Abstract
Background
People living with HIV (PLHIV) are at higher risk for human papillomavirus (HPV)-related oropharyngeal cancers compared to the general population. Xpert HPV test is a polymerase chain reaction (PCR) assay capable of rapid HPV detection. Performing the assay requires minimal intervention by laboratory personnel. Its use could improve oropharyngeal cancer screening among PLHIV living in low-and middle-income countries (LMICs) with limited diagnostic capacities. However, Xpert HPV performance for oral samples has not been evaluated. Here, we describe our experience with Xpert HPV and compare its results with traditional PCR, for oral samples.
Methods
Oral samples from 429 PLHIV receiving care at a tertiary care hospital affiliated antiretroviral therapy center in Pune, India were used. Samples were collected either after a 30s oral rinse and gargle (n = 335) or in combination with cytobrush scraping of the oral mucosa (n = 91). Unsuccessful tests were those that generated an invalid or error result on Xpert HPV. Successful tests were those that generated a positive or negative result. Kappa statistic was used to compare concordance between Xpert HPV and traditional real-time PCR results.
Results
There were 29.8% (n = 127) unsuccessful tests, of which 78.7% (n = 100) were invalid and 21.3% (n = 27) were error results. Adding cytobrush scraping to oral rinse as a collection procedure did not significantly reduce the proportion of unsuccessful tests (p = 0.9). For successful tests, HPV positivity on Xpert was 0.3% (n = 1/299). Kappa statistic was 0.11, indicating poor agreement between Xpert HPV and traditional PCR results.
Conclusions
Presently, Xpert HPV appears to have limited use for oral HPV detection among PLHIV using oral samples. More research to improve the diagnostic capabilities of Xpert HPV for oral samples among PLHIV is needed.
Similar content being viewed by others
Introduction
People living with HIV (PLHIV) have 2-3-fold higher odds of prevalent oral human papillomavirus (HPV) compared to HIV-uninfected individuals [1]. Oncogenic high-risk HPV (hrHPV) types (mostly HPV16, HPV18 and HPV33) [2], have been isolated in 12–26% of oral samples of PLHIV in previous studies [1]. This puts PLHIV at an increased risk of oropharyngeal squamous cell carcinomas (OPSCCs), including cancers of the base of tongue, lingual and palatine tonsils [1, 2].
Traditional diagnostic methods for oral HPV rely on polymerase chain reaction (PCR) or in-situ hybridization (ISH) techniques [3]. These techniques require skilled laboratory personnel and several hours to complete [4]. In low-and middle-income countries (LMICs) where the dual burden of HIV and OPSCCs is high [5,6,7], trained personnel are lacking, and health systems congested, the feasibility of these techniques may be limited [5].
The Xpert HPV (Cepheid Sunnyvale, CA) test is a rapid, PCR assay for the qualitative real time detection of 14 types of hrHPV DNA [8]. Sample extraction, PCR amplification, and HPV detection are fully automated on Xpert HPV. The assay is performed on Cepheid GeneXpert instrument system. Positive qualitative findings can further be reported as positive or negative for HPV 16, HPV 18/45, and a pooled result for 11 hrHPV types (31, 33, 35, 39, 51, 52, 56, 58, 59, 66 and 68). The assay contains two internal controls, a Sample Adequacy Control (SAC) and a Probe Check Control (PCC). SAC reagents detect the presence of a single copy human gene and monitor the adequacy of human cells to carry out a qualitative HPV assessment. Failure of the SAC leads to an invalid result. The PCC verifies reagent rehydration, PCR tube filling, probe integrity, and dye stability. Failure of the PCC leads to an error result [8]. Running the assay requires minimal training and the instrument provides results within one hour, allowing for same day HPV screening [4, 9]. In LMICs, Xpert HPV could bolster oral cancer screening strategies by rapidly identifying PLHIV with oral hrHPV, who may benefit from same-day HPV counselling, closer clinical examination and follow-up.
Xpert HPV has been successfully deployed with acceptable validity for HPV detection among women living with HIV using cervical fluid samples [4], and more recently anal fluid samples [10, 11]. It has also been used for HPV detection in formalin-fixed paraffin-embedded oropharyngeal cancer samples [12]. However, the use of oral samples has not been evaluated. There is also limited evidence on the implementational challenges of Xpert HPV use. Previous studies of Xpert MTB/RIF assays for Mycobacterium tuberculosis have reported different proportions of invalid and error results globally [13,14,15], limiting the optimal use of the assay.
In this manuscript, using data collected from PLHIV in Pune, India our objectives are, (1) To describe the implementational challenges of HPV Xpert using oral samples, particularly SAC and PCC failures; (2) To assess the agreement of Xpert HPV with traditional PCR results for oral samples.
Method
Study population
We used data from a parent cross-sectional study that sought to evaluate the prevalence of oral potentially malignant disorders (OPMDs) among PLHIV (n = 601) and HIV-uninfected individuals (n = 633) [16]. For this analysis, we excluded HIV-uninfected individuals. Brief recruitment procedures for PLHIV described below were those followed in the parent study.
PLHIV were enrolled from the antiretroviral therapy (ART) center of Byramjee Jeejeebhoy Government Medical College – Sassoon General Hospitals (BJGMC-SGH) in Pune, a city in western India. The ART center caters to approximately 5000 PLHIV, belonging to lower and middle socioeconomic status. A registry-based study showed that the 28-to-60-month standardized incidence ratio of oral and oropharyngeal cancers was 27 times higher (95% CI: 19.7, 36.1) among PLHIV compared to the general population of Pune [17].
All PLHIV ≥ 21 years with no prior history of oral cancer attending the ART center between June 2017 and June 2019 were approached by two study counselors. Eligible participants that provided informed consent were enrolled into the study. Enrollees completed counsellor-administered questionnaires, provided oral samples and photographs of the oral cavity. Study procedures have been described at length elsewhere [16]. Sociodemographic, tobacco and alcohol use, sexual history, CD4 count, suspected OPMDs, Xpert HPV results, and traditional PCR results data were extracted from the database of the parent study.
The study was approved by the Ethics Committee of BJGMC-SGH and the Institutional Review Board of Johns Hopkins University (JHU).
Laboratory methods
All laboratory procedures (unless explicitly stated) were carried out at the JHU-Clinical Research Site (CRS) laboratory associated with BJGMC-SGH. The laboratory is approved by the Division of AIDS, United States National Institutes of Health (NIH) and was involved in an NIH-funded HPV-related clinical trial (A5282) [18].
Procedures for oral sample collection and processing
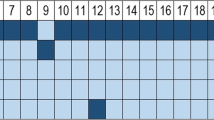
Due to procurement delays for Xpert HPV supplies, we were able to test only 426 oral samples from PLHIV using the assay (Fig. 1). The procedures for sample collection and processing are described below. Most samples (n = 403) were collected between 9 am and 12 pm.
Flowchart showing the number of participant samples processed on Xpert HPV and traditional PCR respectively. Xpert HPV identifies only certain high risk HPV types (HPV 16, 18/45, 31, 33, 35, 39, 51, 52, 56, 58, 59, 66, 68). Therefore, even under perfect agreement with traditional PCR, Xpert HPV would have deemed positive only 16 of the 27 PCR HPV positive samples. Other low risk HPV types detected by conventional PCR (HPV 7, 13, 27, 32, 42, 44, 72, 90, 107, 120) would have been deemed negative by Xpert HPV (represented by dotted boxes)
Procedure 1
Collection
For the first 335 participants, a 15 mL oral rinse sample was collected by instructing participants to alternate between swishing and gargling with alcohol-free Colgate® Plax mouthwash for 30 s. Samples were collected aseptically in a 50 mL Falcon™ conical tube (Becton Dickinson) and kept on ice until processed within four hours of collection.
Processing
The collected sample was centrifuged twice, at 5000 RPM and 4 degrees Celsius for 10 min each time. A 2 mL final suspension in Cervi-Collect solution (Abbott Molecular) was created using the pellet obtained after two centrifugations.
Procedure 2
Collection
The next 91 participants were first instructed to rinse their oral cavity with water and wait for 30 min. This was done to remove any particulate matter (particularly betel quid or tobacco residues) from the oral cavity. Using a cytobrush (Abbott Molecular), participants were then instructed to scrape their right and left buccal mucosa and the surface of any suspected OPMD. The cytobrush scraping was placed in Cervi-Collect solution. This was followed by an oral rinse as for Procedure 1.
Processing
A suspension using the oral rinse (as for Procedure 1) was created first. A final pooled suspension (2.5 mL) was created by vortexing the oral rinse suspension and the Cervi-Collect solution in which the cytobrush scraping was placed.
Final suspensions obtained from each procedure were divided into two vials, each of 1 to 1.5 mL (Fig. 2).
For the Xpert HPV assay, 1 mL (recommended volume) of the final suspension was used [8]. All samples were processed on the day of collection. Suspensions were stored at negative 80 degrees Celsius if not tested immediately. All testing using Xpert HPV assay was performed within two weeks of sample collection.
We changed from Procedure 1 to Procedure 2, because there were many Xpert invalid (n = 78) and error (n = 21) results for Procedure 1 (i.e., SAC or PCC failures). After consulting with experts at the NIH funded Virology Quality Assurance (VQA) program at Rush University, Chicago, USA [19], the addition of cytobrush scraping was recommended to mimic cervical sample collection methods more closely [9]. It was hypothesized that this may reduce SAC failures by increasing epithelial cell concentration of the final suspension. Simultaneously we posited that potential oral particulate matter could be a source of interference leading to invalid and error results. Therefore, a preliminary oral rinse with water was also included in Procedure 2, consistent with a recommendation to reduce the proportion of unsuccessful tests on Xpert MTB/RIF [20].
Procedures to limit SAC and PCC failures
We undertook several steps to limit SAC and PCC failures. Prior to the start of the parent study, to verify that internal controls were functioning optimally, we pilot tested eleven Xpert HPV assays using a quality control sample for HPV created by VQA and 10 Xpert HPV assays using oral samples (utilizing Procedure 1). Pilot testing was conducted under the supervision of a Cepheid representative. There were no invalid or error results for these preliminary 21 samples. To reduce the variability in the instructions provided to participants all sample collections were supervised by the same two trained laboratory technicians. Further, to reduce variability in sample preparation, all centrifugations, suspension preparations, and assay runs (including pipetting 1mL of the final suspension into the Xpert cartridge) were conducted by the same technicians, supervised by a virologist trained in Xpert methodology. (Table 1)
All tests were conducted in an air-conditioned laboratory, where room temperature was charted regularly and maintained at or below 25 degrees Celsius. There were no interruptions to electricity supply, and all assays were stored at 20 degrees Celsius (recommended 2 to 28 degrees Celsius). The Xpert instrument was kept at 15 cm from the wall to allow any heat generated to dissipate easily. All these conditions were maintained to prevent other sources of error results that could arise due to interrupted electricity supply, loss of assay integrity due to poor storage and overheating of the Xpert instrument [13].
Oral HPV testing via traditional PCR and next generation sequencing
Of the 426 samples available for Xpert HPV, there were 407 samples concomitantly tested using traditional SYBR Green Real-Time PCR (Fig. 1). Nineteen samples were deemed to have insufficient volume for traditional PCR.
A pool of primers targeting the L1/L2 (PGMY11/09) region was used. Testing was done at a private laboratory (GenePath Diagnostics, Pune). The primer pool used included those from literature [21] and proprietary primers designed to improve coverage. Positive samples from the first PCR were further processed using a second nested PCR, with typing primers targeting the GP5+/6 + region within the L1 region using modified primers that contained proprietary in-house next generation sequencing (NGS) adapters and indexing tags. The adjusted and pooled amplicons were sequenced using paired-end sequencing by synthesis chemistry (Illumina MiSeq). Genotyping was determined using an in-house developed bioinformatics pipeline. Details of the PCR and NGS methods are provided in the supplementary file.
Study definitions
We classified Xpert tests results as successful and unsuccessful, as previous studies evaluating the Xpert MTB/RIF have done [13,14,15]. Samples that generated either negative or positive Xpert results were deemed successful. Samples that generated either invalid or error results were deemed unsuccessful.
Statistical analyses
We described successful and unsuccessful results across participant characteristics. Kruskal-Wallis and Fisher’s exact tests were used to compare across continuous and categorical variables, respectively. Statistical significance was set to a p-value of 0.05.
For successful tests, we compared the concordance between the Xpert HPV and SYBR Green Real-Time PCR results using the kappa statistic.
Analyses were performed using Stata 17.0.
Results
Successful and unsuccessful xpert tests
Of 426 samples tested on Xpert HPV, 29.8% (n = 127) were unsuccessful. Of these, 78.7% (n = 100) were invalid and the remainder (21.2%, n = 27) error results, respectively (Table 2). All samples with adequate volume (n = 407) were successfully tested on traditional PCR. (Fig. 1).
The median age of participants that contributed oral samples tested on Xpert HPV was 40 years (IQR: 34 to 46), with 51.2% (n = 218) of the samples collected from biological males. More than a quarter of the samples (26.8%, n = 114) were from PLHIV that reported multiple sexual partners in their lifetime. Only 12.2% (n = 52) of the samples came from PLHIV that reported having given oral sex in their lifetime. None of the participants that contributed samples had received any HPV vaccinations.
Successful and unsuccessful tests were not statistically significantly different across Procedure 1 and Procedure 2, or any other variables. (Table 2)
Agreement of successful Xpert HPV and traditional PCR results
Of 299 successful Xpert HPV tests, there were 286 samples correspondingly tested using traditional PCR. (Fig. 1)
Only one sample was identified as HPV positive by Xpert, resulting in an HPV positivity of 0.3% (i.e., 1/299). Traditional PCR identified 27 samples as HPV positive, resulting in a positivity of 9.4% (i.e., 27/286). (Fig. 1)
The kappa statistic was 0.11, indicating poor agreement between Xpert HPV and traditional PCR results. (Table 3).
Discussion
Approximately a third of the oral samples tested on Xpert HPV had unsuccessful results. Additionally, for successful tests, there was poor agreement between Xpert HPV and traditional PCR results. Our findings indicate that Xpert HPV may not be useful as a screening tool for HPV detection using oral samples among PLHIV.
Estimates for the proportions of unsuccessful Xpert HPV tests using cervical fluid and anal fluid are not available. However, our proportion of unsuccessful tests (29.8%) is higher than those reported for Xpert MTB/RIF across different studies (5–11%) [13,14,15, 22, 23]. Furthermore, neither SAC nor PCC failures were significantly reduced with a change in oral sample collection methods i.e., the proportion of invalid and error results remained comparable before and after changing oral sample collection methods. These findings suggest that potential oral particulate matter did not contribute significantly to unsuccessful tests, as had been hypothesized.
Most of the unsuccessful tests were due to invalid results. We hypothesize that oral samples even when cytobrush scrapings were included may not consistently have the adequate number of human cells required by Xpert HPV SAC reagents. Moreover, despite ensuring uninterrupted electricity supply, proper assay storage, and adequate sample volume for all tests, the proportion of error results in our study was higher than that recommended by the Xpert manufacturer (i.e., 6.3% vs. 5%) [14]. Error results could also be due to poor sample preparation (e.g., sample could be too viscous) causing tube pressure to increase beyond the acceptable pressure limit. Although the same two laboratory technicians were used throughout the study, we cannot completely rule out improper sample preparation as a cause for error results.
The Xpert HPV limit of detection for different HPV genotypes varies between 10 (for HPV16, 18, 31, 33, 45, 51, 59) to 30 (for HPV 66) HPV DNA plasmid copies per PCR reaction [24]. The low positivity observed for Xpert HPV could be secondary to HPV viral load levels being below these limits of detection in oral samples. Moreover, the comparative traditional approach employed a nested PCR, which may have increased its sensitivity for HPV detection [25], further reducing the agreement with Xpert HPV results.
Our study has several limitations that merit mention. The Xpert HPV is standardized for cervical fluid samples and not oral samples [8]. Though it has been successfully tested using anal fluid samples [10, 11], functionally, the oral cavity constitutes a more dynamic environment relative to the cervix or anal canal (i.e., due to regular ingestion of food, water, salivary secretions, etc.). This dynamicity may itself present a challenge with using oral samples, as exfoliated cell concentration and HPV viral loads could be variably affected by voluntary (i.e., eating, drinking, etc.) and involuntary (salivary secretion) processes. While the time and instructions for oral sample collections were consistent for participants, we were unable to control for variations in voluntary and involuntary processes. We did not retest or recollect samples when an error or invalid result was reported, as recommended by Cepheid [8]. Retesting or recollecting oral samples may have improved the performance of Xpert HPV. Future studies should evaluate the extent to which Xpert HPV performance can be improved with retests and recollections of oral samples. However, in care settings with a high number of people seeking care, retests and recollections may not be practicable. Further, we did not quantify HPV viral loads in oral samples, precluding us from drawing definite conclusions about the association between low viral loads and low Xpert positivity. We did not document the codes for the error results when samples were processed [8, 20]. Therefore, we are unable to identify the exact source (i.e., compromised tube integrity, high tube pressure, overheating, etc.) for them. The files (.gxx files) that contained this information were found to be corrupted when we tried to access them later and could not be retrieved even with the assistance of Cepheid representatives. Lastly, as mentioned, HPV is associated with oropharyngeal cancers. Using a tonsillar brush [26] instead of an oral cytobrush may have improved Xpert positivity.
Based on our findings, we believe that currently Xpert HPV has limited utility for oral HPV screening using oral samples among PLHIV. Otimization of oral sample collection methods may reduce SAC and PCC failures, but the issue of poor concordance with traditional PCR methods remains. However, most samples were successfully tested, and one sample was correctly identified to be HPV positive. This leads us to believe that the performance of Xpert HPV using oral samples could be improved. More research to improve the performance of Xpert HPV and evaluation of its utility for oral samples among PLHIV is required.
Data Availability
Many of the participants in the study have disclosed their HIV status only to the study staff and their treating physician, apart from their spouses or close family members. Thus, the datasets are not publicly available. However, researchers can contact the corresponding author if they are interested in using these data.
Abbreviations
- PLHIV:
-
People living with HIV
- HPV:
-
Human papillomavirus
- hrHPV:
-
High risk HPV
- OPSCCs:
-
Oropharyngeal squamous cell carcinomas
- PCR:
-
Polymerase chain reaction
- ISH:
-
In-situ hybridization
- SAC:
-
Sample adequacy control
- PCC:
-
Probe check control
- LMICs:
-
Low- and middle-income countries
- ART:
-
Antiretroviral therapy (ART)
- BJGMC-SGH:
-
Byramjee Jeejeebhoy Government Medical College – Sassoon General Hospitals
- CRS:
-
Clinical Research Site
- NIH:
-
US National Institutes of Health
- VQA:
-
Virology Quality Assurance
- OPMD:
-
Oral potentially malignant disorder
- NGS:
-
Next generation sequencing
- MSM:
-
Men who have sex with men
- SLT:
-
Smokeless tobacco
References
Beachler DC, D’Souza G. Oral human papillomavirus infection and head and neck cancers in HIV-infected individuals. Curr Opin Oncol. 2013;25(5):503–10.
Ganly I, Pei Z, Hao Y, Ma Y, Rosenthal M, Wu Z, Migliacci J, Huang B, Katabi N, Tseng W, et al. Case control study comparing the HPV genome in patients with oral cavity squamous cell carcinoma to normal patients using metagenomic shotgun sequencing. Sci Rep. 2021;11(1):3867.
Augustin JG, Lepine C, Morini A, Brunet A, Veyer D, Brochard C, Mirghani H, Pere H, Badoual C. HPV Detection in Head and Neck squamous cell carcinomas: what is the issue? Front Oncol. 2020;10:1751.
Mbulawa ZZA, Wilkin TJ, Goeieman B, Swarts A, Williams S, Levin S, Faesen M, Smith JS, Chibwesha CJ, Williamson AL, et al. Xpert human papillomavirus test is a promising cervical cancer screening test for HIV-seropositive women. Papillomavirus Res. 2016;2:56–60.
Adebamowo CA, Casper C, Bhatia K, Mbulaiteye SM, Sasco AJ, Phipps W, Vermund SH, Krown SE. Challenges in the detection, prevention, and treatment of HIV-associated malignancies in low- and middle-income countries in Africa. J Acquir Immune Defic Syndr. 2014;67(Suppl 1):17–26.
Shrestha AD, Vedsted P, Kallestrup P, Neupane D. Prevalence and incidence of oral cancer in low- and middle-income countries: a scoping review. Eur J Cancer Care (Engl). 2020;29(2):e13207.
2020, International Agency for Research on Cancer, Globocan, Oropharynx. [https://gco.iarc.fr/today/data/factsheets/cancers/3-Oropharynx-fact-sheet.pdf] Accessed on February 28,2023
(WHO) WHO: WHO Prequalification of In Vitro Diagnostics Product: Xpert HPV version 4.0. In. 2020. https://extranet.who.int/pqweb/sites/default/files/PQDx0268-070-00-XpertHPV_4.0.pdf, Accessed on February 15, 2023.
Einstein MH, Smith KM, Davis TE, Schmeler KM, Ferris DG, Savage AH, Gray JE, Stoler MH, Wright TC Jr, Ferenczy A, et al. Clinical evaluation of the cartridge-based GeneXpert human papillomavirus assay in women referred for colposcopy. J Clin Microbiol. 2014;52(6):2089–95.
Ellsworth GB, Stier EA, Chiao EY, Lensing SY, Darragh T, Jay N, Berry-Lawhorn JM, Einstein M, Barroso LF, Cranston RD, et al. Xpert HPV as a Screening Tool for Anal histologic High-Grade squamous intraepithelial lesions in women living with HIV. J Acquir Immune Defic Syndr. 2021;87(3):978–84.
Mbulawa ZZA, Wilkin T, Goeieman BJ, Jong E, Michelow P, Swarts A, Smith JS, Kegorilwe P, Firnhaber CS, Williamson AL. Prevalence of Anal Human Papillomavirus (HPV) and performance of Cepheid Xpert and Hybrid capture 2 (hc2) HPV assays in south african HIV-Infected women. Am J Clin Pathol. 2017;148(2):148–53.
Dona MG, Rollo F, Pichi B, Spriano G, Pellini R, Covello R, Pescarmona E, Fabbri G, Scalfari M, Gheit T, et al. Evaluation of the Xpert(R) HPV assay in the detection of human papillomavirus in formalin-fixed paraffin-embedded oropharyngeal carcinomas. Oral Oncol. 2017;72:117–22.
Sikhondze W, Dlamini T, Khumalo D, Maphalala G, Dlamini S, Zikalala T, Albert H, Wambugu J, Tayler-Smith K, Ali E, et al. Countrywide roll-out of Xpert((R)) MTB/RIF in Swaziland: the first three years of implementation. Public Health Action. 2015;5(2):140–6.
Gidado M, Nwokoye N, Nwadike P, Ajiboye P, Eneogu R, Useni S, Onazi J, Lawanson A, Elom E, Tubi A, et al. Unsuccessful xpert((R)) MTB/RIF results: the nigerian experience. Public Health Action. 2018;8(1):2–6.
Agizew T, Boyd R, Ndwapi N, Auld A, Basotli J, Nyirenda S, Tedla Z, Mathoma A, Mathebula U, Lesedi C, et al. Peripheral clinic versus centralized laboratory-based Xpert MTB/RIF performance: experience gained from a pragmatic, stepped-wedge trial in Botswana. PLoS ONE. 2017;12(8):e0183237.
Marbaniang I, Joshi S, Sangle S, Khaire S, Thakur R, Chavan A, Gupte N, Kulkarni V, Deshpande P, Nimkar S, et al. Smokeless tobacco use and oral potentially malignant disorders among people living with HIV (PLHIV) in Pune, India: implications for oral cancer screening in PLHIV. PLoS ONE. 2022;17(7):e0270876.
Godbole SV, Nandy K, Gauniyal M, Nalawade P, Sane S, Koyande S, Toyama J, Hegde A, Virgo P, Bhatia K, et al. HIV and cancer registry linkage identifies a substantial burden of cancers in persons with HIV in India. Med (Baltim). 2016;95(37):e4850.
Wilkin T, Chen H, Sahasrabuddhe V, Matining R, Mngqibisa R, Chinula L, Mbilizi Y, Magure T, Omoz-Oarhe AE, Rassool M et al. A randomized clinical trial of HPV test-and-treat as compared to cytology-based screening for prevention of cervical cancer among women living with HIV: AIDS Clinical Trials Group Protocol A5282. Clin Infect Dis 2022.
HIV/AIDS Network Coordination. Virological Quality Assurance Program Resources. Available at: https://www.hanc.info/resources/sops-guidelines-resources/laboratory/virology-quality-assurance-program-resources.html. Accessed June 20, 2022.
Creswell J, Codlin AJ, Andre E, Micek MA, Bedru A, Carter EJ, Yadav RP, Mosneaga A, Rai B, Banu S, et al. Results from early programmatic implementation of Xpert MTB/RIF testing in nine countries. BMC Infect Dis. 2014;14:2.
Gravitt PE, Peyton CL, Alessi TQ, Wheeler CM, Coutlée F, Hildesheim A, Schiffman MH, Scott DR, Apple RJ. Improved amplification of genital human papillomaviruses. J Clin Microbiol. 2000;38(1):357–61.
Raizada N, Sachdeva KS, Sreenivas A, Vadera B, Gupta RS, Parmar M, Kulsange S, Babre A, Thakur R, Gray C, et al. Feasibility of decentralised deployment of Xpert MTB/RIF test at lower level of health system in India. PLoS ONE. 2014;9(2):e89301.
Kebede A, Beyene D, Yenew B, Diriba G, Mehamd Z, Alemu A, Amare M, Ameni G. Monitoring quality indicators for the Xpert MTB/RIF molecular assay in Ethiopia. PLoS ONE. 2019;14(11):e0225205.
Cepheid. Xpert HPV Data sheet. Available at: https://p.widencdn.net/tfeiyy/Cepheid-Xpert-HPV-Datasheet-CEIVD-3011-English. Accessed June 12, 2022.
Green MR, Sambrook J. Nested Polymerase Chain Reaction (PCR).Cold Spring Harb Protoc2019, 2019(2).
Uken RB, Brummer O, von Schubert-Bayer C, Brodegger T, Teudt IU. Oral HPV prevalence in women positive for cervical HPV infection and their sexual partners: a german screening study. Eur Arch Otorhinolaryngol. 2016;273(7):1933.
Acknowledgements
We thank the study staff Archana Pawar and Suhasini Surwase and extend our gratitude to all the staff at BJGMC-SGH ART center. Most of all we thank all our participants, without whom this study would not have been possible.
Funding
This work was supported by amfAR, The Foundation for AIDS Research, with support from the U.S. National Institutes of Health’s National Institute of Allergy and Infectious Diseases, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Cancer Institute, the National Institute of Mental Health, the National Institute on Drug Abuse, the National Heart, Lung, and Blood Institute, the National Institute on Alcohol Abuse and Alcoholism, the National Institute of Diabetes and Digestive and Kidney Diseases, and the Fogarty International Center, as part of the International Epidemiology Databases to Evaluate AIDS (IeDEA; U01AI069907) and the NIH-funded Johns Hopkins Baltimore-Washington-India Clinical Trials Unit for NIAID Networks [UM1AI069465 to VM]. AA is also funded through the Woodrow Wilson Research Fellowship, a part of the Zanvyl Krieger School of Arts and Sciences Undergraduate Research, Scholarly, and Creative Activity office. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
AA, IM: conceived the idea for the manuscript, analyzed the data and drafted the manuscript; SJ, RB, SK, RT: provided clinical inputs; PD, VK: conducted the laboratory examinations; AC: assisted with data analysis; IM, SN: conducted the study on the ground; VM: provided funds to conduct the study. All authors reviewed the final form of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The BJGMC- SGH (Approval date: September 19, 2016) and Johns Hopkins University Ethics Committees (IRB00118708, Approval date: December 13, 2016) approved this study. All study participants provided written informed consent, including written consent for collection of oral samples that are in accordance with the Indian Council of Medical Research (ICMR) guidelines. Please note that BJGMC-SGH does not issue approval numbers.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Admase, A., Joshi, S., Borse, R. et al. Challenges with the use of Xpert HPV as a screening tool for oral HPV among people living with HIV (PLHIV): experiences from Pune, India. BMC Infect Dis 23, 233 (2023). https://doi.org/10.1186/s12879-023-08210-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08210-2