Abstract
Background
Acute myeloid leukemia (AML) is a progressive hematological malignancy that can be fatal when left untreated. However, spontaneous remission is rarely observed in the presence of infectious diseases.
Case presentation
We treated an 80-year-old woman with AML who spontaneously underwent remission after infections. Spontaneous remission was observed after each of three independent clinical infections caused by different pathogens—nontuberculous Mycobacterium infection, pulmonary aspergillosis, and Escherichia coli bacteremia. All infections were treated promptly with antimicrobials. Mycobacterium avium infection was treated with azithromycin, rifampin, and ethambutol. Pulmonary aspergillosis was treated with itraconazole followed by voriconazole. E. coli infection was treated with meropenem. During each infectious episode, leukemic cells disappeared from the patient’s peripheral blood and pancytopenia improved without routine blood transfusion. These clinical effects lasted for several months. The patient has survived for > 2 years beyond the median survival time of end-stage AML. Thus, this case represents an immunological antileukemic effect of systemic infections.
Conclusions
We have discussed a common mechanism of spontaneous remission of AML without chemotherapy, clinically exhibited by infection immunology. We believe that infections exert a limited immunological effect against AML, which may prolong survival among elderly individuals with AML.
Similar content being viewed by others
Background
Acute myeloid leukemia (AML) is a fatal and progressive hematological malignancy [1]. Spontaneous regression (SR) is observed as a rare phenomenon in AML, and some contributing factors for AML SR have been reported [2, 3]. Infectious diseases are an important and common cause of SR [4, 5]. The causative mechanisms of SR in AML are immunological in nature [4, 5], including cellular immunity, serological inducers, cytokine pathways, and indirect immunological mechanisms. We experienced a case of repeated spontaneous remission of AML associated with systemic infections.
Case presentation
An 80-year-old Japanese woman was diagnosed with AML with myelodysplasia-related changes (AML/MRC) via bone marrow examination. She was referred to our hospital with the complication of gradually developing bicytopenia (leukocytopenia and thrombocytopenia), as determined via peripheral blood examination. She had a history of bipolar disorder, which was diagnosed at the age of 78 years, and was treated in the outpatient department of the psychiatric clinic at our hospital. She had no medical history of chemotherapy or radiotherapy. Moreover, she had no history of precedent immunological diseases, such as collagen diseases. She did not receive any immunosuppressive therapy. She had no previous medical history of allergies. However, she had a history of smoking from the age of 20 to 50 years.
Laboratory findings at the first visit of the patient to our hospital were as follows: mild bicytopenia, decrease in white blood cell count to 1600/μL (neutrophils, 31.0%; eosinophils, 2.5%; basophils, 0.0%; lymphocytes, 62.5%; monocytes, 3.0%; and blasts, 0.5%), hemoglobin level of 12.3 g/dL, and decrease in platelet count to 67,000/μL. Mild macrocytic change (mean corpuscular volume, 101.3 fL) was also noted. Biochemical findings, including CRP (0.09 mg/dL) and LDH (192 U/L) levels, showed no abnormalities. The level of WT1 mRNA, a biomarker, increased to 22,000 (normal range < 50) copies/mL. Bone marrow cell count clonally increased to 4.01 × 104/μL; megakaryocyte count decreased to 18/μL, and blast count increased to 45.4%. She exhibited morphological abnormalities with dysplastic changes, including pseudo Pelger–Huet anomaly, degranular neutrophils, micromegakaryocytes, and ringed sideroblasts, in the three lineages of granulocytes, megakaryocytes, and erythroblasts (Fig. 1). Results of screening for chimeras—major BCR-ABL1, minor BCR-ABL1, PML-RARA, RUNX1-RUNX1T1, CBFB-MYH11, DEK-NUP214, NUP98-HOXA9, ETV6-RUNX1, TCF3-PBX1, STIL-TAL1, KMT2A-AFF1, KMT2A-AFDN, KMT2A-MLLT3, and KMT2A-MLLT1—were negative. The chromosomal test revealed a defective del(5q) clone [6/20]. She was diagnosed with AML/MRC, according to the WHO classification, and M2, according to the FAB classification. According to a consensus of geriatric medicine, owing to her age and underlying illness, she was treated with supportive therapy, such as blood transfusion therapy, instead of aggressive therapy.
Bone marrow findings of the case. The leukemic cell morphology includes basophilic cytoplasm with deformed nuclei (upper panels). Erythrocytes, granulocytes, and megakaryocytes, all showed dysplastic changes. Erythrocytes showed megaloblastic changes, and granulocytes were hypogranular and agranular (bottom left panel). Micromegakaryocytes were also observed (bottom right panel). All images were acquired using May Grunwald–Giemsa stain at ×100 magnification
During supportive blood transfusion therapy, her condition was complicated by the following three infectious diseases: nontuberculous Mycobacterium (NTM) infection, pulmonary aspergillosis, and Escherichia coli bacteremia. The course of each of these diseases is summarized as follows. (1) NTM: In August 2020, she complained of hypoxemia (SpO2 level, 91%) and fever (37.5–37.9 °C). She visited the outpatient clinic at our hospital, and initial chest X-ray revealed multiple small granular shadows in both lungs (Fig. 2). She was positive for anti-MAC antibodies, and PCR was positive for Mycobacterium avium in the sputum. We thus diagnosed her with NTM infection. She received triple anti-Mycobacterium (azithromycin, rifampin, and ethambutol) treatment for 2 weeks. Consequently, the pulmonary granular shadows reduced, hematopoiesis recovered (with normalized platelet and erythrocyte counts), and precursor cell count in the peripheral blood decreased. This spontaneous remission status persisted for 3 months. Bone marrow examination was performed during the first spontaneous remission. Blast count was 4.6%, and chromosomal abnormality with del(5q) were detected in 2 of 20 analyzed cells (10%). Background myelodysplasia persisted, with hypogranular neutrophils, pseudo Pelger–Huet anomaly, megaloblastoid changes, ringed sideroblasts, and micromegakaryocytes. Flowcytometry detected a scanty of stem cell clones (1.8%) expressing abnormal phenotypes; HLA-DR+, CD13+, CD34+, CD117+, all of these are originally expressed aberrant phenotype. This result indicated that she achieved hematological remission with cytogenetically minor residual disease. (2) Pulmonary aspergillosis: In March 2021, she presented with fever (38.4 °C) and hypoxemia (SpO2 level, 93%) again. She was treated with levofloxacin for a few weeks, but it did not relieve her fever. In April 2021, chest X-ray revealed pneumonia, with a 43 mm-diameter nodule in her left upper lobe (Fig. 3). She showed elevated levels of β-d-glucan and Aspergillus antigen, suggesting pulmonary aspergillosis. She was treated with itraconazole followed by voriconazole for 20 days, after which inflammation and the lung nodule diminished. Following treatment, hematopoiesis recovered and blasts disappeared from the peripheral blood. The del(5q) clones in the bone marrow were detected in 2 of the 20 analyzed cells. She remained in the state of spontaneous remission for 5 months. (3) E. coli bacteremia: In December 2021, she presented to the outpatient clinic with a fever of 38.4 °C; she was positive for blood procalcitonin (1.55 ng/mL). We assumed that she had sepsis and thus hospitalized her on the same day. Upon hospitalization, ESBL-positive E. coli was detected in two sets of blood cultures, and meropenem treatment was provided. On day 10 of hospitalization, cellulitis of the right lower extremity developed with neutrophil recovery, and ESBL-positive E. coli was detected in the subcutaneous abscess at the same site (Fig. 4). The antimicrobial susceptibility to the isolated E. coli is shown in Fig. 4.
CT imaging of the right lower leg of the patient with Escherichia coli cellulitis and subcutaneous abscess with drug susceptibility. The CT scan of the patient’s lower leg revealed an abscess in the lateral side (indicated by red arrow-heads). E. coli was detected as the causative pathogen through the culture of blood and subcutaneous abscess. The table on the left shows the antimicrobial susceptibility of the isolated E. coli
Her condition improved with puncture drainage and continued antibiotic treatment. During the course of treatment for bacteremia, hematopoiesis recovered and peripheral blood precursor cell count decreased. The del(5q) clones in the bone marrow were only detected in 1 of the 20 analyzed cells. The frequency of blood transfusions decreased; thus, she was temporarily discharged from the hospital. This partial remission status persisted for 3 months. She is still alive and has survived significantly longer than the median survival time of end-stage AML (2 months) [6].
In summary, regarding the mechanisms of the three infectious diseases, we observed multiple therapeutic effects of infectious diseases on AML:
-
(1)
Hematopoiesis recovery and disappearance of peripheral blood precursor cells.
-
(2)
Quantifiable improvement in dysplasia.
-
(3)
Reduced detection of a specific abnormal clone del(5q), as determined using the chromosomal test and FISH.
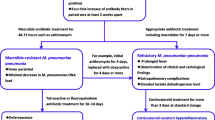
Thus, she continued to survive 2 years after AML onset due to clinical infectious diseases caused by various pathogens. Figure 5 presents the course of all spontaneous remissions in this case.
Clinical course of the three infectious diseases causing spontaneous remission of acute myeloid leukemia in our patient. The bar graph shows the white blood cell (WBC) count, neutrophil (NEUT) count, and blast cell (BLA) count on the left axis. The line graph shows the CRP level, hemoglobin (HGB) level, and platelet (PLT) count on the right axis. Recovery of the WBC count, NEUT count, HGB level, and PLT count and a decrease or disappearance of the peripheral blood BLA count were observed after each of the three infections, which persisted for several months. (* indicates the time point of disease diagnosis by bone marrow examination) (AZM azithromycin, EB ethambutol, MEPM meropenem, RFP rifampicin, VRCZ voriconazole)
Discussion and conclusions
We observed three spontaneous remissions associated with clinical infectious diseases in an 80-year-old woman with AML. In each infectious episode, AML ameliorated without any intervention with cytotoxic or molecularly targeted agents. The depth of remission was determined by the decrease in the detection of specific del(5q) clone in cells from 6/20 cells at the onset to 1/20 cells after three infectious episodes. Overall, the spontaneous remissions led to a longer progression-free survival than the median survival time of end-stage AML (2 months). In each episode, the remission status was maintained for 3–5 months, resulting in a total progression-free survival of > 2 years with the help of effective supportive care [7]. The case progression clinically proved infection-related spontaneous remission of AML in response to infection by three different pathogen types: Mycobacterium avium (mycobacterium), Aspergillus (fungus), and E. coli (bacteria).
There have been multiple reports of various infectious diseases ameliorating AML [8, 9]. In our case, systemic infections caused by three different pathogens exerted an antileukemic effect. These antitumor effects may be caused by cell-mediated immunity, cytokines, and growth factors [10,11,12,13,14]. The cytotoxic effects of NK cells [11] and cytotoxic T lymphocytes, which are involved in innate and acquired immunity respectively, are the main contributors to the remission of AML in response to infection [10]. The second most common contributors to the antileukemic effect of infectious diseases are inflammatory cytokines, such as IL-1, IL-6, IL-2, and TNF-α [12, 13]. Some reports have also revealed that G-CSF and GM-CSF exert an antileukemic effect under specific conditions [14].
Although natural remission of AML can be confirmed through genetic or molecular biological analyses, it is a temporary phenomenon [5, 9, 15]. This is because patients with spontaneous remission of AML experience relapse repeatedly without absolute disease resolution. Some genomic analyses have revealed the presence of residual AML clones during spontaneous remission [16, 17]. A clonal study showed that leukemic cells continue to undergo clonal evolution during spontaneous remission [16]. Residual clones may cause AML relapse; however, little is known about the acquisition of resistance by these clones after spontaneous remission. In our case, the molecular maker del(5q) was used for assessing residual diseases. In general, such molecular makers are useful for estimating the depth of remission. No studies have reported an association between spontaneous remission and specific chromosomal abnormality or genetic mutation. However, the deletion (5q) karyotype in MDS is considered a good risk feature. Immunotherapy such as lenalidomide treatment [18] and hematopoietic stem cell transplantation [19] may provide a better response.
With this scientific background, infectious immunity may exert a better effect in MDS. Finally, a sequential antileukemic effect was repeatedly observed over a brief period (20 months). This suggests that an innate or cytokine effect is durable under certain conditions. Interestingly, a previous report proposed that the preleukemic state is observed in older normal individuals and preleukemic remission can occur shortly after chemotherapy [17]. This model suggests the reversion of AML to a preleukemic state during the natural remission period and its conversion to complete leukemia after the diminishing of the immunologic antileukemic effect. According to this model, chronic infection can ameliorate AML temporarily but not permanently.
In conclusion, the patient in our case showed repeated spontaneous remission of AML due to various infectious diseases. The immunological effects of the infectious diseases causing these remissions were clinically confirmed by the decrease in specific chromosomally aberrant clones.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- AML:
-
Acute myeloid leukemia
- MRC:
-
Myelodysplasia-related changes
- NTM:
-
Non-tuberculous Mycobacterium
- SR:
-
Spontaneous regression
References
Estey E, Döhner H. Acute myeloid leukaemia. Lancet. 2006;368(9550):1894–907. https://doi.org/10.1016/S0140-6736(06)69780-8.
Paul R, Remes K, Lakkala T, Pelliniemi TT. Spontaneous remission in acute myeloid leukaemia. Br J Haematol. 1994;86(1):210–2. https://doi.org/10.1111/j.1365-2141.1994.tb03281.x.
Rashidi A, Fisher SI. Spontaneous remission of acute myeloid leukemia. Leuk Lymphoma. 2015;56(6):1727–34. https://doi.org/10.3109/10428194.2014.970545.
Coley WB. Treatment of inoperable malignant tumors with toxins of erysipelas and the Bacillus prodigiosus. Trans Am Surg Assoc. 1984;12:183–212.
Fozza C, Bellizzi S, Bonfigli S, Campus PM, Dore F, Longinotti M. Cytogenetic and hematological spontaneous remission in a case of acute myelogenous leukemia. Eur J Haematol. 2004;73(3):219–22. https://doi.org/10.1111/j.1600-0609.2004.00281.x.
Menzin J, Lang K, Earle CC, Kerney D, Mallick R. The outcomes and costs of acute myeloid leukemia among the elderly. Arch Intern Med. 2002;162(14):1597–603. https://doi.org/10.1001/archinte.162.14.1597.
Yoshida C, Kondo T, Ito T, Kizaki M, Yamamoto K, Miyamoto T, Morita Y, Eto T, Katsuoka Y, Takezako N, Uoshima N, Imada K, Ando J, Komeno T, Mori A, Ishikawa Y, Satake A, Watanabe J, Kawakami Y, Morita T, Taneike I, Nakayama M, Duan Y, Garbayo Guijarro B, Delgado A, Llamas C, Kiyoi H. Real-world treatment patterns and clinical outcomes in patients with AML in Japan who were ineligible for first-line intensive chemotherapy. Int J Hematol. 2022;116(1):89–101. https://doi.org/10.1007/s12185-022-03334-8.
Hoption Cann SA, van Netten JP, van Netten C. Dr William Coley and tumour regression: a place in history or in the future. Postgrad Med J. 2003;79(938):672–80.
Müller CI, Trepel M, Kunzmann R, Lais A, Engelhardt R, Lübbert M. Hematologic and molecular spontaneous remission following sepsis in acute monoblastic leukemia with translocation (9;11): a case report and review of the literature. Eur J Haematol. 2004;73(1):62–6. https://doi.org/10.1111/j.1600-0609.2004.00248.x.
Spadea A, Latagliata R, Martinelli E, Concetta PM. Transient spontaneous remission in a case of adult acute myelogenous leukaemia. Br J Haematol. 1990;76(1):154. https://doi.org/10.1111/j.1365-2141.1990.tb07856.x.
Müller-Schmah C, Solari L, Weis R, Pfeifer D, Scheibenbogen C, Trepel M, May AM, Engelhardt R, Lübbert M. Immune response as a possible mechanism of long-lasting disease control in spontaneous remission of MLL/AF9-positive acute myeloid leukemia. Ann Hematol. 2012;91(1):27–32. https://doi.org/10.1007/s00277-011-1332-y.
Kleef R, Jonas WB, Knogler W, Stenzinger W. Fever, cancer incidence and spontaneous remissions. Neuroimmunomodulation. 2001;9(2):55–64. https://doi.org/10.1159/000049008.
Musto P, D’Arena G, Melillo L, Cascavilla N, La Sala A, Ladogana S, Carotenuto M. Spontaneous remission in acute myeloid leukaemia: a role for endogenous production of tumour necrosis factor and interleukin-2? Br J Haematol. 1994;87(4):879–80. https://doi.org/10.1111/j.1365-2141.1994.tb06761.x.
Nimubona S, Grulois I, Bernard M, Drénou B, Godard M, Fauchet R, Lamy T. Complete remission in hypoplastic acute myeloid leukemia induced by G-CSF without chemotherapy: report on three cases. Leukemia. 2002;16(9):1871–3. https://doi.org/10.1038/sj.leu.2402592.
Maywald O, Buchheidt D, Bergmann J, Schoch C, Ludwig WD, Reiter A, Hastka J, Lengfelder E, Hehlmann R. Spontaneous remission in adult acute myeloid leukemia in association with systemic bacterial infection-case report and review of the literature. Ann Hematol. 2004;83(3):189–94. https://doi.org/10.1007/s00277-003-0741-y.
Grunwald VV, Hentrich M, Schiel X, Dufour A, Schneider S, Neusser M, Subklewe M, Fiegl M, Hiddemann W, Spiekermann K, Rothenberg-Thurley M, Metzeler KH. Patients with spontaneous remission of high-risk MDS and AML show persistent preleukemic clonal hematopoiesis. Blood Adv. 2019;3(18):2696–9. https://doi.org/10.1182/bloodadvances.2019000265.
Koeffler HP, Leong G. Preleukemia: one name, many meanings. Leukemia. 2017;31(3):534–42. https://doi.org/10.1038/leu.2016.364.
Kelaidi C, Eclache V, Fenaux P. The role of lenalidomide in the management of myelodysplasia with del 5q. Br J Haematol. 2008;140(3):267–78. https://doi.org/10.1111/j.1365-2141.2007.06910.x.
Stewart B, Verdugo M, Guthrie KA, Appelbaum F, Deeg HJ. Outcome following haematopoietic cell transplantation in patients with myelodysplasia and del (5q) karyotypes. Br J Haematol. 2003;123(5):879–85. https://doi.org/10.1046/j.1365-2141.2003.04713.x.
Acknowledgements
Not applicable.
Funding
This work was supported by internal funding, JSPS KAKENHI Grant Numbers JP19K17927 and JP22K06768. The funder’s role was academic financial support. The funder had no role in the design and conduct of the study. We don’t have any other financial relationships to disclose.
Author information
Authors and Affiliations
Contributions
OI, TI and HF managed the patient’s case, contributed to the literature search, and wrote the manuscript. JK and MU made substantial contributions to the concept and design of this report. HF qualified the patient’s data, suggested important intellectual content. HF and NK took part in critical discussions. MU was involved in supervision of the manuscript and managed the research. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We obtained approval from the Kagawa University Hospital Institutional Review Board (H23-023). This research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The subject have given their written informed consent to publish their case (including publication of images).
Consent for publication
Written informed consent was obtained from the patients for publication of this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Imataki, O., Ishida, T., Kida, Ji. et al. Repeated spontaneous remission of acute myeloid leukemia in response to various infections: a case report. BMC Infect Dis 23, 215 (2023). https://doi.org/10.1186/s12879-023-08108-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08108-z