Abstract
Background
It is unclear whether Saccharomyces boulardii (S. boulardii) supplementation in standard triple therapy (STT) is effective in eradicating Helicobacter pylori (H. pylori) infection in children. We therefore conducted a meta-analysis of randomized controlled trials (RCTs) to assess the effect of S. boulardii supplementation on H. pylori eradication in children.
Methods
We conducted electronic searches in PubMed, Embase, the Cochrane Library, China National Knowledge Infrastructure and Wanfang database from the beginning up to September 2023. A random-effects model was employed to calculate the pooled relative risk (RR) with 95% confidence intervals (CI) through a meta-analysis.
Results
Fifteen RCTs (involving 2156 patients) were included in our meta-analysis. Results of the meta-analysis indicated that S. boulardii in combination with STT was more effective than STT alone (intention-to-treat analysis : 87.7% vs. 75.9%, RR = 1.14, 95% CI: 1.10–1.19, P < 0.00001; per-protocol analysis : 88.5% vs. 76.3%, RR = 1.15, 95% CI: 1.10–1.19, P < 0.00001). The S. boulardii supplementation group had a significantly lower incidence of total adverse events (n = 6 RCTs, 9.2% vs. 29.2%, RR = 0.32, 95% CI: 0.21–0.48, P < 0.00001), diarrhea (n = 13 RCTs, 14.7% vs. 32.4%, RR = 0.46, 95% CI: 0.37–0.56, P < 0.00001), and nausea (n = 11 RCTs, 12.7% vs. 21.3%, RR = 0.53, 95% CI: 0.40–0.72, P < 0.0001) than STT group alone. Similar results were also observed in the incidence of vomiting, constipation, abdominal pain, abdominal distention, epigastric discomfort, poor appetite and stomatitis.
Conclusions
Current evidence indicated that S. boulardii supplementing with STT could improve the eradication rate of H. pylori, and concurrently decrease the incidence of total adverse events and gastrointestinal adverse events in children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Helicobacter pylori (H. pylori), a microaerobic gram-negative bacterium that colonizes the gastric mucosa, is a very common infection across the world and is a significant public health problem [1]. According to the latest meta-analysis study, the rate of H. pylori infection in developing countries was found to be 50.8%, 34.7% in developed countries, and 32.6% for children worldwide [2]. H. pylori is usually contracted in early childhood and, if not addressed, can remain for a long time [3]. It is generally believed that H.pylori infection is the primary cause of chronic gastritis, peptic ulcers, and gastric malignancies [3, 4]. Additionally, recent studies have indicated a possible correlation between H.pylori infection and some extra-gastroduodenal diseases (cardiovascular diseases, metabolic disorders, diabetes mellitus, neurodegenerative diseases, and skin diseases) [4]. Eliminating H.pylori is the most effective way to prevent and treat illnesses associated with H.pylori.
The standard triple therapy (STT) based on a proton pump inhibitor (PPI) combined with two antibiotics (amoxicillin and clarithromycin or metronidazole) was the first-line regimen for H. pylori eradication in children in several recent guidelines and expert consensus for eradicating H. pylori [5,6,7]. However, due to the increasing resistance rate of antibiotics (mainly clarithromycin), the eradication rate has decreased. Additionally, the adverse events of antibiotics during the eradication process can lead to poor compliance [1, 8,9,10]. Therefore, new effective therapies are needed to eradicate H. pylori. Scientists have started to explore other alternative and complementary treatments to tackle these issues.
Over the past few years, probiotics have been extensively utilized in clinical practice, providing a novel approach for eradicating H. pylori [8,9,10]. Probiotics, live microorganisms that can be advantageous to one’s wellbeing when taken in the right amount, are a type of beneficial microorganism [11]. Saccharomyces boulardii (S. boulardii) is the only fungal probiotic preparation that is being employed around the world. Previously, Zhou et al. [12] conducted a meta-analysis to explore the effect of S. boulardii in combination with standard eradication therapy (triple therapy, quadruple therapy and sequential therapy) on H. pylori eradication. Nevertheless, the previous meta-analysis mainly concentrated on adults, with only three studies on children having small sample sizes. What is more, recent several guidelines and expert consensus on H. pylori eradication in children have highlighted the absence of adequate clinical evidence to back up the regular inclusion of probiotics during H. pylori eradication therapy [5,6,7]. There has yet to be a definitive conclusion concerning the effectiveness of using S. boulardii to treat H. pylori infection. Hence, we conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) to evaluate the effect of S. boulardii supplementing with STT on H. pylori eradication in children and provide evidence-based medical evidence for clinical decision-making.
Methods
This study has been pre-registered in PROSPERO, which is an International Prospective Register of Systematic Reviews and Meta-Analyses (registration number. CRD42023462632). This systematic review followed the PRISMA 2020 statement for Systematic Reviews and Meta-Analysis [13].
Literature search strategy
We conducted electronic searches in PubMed, Embase, the Cochrane Library, China National Knowledge Infrastructure (CNKI) and Wanfang database using pre-determined search terms from the beginning up to September 10, 2023.The terms used for the search were: helicobacter, “helicobacter pylori”, “campylobacter pylori”, “H.pylori”, “Hp”, “saccharomyces boulardii”, “S. boulardii”, “bioflor”, probiotics, probiotic, “children”, “childhood”, “pediatric”, “pediatrics”, “adolescents”. For details on search terms and strategies used in PubMed, please refer to the online Supplementary Table S1. We employed MeSH headings and text word terms searching without any language limitations. Furthermore, we scanned the reference lists of evaluated studies to find additional suitable studies.
Study selection criteria
The following criteria were used to determine which studies were eligible: (1) Study design: RCTs; (2) Participants: Participants in the study were first-time treatment patients with H.pylori infection (aged < 18 years old), which was determined through urea breath test (UBT), rapid urease test (RUT), histology, stool antigen test (SAT), or culture, with one positive result at least; (3) Intervention group (S. boulardii supplementation group): S. boulardii in combination with STT; (4) Control group (STT group): the same STT as intervention group (with or without placebo); (5) Outcome: (i) primary outcome: H.pylori eradication rate (after ceasing medication for at least 4 weeks, re-examination using established H.pylori testing methods, and a negative result for H.pylori eradication); (ii) secondary outcomes: the incidence of adverse events (including the total and specific adverse events). Studies involving other probiotics, adults, repeated published research, non-RCTs, conference abstracts, letters, animal experiments, meta-analyses, reviews, and studies where data or full text cannot be obtained will be excluded. After reviewing titles, abstracts and full texts of the obtained literatures, two researchers (Liu LH and Tao J) independently excluded any studies that did not meet the inclusion criteria. In case of any disagreement, consensus was reached through discussion or with the help of a third researcher.
Data extraction
Two researchers (Zhang K and Wang WK) were delegated to independently extract data, using a unified data extraction form. Agreement on data extraction was established by discussion.The data extracted from the eligible studies was as follows: the first author, publication year, country, sample size, age, diagnostic methods of H. pylori (initial/rechecking), details of the intervention group and the control group, and details of outcomes of interest.
Risk of bias and grading the strength of evidence
Two researchers (Liu LH and Tao J) separately evaluated the risk of bias and quality of evidence for each study, and consensus was used to settle any disputes. The Cochrane Collaboration’s tool was employed to assess the risk of bias of the included studies. The main domains of evaluation were random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases [14]. We evaluated each domain based on three categories (low risk, high risk, and uncertain risk). Utilizing the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach and GRADE profiler software (Version 3.6.1, McMaster University, 2014), the quality of evidence was appraised and categorized into four levels: high, moderate, low, and very low [15].
Statistical analysis
Meta-analysis was performed utilizing RevMan5.3 software (Cochrane Collaboration, Copenhagen, Denmark), and relative risk (RR) and its 95% confidence intervals (CIs) were employed as efficacy analysis statistics for counting data.
To get a conservative estimate of the 95% CI, we utilized a random-effects model to analyze the data for all outcomes [16]. For H.pylori eradication rate, data were analyzed by intention-to-treat (ITT) and per-protocol (PP) analysis. Assessing the heterogeneity between studies, the I2 statistic and the chi-square test with a P value < 0.10 were used, the latter to define substantial heterogeneity. Heterogeneity was classified as insignificant, low, moderate, and high when I2 values were 0–25%, 26–50%, 51–75%, and above 75%, respectively [17]. For primary outcome (H.pylori eradication rate), subgroup analyses was conducted based ITT analysis. To determine whether the exclusion of any single study would significantly alter the results of the remainders, sensitivity analyses were conducted by omitting each trial one at a time. An evaluation of publication bias was conducted with the aid of funnel plot, Begg’s test [18] and Egger’s test [19], which were all implemented using STATA/SE (Version 12.0, STATA Corporation, Texas, USA).
Results
Study selection
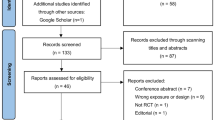
The literature search produced 596 records. After eliminating 201 duplicate articles, 327 were further excluded from the 395 articles by reading titles or abstracts. Subsequently, 68 articles were assessed in full text, out of which 53 were excluded for various reasons (see Supplementary Table S2). Consequently, 15 studies [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34] were included in this meta-analysis. A visual representation of the multi-step selection process was depicted in Fig. 1.
Study characteristics
The 15 RCTs (involving 2156 patients) included were conducted between 2009 and 2023, with one [20] in Europe (Romania) and the rest in Asia (China) [21,22,23,24,25,26,27,28,29,30,31,32,33,34]. The sample size of the trials spanned from 60 to 500 individuals. Regarding H. pylori eradication regimens, the vast majority of the regimens were standard triple therapy (omeprazole + amoxicillin + clarithromycin), and the duration of eradication regimen vary from a week to two weeks. Most studies have included S. boulardii with a dosage of 500 mg/day for a period of 14 days. Table 1 outlines the basic characteristics of the studies that were included in the meta-analysis.
Risk of bias
Of the 15 RCTs, 7 RCTs [20, 24, 28, 30, 31, 33, 34] were assessed as low risk of randomization due to their sufficient random sequence generation methods, while the remaining 8 RCTs [21,22,23, 25,26,27, 29, 32] were deemed unclear risk. Regarding blinding, one study [20] was an open trial and was judged to be of high risk, the other 14 RCTs were considered to have an unclear risk of bias due to a lack of adequate information. All studies failed to provide information for allocation concealment, making the risk of bias unclear. All studies indicated low risk in terms of incomplete outcome data, selective reporting, and other bias. A thorough examination of the risk of bias can be found in Supplementary Figures S1 and S2.
Primary outcome: H. Pylori eradication rate
Fifteen RCTs provided information on the H. pylori eradication rate. Results of the meta-analysis indicated that
S. boulardii in combination with STT was more effective than STT alone, regardless of ITT analysis (87.7% vs. 75.9%, RR = 1.14, 95% CI: 1.10–1.19, P < 0.00001) (Fig. 2) or PP analysis (88.5% vs. 76.3%, RR = 1.15, 95% CI: 1.10–1.19, P < 0.00001) (Fig. 3). No heterogeneity was identified across studies (I2 = 0).
Subgroup analyses based on the dose and duration of S. boulardii were conducted to explore the potential influencing factor on the overall results. The results indicated that S. boulardii supplementation significantly improved H. pylori eradication rate in both low dose and duration S. boulardii group (250 mg/days, 7–10 days) (n = 2 RCTs, RR = 1.17, 95%CI:1.03-1.32, P = 0.02) and high dose and duration S. boulardii group (500 mg/days, 14–28 days) (n = 13 RCTs, RR = 1.14, 95%CI:1.10–1.19, P < 0.00001) (Fig. 4). Performing a sensitivity analysis by omitting one trial at a time revealed that the pooled results of the remaining studies remained unchanged, indicating the results were stable.
Secondary outcomes: adverse events
Data on total adverse events was reported in six RCTs [20, 22, 24, 29, 31, 34] involving 583 patients. The meta-analysis revealed that the combination of S. boulardii and STT had a significantly lower incidence of total adverse events than STT alone (9.2% vs. 29.2%, RR = 0.32, 95% CI: 0.21–0.48, P < 0.00001). No heterogeneity was observed (I2 = 0, P = 0.96) (Fig. 5).
Regarding specific adverse events, the meta-analysis revealed that S. boulardii combined STT group had a significantly lower incidence of diarrhea (n = 13 RCTs, 14.7% vs. 32.4%, RR = 0.46, 95% CI: 0.37–0.56, P < 0.00001) (Fig. 6) and nausea (n = 11 RCTs, 12.7% vs. 21.3%, RR = 0.53, 95% CI: 0.40–0.72, P < 0.0001) (Fig. 7) when compared to the STT group. Similarly, the incidence of vomiting, constipation, abdominal pain, abdominal distention, epigastric discomfort, poor appetite and stomatitis in the S. boulardii combined with STT group was significantly lower than that in the STT group (Supplementary Figure S3-S4). However, we did not observe any considerable difference between the research groups in terms of taste disorder (n = 1 RCT, RR = 0.50, 95% CI: 0.16–1.53, P = 0.22) and rash (n = 4 RCTs, RR = 0.32, 95% CI: 0.09–1.18, P = 0.09). The results of adverse events can be seen in Table 2.
GRADE assessment
We employed the GRADE approach to assess the quality of evidence. According to the GRADE assessment, the H. pylori eradication rate (ITT data) has a low quality rating, largely due to the potential for bias stemming from unclear random sequence generation and allocation concealment, no or unclear blinding, and reporting bias.The quality of evidence for the incidence of all adverse events was assessed as low to medium, mainly because of risk of bias in study design, the possibility of bias, statistical heterogeneity, or reporting bias. The GRADE evidence profiles for all the outcomes can be found in Supplementary Tables S3-S4.
Publication bias
An examination of publication bias was conducted on three outcomes (H. pylori eradication rate, incidence of diarrhea and nausea) that had more than 10 studies, and the visual funnel plot revealed a slight asymmetry (Supplementary Figure S5-S7). Furthermore, we utilized Begg’s test and Egger’s test for quantitative detection of publication bias. For H. pylori eradication rate, Begg’s test did not detect any evidence of publication bias (PBegg = 0.06), but Egger’s test suggested that there may be a publication bias (PEgger = 0.034). Similar results were observed for nausea (PBegg = 1.000, PEgger = 0.041). For diarrhea, results from both Begg’s test and Egger’s test indicate the possibility of publication bias (PBegg = 0.009, PEgger = 0.000).
Discussion
Currently, probiotics are commonly supported for their positive effects on human health and are frequently employed to treat antibiotic-induced diarrhea, inflammatory bowel disease, irritable bowel syndrome, allergic illnesses, and cancer [1, 35]. With the deepening of research into intestinal microecology in recent years, the concept of “probiotics inhibiting bacteria” has brought forth new ideas for eradicating H. pylori. S. boulardii is a non-pathogenic yeast that is able to resist stomach acid, bile, and proteolytic enzymes. Compared to other bacterial probiotics, its major distinction is its inherent resistance to antibiotics, making it suitable for use in conjunction with antibiotics [36, 37]. It is unclear exactly how
S. boulardii eliminates H. pylori, but there are a few possible explanations. One is that it produces substances, such as short chain fatty acids, that inhibit H. pylori growth [38]. Additionally, S. boulardii has a larger surface area than other probiotics, so it can better adhere to the gastric mucosa, preventing H. pylori colonization and adhesion [37]. The neuraminidase present in S. boulardii can also remove H. pylori adhesin ligands and stop the bacteria from attaching to the duodenal mucosa [39]. Furthermore, S. boulardii has been shown to stabilize the tight junction of gastric mucosal epithelial cells, stimulating SIgA response and strengthening the gastric mucosal barrier [40, 41]. Finally, by reducing adverse reactions and improving patient compliance, S. boulardii may indirectly improve the eradication rate of H. pylori.
As far as we are aware, this is the first meta-analysis to explore the effect of S. boulardii supplementing with STT in eradicating H. pylori in children. In this meta-analysis of 15 RCTs (2156 children), we found that S. boulardii was beneficial in improving the H. pylori eradication rate of STT, which was consistent with the findings of the previous meta-analysis [12]. However, the prior meta-analysis took into account 18 RCTs, mostly concerning adults, with only three of the RCTs involving children. Our meta-analysis focused solely on children, and all the RCTs included in previous studies were included in our meta-analysis. Thus, the conclusions drawn are more comprehensive and reliable. Antibiotics may disrupt the balance of the gastrointestinal microbiota, resulting in gastrointestinal adverse events such as diarrhea, nausea, vomiting, abdominal pain, and abdominal distention. This study found that the addition of S. boulardii reduced the total incidence of adverse events by 20% and decreased the incidence of major gastrointestinal adverse events such as diarrhea, nausea, vomiting, constipation, abdominal pain, abdominal distention, epigastric discomfort, and poor appetite.
Nowadays, H. pylori infection has become a major public health concern. Treating H. pylori is becoming more difficult due to the rising antibiotic resistance and patient noncompliance [42]. Our research has significant clinical implications as it provides a good treatment strategy for H. pylori infection, i.e. supplementing with S. boulardii in STT can significantly improve the eradication rate of H. pylori and reduce some adverse events during eradication treatment. Despite the lack of strong evidence (low evidence for H. pylori infection rate and low to medium evidence for adverse events) to support its widespread recommendation, physicians should be cognizant of these strategies when attempting to eradicate H. pylori.
Our meta-analysis has several strengths. Our meta-analysis collected data limited to a single probiotic, S. boulardii, as it appears not all probiotics are effective in eradicating H. pylori. To our knowledge, this is the first meta-analysis to explore the efficacy of supplementing S. boulardii with STT in eradicating H. pylori only in the pediatric population. In addition, we employed a thorough search strategy, explicit selection criteria, and a stringent quality assessment with the aid of the Cochrane Collaboration tool and GRADE approach, in addition to strictly adhering to the PRIMSA statement for reporting, with no heterogeneity detected among estimates for primary outcome. Hence, our meta-analysis provided the most comprehensive and convincing evidence for the efficacy of the STT for the elimination of H. pylori in children with S. boulardii.
Despite its strengths, this meta-analysis has certain limitations that should be taken into consideration. Firstly, this meta-analysis only included RCTs, however, most studies had obscured allocation and uncertain blinding, which could have an effect on subjective outcome indicators, such as the incidence of adverse events. In the future, it is necessary to conduct open and transparent RCTs with large samples and high-quality multicenter placebo controls for further exploration of the effect of S. boulardii in assisting in eradicating H. pylori. Secondly, most of the studies were conducted in Asia (China), while one was conducted in Europe (Romania). Given the antibiotic resistance patterns of H. pylori infection and the potential variability of population characteristics, additional research is necessary in Western countries in the future. Thirdly, there were certain differences in the eradication regimen and treatment durations and doses of S. boulardii among different studies, but this was only a small part of the included studies. The majority of the eradication regimens in most studies were omeprazole + amoxicillin + clarithromycin, and most studies studies have included S. boulardii with a dosage of 500 mg/day for a period of 14 days. Therefore, we believe that the impact on our results can be negligible. Finally, our publication bias test indicated the possibility of publication bias. We have adopted a wide range of retrieval strategies, including papers and conference abstracts, to reduce the possibility of such bias.
Conclusion
To conclude, current evidence indicated that S. boulardii supplementing with STT could improve the eradication rate of H. pylori, and concurrently decrease the incidence of total adverse events and gastrointestinal adverse events in children. In the future, it is essential to carry out more large-scale, high-quality, and multicenter RCTs to further investigate the effect of different doses and durations of S. boulardii on H. pylori eradication in children.
Data availability
The data presented in the study are included in the original article/Supplementary Material. Further inquiries can be directed to the corresponding author.
References
Liang B, Yuan Y, Peng XJ, Liu XL, Hu XK, Xing DM. Current and future perspectives for Helicobacter pylori treatment and management: from antibiotics to probiotics. Front Cell Infect Microbiol. 2022;12:1042070.
Zamani M, Ebrahimtabar F, Zamani V, Miller WH, Alizadeh-Navaei R, Shokri-Shirvani J, et al. Systematic review with meta-analysis: the worldwide prevalence of Helicobacter pylori Infection. Aliment Pharmacol Ther. 2018;47(7):868–76.
Malfertheiner P, Camargo MC, El-Omar E, Liou JM, Peek R, Schulz C, et al. Helicobacter pylori Infection. Nat Rev Dis Primers. 2023;9(1):19.
Malfertheiner P, Megraud F, Rokkas T, Gisbert JP, Liou JM, Schulz C et al. Management of Helicobacter pylori Infection: the Maastricht VI/Florence consensus report. Gut. 2022 Aug 8:gutjnl-2022-327745. https://doi.org/10.1136/gutjnl-2022-327745. Epub ahead of print.
Jones NL, Koletzko S, Goodman K, Bontems P, Cadranel S, Casswall T, et al. Joint ESPGHAN/NASPGHAN guidelines for the management of Helicobacter pylori in Children and adolescents (Update 2016). J Pediatr Gastroenterol Nutr. 2017;64(6):991–1003.
Kato S, Shimizu T, Toyoda S, Gold BD, Ida S, Ishige T, et al. The updated JSPGHAN guidelines for the management of Helicobacter pylori Infection in childhood. Pediatr Int. 2020;62(12):1315–31.
Subspecialty Group of Gastroenterology, the Society of Pediatrics, Chinese Medical Association; National Children′s Medical Center Digestive Specialist Alliance. Editorial Board, Chinese Journal of Pediatrics. Expert consensus on the diagnosis and management of Helicobacter pylori Infection in Chinese children (2022). Zhonghua Er Ke Za Zhi. 2023;61(7):580–7.
Qureshi N, Li P, Gu Q. Probiotic therapy in Helicobacter pylori Infection: a potential strategy against a serious pathogen? Appl Microbiol Biotechnol. 2019;103(4):1573–88.
Keikha M, Karbalaei M. Probiotics as the live microscopic fighters against Helicobacter pylori gastric Infections. BMC Gastroenterol. 2021;21(1):388.
Daelemans S, Deseck V, Levy EI, Vandenplas Y. Are pro- and/or synbiotics beneficial in Helicobacter pylori eradication therapy in children? A narrative review. Eur J Pediatr. 2022;181(9):3225–34.
Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11(8):506–14.
Zhou BG, Chen LX, Li B, Wan LY, Ai YW. Saccharomyces boulardii as an adjuvant therapy for Helicobacter pylori eradication: a systematic review and meta-analysis with trial sequential analysis. Helicobacter. 2019;24(5):e12651.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
DerSimonian R. Meta-analysis in the design and monitoring of clinical trials. Stat Med. 1996;15:1237–48.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Egger M, Smith Gd, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Hurduc V, Plesca D, Dragomir D, Sajin M, Vandenplas Y. A randomized, open trial evaluating the effect of Saccharomyces boulardii on the eradication rate of Helicobacter pylori Infection in children. Acta Paediatr. 2009;98(1):127–31.
Zhang Y, Li J. The effect of Saccharomyces boulardii on triple therapy for Helicobacter pylori Infection in children. J Clin Pediatr. 2012;30(10):928–31.
Zhang H. Analysis of the therapeutic effect of combination therapy with Saccharomyces boulardii on Helicobacter pylori Infection in children. Chin Minkang Med. 2013;25(1):38–40.
Zhao HM, Ou-Yang HJ, Duan BP, Xu B, Chen ZR, Tang J, et al. Clinical effect of triple therapy combined with Saccharomyces boulardii in the treatment of Helicobacter pylori Infection in children. Zhong Guo Dang Dai Er Ke Za Zhi. 2014;16(3):230–3.
Zhou F, Li XQ. A study on the efficacy of combined triple therapy with Saccharomyces boulardii in eradicating Helicobacter pylori Infection in children. J China Modern Doctor. 2015;13:71–3.
Bin Z, Ya-Zheng X, Zhao-Hui D, Bo C, Li-Rong J, Vandenplas Y. The Efficacy of Saccharomyces boulardii CNCM I-745 in Addition to Standard Helicobacter pylori Eradication Treatment in Children. Pediatric gastroenterology, hepatology & nutrition. 2015, 18(1):17-22.
Chen LZ. A study on drug treatment plans for Helicobacter pylori Infection in children. Chin J Integr Traditional Chin Western Med Digestion. 2015;23(12):865–7.
Wang Ht, Kang LM, Zhao Q. Observation of the efficacy of microecological adjuvant therapy in 107 children with Helicobacter pylori Infection. Chin J Med Clin Sci. 2017;17(10):1476–8.
Xiang M, Du M, Deng XZ, Shang LH. Clinical value of triple therapy combined with Saccharomyces boulardii in the treatment of Helicobacter pylori Infection in children. Practical Hosp Clin J. 2017;14(5):98–101.
Dong N, Xu W, Zhu DR, Sheng WS. The efficacy of triple therapy combined with probiotics in the treatment of Helicobacter pylori Infection in children. Jiangsu Med J. 2018;44(11):1287–9.
He J, Wang W, Gao CY. The treatment of Helicobacter pylori Infection in children with the combination of bladder’s yeast powder and triple therapy. Chin J Microbiol. 2019;31(02):171–3.
Zhu J, Hu C, Lu M, Wang X, Liu Y, Luo Y, et al. Efficacy analysis of probiotic combined with standard treatment regimen for eradicating Helicobacter pylori in children. Chin J Practical Pediatr Clin. 2019;19:1454–7.
Xiao Q, Shao Z. Observation on the effect of Saccharomyces boulardii assisted eradication of Helicobacter pylori. Med Forum. 2021;25(20):2861–3.
Zhang J, Wang Y, Li X, Zhang Y. The effect of adding Saccharomyces boulardii powder combined with triple therapy in the treatment of Helicobacter pylori Infection in children at different stages. Henan Med Res. 2021;30(20):3670–3.
Liu QJ. A study on the efficacy of adding probiotics based on a first-line plan in the eradication of Helicobacter pylori. Yan’an Univ. 2023. https://doi.org/10.27438/d.cnki.gyadu.2022.000718.
Guarner F, Khan AG, Garisch J, Eliakim R, Gangl A, Thomson A, et al. World Gastroenterology Organisation Global Guidelines: probiotics and prebiotics October 2011. J Clin Gastroenterol. 2012;46(6):468–81.
Vandenplas Y, Brunser O, Szajewska H. Saccharomyces boulardii in childhood. Eur J Pediatr. 2009;168(3):253–65.
Czerucka D, Piche T, Rampal P. Review article: yeast as probiotics-Saccharomyces boulardii. Aliment Pharmacol Ther. 2007;26(6):767–78.
McFarland LV. Systematic review and meta-analysis of Saccharomyces boulardii in adult patients. World J Gastroenterol. 2010;16(18):2202–22.
Sakarya S, Gunay N. Saccharomyces boulardii expresses neuraminidase activity selective for α2,3-linked sialic acid that decreases Helicobacter pylori adhesion to host cells. APMIS. 2014;122(10):941–50.
Buts JP, Bernasconi P, Vaerman JP, Dive C. Stimulation of secretory IgA and secretory component of immunoglobulins in small intestine of rats treated with Saccharomyces Boulardii. Dig Dis Sci. 1990;35(2):251–6.
Dahan S, Dalmasso G, Imbert V, Peyron JF, Rampal P, Czerucka D. Saccharomyces boulardii interferes with enterohemorrhagic Escherichia coli-induced signaling pathways in T84 cells. Infect Immun. 2003;71(2):766–73.
Zhou BG, Yan XL, Wan LY, Zhang Q, Li B, Ai YW. Effect of enhanced patient instructions on Helicobacter pylori eradication: a systematic review and meta-analysis of randomized controlled trials. Helicobacter. 2022;27(2):e12869.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Lian-Hua Liu, Bin Han and Wen-Yu Wang designed the study. Lian-Hua Liu, Jing Tao, Kai Zhang and Xi-Ke Wang performed the literature search, screened the literature, collected and assembled the data. Lian-Hua Liu and Bin Han analyzed and interpreted the data. Lian-Hua Liu drafted the manuscript. Wen-Yu Wang proofread the manuscript. All authors reviewed the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, LH., Han, B., Tao, J. et al. The effect of Saccharomyces boulardii supplementation on Helicobacter pylori eradication in children: a systematic review and meta-analysis of Randomized controlled trials. BMC Infect Dis 23, 878 (2023). https://doi.org/10.1186/s12879-023-08896-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08896-4