside Hunan province. According to previous reports, a previous history of DS-TB treatment [38] and health system factors (staff shortages, cost of services, drug stockout, and poor health infrastructure) [11] are significantly associated with treatment delay.
Limitations of the study
The study had several limitations. The absence of a WHO-endorsed, international standard cut-off point to determine diagnosis and treatment delay can significantly impact estimates of the burden of delays and cause misclassification bias when investigating factors associated with the delays. Some important variables that might be associated with diagnosis and treatment delay, such as education status, income level, geographical inaccessibility, knowledge of MDR-TB, and presence of comorbidities (e.g., diabetes mellitus, HIV infection, mental ill health), were not assessed in the current study. Future research should prioritize undertaking prospective studies that measure these variables. Only patients attending the designated health facilities were included in the study. This might have caused selection bias, and findings might not be generalizable to all MDR-TB patients in Hunan province. Recall bias might also have been an issue for patients specifying the exact date of symptom onset. Finally, all sputum specimens were transported to Hunan Chest Hospital for DST might introduce turnaround time that will further influence on the diagnosis delay.
Conclusion
Long diagnosis and treatment delays still occur for many MDR-TB patients in Hunan province. Under-15 children and patients identified through passive case detection were found to experience a higher probability of diagnosis delay. Ethnic minority groups and patients who were previously treated for MDR-TB had lower odds of treatment delay. On the other hand, the odds of treatment delay in patients coming from areas other than the Hunan province and severely ill patients were high. Giving attention to new MDR-TB patients, severely ill patients and patients from outside Hunan province will potentially reduce the burden of treatment delay among MDR-TB patients.
Availability of data and materials
Data will be available upon request from the corresponding author.
Abbreviations
- AOR:
-
Adjusted Odds Ratio
- ARR:
-
Adjusted Relative Risk
- CI:
-
Confidence Interval
- DST:
-
Drug Susceptibility Testing
- DS-TB:
-
Drug Susceptible Tuberculosis
- HIV:
-
Human Immune Deficiency Virus
- IQR:
-
Inter Quartile Range
- MDR-TB:
-
Multidrug Resistant Tuberculosis
- TB:
-
Tuberculosis
- WHO:
-
World Health Organization
- XDR-TB:
-
Extensively Drug Resistant Tuberculosis
References
Yew WW. Management of multidrug-resistant tuberculosis and extensively drug-resistant tuberculosis: current status and future prospects. Kekkaku. 2011;86(1):9–16.
WHO. Global tuberculosis report 2021. 2021.
Gandhi NR, Nunn P, Dheda K, Schaaf HS, Zignol M, Van Soolingen D, et al. Multidrug-resistant and extensively drug-resistant tuberculosis: a threat to global control of tuberculosis. Lancet. 2010;375(9728):1830–43.
Sicular T, Ximing Y, Gustafsson B, Shi L. The urban–rural income gap and inequality in China. Rev Income Wealth. 2007;53(1):93–126.
Chakaya J, Petersen E, Nantanda R, Mungai BN, Migliori GB, Amanullah F, et al. The WHO global tuberculosis 2021 report – not so good news and turning the tide back to end TB. Int J Infect Dis. 2022;124:S26–9.
Loddenkemper R, Sagebiel D, Brendel A. Strategies against multidrug-resistant tuberculosis. Eur Respir J Suppl. 2002;36:66s–77s.
Hou W, Song F, Zhang N, Dong X, Cao S, Yin X, et al. Implementation and community involvement in DOTS strategy: a systematic review of studies in China. Int J Tuberc Lung Dis. 2012;16(11):1433–40.
Liang L, Wu Q, Gao L, Hao Y, Liu C, Xie Y, et al. Factors contributing to the high prevalence of multidrug-resistant tuberculosis: a study from China. Thorax. 2012;67(7):632–8.
Van Cutsem G, Isaakidis P, Farley J, Nardell E, Volchenkov G, Cox H. Infection control for drug-resistant tuberculosis: early diagnosis and treatment is the key. Clin Infect Dis. 2016;62(suppl_3):S238–43.
Evans D, Sineke T, Schnippel K, Berhanu R, Govathson C, Black A, et al. Impact of Xpert MTB/RIF and decentralized care on linkage to care and drug-resistant tuberculosis treatment outcomes in Johannesburg, South Africa. BMC Health Serv Res. 2018;18(1):973.
Htun YM, Khaing TMM, Yin Y, Myint Z, Aung ST, Hlaing TM, et al. Delay in diagnosis and treatment among adult multidrug resistant tuberculosis patients in Yangon Regional Tuberculosis Center, Myanmar: a cross-sectional study. BMC Health Serv Res. 2018;18(1):1–13.
https://en.wikipedia.org/wiki/Hunan. Accessed 22 Dec 2022.
Liu Q, Yang D, Xu W, Wang J, Lv B, Shao Y, et al. Molecular typing of Mycobacterium tuberculosis isolates circulating in Jiangsu province. China. BMC Infect Dis. 2011;11(1):1–10.
Roelens M, Battista Migliori G, Rozanova L, Estill J, Campbell JR, Cegielski JP, et al. Evidence-based definition for extensively drug-resistant tuberculosis. Am J Respir Crit Care Med. 2021;204(6):713–22.
Diagnostics FfIN, Research SPf, Diseases TiT, Organization WH. Diagnostics for tuberculosis: global demand and market potential. World Health Organization. 2006.
Organization WH. Multidrug-resistant tuberculosis (MDR-TB) indicators: a minimum set of indicators for the programmatic management of MDR-TB in national tuberculosis control programmes. World Health Organization; 2010.
Htun YM, Khaing TMM, Yin Y, Myint Z, Aung ST, Hlaing TM, et al. Delay in diagnosis and treatment among adult multidrug resistant tuberculosis patients in Yangon Regional Tuberculosis Center, Myanmar: a cross-sectional study. BMC Health Serv Res. 2018;18(1):878.
Rifat M, Hall J, Oldmeadow C, Husain A, Milton AH. Health system delay in treatment of multidrug resistant tuberculosis patients in Bangladesh. BMC Infect Dis. 2015;15(1):1–8.
Xu C, Li R, Shewade HD, Jeyashree K, Ruan Y, Zhang C, et al. Attrition and delays before treatment initiation among patients with MDR-TB in China (2006–13): magnitude and risk factors. PLoS One. 2019;14(4):e0214943.
Cox HS, Daniels JF, Muller O, Nicol MP, Cox V, van Cutsem G, et al. Impact of decentralized care and the Xpert MTB/RIF test on rifampicin-resistant tuberculosis treatment initiation in Khayelitsha, South Africa. Open Forum Infect Dis. 2015;26:ofv014. Oxford University Press.
Tamirat KS, Kebede FB, Baraki AG, Akalu TY. The role of GeneXpert MTB/RIF in reducing treatment delay among multidrug resistance tuberculosis patients: a propensity score matched analysis. Infect Drug Resist. 2022;15:285–94.
Dlamini-Mvelase NR, Werner L, Phili R, Cele LP, Mlisana KP. Effects of introducing Xpert MTB/RIF test on multi-drug resistant tuberculosis diagnosis in KwaZulu-Natal South Africa. BMC Infect Dis. 2014;14:442.
Naidoo P, Du Toit E, Dunbar R, Lombard C, Caldwell J, Detjen A, et al. A comparison of multidrug-resistant tuberculosis treatment commencement times in MDRTBPlus line probe assay and Xpert® MTB/RIF-based algorithms in a routine operational setting in Cape Town. PLoS One. 2014;9(7):e103328.
Hoa NB, Khanh PH, Chinh NV, Hennig CM. Prescription patterns and treatment outcomes of MDR-TB patients treated within and outside the N ational T uberculosis P rogramme in P ham N goc T hach hospital, V iet N am. Trop Med Int Health. 2014;19(9):1076–81.
Yagui M, Perales M, Asencios L, Vergara L, Suarez C, Yale G, et al. Timely diagnosis of MDR-TB under program conditions: is rapid drug susceptibility testing sufficient? Int J Tuberc Lung Dis. 2006;10(8):838–43.
Xu CA-O, Li R, Shewade HA-O, Jeyashree K, Ruan Y, Zhang CA-O, et al. Attrition and delays before treatment initiation among patients with MDR-TB in China (2006–13): magnitude and risk factors. PLoS One. 2019;14:943. 1932-6203 (Electronic).
Negin J, Abimbola S, Marais BJ. Tuberculosis among older adults – time to take notice. Int J Infect Dis. 2015;32:135–7.
Seddon JA, Johnson S, Palmer M, van der Zalm MM, Lopez-Varela E, Hughes J, et al. Multidrug-resistant tuberculosis in children and adolescents: current strategies for prevention and treatment. Expert Rev Respir Med. 2021;15(2):221–37.
Outhred AC, Britton PN, Marais BJ. Drug-resistant tuberculosis–primary transmission and management. J Infect. 2017;74:S128–35.
Sebastian N, Haveri SP, Nath AS. Delay in diagnosis of tuberculosis and related factors from a district in Kerala, India. Indian J Tuberc. 2021;68(1):59–64.
Das D, Dwibedi B. Delay in diagnosis among pulmonary tuberculosis patients of Rayagada District, Odisha, India. Int J Mycobacteriol. 2016;5(Suppl 1):S172–3.
Ngangro NN, Chauvin P, Des Fontaines VH. Determinants of tuberculosis diagnosis delay in limited resources countries. Epidemiol Public Health. 2012;60(1):47–57.
Yang R, Wu M. Education for ethnic minorities in China: a policy critique. SA-eDUC J. 2009;6(2):117–31.
Obsa MS, Daga WB, Wosene NG, Gebremedhin TD, Edosa DC, Dedecho AT, et al. Treatment seeking delay and associated factors among tuberculosis patients attending health facility in Ethiopia from 2000 to 2020: a systematic review and meta analysis. PLoS One. 2021;16(7):e0253746.
Xu X, Liu J, Cao S, Zhao Y, Dong X, Liang Y, et al. Delays in care seeking, diagnosis and treatment among pulmonary tuberculosis patients in Shenzhen, China. Int J Tuberc Lung Dis. 2013;17(5):615–20.
Song Q, Smith JP. Hukou system, mechanisms, and health stratification across the life course in rural and urban China. Health Place. 2019;58:102150.
Kuang L, Liu L. Discrimination against rural-to-urban migrants: the role of the Hukou system in China. PLoS One. 2012;7(11):e46932.
Paul D, Busireddy A, Nagaraja SB, Satyanarayana S, Dewan PK, Nair SA, et al. Factors associated with delays in treatment initiation after tuberculosis diagnosis in two districts of India. PLoS One. 2012;7(7):e39040.
Acknowledgements
This work was supported by the Australian National Health and Medical Research Council (NHMRC) through an Emerging Leadership Investigator Grant APP1196549. KAA is a senior researcher at Curtin University who received the fund. TYA is also supported by the Curtin University HDR Scholarship and acknowledges Curtin University for providing support.
Funding
The National Health and Medical Research Council funds KAA, and the Curtin University Higher Degree Research (HDR) Scholarship also supports TYA. The funders had no role in the study design, publication decision, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
TYA, ACAC, and KAA conceptualised the study. TYA, ACAC, EAG, ZX, LB, and KAA performed data curation. TYA and KAA carried out the statistical analysis and accessed and verified the data. TYA wrote the first draft of the manuscript with input from ACAC, EAG, and KAA. All authors reviewed the final draft of the manuscript for intellectual content. All authors had full access to the data and decision to submit for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Curtin University Human Research Ethics Committee obtained ethical approval, and the Hunan TB Control Institute provided written informed consent for all study subjects. Due to the retrospective nature of the data, it is not practicable to obtain consent directly from study subjects. As a result, the informed consent was waived by the ethics committee of Hunan research ethics. Medical records of study subjects were de-identified and password-protected to maintain patient confidentiality. The study was conducted according to the Declaration of Helsinki.
Consent for publication
Not required.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary file Fig S1.
The distribution of diagnosis delay among multidrug-resistant tuberculosis stratified by number of days in Hunan Province. Supplementary file Fig S2. The distribution of treatment delay among multidrug-resistant tuberculosis stratified by the number of days. Supplementary file Table S1. A sensitivity analysis: Univariable and multivariable logistic regression for diagnosis delay among multidrug-resistant tuberculosis patients in Hunan Province, 2013-2018 (Using median as a cut-off point). Supplementary file Table S2. A sensitivity analysis: Univariable and multivariable logistic regression for diagnosis delay stratified by treatment category among multidrug-resistant tuberculosis patients in Hunan Province, 2013-2018. Supplementary file Table S3. A sensitivity analysis: Univariable and multivariable negative binomial regression assessment of factors associated with time from symptoms to diagnosis in multidrug-resistant tuberculosis patients registered in Hunan Province, 2013-2018. Supplementary file Table S4. A sensitivity analysis: Univariable and multivariable logistic regression for treatment delay among multidrug-resistant tuberculosis patients in Hunan Province, 2013-2018 (Using the upper quartile as a cut-off point). Supplementary file Table S5. A sensitivity analysis: Univariable and multivariable logistic regression for treatment delay stratified by treatment category among multidrug-resistant tuberculosis patients in Hunan Province, 2013-2018. Supplementary file Table S6. A sensitivity analysis: Univariable and multivariable negative binomial regression assessment of factors associated with time from diagnosis to treatment commencement in multidrug-resistant tuberculosis patients registered in Hunan Province, 2013-2018.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Akalu, T.Y., Clements, A.C.A., Gebreyohannes, E.A. et al. Risk factors for diagnosis and treatment delay among patients with multidrug-resistant tuberculosis in Hunan Province, China. BMC Infect Dis 24, 159 (2024). https://doi.org/10.1186/s12879-024-09036-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09036-2