Abstract
Background
Several prolonged typhoid fever epidemics have been reported since 2010 throughout eastern and southern Africa, including Malawi, caused by multidrug-resistant Salmonella Typhi. The World Health Organization recommends the use of typhoid conjugate vaccines (TCVs) in outbreak settings; however, current data are limited on how and when TCVs might be introduced in response to outbreaks.
Methodology
We developed a stochastic model of typhoid transmission fitted to data from Queen Elizabeth Central Hospital in Blantyre, Malawi from January 1996 to February 2015. We used the model to evaluate the cost-effectiveness of vaccination strategies over a 10-year time horizon in three scenarios: (1) when an outbreak is likely to occur; (2) when an outbreak is unlikely to occur within the next ten years; and (3) when an outbreak has already occurred and is unlikely to occur again. We considered three vaccination strategies compared to the status quo of no vaccination: (a) preventative routine vaccination at 9 months of age; (b) preventative routine vaccination plus a catch-up campaign to 15 years of age; and (c) reactive vaccination with a catch-up campaign to age 15 (for Scenario 1). We also explored variations in outbreak definitions, delays in implementation of reactive vaccination, and the timing of preventive vaccination relative to the outbreak.
Results
Assuming an outbreak occurs within 10 years, we estimated that the various vaccination strategies would prevent a median of 15–60% of disability-adjusted life-years (DALYs). Reactive vaccination was the preferred strategy for WTP values of $0–300 per DALY averted. For WTP values > $300, introduction of preventative routine TCV immunization with a catch-up campaign was the preferred strategy. Routine vaccination with a catch-up campaign was cost-effective for WTP values above $890 per DALY averted if no outbreak occurs and > $140 per DALY averted if implemented after the outbreak has already occurred.
Conclusions
Countries for which the spread of antimicrobial resistance is likely to lead to outbreaks of typhoid fever should consider TCV introduction. Reactive vaccination can be a cost-effective strategy, but only if delays in vaccine deployment are minimal; otherwise, introduction of preventive routine immunization with a catch-up campaign is the preferred strategy.
Similar content being viewed by others
Introduction
Typhoid fever is a major source of morbidity and mortality in developing countries. Approximately 10–20 million cases and 100,000–200,000 deaths are attributed to typhoid fever each year [1, 2], accounting for 3.86–13.90 million disability-adjusted life years (DALYs) [2, 3]. Since 2010, there have been several prolonged typhoid outbreaks in eastern and southern Africa, which have imposed considerable costs to the populations impacted [4,5,6,7]. These outbreaks are associated with the emergence of antimicrobial-resistant (AMR) strains and, as a result, more outbreaks are likely as resistance spreads [4, 7, 8].
Typhoid conjugate vaccines (TCVs) are an effective means of typhoid prevention and control with the goal of reducing the burden and spread of typhoid fever [9,10,11]. They have been approved and recommended by the World Health Organization (WHO) and Gavi (the Vaccine Alliance) has pledged support for introduction of TCVs in typhoid-endemic countries. At its April 2022 meeting, the WHO Strategic Advisory Group of Experts on Immunization (SAGE), acknowledged new data demonstrating high efficacy and effectiveness of a single dose of TCV across diverse settings and reaffirmed the current recommendations for TCV use. Likewise, limited data from Harare, Zimbabwe support declines in typhoid cases following TCV use for outbreak control [12]. The vaccine’s short-term efficacy against infection and disease has been shown [9,10,11], but research regarding its longer-term efficacy and role in reducing transmission is still underway [9, 11]. Current data are limited on how and when TCVs should be introduced, and TCV stockpiles do not yet exist [13, 14].
Reactive vaccination has become an important prevention measure for outbreaks of diseases such as cholera, influenza, and Ebola [15,16,17,18,19,20,21,22]. While reactive vaccination can be effective, the impact will be small if implemented late or focused inappropriately on less vulnerable populations [15, 19, 20]. Although TCVs are recommended by the WHO for use in outbreak settings, there is no specific guidance on how to define the start of an outbreak of typhoid fever in order to trigger a reactive vaccination response. Furthermore, policymakers are faced with inevitable delays in securing TCVs for outbreak response and applying for Gavi support to implement routine vaccination. While preventative introduction of TCVs in low-incidence settings is unlikely to be cost-effective in the absence of outbreaks [23, 24], it may help to prevent future outbreaks of typhoid fever associated with introduction of AMR strains. Hence, it is necessary to evaluate the cost-effectiveness of preventative versus reactive vaccination strategies in the presence and absence of outbreaks of typhoid fever.
Here, we use a dynamic transmission model fitted to data from a typhoid fever outbreak in Blantyre, Malawi to investigate the health impact, costs, and cost-effectiveness of alternative vaccine delivery strategies and to inform the use of TCVs in an outbreak setting. We explored a range of preventative and reactive vaccination scenarios to examine the robustness of our findings in the face of uncertainty in outbreak timing, outbreak identification, and delays in vaccine introduction.
Methods
Transmission model and outbreak threshold
We developed an age-specific stochastic model to simulate typhoid fever transmission dynamics in Blantyre, Malawi from January 1995 to December 2031. The time-horizon includes a long pre-outbreak period, the outbreak itself (which peaked in 2013), and a sufficiently long post-outbreak period to account for relevant population-level impacts of vaccination. Details of the model are provided in the Additional file 1. The model was parameterized based on the equivalent deterministic model fitted to routine blood-culture surveillance data from Queen Elizabeth Central Hospital (QECH) in Blantyre from January 1996 to February 2015 [8], which captures the multi-year outbreak of typhoid fever that occurred in Blantyre between 2011 and 2015. We assumed the outbreak was caused by an increase in the duration of infectiousness of Salmonella Typhi associated with the emergence of the multidrug-resistant H58 haplotype [8, 25]. We estimated the pre-outbreak basic reproductive number (R0), timing and magnitude of increase in the duration of infectiousness, amplitude of seasonality in transmission, and relative infectiousness of chronic carriers by fitting to age-stratified data on the number of weekly culture-confirmed typhoid fever cases at QECH; the remaining model parameters were fixed based on data from the literature (see Table 1). We validated the model by comparing it to blood-culture surveillance data from QECH for March 2015 to December 2016. To scale the number of blood-culture-confirmed cases at QECH to the population-based incidence of typhoid fever in Blantyre, we used data from the recently completed Strategic Typhoid Alliance across Africa and Asia (STRATAA) cohort study (Additional file 1: S1.1.4 Text) [26].
Stochastic model projections of the number of typhoid fever cases through time incorporated uncertainty in the transmission dynamics using a Poisson process for each transition between states and a binomial observation process for the (under)reporting of cases over the duration of an individual’s infection. To simulate the impact of vaccination, we incorporated further uncertainty in vaccine efficacy at time 0, the waning of vaccine-induced immunity, and vaccine coverage during the catch-up campaign by sampling from the associated uncertainty distribution for each stochastic iteration (Additional file 1: S1 Text). We assumed vaccination protects against both infection and disease. The dynamic model parameters, their estimates and uncertainty distributions, and sources are listed in Table 1. When possible, we used parameter values estimated in previous studies, noted in Table 1. For other parameters, the estimation methods are unique to each parameter and are described in more detail in the supplement. For each intervention strategy, we simulated the outbreak 1000 times.
Since there is no globally-defined threshold for a typhoid fever outbreak, we explored different definitions of the epidemic threshold. For the purposes of our analysis and to facilitate outbreak identification from passive hospital-based surveillance data across different populations and contexts, we specified the epidemic threshold in terms of the number of standard deviations (SD) above the mean monthly reported typhoid fever cases for the baseline period of 2000–2010. We examined thresholds ranging from 6 to 16 SD above the mean, and defined the “true” start of the outbreak as April 10, 2011, identified during model-fitting. For reference, this corresponded to a range of approximately 10–25 typhoid fever cases per month above the monthly mean of approximately 1.4 cases per month in this setting. Setting a threshold too low would trigger too many false positive identifications of the outbreak, while setting the threshold too high could fail to identify a true outbreak in a timely manner. To address this issue, we compared the sensitivity and specificity of each outbreak definition. We defined the sensitivity of each threshold as the percentage of simulations in which the outbreak was identified within 18 months of April 2011, while the specificity was defined as the percentage of simulations in which the outbreak threshold was not exceeded prior to April 2011. Once the outbreak threshold was crossed, all subsequent months were considered to be part of the outbreak. For our primary analysis, we used the outbreak identification threshold that yielded the highest sum of sensitivity and specificity.
Vaccination scenarios
We considered three scenarios under the assumption that a country has not yet implemented routine vaccination: (1) an outbreak is likely to occur over the next 10 years; (2) an outbreak is unlikely to occur (and hence, the country maintains the same pre-outbreak seasonal incidence); and (3) an outbreak has already occurred and is unlikely to happen again (and hence, the country has a higher incidence post-outbreak compared to pre-outbreak). The most likely scenario depends on the recent history of typhoid incidence and that of nearby regions. If surrounding regions have been experiencing outbreaks but the country has not yet had one, we assume that it is likely that an outbreak will occur at some point within the next 10 years (Scenario 1). For this scenario, we randomized the timing of the start of the outbreak to follow a uniform distribution over Years 0–10; we assumed only a single outbreak occurs. However, if surrounding regions are not experiencing outbreaks, it may be unlikely that an outbreak would occur (Scenario 2). If an outbreak has already occurred, as it did in Malawi, we assume another outbreak is unlikely within the next 10 years (Scenario 3).
Because the outbreak in Malawi was driven by the emergence of multi-drug resistance, typhoid incidence under the Scenario 3 (post-outbreak) is higher than the incidence under Scenario 2 (pre-outbreak). For Scenario 2, we assume typhoid fever incidence is comparable to that estimated for Blantyre for 1995–2005, whereas for Scenario 3, we assume it is comparable to that predicted for Blantyre for 2021–2031. These scenarios are comparable to previous cost-effectiveness analyses and allow us to examine whether it would be beneficial to introduce TCV in an endemic setting when typhoid fever incidence is lower (Scenario 2: pre-outbreak) or higher (Scenario 3: post-outbreak).
We simulated four alternative vaccination strategies, following previous cost-effectiveness analyses of TCV strategies and the current WHO recommendation in endemic settings [14, 23, 24, 31]: no vaccination (base case), preventive routine TCV introduction at 9 months of age (in Year 0), preventive routine vaccination plus a one-time catch-up to age 15 (also in Year 0), and (for Scenario 1 only) reactive routine vaccination plus a catch-up campaign to age 15 once the outbreak was identified (Table 2). Vaccine efficacy parameters (including the initial vaccine efficacy and exponential rate of waning immunity) were estimated by fitting to data from a phase 3, double-blind, randomized active-controlled clinical trial of single-dose Typbar TCV in Blantyre, Malawi [9, 23] (Table 1, Additional file 1: S1.1.2.2 Text, Fig. S2). Routine vaccination coverage was assumed to increase from 85 to 95% over the first ten years of vaccination and then remain at 95% [23]. For catch-up campaign coverage, we varied the proportion vaccinated uniformly from 60 to 90%.
Economic evaluation
To measure disease burden and hence identify vaccination strategies that most effectively reduce the burden of typhoid fever in this setting, we calculated disability-adjusted life-years (DALYs) due to typhoid fever. The stochastic model output for the number of typhoid fever cases and vaccine doses administered per 100,000 people under each strategy was used to calculate the DALYs due to typhoid, costs of treatment, and costs of vaccine delivery. Costs of vaccination programs are generally incurred by the government and donors in Malawi; hence, we considered the healthcare system perspective and only accounted for direct treatment and vaccination costs accrued by the healthcare system. Costs were converted to 2020 USD. We conducted the analysis in accordance with WHO guidelines and recommendations of the Bill and Melinda Gates Foundation’s reference case [32,33,34,35]. All costs and effects were discounted at a rate of 3% per year. The analysis adheres to the Consolidated Health Economic Evaluation Reporting Standards (CHEERS), where applicable [32] (Additional file 1: S3 Text).
Consistent with WHO guidelines and recommendations of the Bill and Melinda Gates Foundation’s reference case [32,33,34,35], we evaluated the effectiveness of each strategy in terms of DALYs. DALYs represent the total years of life lost due to death (YLL) and lived with disability (YLD) due to the disease: \(DALY=YLL+YLD\) [36]. To estimate the YLLs due to typhoid fever, we multiplied the number of cases of typhoid fever by the probability of hospitalization and the probability of death for inpatients (Additional file 1: S1.2.6 Text) [37, 38]. We then divided by the proportion of deaths occurring in hospital, which we assumed was uniformly distributed between 0.25–1 [23], to obtain an estimate of the total number of deaths, and subtracted the average age of death from typhoid fever from Malawi’s life expectancy [39]. The YLDs were calculated based on the number of cases, duration of illness, and disability weights (Additional file 1: S1.2.3 Text).
To estimate the treatment costs for typhoid fever, we assumed 71% (95% CrI: 64–77%) of typhoid fever cases would seek medical care and 4% (95% CrI: 1–11%) would be hospitalized; we updated prior distributions for these parameters based on data from the STRATAA cohort study [26] (Table 3; Additional file 1: S1.2.4–1.2.5 Texts). The number of outpatient cases was calculated by subtracting the number of hospitalized cases from the number of individuals seeking care. We assumed cases not seeking medical care would not incur treatment costs. We estimated treatment costs for typhoid fever using a recent cohort study on treatment costs for typhoid fever in Blantyre, Malawi [40].
Antimicrobial resistance is likely to affect the burden and costs associated with typhoid fever. In the absence of sufficient data to parameterize the relative burden and costs of AMR typhoid fever, we assumed the case fatality risk, years of life lived with disability, and treatment costs were twice as high on average (uniformly 1–3 times higher) for AMR cases. Since recent outbreaks are thought to be caused by new AMR strains of typhoid, we allowed the proportion of AMR typhoid cases to vary with time based on data from a longitudinal study in Blantyre (Additional file 1: S1.2.7 Text) [25].
In our analysis, we included only the costs to be paid by the government of Malawi (i.e. accounting for Gavi support), assuming Malawi remains in the initial self-financing phase of Gavi support. Thus, we assumed a vaccine procurement cost of $0.20 per routine dose and $0 for campaign doses ($1.50/dose prior to Gavi support) (Table 3; Additional file 1: S1.2.2 Text). We also accounted for Gavi support for the delivery of routine doses in the first year of vaccination ($0.80/dose). All costs were adjusted for inflation to 2020 USD.
Sensitivity analyses
To assess the robustness of our economic evaluation to the underlying parameter uncertainty, we accounted for uncertainty with probabilistic sensitivity analysis and explored its impact in two ways: (1) we examined cost-effectiveness acceptability frontiers to assess how parameter uncertainty contributes to uncertainty in the optimal strategy; (2) value of information analysis to identify the most influential parameters and to inform if it is worth delaying the decision in anticipation of better information at a later date, by estimating the expected value of partially perfect information (EVPPI) for each parameter with the one-level method devised by Strong and Oakley [45].
We randomly drew 5000 independent samples from the uncertainty distributions of each input parameter in the economic evaluation (Additional file 1: Table S2). Each sample was combined with one of the samples from the stochastic transmission model (1000 simulations repeated five times to achieve a manageable computational burden) to estimate 5000 net monetary benefit (NMB) values for each strategy and for a range of willingness-to-pay (WTP) values from $0–$1000 in increments of $10. The NMB is calculated as \(NMB=\Delta E*WTP-\Delta C\), where \(\Delta E\) is the DALYs averted by each vaccination strategy compared to the base case of no vaccination, \(\Delta C\) is the incremental cost of the vaccination strategy compared to the base case, and WTP is the willingness-to-pay threshold. We quantified the uncertainty surrounding the optimal strategy by calculating the proportion of samples for which a strategy yielded the highest NMB for each WTP. We also measured the contribution of each input parameter to the uncertainty around the optimal vaccination strategy by calculating the EVPPI.
Scenario analyses
While countries have the option of introducing TCVs into the routine immunization program, to date no vaccine stockpile exists for TCV introduction in the event of an outbreak.
To address this uncertainty, we account for varying delays in reactive vaccine deployment. For our primary analysis, we assumed an “idealized” scenario in which vaccination is introduced within 1 month of identifying the outbreak. In scenario analyses, we explored deployment delays of 6, 12, and 24 months after the epidemic threshold was exceeded.
The optimal strategy may also depend on how long until the outbreak occurs. We examined scenarios in which TCV introduction occurs exactly 10 years or 1 year before the epidemic threshold is crossed. For this comparison, we assessed the burden of typhoid fever and costs of treatment and vaccination for the preventative and reactive vaccination scenarios over a 20-year time horizon spanning from 2000 to 2020. For all other analyses, we used the same 10-year time horizon to match previous cost-effective analyses.
A previous cost-effectiveness analysis of TCVs used WHO-CHOICE data for cost-of-illness estimates [23, 46]. Since the Malawi-specific cost-of-illness estimates used in this analysis were higher, we additionally evaluated the cost-effectiveness of the idealized scenario using the previous WHO-CHOICE cost-of-illness estimates.
The stochastic transmission model and economic model were implemented in R version 3.4.0 [47]. The transmission model code is available on GitHub at https://github.com/mailephillips/typhoid_outbreak_Malawi.
Results
The model accurately reproduced the number and age distribution of observed blood-culture confirmed typhoid fever cases at QECH during both the fitting period (January 1996–February 2015) and the validation period (March 2015–December 2016) (Additional file 1: Figs. S5, S6). Over the 10-year simulation period with randomized outbreak timing (Scenario 1), we estimated a median of 1989 (95% CrI: 210–3508) cases and 18 (95% CrI: 1–145) deaths per 100,000 people for a total of 398 (95% CrI: 21–3109) DALYs and $126,754 (95% CrI: 9267–290,227) in treatment costs per 100,000 people for typhoid fever under the no vaccination strategy (Additional file 1: Table S3).
All vaccination strategies substantially reduced the expected number of typhoid fever cases, but did not completely prevent an outbreak from occurring. Preventive routine vaccination with a catch-up campaign delayed the start of the outbreak and reduced typhoid fever incidence substantially more than routine vaccination alone. When reactive vaccination was deployed within 1 to 6 months of the outbreak threshold being crossed, the epidemic was substantially smaller and delayed by 1–2 years (Additional file 1: Fig S8). However, when reactive vaccination occurred 12 to 24 months after the outbreak was identified, it failed to prevent the peak in typhoid fever cases, although incidence was substantially reduced after vaccine deployment. The number of typhoid fever cases, deaths, and DALYs averted by each vaccination strategy compared to no vaccination, as well as the associated costs, are detailed in Additional file 1: Table S4.
Under Scenario 1, our findings suggest that TCV introduction was cost-effective compared to no vaccination for all WTP values above $0 (Table 4 and Fig. 1B). Reactive vaccination (with a 1-month delay in implementation) was cost-saving, with estimated total costs averted of $17,147 (95% CrI: − $3500–$65,080) per 100,000 people. Reactive vaccination was preferred for a WTP range of $0–$307 (dominating the base case of no vaccination), whereas preventive routine vaccination with a catchup campaign was optimal for WTP values above $307. Routine vaccination including a catch-up campaign to 15 years of age was always preferred over routine vaccination alone.
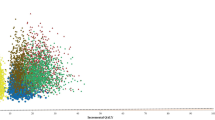
Cost-effectiveness planes and acceptability frontiers. The cost-effectiveness planes (left) and cost-effectiveness acceptability frontiers (CEAFs; right) are plotted for A, B Scenario 1 (randomized outbreak timing), C, D Scenario 2 (no outbreak), and E, F Scenario 3 (outbreak has already occurred). In the cost-effectiveness planes, each dot represents the incremental costs (in 2020 USD) and DALYs averted for one simulation when compared with the base case of no vaccination. The bold Xs denote the expected additional cost and DALYs averted for each vaccination strategy with respect to no vaccination. Strategies are indicated by the color of the dot or X (purple: preventive routine vaccination; green: preventive routine vaccination plus a catch-up campaign up to age 15; or orange: reactive routine vaccination plus a catch-up campaign to age 15—for Scenario 1 only). In the CEAFs, the preferred strategy (i.e. the strategy that yielded the highest average net benefit) for each willingness-to-pay threshold ($0–1000 per DALY averted; x-axis, 2020 USD) is indicated by the color of the line (black: no vaccination; and same strategy colors as other panels), while the proportion of samples in which that strategy yielded the highest net benefit is indicated by the value on the y-axis; this can be interpreted as our certainty in the optimal strategy
If no outbreak occurs (Scenario 2, assuming the lower pre-outbreak incidence), no vaccination is the preferred strategy for all WTP thresholds < $902 (Fig. 1D). If the outbreak has already occurred (Scenario 3, assuming the higher post-outbreak incidence), routine vaccination with a catch-up campaign is preferred for WTP values of $150 or higher (Fig. 1F). Again, routine vaccination alone is never the preferred strategy. The number of typhoid fever cases, deaths, and DALYs averted, as well as the costs for each scenario, are presented in Additional file 1: Table S4.
The WTP threshold at which the preferred strategy switches from reactive vaccination to preventative vaccination decreased as the delay in TCV deployment for the reactive vaccination strategy increased (Fig. 2). For a 6-month delay, reactive vaccination was the preferred strategy for WTP thresholds between $0–190 per DALY averted (Fig. 2A), while for a 12-month delay, reactive vaccination was preferred at $0–60 per DALY averted (Fig. 2B). If the delay extended up to 24 months, reactive vaccination was never preferred; preventative vaccination with a catch-up campaign was the optimal strategy when the WTP threshold was at least $10 per DALY averted; this was the only scenario in which no vaccination was ever preferred (for a WTP of $0 per DALY averted) (Fig. 2C).
Cost-effectiveness acceptability frontiers for Scenario 1 with varying delays in reactive vaccination. The cost-effectiveness acceptability frontiers for Scenario 1 (randomized outbreak timing) are shown for a range of willingness-to-pay thresholds ($0–1000; x-axis, 2020 USD for A a 6-month delay in reactive vaccination after the outbreak threshold is exceeded, B a 12-month delay in reactive vaccination after the outbreak threshold is exceeded, and C a 24-month delay in reactive vaccination after the outbreak threshold is exceeded. The preferred strategy (i.e. the strategy that yielded the highest average net benefit) is indicated by the color of the line (black: no vaccination; purple: preventive routine vaccination; green: preventive routine vaccination plus a catchup campaign up to 15 years; or orange: reactive routine vaccination plus a catchup campaign), while the proportion of samples in which that strategy yielded the highest net benefit is indicated by the value on the y-axis (which can be interpreted as our certainty in the optimal strategy)
The optimal vaccination strategy did not vary substantially depending on how long before the outbreak preventive vaccination was implemented. Whether the outbreak occurred within 10 years or 1 year of vaccine introduction for the preventive strategies, the preferred strategy remained essentially the same (Additional file 1: Fig S10).
When using WHO-CHOICE instead of Blantyre-specific cost of illness data, the probability that a particular vaccination strategy was preferred followed a similar pattern. However, since the WHO-CHOICE costs were lower compared to the Blantyre-specific costs, the willingness-to-pay thresholds at which different vaccination strategies were preferred was shifted approximately $100 higher (Additional file 1: Fig S11). For example, under Scenario 1 using the WHO-CHOICE cost of illness data, TCV introduction was optimal compared to no vaccination for WTP values greater than $100 (Additional file 1: Table S5 and Fig. S11B). Reactive vaccination (with a 1-month delay in implementation) was preferred for a WTP range of $110–$430, whereas preventive routine vaccination with a catch-up campaign was optimal for WTP values above $430. Routine vaccination alone was never the preferred strategy.
For all of the economic evaluations, uncertainty around the probability of death among inpatients contributed most to uncertainty in the preferred strategy, followed by the probability of hospitalization, percentage of deaths occurring among hospitalized patients, and routine vaccine delivery costs (Additional file 1: Figs. S12–S14).
Discussion
Multi-year outbreaks of typhoid fever have occurred in numerous settings following the introduction of AMR strains. In countries where typhoid incidence is low and antimicrobial resistance is rare, but where surrounding countries in the region are experiencing outbreaks of drug-resistant typhoid fever, it is likely that AMR strains will spread, triggering further outbreaks. Our findings indicate that if an outbreak of typhoid fever is likely to occur within the next 10 years, introduction of TCVs with a catch-up campaign is likely to be cost-effective compared to no vaccination, and reactive vaccination may be cost saving if deployed within 12 months. However, if the WTP threshold is greater than $300 per DALY averted, it is generally better (in terms of cost-effectiveness) to preventively introduce routine vaccination with a catch-up campaign rather than waiting for the outbreak to occur. These findings hold true regardless of when the outbreak occurs, provided it occurs within 10 years.
As TCV stockpiles do not yet exist, there is uncertainty in how long it will take to mobilize vaccine introduction once an outbreak is identified. The cost-effectiveness of reactive vaccination largely depends on the length of delay in vaccine deployment. Decision-makers should try to realistically determine how quickly they would be able to identify a typhoid fever outbreak and mobilize resources to implement both routine TCV introduction and a catch-up campaign, and seek to minimize delays in vaccine deployment when considering reactive vaccination strategies. In settings that lack established platforms for blood culture surveillance and the resources to implement TCV campaigns within a year, preventative introduction of TCVs should be favored. Nevertheless, improved surveillance of typhoid fever is needed.
There is currently no threshold for defining and identifying outbreaks of typhoid fever across different settings. In a recent review of typhoid fever outbreaks occurring between 1989 and 2018, the number of reported cases ranged from 3 to 10,677 [48]. In our analysis, we found that an increase in the monthly number of blood-culture-confirmed typhoid fever cases of more than 15 standard deviations above the mean accurately identified the start of the outbreak in Blantyre, Malawi while avoiding false alarms due to normal seasonal variations. It is not yet clear whether this threshold may be applicable to other settings. However, the results of our analysis are unlikely to depend on the outbreak identification threshold used. While lower thresholds may falsely identify an outbreak before it occurs, a false alarm may not be problematic provided the outbreak still occurs. If the outbreak is falsely identified too early, “reactively” vaccinating in response to the false outbreak is comparable to a preventative vaccination strategy, which in our analysis was still cost-effective for WTP thresholds above $300, provided an outbreak occurs sometime within the next 10 years. Given the consequences of delaying outbreak response, it is preferable to err on the side of early (false) outbreak alarms. These findings are encouraging as typhoid resources and surveillance systems are often sub-optimal in areas where typhoid is endemic.
For scenarios in which an outbreak does not occur, our results are consistent with previous cost-effectiveness analyses, though with lower WTP thresholds where vaccination is preferred. Before the outbreak in Blantyre, we estimated that typhoid fever incidence was 26.1 cases (95% CrI: 14.0–45.7 cases) per 100,000 person-years, which represents a fairly limited health burden, with an average of only 14 culture-confirmed cases per year at QECH [25]. Under these circumstances, we found that no vaccination is the preferred strategy for WTP thresholds less than $900. In general, previous analyses have found that TCV introduction is unlikely to be cost-effective at WTP thresholds below $1000 when incidence is less than 30–50 cases per 100,000 person-years [23, 24, 31]. Similarly, we estimated that the post-outbreak incidence in Blantyre was 224 typhoid fever cases (95% CrI: 169–368 cases) per 100,000 person-years, and routine vaccination with a catch-up campaign was cost-effective at WTP thresholds of $150 and above, similar to results of a previous economic evaluation for Malawi [23]. Considering the likely cost-effectiveness for this current scenario, decision-makers in Malawi chose to introduce TCVs and applied for Gavi support in 2020.
Due to suboptimal surveillance and diagnostics, there is considerable uncertainty surrounding the incidence and burden of typhoid fever, which leads to uncertainty in the preferred vaccination strategy. Nevertheless, some of the uncertainty has been reduced in our analysis compared to previous cost-effectiveness analyses for Malawi. In Bilcke et al. [26], lack of data surrounding the probability of hospitalization, the case fatality risk among inpatients, vaccine delivery costs, and typhoid incidence contributed substantially to uncertainty in the cost-effectiveness of TCV introduction. Since then, additional data have been collected in Malawi [42, 49]. While the parameters contributing most to uncertainty in our analysis included parameters that were and were not updated with new data, the overall expected value of information for the parameters contributing the most to uncertainty was substantially lower compared to the previous cost-effectiveness analyses.
There are several important limitations to our analysis. We assume TCV reduces the burden of typhoid fever by reducing the number of infections and lowering transmission. However, we lack direct data on vaccination impact in this population. We used results from the recent TyVAC trial in Malawi to update our estimates of vaccine efficacy and duration of protection, but observations of vaccine impact following widespread implementation are not yet available. Additionally, the duration of vaccine protection is not fully understood. While we incorporated substantial uncertainty associated with this parameter in our analyses, longer follow-up is needed to validate our assumptions. This analysis also uses parameters and data based on an outbreak in one location. Since the timing of a typhoid fever outbreak is unknown, it is difficult to plan for control. The peak and length of outbreaks, as well as treatment costs and severity of disease, may differ in other contexts. It can also be difficult to collect site-specific data, as typhoid fever surveillance is limited in many countries. We made every effort to incorporate additional uncertainty in the model parameters (which were not only Malawi-specific) and the outbreak itself (using a stochastic model that varied the peak and length of the outbreak). The framework we present may be generalizable to other settings where the introduction of drug-resistant strains may lead to prolonged outbreaks of typhoid fever. However, we do not fully understand why outbreaks occur in some places but not others.
With WHO recommendations for TCV use, an increasing body of evidence supporting TCV efficacy in diverse settings, and studies assessing longer-term efficacy and impact underway, governments are looking to prioritize the allocation of resources to prevent typhoid fever. While for most endemic countries the introduction of TCV into routine immunization programs is the preferred option, studies are needed to compare prevention strategies across different settings, including the use of TCV in response to outbreaks. Findings from this analysis can play an essential role in making the case for vaccination in an outbreak setting to reduce the global burden of typhoid fever. However, typhoid control can be expensive, and the majority of the burden of typhoid fever occurs in low- and middle-income countries. Cost-effectiveness analyses are needed to inform decisions for the optimal allocation of funding. Results from this research can inform policy- and decision-making regarding typhoid prevention and control strategies by providing estimates of which strategies are most cost-effective compared to others under which circumstances.
Availability of data and materials
The data and code used for the dynamic model are available at https://github.com/mailephillips/typhoid-outbreak_Malawi.
References
Antillon M, Warren J, Crawford F, Weinberger D, Kurum E, Pitzer V. The burden of typhoid fever in low- and middle-income countries: a meta-regression approach. PLoS Negl Trop Dis. 2017. https://doi.org/10.1371/journal.pntd.0005376.
GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet (London, England). 2018;392(10159):1923–94. https://doi.org/10.1016/S0140-6736(18)32225-6.
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2016 (GBD 2016) Results. Seattle2017. http://ghdx.healthdata.org/gbd-results-tool.
Hendriksen RS, Leekitcharoenphon P, Lukjancenko O, Lukwesa-Musyani C, Tambatamba B, Mwaba J, et al. Genomic signature of multidrug-resistant salmonella enterica serovar typhi isolates related to a massive outbreak in Zambia between 2010 and 2012. J Clin Microbiol. 2015;53(1):262–72. https://doi.org/10.1128/jcm.02026-14.
Imanishi M, Kweza PF, Slayton RB, Urayai T, Ziro O, Mushayi W, et al. Household water treatment uptake during a public health response to a large typhoid fever outbreak in Harare, Zimbabwe. Am J Trop Med Hyg. 2014;90(5):945–54. https://doi.org/10.4269/ajtmh.13-0497.
Neil KP, Sodha SV, Lukwago L, O-Tipo S, Mikoleit M, Simington SD, et al. A large outbreak of typhoid fever associated with a high rate of intestinal perforation in Kasese District, Uganda, 2008–2009. Clin Infect Dis. 2012;54(8):1091–9. https://doi.org/10.1093/cid/cis025.
Gordon MA, Graham SM, Walsh AL, Wilson L, Phiri A, Molyneux E, et al. Epidemics of invasive Salmonella enterica serovar enteritidis and S. enterica Serovar typhimurium infection associated with multidrug resistance among adults and children in Malawi. Clin Infect Dis. 2008;46(7):963–9. https://doi.org/10.1086/529146.
Pitzer VE, Feasey NA, Msefula C, Mallewa J, Kennedy N, Dube Q, et al. Mathematical modeling to assess the drivers of the recent emergence of typhoid fever in Blantyre, Malawi. Clin Infect Dis. 2015;61:S251–8. https://doi.org/10.1093/cid/civ710.
Patel P, Patel P, Liang Y, Meiring J, Misiri T, Mwakiseghile F, et al. Safety and efficacy of a typhoid conjugate vaccine in Malawian children. N Engl J Med. 2021. https://doi.org/10.1056/NEJMoa2035916.
Shakya M, Voysey M, Theiss-Nyland K, Colin-Jones R, Pant D, et al. Efficacy of typhoid conjugate vaccine in Nepal: final results of a phase 3, randomised, controlled trial. Lancet Glob Health. 2021;9(11):E1561–8. https://doi.org/10.1016/S2214-109X(21)00346-6.
Qadri F, Khanam F, Liu X, Theiss-Nyland K, Biswas PK, Bhuiyan AI. Protection by vaccination of children against typhoid fever with a Vi-tetanus toxoid conjugate vaccine in urban Bangladesh: a cluster-randomised trial. Lancet (London, England). 2021;398(10301):675–84. https://doi.org/10.1016/S0140-6736(21)01124-7.
Olaru ID, Mtapuri-Zinyowera S, Feasey N, Ferrand RA, Kranzer K. Typhoid Vi-conjugate vaccine for outbreak control in Zimbabwe. Lancet (London, England). 2019;19:930.
Watson CH, Edmunds WJ. A review of typhoid fever transmission dynamic models and economic evaluations of vaccination. Vaccine. 2015;33:C42–54. https://doi.org/10.1016/S0022-5193(03)00031-6.
World Health Organization. Typhoid vaccines: WHO position paper, March 2018—Recommendations. Vaccine. 2019;37(2).
Azman AS, Lessler J. Reactive vaccination in the presence of disease hotspots. Proc Biol Sci. 2015. https://doi.org/10.1098/rspb.2014.1341.
Alberti KP, King LA, Burny ME, Ilunga BK, Grais RF. Reactive vaccination as an effective tool for measles outbreak control in measles mortality reduction settings, Democratic Republic of Congo, 2005–2006. Int Health. 2010;2(1):65–8. https://doi.org/10.1016/j.inhe.2009.12.009.
Tildesley MJ, Savill NJ, Shaw DJ, Deardon R, Brooks SP, Woolhouse MEJ, et al. Optimal reactive vaccination strategies for a foot-and-mouth outbreak in the UK. Nature. 2006;440(7080):83. https://doi.org/10.1038/nature04324.
Ciglenecki I, Sakoba K, Luquero FJ, Heile M, Itama C, Mengel M, et al. Feasibility of mass vaccination campaign with oral cholera vaccines in response to an outbreak in Guinea. PLoS Med. 2013;10(9): e1001512. https://doi.org/10.1371/journal.pmed.1001512.
Azman AS, Luquero FJ, Rodrigues A, Palma PP, Grais RF, Banga CN, et al. Urban cholera transmission hotspots and their implications for reactive vaccination: evidence from Bissau City, Guinea Bissau. PLoS Negl Trop Dis. 2012;6(11): e1901. https://doi.org/10.1371/journal.pntd.0001901.
Grais RF, Conlan AJK, Ferrari MJ, Djibo A, Menach AL, Bjørnstad ON, et al. Time is of the essence: exploring a measles outbreak response vaccination in Niamey, Niger. J R Soc Interface. 2008;5(8):67–74. https://doi.org/10.1098/rsif.2007.1038.
Rosado RM, Charles-Smith L, Daniel B. Control and cost-benefit analysis of fast spreading diseases: the case of ebola. Online J Public Health Inform. 2017. https://doi.org/10.5210/ojphi.v9i1.7584.
Minetti A, Hurtado N, Grais RF, Ferrari M. Reaching hard-to-reach individuals: nonselective versus targeted outbreak response vaccination for measles. Am J Epidemiol. 2019;179(2):245–51. https://doi.org/10.1093/aje/kwt236.
Bilcke J, Antillon M, Pieters Z, Kuylen E, Abboud L, Neuzil KM, et al. Cost-effectiveness of routine and campaign use of typhoid Vi-conjugate vaccine in Gavi-eligible countries: a modelling study. Lancet Infect Dis. 2019;19(7):728–39. https://doi.org/10.1016/S1473-3099(18)30804-1.
Lo N, Gupta R, Stanaway J, Garrett D, Bogoch I, Luby S, et al. Comparison of strategies and incidence thresholds for vi conjugate vaccines against typhoid fever: a cost-effectiveness modeling study. J Infect Dis. 2018. https://doi.org/10.1093/infdis/jix598.
Feasey N, Gaskell K, Wong V, Msefula C, Selemani G, Kumwenda S, et al. Rapid emergence of multidrug resistant, H58-lineage Salmonella Typhi in Blantyre, Malawi. PLOS Negl Trop Dis. 2015;9(4): e0003748. https://doi.org/10.1371/journal.pntd.0003748.
Phillips MT, Meiring JE, Voysey M, Warren JL, Baker S, Basnyat B, et al. A Bayesian approach for estimating typhoid fever incidence from large-scale facility-based passive surveillance data. Stat Med. 2021;40(26):5853–70. https://doi.org/10.1002/sim.9159.
United Nations Department of Economic and Social Affairs. World Population Prospects, the 2012 Revision [Report]. 2013 [updated 2013]. https://www.un.org/en/development/desa/publications/world-population-prospects-the-2012-revision.html.
Hornick RB, Greisman SE, Woodward TE, DuPont HL, Dawkins AT, Snyder MJ. Typhoid fever: pathogenesis and immunologic control (part 1). N Engl J Med. 1970;1970(283):686–91. https://doi.org/10.1056/NEJM197009242831306.
Ames WR, Robins M. Age and sex as factors in the development of the typhoid carrier state, and a method for estimating carrier prevalence. Am J Public Health Nations Health. 1943;33(3):221–30.
Crump JA, Luby SP, Mintz ED. The global burden of typhoid fever. Bull World Health Organ. 2004;82(5):346–53.
Antillon M, Bilcke J, Paltiel AD, Pitzer VE. Cost-effectiveness analysis of typhoid conjugate vaccines in five endemic low- and middle-income settings. Vaccine. 2017;35(27):3506–14. https://doi.org/10.1016/j.vaccine.2017.05.001.
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. 2013. https://doi.org/10.1136/bmj.f1049.
World Health Organization. Making choices in health: WHO guide to cost-effectiveness analysis. WHO. 2003. entity/choice/book/en/index.html.
World Health Organization. WHO guide for standardization of economic evaluations of immunization programmes. Geneva : World Health Organization, 2008 2008. Report No.
NICE International. Bill and Melinda Gates Foundation Methods for Economic Evaluation Project (MEEP): Final Report. 2014.
Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet (London, England). 2012;380(9859):2197–223. https://doi.org/10.1016/s0140-6736(12)61689-4.
Crump JA, Youssef FG, Luby SP, Wasfy MO, Rangel JM, Taalat M, et al. Estimating the incidence of typhoid fever and other febrile illnesses in developing countries. Emerg Infect Dis. 2003;9(5):539–44. https://doi.org/10.3201/eid0905.020428.
Pieters Z, Saad NJ, Antillón M, Pitzer VE, Bilcke J. Case fatality rate of enteric fever in endemic countries: a systematic review and meta-analysis. Clin Infect Dis. 2018;67(4):628–38. https://doi.org/10.1093/cid/ciy190.
World Bank. Life expectancy at birth, total (years) 2021. 2019 Revision: https://data.worldbank.org/indicator/SP.DYN.LE00.IN.
Limani F, Smith C, Wachepa R, Chafuwa H, Meiring J, Noah P, et al. Estimating the economic burden of typhoid in children and adults in Blantyre, Malawi: a costing cohort study. Res Square. 2021. https://doi.org/10.21203/rs.3.rs-1214074/v1.
Marchello CS, Birkhold M, Crump JA. Complications and mortality of typhoid fever: a global systematic review and meta-analysis. J Infect. 2020;81(6):902–10. https://doi.org/10.1016/j.jinf.2020.10.030.
Darton TC, Meiring JE, Tonks S, Khan MA, Khanam F, Shakya M, et al. The STRATAA study protocol: a programme to assess the burden of enteric fever in Bangladesh, Malawi and Nepal using prospective population census, passive surveillance, serological studies and healthcare utilisation surveys. 2017. doi: https://doi.org/10.1136/bmjopen-2017-016283.
Abboud L. Global hospitalization rate of typhoid fever: a meta-regression. Antwerp: University of Antwerp; 2017.
Salomon JA, Vos T, Hogan DR, Gagnon M, Naghavi M, Mokdad A, et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet (London, England). 2012;380(9859):2129–43. https://doi.org/10.1016/s0140-6736(12)61680-8.
Strong MO, Jeremy E. An efficient method for computing single-parameter partial expected value of perfect information. Med Decis Making. 2012;33(6):755–66. https://doi.org/10.1177/0272989X12465123.
Stenberg K, Lauer JA, Gkountouras G, Fitzpatrick C, Stanciole A. Econometric estimation of WHO-CHOICE country-specific costs for inpatient and outpatient health service delivery. Cost Effect Resour Alloc. 2018;16(1):1–15. https://doi.org/10.1186/s12962-018-0095-x.
R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2017.
Appiah GD, Chung A, Bentsi-Enchill AD, Kim S, Crump JA, Mogasale V, et al. Typhoid outbreaks, 1989–2018: implications for prevention and control. Am J Trop Med Hyg. 2022;102(6):1296–305. https://doi.org/10.4269/ajtmh.19-0624.
Meiring JE, Shakya M, Khanam F, Voysey M, Phillips MT, Tonks S, et al. Burden of enteric fever at three urban sites in Africa and Asia: a multicentre population-based study. Lancet Glob Health. 2022;9(12):E1688–96. https://doi.org/10.1016/S2214-109X(21)00370-3.
Acknowledgements
Not applicable.
Funding
This work was supported the Bill and Melinda Gates Foundation [OPP1151153]. The funder had no role in the identification, design, conduct, or reporting of the analyses. Under the grant conditions of the Foundation, a Creative Commons Attribution 4.0 Generic License has already been assigned to the Author Accepted Manuscript version that might arise from this submission.
Author information
Authors and Affiliations
Contributions
VEP conceived of and presented idea. VEP and MTP designed the analysis. NBZ, FL, DT contributed data or analysis tools. MTP performed the analysis. MTP and VEP wrote the paper. All authors provided critical feedback and helped shape the research and manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
VEP is a member of the World Health Organization's (WHO) Immunization and Vaccine-related Implementation Research Advisory Committee and has received reimbursements from Merck and Pfizer for travel to Scientific Input Engagements unrelated to the topic of this manuscript. The views expressed in this manuscript are those of the authors and do not necessarily reflect the views of the WHO. All other authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Options for disability weights assigned to different healthcare use groups. Disability weights presented for the two options are for infectious disease, acute, and for the specified level of typhoid episode (mild, moderate, or severe). Table S2. Input parameters for transmission model and cost-effectiveness analysis, with distributions. Typhoid incidence and age distribution, mortality, antimicrobial resistance, healthcare use, treatment cost, vaccine-related costs, and disability-adjusted life-year uncertainty distributions and their page location in the text are shown. Table S3. Predicted disease and economic burden in the absence of vaccination. The median (95% credible interval) estimates for predicted cases, deaths, DALYs, and treatment costs per 100,000 people over 10 years are shown for each scenario in the absence of vaccination. Table S4. Predicted vaccine impact with randomized outbreak timing, pre-outbreak incidence and post-outbreak incidence per 100,000 individuals. The median (95% credible interval) estimates for averted cases, deaths, DALYs, treatment costs, costs of vaccinations and net costs per 100,000 people are shown for each vaccination strategy compared to no vaccination for randomized outbreak timing (“randomized”), pre-outbreak incidence (“pre”), and post-outbreak incidence (“post”). Vaccination strategies include routine vaccination at nine months of age in year 0 with or without a catchup campaign up to 15 years of age. Reactive routine vaccination strategies (with a catchup campaign) include delays of 1, 6, 12, and 24 months to deployment (“1 m”, “6 m”, “12 m”, “24 m”, respectively). All values are presented as incidence per 100,000 people. R = routine vaccination; RC = routine vaccination plus a catchup campaign. Table S5. Predicted vaccine impact with fixed outbreak timing incidence per 100,000 individuals. The median (95% credible interval) estimates for averted cases, deaths, DALYs, treatment costs, costs of vaccinations and net costs per 100,000 people are shown for each vaccination strategy compared to no vaccination with fixed outbreak timing. vaccination strategies include routine vaccination at nine months of age in year 0 with or without a catchup campaign up to 15 years of age. Preventive strategy results are shown for 10, 5, 2, and 1 year(s) (“10y”, “5y”, “2y”, “1y”) before the outbreak starts. Reactive routine vaccination strategies (with a catchup campaign) include delays of 1, 6, 12, and 24 months to deployment (“1 m”, “6 m”, “12 m”, “24 m”, respectively). All values are presented as incidence per 100,000 people. R = routine vaccination; RC = routine vaccination plus a catchup campaign. Table S6. Predicted vaccine impact with WHO-CHOICE cost of illness data: randomized outbreak timing, pre-outbreak incidence and post-outbreak incidence. The median (95% credible interval) estimates for averted treatment costs and net costs per 100,000 people are shown (averted cases, deaths, DALYs, and costs of vaccinations are the same as the main scenarios) for each vaccination strategy compared to no vaccination for randomized outbreak timing (“randomized”), pre-outbreak incidence (“pre”), and post-outbreak incidence (“post”) using previous WHO-CHOICE cost of illness data. Vaccination strategies include routine vaccination at nine months of age in year 0 with or without a catchup campaign up to 15 years of age. Reactive routine vaccination strategies (with a catchup campaign) include delays of 1, 6, 12, and 24 months to deployment (“1 m”, “6 m”, “12 m”, “24 m”, respectively). All values are presented as costs per 100,000 people. R = routine vaccination; RC = routine vaccination plus a catchup campaign. Fig S1. Ordinary differential equations and corresponding dynamic compartmental model for typhoid disease dynamics. Black compartments and text indicate the scenario in which there is no vaccination, and the blue compartments and text indicate the added scenarios in which vaccination is introduced. Note that this model is also age-structured, though not shown. Fig S2. Observed and modeled vaccine efficacy over time. Observed data from a phase 3, double-blind, randomized active-controlled clinical trial of single-dose TCV in Blantyre, Malawi at 3 time points (12, 18, and 24 months) (black points with 95% confidence interval error bars) and the modeled vaccine efficacy after vaccination (median estimate: solid blue line; 95% credible interval in shaded light blue) are shown. Fig S3. Sensitivity and specificity of outbreak identification threshold definitions. The sensitivity (purple) and specificity (green) are shown for each outbreak identification definition (x-axis; ranging from 6–16 standard deviations above the mean monthly reported typhoid fever cases). Fig S4. Estimated specificity of outbreak identification thresholds 6 to 16 standard deviations above the monthly mean reported typhoid fever cases. The median outbreak identification date (dot) and 95% credible interval (line) is shown for outbreak identification thresholds of 6–16 standard deviations above the monthly mean number of typhoid cases for 1000 simulations of the dynamic model. The black dashed line represents the “true” start date of the outbreak, and the shaded grey area represents 0–18 months after the outbreak started (sensitivity window). Fig S5. Observed and fitted proportion of typhoid infections that are resistant to antimicrobial treatment in Blantyre, Malawi from 1995–2025. Observed data points of the yearly proportion of antimicrobial resistant typhoid fever infections over time are shown in black dots, while the fitted estimates from the beta regression model are shown in the dashed blue line and the prediction intervals are shown in the turquoise dotted lines. Fig S6. Predicted and observed weekly blood-culture confirmed typhoid fever cases in the absence of vaccination. The 1000 stochastic realizations of weekly blood-culture confirmed typhoid fever case incidence per 100,000 people in the absence of vaccination from the dynamic transmission model are show in purple. The observed (reported) typhoid fever cases used to fit the dynamic model is represented by the bold black line, while the observed incidence collected after model fitting is represented by the dashed red line. Fig S7. Observed versus fitted age distribution of reported typhoid cases. The proportion of observed cases in each age group are denoted by light blue bars, while the model-predicted age distribution is shown in darker blue. Fig S8. Predicted weekly blood-culture confirmed typhoid infections in Scenario 1 for reactive vaccination strategies. The 1000 simulated predictions for weekly blood-culture confirmed typhoid infections are shown in purple, with the median of all stochastic realizations shown in orange for each reactive vaccination strategy. Four situations are shown, representing the four different delays in timing to implement vaccination once the outbreak is identified (1, 6, 12, and 24 months). The median typhoid infections in the absence of vaccination from 1000 realizations is shown in black, and the median date of vaccination deployment for each situation is denoted by the vertical dashed green line. Fig S9. Predicted weekly blood-culture confirmed typhoid fever cases in Scenario 1 for preventive vaccination strategies. The 1000 stochastic realizations of weekly typhoid cases are shown in purple, with the median of all simulations shown in orange for each preventive vaccination strategy. Eight situations are shown, representing each preventive routine vaccination timing strategy (10, 5, 2, and 1 year(s) before the outbreak for routine vaccination at 9 months of age with and without a catchup campaign up to 15 years of age). The median number of typhoid infections in the absence of vaccination from 1,000 realizations is shown in black, and the date of vaccination deployment for each situation is denoted by the vertical dashed green line. Fig S10. Heatmap of optimal intervention strategy and its estimated uncertainty across a range of willingness to pay values for each strategy comparison and a range of deployment delays, and years before the outbreak. Each column in a single panel shows the preferred strategy (i.e. the strategy that yields the highest average net benefit) for one cost-effectiveness analysis comparing no vaccination (grey), preventive routine vaccination (purple), preventive routine vaccination with a catch-up campaign (green), and reactive vaccination with a catch-up campaign (orange) for delays of 1, 6, 12, or 24 months after the outbreak has been identified (x-axis). The y-axis represents willingness-to-pay (WTP) values ranging from $0-$1000 (USD 2020). The shading represents the probability that the preferred strategy yields the highest net benefit (lighter: lower probability; darker: higher probability). Results are plotted for whether preventive vaccination is introduced 10 years (top panel) or 1 year (bottom panel) before the outbreak for a 20-year time horizon. Note that preventive routine vaccination without a catchup campaign is never a preferred strategy, and as a result does not appear in the plots. Fig S11. Cost-effectiveness planes and acceptability frontiers for sensitivity analysis assuming WHO-CHOICE treatment costs. The cost-effectiveness planes (left) and cost-effectiveness acceptability frontiers (CEAFs; right) are plotted for (A-B) Scenario 1 (randomized outbreak timing), (C-D) Scenario 2 (no outbreak, assuming pre-outbreak incidence), and (E–F) Scenario 3 (outbreak has already occurred). In the cost-effectiveness planes, each dot represents the incremental costs (in 2020 USD) and DALYs averted for one simulation when compared with the base case strategy of no vaccination. The bold Xs denote the expected additional cost and DALYs averted for each vaccination strategy with respect to no vaccination. Strategies are indicated by the color of the dot or X (purple: preventive routine vaccination; green: preventive routine vaccination plus a catch-up campaign up to age 15; or orange: reactive routine vaccination plus a catch-up campaign to age 15—for Scenario 1 only). In the CEAFs, the preferred strategy (i.e. the strategy that yielded the highest average net benefit) for each willingness-to-pay threshold ($0–1,000 per DALY averted; x-axis, 2020 USD) is indicated by the color of the line (black: no vaccination; and same strategy colors as other panels), while the proportion of samples in which that strategy yielded the highest net benefit is indicated by the value on the y-axis; this can be interpreted as our certainty in the optimal strategy. Fig S12. Expected value of partially perfect information for differing delays in vaccination deployment for reactive strategies with randomized outbreak timing (Scenario 1). The expected value of partial perfect information (EVPPI) for each parameter is shown for a range of willingness-to-pay values. Results are shown for 5000 parameter samples (in 2020 USD). Each panel shown represents the EVPPI for one cost-effectiveness analysis comparing 4 strategies: no vaccination (base case), preventive routine vaccination at 9 months, preventive routine vaccination with a catch-up campaign up to 15 years, and reactive routine vaccination with a catch-up campaign. The four panels (left to right) correspond to different delays in the reactive strategy (1-, 6-, 12-, or 24-month delays). The grey vertical dashed line corresponds to the 2020 gross domestic product per capita for Malawi. Fig S13. Expected value of partially perfect information for Scenario 2 (pre-outbreak incidence). The expected value of partial perfect information (EVPPI) for each parameter is shown for a range of willingness-to-pay values. Results are shown for 5000 parameter samples in 2020 USD. Fig S14. Expected value of partially perfect information for Scenario 3 (post-outbreak incidence). The expected value of partial perfect information (EVPPI) for each parameter is shown for a range of willingness-to-pay values. Results are shown for 5000 parameter samples in 2020 USD.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Phillips, M.T., Antillon, M., Bilcke, J. et al. Cost-effectiveness analysis of typhoid conjugate vaccines in an outbreak setting: a modeling study. BMC Infect Dis 23, 143 (2023). https://doi.org/10.1186/s12879-023-08105-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08105-2