Abstract
Background
Cardiovascular disease is a major cause of morbidity and mortality in people with HIV. The detection of subclinical atherosclerosis through vascular ultrasound allows us to identify patients at an increased risk of cardiovascular disease as a primary prevention strategy; this test is not routine. Our objective is to identify predictors of subclinical atherosclerosis in a population with HIV.
Methods
People with HIV infection were selected for primary prevention and underwent carotid and femoral ultrasound to detect atheromatous plaques. Logistic regression analysis including vascular risk factors was performed to predict the presence of atherosclerosis.
Results
One hundred eighty-three patients were included, 54% of whom were smokers; the mean duration of HIV infection was 9.52 years, and all patients were undergoing antiretroviral treatment. Subclinical atherosclerosis was present in 62.29% of the patients; 83.32% had plaque in the carotid territory, 57.93% in the femoral territory and 25.6% in both vascular territories. Compared to those without atherosclerosis, patients with atherosclerosis were on average 5.35 years older (53.86 vs. 48.51, p < 0.001) and had a higher prevalence of smoking (63.23% vs. 39.12%, p = 0.020) and a CD4/CD8 ratio below 0.7 (44.23% vs. 29.02%, p = 0.043). A CD4/CD8 ratio lower than 0.3 was always associated with subclinical atherosclerosis (95% confidence interval (CI): 83.9–100%). The inclusion of smoking, the CD4/CD8 ratio and age in the logistic regression analysis led to a diagnostic yield of 72% measured by the area under the receiving operator characteristic (ROC) curve (95% CI: 64–80%).
Conclusions
Tobacco use, age and a CD4/CD8 ratio below 0.7 allow prediction of the presence of subclinical atherosclerosis in primary prevention. A CD4/CD8 ratio below 0.3 was a diagnostic indicator of atherosclerosis in HIV patients undergoing primary prevention in our sample.
Similar content being viewed by others
Background
The development of antiretroviral therapies (ARTs) and their greater accessibility have allowed better control of human immunodeficiency virus (HIV) infection and diseases related to acquired immunodeficiency syndrome (AIDS). The life expectancy of people with HIV has therefore increased and is currently similar to that of the general population [1]. Consequently, cardiovascular disease (CVD) is currently one of the main causes of morbidity and mortality [2] in this group of people.
People with HIV have an increased vascular risk, which extends beyond what can be explained by recognized traditional risk factors [3] and may be related to HIV infection itself and to antiretroviral treatment.
Despite effective antiretroviral treatment, HIV infection results in degrees of residual viremia and is associated with persistent immune activation, which generates a direct chronic inflammatory effect on artery walls. Along with other related mechanisms, such as coagulation failure, dyslipidaemia, alteration of the elasticity of arterial walls and endothelial dysfunction, residual viremia accelerates the formation of atheromatous plaques [4, 5], which are precursors of the onset of cardiovascular events.
Atheromatosis detection in the carotid and femoral territories by ultrasound in people with HIV without a history of CVD, which is called subclinical atheromatosis (SAT), would have value in the prediction of new cardiovascular events [6]. However, despite being an innocuous and low-cost technique, it is not always accessible to clinicians. Therefore, the identification of participants with a high probability of presenting with SAT would be of interest to select those with a greater risk of suffering CVD in the future.
The purpose of our study was to identify predictive factors of SAT in people with HIV without a history of established CVD.
Methods
Study design and population
A cross-sectional and multicentre study was carried out by the Lipid and Vascular Risk Unit of the Infanta Elena Hospital together with the Infectious Diseases Units of the Infanta Elena and Juan Ramón Jiménez Hospital in Huelva, Spain. This study was approved by the Research Ethics Committee of the province of Huelva with the code JFS-ATE-2017-01.
The HIV population of the province of Huelva is registered in a database, which currently includes a total of 1208 patients and is managed by the computer program Hospital Control Application (Aplicación de Control Hospitalario—AC&H™) used by the Infectious Diseases Units of the Infanta Elena and Juan Ramón Jiménez Hospitals in Huelva. This program is widely used in several hospitals of the National Health System, is a component of the VIH-Aplicación de Control Hospitalario (VACH) cohort [7] and collects demographic and clinical data, HIV transmission category, serological and immunovirological data, history of antiretroviral treatments performed, comorbidities, opportunistic diseases and specific data on diseases unrelated to HIV.
To enter the study, participants had to meet the following inclusion criteria: HIV infection with more than 10 years of evolution, age between 18 and 65 years and signed informed consent.
The presence of any of the following criteria excluded the participants from the study: class C cirrhosis according to the Child‒Pugh classification; positive serology for hepatitis B virus (HBV); type 1 diabetes mellitus; renal failure (glomerular filtrate < 60 mL/min by Chronic Kidney Disease Epidemiology Collaboration); recorded history of vascular disease including acute coronary syndrome, acute myocardial infarction, aortic aneurysm, ischaemic or haemorrhagic stroke, transient ischaemic attack (TIA), peripheral arterial disease (intermittent claudication, pain or paraesthesia at rest, trophic lesions, established gangrene), coronary revascularization (percutaneous or bypass) or any other arterial revascularization procedure, plaque visualized on coronary angiography or carotid ultrasound or arterial stenosis at any level (> 50%).
After informed consent was signed by each patient, an imaging study of the carotid (common carotid artery, bulbar, right and left internal and external carotid arteries) and femoral (common and superficial vessels, also on both sides) vascular territories was performed with a Toshiba Medical Systems Aplio XG scanner. The presence of atherosclerotic plaque was assessed by high-resolution colour vascular Doppler ultrasound following the Mannheim consensus protocol of 2004–2006 [8], which defines an atheroma plaque as a focal structure that encroaches on the arterial lumen by at least 0.5 mm.
The measurements obtained from the digital images were performed by the same experienced technician who did not know the clinical characteristics of the participants.
The results were included in a database created for this purpose, which complies with confidentiality guarantees and data protection regulations. Access to the database by professionals is restricted, and the use of data for this research was carried out anonymously.
We evaluated the presence of the classic risk factors associated with atherosclerosis in each participant: age, arterial hypertension, diabetes, dyslipidaemia, active smoking and a family history of early cardiovascular events following the definition criteria of the European Atherosclerosis Society [9]. We also considered analytical parameters such as total cholesterol, cholesterol bound to low- (LDL-C) and high-density lipoproteins (HDL-C), triglycerides, CD4/CD8 ratio at the beginning of treatment, CD4 nadir and viral suppression time, which was defined as < 200 copies/mL or < 50 copies/mL of HIV-1 RNA in plasma according to the method used (< 200 copies/mL from 1996 to 2006 and < 50 copies/mL subsequently), as well as the history of coinfection by hepatitis C virus (HCV), immunoglobulin G (IgG) positive for cytomegalovirus (CMV) and ART history. We considered treatments performed when any of the following therapeutic groups were used for at least one year: non-nucleoside reverse transcriptase inhibitors (NNRTIs), nucleoside and nucleotide reverse transcriptase inhibitors (NRTIs), protease inhibitors (PIs) and integrase strand transfer inhibitors (INSTIs).
Statistical analysis
Descriptive statistics were performed for all variables: the mean and standard deviation for continuous variables and frequencies with percentages for categorical and ordinal variables.
Student t tests were used to compare parametric quantitative variables, and Mann‒Whitney U tests were used for variables that did not follow normality. The chi-square test (or Yates’ correction for continuity) was used for categorical and ordinal variables.
Through logistic regression analysis, we evaluated possible independent predictors of the presence of atheromatous plaque among all the variables studied using the Wald test. The diagnostic performance of the model was obtained by the area under the receiver operating characteristics (ROC) curve (AUC).
The cutoff points were established using the ROC curve. A cutoff point of 0.3 was chosen to achieve a specificity of 100%, and a cutoff point of 1.7 was chosen to achieve a sensitivity of 0%.
The cutoff point 0.7 was selected because it contributed the most information to the model and yielded the highest diagnostic performance. Cutoff points 0.3 and 1.7 did not contribute additional information.
All analyses were performed using the statistical package R Commander UCA, version 4.4.1, released September 26, 2021, from the University of Cádiz (Spain). An alpha error of 0.05 was considered statistically significant.
Results
Of the 1208 HIV patients registered in the AC&H database, records for 809 were discarded because they met the following exclusion criteria: 38 were older than 65 years or younger than 18 years, 427 had HIV infection with less than 10 years of evolution, 54 had suffered previous CVD, 147 had renal failure (filtering less than 60 mL/min), and 143 had HBV infection.
A total of 399 patients were selected, 183 of whom agreed to participate in the study and signed the informed consent form (Fig. 1).
We included data from 183 patients collected from October 2020 to July 2021. A total of 114/183 (62.29%) presented with SAT. A total of 95/114 (83.32%) had plaque in the carotid territory, and 66/114 (57.93%) had plaque in the femoral territory. A total of 47/114 (41.23%) had plaques in both vascular territories.
The general characteristics of the HIV population with and without SAT are described in Table 1. We found differences between the two groups in age (53.86 vs. 48.51, p < 0.001) and smoking behaviour (63.23% vs. 39.12%, p = 0.020). Other vascular risk factors, such as female sex, diabetes, dyslipidaemia, arterial hypertension and family history of early CVD, were more frequent in the SAT group, although without statistical significance. Lipid profiles were similar in both groups (Table 1).
In terms of characteristics related to HIV infection, the years of exposure to HIV for patients with SAT compared to those without SAT were 22.28 vs. 18.42 (p = 0.002). A low CD4 nadir was associated with the presence of SAT compared to the absence of SAT (166.17 vs. 231.94 cells/µL, p = 0.013).
We found an inverse relationship between the CD4/CD8 ratio and SAT; a CD4/CD8 ratio lower than 0.7 was associated the presence of SAT compared to the absence of SAT (44.23% vs. 29.02%, p = 0.043). All patients with a CD4/CD8 ratio < 0.3 had SAT (95% confidence interval (CI): 83.9–100%), and none of the patients with a CD4/CD8 ratio > 1.7 showed SAT (95% CI: 84.7–100%).
The history of HCV coinfection was higher in the SAT group (42.12% vs. 24.64%, p = 0.017). Regarding the treatments performed, we found that PI use was higher in the SAT group (63.21% vs. 41.83%, p = 0.006). The use of reverse transcriptase (RT) inhibitors, both analogues and non analogues, was more frequent in the group without SAT, although without statistical significance. The use of integrase inhibitors was more frequent in the SAT group, but the difference was not significant. The duration of viral suppression measured in years was similar in both groups (10.03 vs. 9.01, p = 0.161). No differences in positive CMV serology were found.
Adjusting for all the variables present in the model, those that provided the most predictive information were selected: age, smoking and CD4/CD8 < 0.7. PI use and the rest of the variables explored were not included in the model.
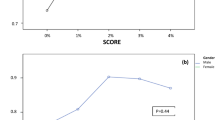
Including active smoking, age and a CD4/CD8 ratio < 0.7 in a prediction equation for subclinical atherosclerosis by means of logistic regression achieved good predictive power. As shown in Fig. 2, the diagnostic performance of this prediction by means of the AUC was 72% (95% CI: 64–80%).
ROC curve for subclinical atheromatosis (SAT) detection in HIV participants without previous cardiovascular disease. Receiver operating characteristics curve evaluating the accuracy SAT detection in participants with HIV without previous CVD. AUC: area under the curve (95% confidence interval); X: mean; SD: standard deviation. The probability of presenting atheromatous plaque was calculated using the following formula: \(\mathrm{P }(\mathrm{Plaque}) =\frac{1}{{1+e}^{-(3.963-0.077*Age-0.092*CD4/CD8\left(if<0.7\right)-0.933*(if active smoker)}}\) where P: the probability of presenting atheromatous plaque; e: exponential constant; Age: age in years; CD4/CD8: 1 if CD4/CD8 < 0.7; Active smoker: 1 if an active smoker
Discussion
The increase in the incidence of CVD in people with HIV and underestimation of the CVD risk through commonly used tools necessitate exploration of new resources to adequately assess vascular risk in these patients. SAT is the pathophysiological basis of CVD. The high prevalence of SAT among the HIV population may explain the greater number of cardiovascular events in people with HIV [10].
In our cohort, the prevalence of SAT among HIV participants without previous CVD was 62.29%, which is much higher than that published in the literature. In a recent meta-analysis by Liu et al. [11], a prevalence of carotid SAT between 31.6% and 37% was reported.
The higher frequency of atheromatous plaque recorded in our study can be explained by several factors.
Factors related to the population studied
Our study was developed in Europe, where the prevalence of traditional cardiovascular risk factors (CVRFs), such as smoking, obesity and alcohol abuse, is high [12]. Most of the participants in our study were men (66.6%) and were over 40 years old.
On the other hand, we selected patients with HIV infection with more than 10 years of evolution, which may have influenced the high prevalence of atheromatosis observed in our patients.
Factors related to the type of study
High variability is evident among published reports on the SAT prevalence in the HIV population. These diverse findings can be explained by the heterogeneity of the populations studied and the different criteria used to define atheromatous plaque. A total of 83.32% of the plaques found in our patients were in the carotid territory, and if we exclude the plaques found in the femoral territory, the prevalence of plaque was 52%, which was even higher than published rates. However, the number of territories studied must be considered. In most studies, the estimation of atheromatous plaque is performed on the common carotid [11], while in our case, we performed this estimation on the common carotid, bulbar, internal carotid, external carotid, common femoral and superficial femoral territories.
HIV infection is related to selective depletion of CD4 lymphocytes and increased expression of CD8, which lead to an inverted CD4/CD8 ratio (< 1) [13]. This ratio has recently emerged as a marker of immunosenescence and is independently associated with risk factors for both AIDS and non-AIDS events and mortality. In addition, it has been independently associated with intima-media thickness (IMT) progression [14] and SAT [15]. Specifically, a CD4/CD8 ratio < 0.5 or < 0.3 has been determined to be a risk factor for non-AIDS events or mortality, especially when the CD4 count is high (≥ 500 cells/μL) [16].
A decreased ratio can be maintained despite having achieved viral suppression and normalization of CD4 levels with ART [17]. Among the factors associated with a persistent inversion of the CD4/CD8 ratio are the presence of positive CMV serology, ART initiation before 1997, a low CD4 nadir and a short duration of viral suppression [18]. An inverted CD4/CD8 ratio and a low CD4 nadir have been associated with an increased risk of non-AIDS events [19].
The CD4/CD8 ratio tends to present greater stability over time than the absolute counts of CD4 and CD8 cells, and its predictive value for events unrelated to AIDS has been described as exceeding that of the absolute CD8 count in individuals with restored CD4 counts (> 500 cells/µL) [20].
This ratio can be used as a marker of immune dysregulation and as a predictor of non-AIDS events in these patients.
In our cohort, we observed an association between inversion of the CD4/CD8 ratio and the presence of carotid and femoral atheromatosis, which may constitute a parameter to be considered when estimating the risk of CVD in the HIV population without previous events. In addition, the presence of atheromatous plaque was associated with a low CD4 nadir and positive CMV serology, with no differences in viral suppression time found.
Through the use of predictors included in the logistic regression analysis, we obtained a diagnostic yield measured by the ROC curve of 72%.
In our cohort, we observed greater use of PIs in the SAT group. These results must be considered with caution, since patients with HIV follow different therapeutic regimens throughout their disease courses, and within the PI group, the new generations of PIs are very different in terms of side effects and cardiovascular safety.
Although studies related to normalization of the CD4/CD8 ratio with early ART initiation have been published [20,21,22], no differences have been found among the different classes of ART used [23].
Although the earliest PIs, such as ritonavir, have been associated with an increased risk of CVD [24], the use of new therapies, such as atazanavir, has been associated with slower progression of atheromatous plaque and a lower incidence of CVD [25].
Vascular ultrasound of the carotid and femoral territories allows assessment of the presence of atheromatous plaque in these locations and provides information on the extent of atherosclerosis at the systemic level.
This approach is fast and innocuous and may be useful to reclassify the vascular risk of people with HIV [26], allowing treatment readjustment with the objective of reducing the vascular risk and avoiding CVD in the future.
Performing ultrasound in primary prevention in intermediate-risk patients is relevant since it can permit vascular risk reclassification.
However, despite the high prevalence of plaque in the HIV population, this technique is normally not included in routine check-ups for several reasons, including a lack of ultrasound time and a necessary learning curve.
Identifying the predictive factors for the presence of SAT is essential to be able to reclassify patients and select those who will obtain a greater benefit from evaluations for SAT.
Therefore, the findings obtained in our cohort may be relevant to vascular risk assessments in these patients.
Advantages
The CD4/CD8 ratio can play a role in comprehensive assessments of vascular risk in people with HIV, constituting a simple and accessible tool.
Through three clinical-analytical parameters easily extracted from the clinical history of participants (CD4/CD8 ratio less than 0.7, age and active smoking), we were able to predict the presence of SAT in HIV patients without previous CVD.
Limitations
As the sample size was small due to the design of the study, these results should be considered with caution, and additional studies are necessary to confirm the findings.
A tendency towards a greater incidence of traditional vascular risk factors, such as hypertension and diabetes, was evident in the group with atheromatous plaque, although without significance, probably due to the insufficient sample size. We must also consider the greater use of PIs by patients with atheromatous plaque, which have been associated with an elevated vascular risk in people with HIV in other studies.
Conclusions
With three simple parameters—tobacco, age and a CD4/CD8 ratio less than 0.7—we were able to predict the presence of atheromatous plaque in HIV participants without previous CVD with a good diagnostic yield (AUC: 0.72; 95% CI: 0.64–0.80). The CD4/CD8 ratio is a biomarker that may be relevant in comprehensive assessments of people with HIV. A CD4/CD8 ratio < 0.3 was associated with a 100% presence of SAT in our sample (95% CI: 81.6–100%).
Availability of data and materials
The datasets generated and/or analysed during the current study are not public but are available from the corresponding author upon reasonable request.
Abbreviations
- AIDS:
-
Acquired immunodeficiency syndrome
- ARTs:
-
Antiretroviral therapies
- AUC:
-
Area under the curve
- CVD:
-
Cardiovascular disease
- CVRFs:
-
Cardiovascular risk factors
- HCV:
-
Hepatitis C virus
- HDL-C:
-
High-density lipoprotein cholesterol
- HIV:
-
Human immunodeficiency virus
- INSTIs:
-
Integrase strand transfer inhibitors
- LDL-C:
-
Low-density lipoprotein cholesterol
- NNRTIs:
-
Non-nucleoside reverse transcriptase inhibitors
- NRTIs:
-
Nucleoside and nucleotide reverse transcriptase inhibitors
- PIs:
-
Protease inhibitors
- ROC:
-
Receiver operating characteristics
- SAT:
-
Subclinical atheromatosis
- TIA:
-
Transient ischaemic attack
References
Wandeler G, Johnson LF, Egger M. Trends in life expectancy of HIV-positive adults on antiretroviral therapy across the globe: comparisons with general population. Curr Opin HIV AIDS. 2016;11:492–500.
Nou E, Lo J, Hadigan C, Grinspoon SK. Pathophysiology and management of cardiovascular disease in patients with HIV. Lancet Diabetes Endocrinol. 2016;4:598–610.
Hasse B, Ledergerber B, Furrer H, Battegay M, Hirschel B, Cavassini M, et al. Morbidity and aging in HIV-infected persons: the Swiss HIV cohort study. Clin Infect Dis. 2011;53:1130–9.
Freiberg MS, Chang CC, Kuller LH, Skanderson M, Lowy E, Kraemer KL, et al. HIV infection and the risk of acute myocardial infarction. JAMA Intern Med. 2013;173:614–22.
So-Armah K, Benjamin LA, Bloomfield GS, Feinstein MJ, Hsue P, Njuguna B, et al. HIV and cardiovascular disease. Lancet HIV. 2020;7:e279–93.
Coll B, Betriu A, Feinstein SB, Valdivielso JM, Zamorano JL, Fernández E. Papel de la ecografía carotídea en la reclasificación del riesgo cardiovascular de sujetos de riesgo bajo-intermedio. Rev Esp Cardiol. 2013;66:929–34.
Suárez-Lozano I, Fajardo JM, Garrido M, Roca B, García-Alcalde ML, Geijo P, et al. Epidemiological trends of HIV infection in Spain. AIDS. 2002;16:2496–9.
Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, et al. Mannheim carotid intima-media thickness consensus (2004–2006). Cerebrovasc Dis. 2006;23:75–80.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41:111–88.
Shah ASV, Stelzle D, Lee KK, Beck EJ, Alam S, Clifford S, et al. Global burden of atherosclerotic cardiovascular disease in people living with HIV: systematic review and meta-analysis. Circulation. 2018;138:1100–12.
Liu X, Sun Y, Zhan Y, Jiang Y. Prevalence and risk of subclinical carotid atherosclerosis in the global population with HIV: a systematic review and meta-analysis. Int J STD AIDS. 2021;32:411–20.
United Nations Economic and Social Commission for Asia and the Pacific. Statistical yearbook for Asia and the Pacific. In United Nations publication. 2015. p. 25–35. ISBN: 978–92–1–120716–3. https://www.unescap.org/sites/default/files/SYB2015_Full_Publication.pdf
Serrano-Villar S, Moreno S, Fuentes-Ferrer M, Sánchez-Marcos C, Ávila M, Sainz T, et al. The CD4:CD8 ratio is associated with markers of age-associated disease in virally suppressed HIV-infected patients with immunological recovery. HIV Med. 2013;15:40–9.
Morell EB, Cabeza JS, Muñoz Á, Marín I, Masiá M, Gutiérrez F, et al. The CD4/CD8 ratio is inversely associated with carotid intima-media thickness progression in human immunodeficiency virus-infected patients on antiretroviral treatment. AIDS Res Hum Retrovir. 2016;32:648–53.
Lo J, Abbara S, Shturman L, Soni A, Wei J, Rocha-Filho JA, et al. Increased prevalence of subclinical coronary atherosclerosis detected by coronary computed tomography angiography in HIV-infected men. AIDS (London, England). 2010;24:243–53.
Serrano-Villar S, Martínez-Sanz J, Ron R, Talavera-Rodríguez A, Fernández-Felix BM, Herrera S, et al. Effects of first-line antiretroviral therapy on the CD4/CD8 ratio and CD8 cell counts in CoRIS: a prospective multicentre cohort study. Lancet HIV. 2020;7:e565–73.
Serrano-Villar S, Gutiérrez C, Vallejo A, Hernández-Novoa B, Díaz L, Fernández MA, et al. The CD4/CD8 ratio in HIV-infected subjects is independently associated with T-cell activation despite long-term viral suppression. J Infect. 2013;66:57–66.
Caby F, Guihot A, Lambert-Niclot S, Guiguet M, Boutolleau D, Agher R, et al. Determinants of a low CD4/CD8 Ratio in HIV-1–infected individuals despite long-term viral suppression. Clin Infect Dis. 2016;62:1297–303.
Castilho JL, Turner M, Shepherd BE, Koethe JR, Furukawa SS, Bofill CE, et al. CD4/CD8 ratio and CD4 nadir predict mortality following noncommunicable disease diagnosis in adults living with HIV. AIDS Res Hum Retrovir. 2019;35:960–7.
Serrano-Villar S, Sainz T, Lee SA, Hunt PW, Sinclair E, Shacklett BL, et al. HIV-infected individuals with low CD4/CD8 ratio despite effective antiretroviral therapy exhibit altered T cell subsets, heightened CD8+ T cell activation, and increased risk of non-AIDS morbidity and mortality. PLoS Pathog. 2014;10: e1004078.
Caby F, Guihot A, Lambert-Niclot S, Guiguet M, Boutolleau D, Agher R, Valantin MA, Tubiana R, Calvez V, Marcelin AG, Carcelain G, Autran B, Costagliola D, Katlama C. Determinants of a low CD4/CD8 ratio in HIV-1-infected individuals despite long-term viral suppression. Clin Infect Dis. 2016;62(10):1297–303. https://doi.org/10.1093/cid/ciw076.
Serrano-Villar S, Martínez-Sanz J, Ron R, Talavera-Rodríguez A, Fernández-Felix BM, Herrera S, Muriel A, Fanjul F, Portilla J, Muñoz J, Amador C, de Zárraga MA, Vivancos MJ, Moreno S, Jarrin I, Alejos B, Muñoz-Fernández Má, Consuegra I, Merino E, Vallejo A. Effects of first-line antiretroviral therapy on the CD4/CD8 ratio and CD8 cell counts in CoRIS: a prospective multicentre cohort study. Lancet HIV. 2020;7(8):e565–73. https://doi.org/10.1016/S2352-3018(20)30202-2.
Zhabokritsky A, Szadkowski L, Cooper C, Loutfy M, Wong A, Mcclean A, Hogg RS, Walmsley SL, Brumme Z, Burchell AN, Cooper C, Kelly D, Klein M, Kroch A, Loutfy M, Machouf N, Montaner J, Salters K, Raboud J, Zhu J. Increased CD4:CD8 ratio normalization with implementation of current ART management guidelines. J Antimicrob Chemother. 2021;76(3):729–37. https://doi.org/10.1093/jac/dkaa484.
Ryom L, Lundgren JD, El-Sadr W, Reiss P, Kirk O, Law M, et al. Cardiovascular disease and use of contemporary protease inhibitors: the D:A: D international prospective multicohort study. Lancet HIV. 2018;5:e291–300.
Li M, Chan WW, Zucker SD. Association between atazanavir-induced hyperbilirubinemia and cardiovascular disease in patients infected with HIV. J Am Heart Assoc. 2020;9: e016310.
Coll B, Betriu A, Feinstein SB, Valdivielso JM, Zamorano JL, Fernández E. The Role of Carotid Ultrasound in Assessing Carotid Atherosclerosis in Individuals at Low-to-intermediate Cardiovascular Risk. Revista Española de Cardiología (English Edition). 2013;66(12):929–34. https://doi.org/10.1016/j.rec.2013.05.030.
Acknowledgements
Not applicable.
Funding
The authors did not receive financial support for the research, authorship and/or publication of this article.
Author information
Authors and Affiliations
Contributions
Study conception and design: JFS and MJR-J. Data acquisition: JFS, EBE, JCAG. Data analysis and interpretation: MÁ, CL, JLSR. Article writing: JFS and MJR-J. Critical revision of the intellectual content: MJR-J, JLSR, JCAG, EBE. Final approval of the version to be presented: JLSR, MJR-J. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of the province of Huelva with the code JFS-ATE-2017-01. Written informed consent was obtained from all study participants. All methods were carried out in accordance with relevant guidelines and regulations or the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fernández Soto, J., Romero-Jiménez, M.J., Alarcón García, J.C. et al. Predictors of subclinical atherosclerosis in HIV. BMC Infect Dis 23, 17 (2023). https://doi.org/10.1186/s12879-022-07976-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07976-1