Abstract
Background
We aimed to elucidate differences in the characteristics of patients with coronavirus disease 2019 (COVID-19) requiring hospitalization in Japan, by COVID-19 waves, from conventional strains to the Delta variant.
Methods
We used secondary data from a database and performed a retrospective cohort study that included 3261 patients aged ≥ 18 years enrolled from 78 hospitals that participated in the Japan COVID-19 Task Force between February 2020 and September 2021.
Results
Patients hospitalized during the second (mean age, 53.2 years [standard deviation {SD}, ± 18.9]) and fifth (mean age, 50.7 years [SD ± 13.9]) COVID-19 waves had a lower mean age than those hospitalized during the other COVID-19 waves. Patients hospitalized during the first COVID-19 wave had a longer hospital stay (mean, 30.3 days [SD ± 21.5], p < 0.0001), and post-hospitalization complications, such as bacterial infections (21.3%, p < 0.0001), were also noticeable. In addition, there was an increase in the use of drugs such as remdesivir/baricitinib/tocilizumab/steroids during the latter COVID-19 waves. In the fifth COVID-19 wave, patients exhibited a greater number of presenting symptoms, and a higher percentage of patients required oxygen therapy at the time of admission. However, the percentage of patients requiring invasive mechanical ventilation was the highest in the first COVID-19 wave and the mortality rate was the highest in the third COVID-19 wave.
Conclusions
We identified differences in clinical characteristics of hospitalized patients with COVID-19 in each COVID-19 wave up to the fifth COVID-19 wave in Japan. The fifth COVID-19 wave was associated with greater disease severity on admission, the third COVID-19 wave had the highest mortality rate, and the first COVID-19 wave had the highest percentage of patients requiring mechanical ventilation.
Similar content being viewed by others
Background
Coronavirus disease 2019 (COVID-19) was first reported in Wuhan, China, in December 2019, as an outbreak of pneumonia of unknown origin, and with subsequent rapid spread of infection worldwide [1]. The first case of COVID-19 in Japan was identified on January 16, 2020. As of September 2022, the country has experienced five waves of COVID-19, with a cumulative number of approximately 20 million individuals infected with COVID-19 [2]. Epidemics in each country vary in severity according to behavioral restrictions and mitigation strategies [3, 4]. In addition, the COVID-19 situation has become more serious with therapeutic advances, mutant variants, and vaccination [5,6,7]. Therefore, elucidating characteristics of each COVID-19 wave is important for preparing for future epidemics.
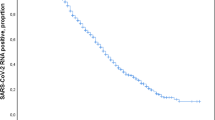
Each COVID-19 outbreak in different regions worldwide has unique characteristics [3, 4, 8]. Similarly, each COVID-19 wave in Japan exhibited unique characteristics. The first COVID-19 wave (2020/1/16 to 2020/6/13), in which the first emergency period was declared, was characterized by a lack of preparation of the health system, with many infections observed in nursing and medical facilities [9, 10]. In the second COVID-19 wave (2020/6/14 to 2020/10/9), after the first emergency was declared, it became apparent that the virus was hiding in the pleasure quarters of large cities and the infection began to spread. In the third COVID-19 wave (2020/10/10 to 2021/2/28), there were more infections than those in the first and second COVID-19 waves as a result of the approach of the Japanese government encouraging economic activities and gradual relaxation of immigration restrictions [11]. In the fourth COVID-19 wave (2021/3/1 to 2021/6/20), the Alpha variant (B.1.1.7), which had a high infectivity and severity rate, became the main strain of the virus [6, 12]. A previous single-center study comparing the fourth COVID-19 wave to the first three COVID-19 waves also showed that the fourth COVID-19 wave was more severe and resulted in a medical crisis in the city [13]. In the fifth COVID-19 wave, the Delta variant (B.1.617), which was associated with increased susceptibility to severe disease, became the main strain, causing a collapse of medical care systems [5, 12]. Figure 1 shows the number of infected people in Japan during each COVID-19 wave [2]. Notably, the country’s medical situation changed dramatically in each COVID-19 wave with advances in treatment and commencement of vaccination [14,15,16,17]. Although previous studies have compared each COVID-19 wave [3, 4, 10, 13, 18], the authors could not find any study characterizing Delta waves in Japan. Moreover, there are no comparisons on how the symptoms, severity, and outcomes changed in each COVID-19 wave and according to available therapeutic agents. This study aimed to determine the severity and patient characteristics of each COVID-19 wave using a Japanese nationwide registry to prepare for the possibility of another pandemic in the future.
Number of newly diagnosed COVID-19 cases between January 2020 and September 2021 in Japan in each COVID-19 wave. The first case of COVID-19 in Japan was reported on January 16, 2020. Remdesivir was approved by Japan on May 7, 2020. Dexamethasone was first published in the Clinical Practice Guide on July 17, 2020. Baricitinib was approved for use on April 23, 2021
Methods
Study design and settings
The study design and setting have been previously described [19]. This study utilized secondary data from a database. All patients infected with COVID-19 were recruited through the Japan COVID-19 Task Force [20], which was established in February 2020 as a nationwide multicenter consortium in Japan to collect and analyze clinical information of and specimens from patients with COVID-19 at more than 100 facilities nationwide with the aim of overcoming COVID-19. This retrospective cohort study was conducted between February 2020 and September 2021. This study was approved by the Ethics Committee of Keio University School of Medicine (ID: 20200061), and written or oral informed consent was obtained from all participants. The study was performed in accordance with the ethical standards set out in the 1964 Declaration of Helsinki and its later amendments.
Study population
Data of consecutive patients aged ≥ 18 years diagnosed with COVID-19 via polymerase chain reaction (PCR) testing or COVID-19 antigen testing at 1 of the 78 participating hospitals in Japan were registered in an electronic case record database by physicians at the affiliated research institution. Participating facilities include a wide range of hospitals in Japan admitting patients with COVID-19. The exclusion criteria were as follows: (1) non-Japanese patients with COVID-19, (2) unknown date of first positive COVID-19 PCR test result, and (3) patients with COVID-19 not hospitalized. Of the 3421 patients who met the inclusion criteria, we excluded 93 non-Japanese patients, 49 patients with unknown first PCR-positive result dates, and 18 patients not hospitalized. Finally, 3261 patients were included in the analysis (Fig. 2).
Flowchart describing patient selection. All consecutive patients with COVID-19 aged ≥ 18 years who were hospitalized during the study period (between February 2020 and September 2021) and recruited through the Japan COVID-19 Task Force were included. After excluding 160 patients, 3261 patients were enrolled in this study
Data collection
The following patient data were obtained from electronic case records: first PCR-positive result date, age, sex, body mass index, number of days in the hospital, comorbidities, and clinical symptoms (disturbance of consciousness, fever, malaise, cough/sputum, dyspnea, nasal discharge/pharyngeal pain, gastrointestinal symptoms: abdominal pain/diarrhea/nausea and vomiting, and taste and smell disturbances) during the course of infection. Similarly, we obtained data on laboratory and radiographic findings, complications after hospitalization, medication (ciclesonide, favipiravir, remdesivir, baricitinib, tocilizumab, and steroids), disease severity on admission, and worst condition during hospitalization.
Disease severity was determined considering oxygen requirement: low-flow oxygen therapy, high-flow oxygen therapy including high-flow nasal cannula oxygen therapy (HFNC) or non-invasive positive pressure ventilation, and invasive mechanical ventilation (IMV) [16, 21]. All laboratory and radiographic tests were performed within 48 h of the initial visit or admission according to clinical care needs of patients. A team of clinicians reviewed the collected data. If core data were missing, we contacted the clinician to collect the data. Missing data regarding patient background were assumed to be unknown.
Statistical analysis
Considering the first PCR-positive result date, the enrolled patients were classified into first–fifth COVID-19 wave groups and clinical characteristics of the patients were compared among the five COVID-19 wave groups. Categorical and continuous variables are presented as number (proportion) and mean ± standard deviation (SD), respectively. Data were compared using the χ2 test or Fisher’s exact test for categorical variables, as appropriate, and analysis of variance followed by the Tukey–Kramer method or Kruskal–Wallis test for continuous variables, as appropriate. Statistical significance was set at p < 0.05. Statistical analyses were performed using the JMP 16 program (SAS Institute Japan Ltd., Tokyo, Japan) and R version 4.1.3 (only for Fisher’s exact test). Visualization was performed using GraphPad Prism 9 (GraphPad Software, San Diego, California, USA) and the R package ggalluvial.
Results
Baseline characteristics of study participants
Baseline patient characteristics are shown in Table 1. The mean age of the 3261 patients with COVID-19 included in this study was 56.9 ± 17.4 years; 67.2% were men. The frequency of each comorbidity ranged from 4.1% to 34.6%. Hypertension (34.6%) and diabetes (21.2%) were the two most prevalent comorbidities.
Comparison of characteristics among first to fifth COVID-19 waves
Baseline patient characteristics for each COVID-19 wave are shown in Table 2 and Additional file 5; Table S5. The numbers of patients per COVID-19 wave enrolled in the study were 211, first COVID-19 wave; 837, second COVID-19 wave; 1,197, third COVID-19 wave; 552, fourth COVID-19 wave; and 464, fifth COVID-19 wave. There was a significant difference in the mean age among patients hospitalized during the five COVID-19 waves (p < 0.0001). The mean age was the lowest in the fifth COVID-19 wave. In addition, there was a significant difference in the number of hospitalization days among patients hospitalized during the five COVID-19 waves (p < 0.0001) with the highest number of hospitalization days recorded in the first COVID-19 wave.
Laboratory data and imaging findings are shown in Additional file 1: Tables S1 and Additional file 2: Table S2, respectively. There were significant differences in laboratory data such as C-reactive protein and D-dimer levels during the five COVID-19 waves (p < 0.0001). Specifically, the C-reactive protein and D-dimer levels were the highest in the first COVID-19 wave compared with other COVID-19 waves.
A comparison of the number of clinical symptoms observed in each COVID-19 wave is shown in Fig. 3A. There was a significant difference in the number of symptoms during the five COVID-19 waves (p < 0.0001). In the fifth COVID-19 wave, patients exhibited more symptoms than those in other COVID-19 waves. There were significant differences in symptoms observed during the five COVID-19 waves, such as fever, malaise, cough/sputum, dyspnea, and gastrointestinal symptoms (p < 0.0001) (Fig. 3B). These symptoms were most frequent in the fifth COVID-19 wave.
Comparison of clinical symptoms. The total number of eight clinical symptoms per COVID-19 wave of SD is shown A. In addition to analysis of variance, all COVID-19 waves were compared using the Tukey–Kramer method (fifth COVID-19 wave vs. first, second, third, and fourth COVID-19 waves: p < 0.0001). A comparison using analysis of variance for each of the eight clinical symptoms (disturbance of consciousness, p = 0.0291; fever, p < 0.0001; malaise, p < 0.0001; cough/sputum, p < 0.0001; dyspnea, p < 0.0001; nasal discharge/pharyngeal pain, p = 0.0256; gastrointestinal symptoms, abdominal pain/diarrhea/nausea and vomiting, p < 0.0001; and taste and smell disturbances, p < 0.0001) are shown in B
Comparison of medications prescribed per COVID-19 waves
A comparison of medications used in each COVID-19 wave is shown in Fig. 4. Significant differences in prescription rates were found among the five waves for all six drugs prescribed for hospitalized patients (p < 0.0001). Ciclesonide and favipiravir were used more frequently in the first COVID-19 wave; however, their frequency of use reduced subsequently. In contrast, remdesivir and steroids were used more frequently in the later COVID-19 waves. Baricitinib was administered from the third COVID-19 wave, and tocilizumab was more commonly used in the fifth COVID-19 wave.
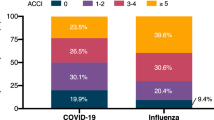
Comparison of severity of COVID-19
Figure 5 and Additional file 3: Table S3 show the change in severity of the COVID-19 waves at the worst patient condition during hospitalization and at admission. On admission and during the worst in progress, there was a significant difference in the percentage of patients requiring oxygen therapy during the five COVID-19 waves (p < 0.0001), with patients in the fifth COVID-19 wave including the highest percentage of patients requiring oxygen therapy. In addition, during the worst in progress, there was a significant difference in the percentage of patients on high-flow oxygen therapy and IMV during the five COVID-19 waves (p < 0.0001). The fifth COVID-19 wave had the highest percentage of patients on high-flow oxygen therapy, while the first COVID-19 wave had the highest percentage of patients on IMV. In addition, there was a significant difference in the percentage of in-hospital deaths, with the third COVID-19 wave including the highest percentage of in-hospital deaths.
Comparison of COVID-19 severity in each COVID-19 wave. The percentage of COVID-19 severity on admission and the worst condition during hospitalization: low-flow oxygen therapy, high-flow oxygen therapy (using high-flow nasal cannula oxygen therapy or non-invasive positive pressure ventilation) using invasive mechanical ventilation, and hospital death data are shown for each wave. The vertical axis of each wave shows rates of 0–100%
Complications after hospitalization are shown in Table 3 and Additional file 6: Table S6. There was a significant difference among the COVID-19 waves in complications, such as bacterial infection, heart failure, and thrombosis, during the five COVID-19 waves (p < 0.0001), as these were more common in the first COVID-19 wave than in other COVID-19 waves. Patient characteristics of in-hospital deaths were compared for each COVID-19 wave; there were significant differences in diabetes (p = 0.0201) and asthma (p = 0.0059) comorbidity; however, no other significant differences were found (Additional file 4: Table S4, Additional file 5: Table S5, Additional file 6: Table S6).
Discussion
In this study, the clinical characteristics of patients with COVID-19 were assessed for different epidemic waves of COVID-19 infection. To our knowledge, this is the first study to compare the detailed clinical characteristics of different COVID-19 waves over a long period of time. It is widely accepted that patient, viral, and social factors contribute in complex ways to the epidemic status of COVID-19 [22, 24]. Particularly, social factors may be diverse from country to country. The Japanese pandemic has been affected by changes in social policies at different time points, such as an increase in the number of people eligible for PCR testing, changes in admission and discharge criteria, and acceptance of patients presenting with mild symptoms of the disease [18]. Therefore, it is postulated that the clinical characteristics and outcomes of patients may differ between COVID-19 waves; however, no previous large-scale multicenter studies have examined this in detail. Consistent with this hypothesis, this study revealed highly distinctive differences in clinical characteristics among the five COVID-19 waves over 1.5 years.
The first COVID-19 wave had the highest percentage of intubated patients during the early stages of infection. The second COVID-19 wave had the largest proportion of young patients and the smallest proportion of patients requiring administration of oxygen. In the third COVID-19 wave, the number of infected patients increased more rapidly than that in the first and second COVID-19 waves, and the percentage of deaths was the highest in this wave. The fourth COVID-19 wave was dominated by the Alpha strain, which was more severe. More patients had required oxygen from the time of admission than that in first–third COVID-19 waves, causing a medical crisis. The fifth COVID-19 wave was dominated by the Delta strain, which was even more severe than the Alpha strain. The number of patients requiring oxygen therapy on admission was the highest during this phase. However, partly owing to advances in treatment and benefits of vaccination, a smaller percentage of patients died or required IMV during the course of admission, and a larger percentage of patients were able to survive up to the point of administration of low-flow or high-flow oxygen therapy [15,16,17, 21, 25, 26].
Previous studies reported the characteristics of patients with COVID-19 to the fourth COVID-19 wave in one prefecture in Japan [10, 13, 18]. However, the present study investigated differences in disease severity between different COVID-19 waves up to the fifth COVID-19 wave in multiple prefectures in Japan. In the first COVID-19 wave, the rate of the required IMV was higher than that in other COVID-19 waves. There are several possible explanations for this finding. First, there was no established treatment for COVID-19 during the first wave [15, 27, 28]. Second, the high incidence of nosocomial infections may have led to severe conditions in the elderly, with many risk factors [9, 10]. Third, the use of HFNC was avoided because of the risk of causing nosocomial infections by generating aerosols and dispersing the virus [29]. In the fourth and fifth COVID-19 waves, the number of patients requiring oxygen increased because of the effects of variants with a higher rate of severe disease manifestations [5, 6]. Meanwhile, there were fewer cases requiring IMV and fewer deaths in the fourth and fifth COVID-19 waves than in the third COVID-19 wave owing to the accumulation of evidence on the development of treatment methods and vaccination. It is noteworthy that in the fifth COVID-19 wave, which consisted primarily of the more virulent Delta variant, final severity of COVID-19 was reduced despite poor blood test results and severity of illness on admission. This indicates the effectiveness of the COVID-19 treatment and vaccination [15,16,17]. Furthermore, with each successive COVID-19 wave, the use of HFNC also increased in response to previous reports, and unnecessary IMV use is thought to have decreased as well [15,16,17, 21, 25, 30].
In this study, the mean age in the fourth COVID-19 wave was lower than that in the third COVID-19 wave [5] [12]. Also, the proportion of patients with severe disease was lower in the fifth COVID-19 wave than in previous COVID-19 waves. These differences may have resulted from the high vaccination rate among the Japanese elderly population. A previous report from Scotland showed that there were fewer severe cases and hospitalizations among elderly patients who had already been vaccinated at least once [31]. Japan implemented a policy of prioritizing vaccination of older adults at high risk of severe disease. The first round of vaccinations of the elderly population began on April 12, 2021, and by the end of July 2021, approximately 80% of older adults had received two doses of a COVID-19 vaccine [14]. This reduced the numbers of patients with serious illness and of hospitalizations among the elderly in the fourth and fifth COVID-19 waves [26].
In this study, ciclesonide and favipiravir were used more frequently in the early COVID-19 waves, while steroids, remdesivir, and baricitinib were used more frequently in the later COVID-19 waves. Currently, COVID-19 treatment is advancing rapidly [30]. Drugs such as ciclesonide and favipiravir, which were experimentally found to be effective, were used in the initial COVID-19 wave of infections [32, 33]. However, their use declined, as validation showed no clear effects [34, 35]. Thereafter, the efficacy of medications such as steroids, remdesivir, and baricitinib was reported [15, 16, 21, 25], and the use of these drugs increased after the third COVID-19 wave. Tocilizumab has also shown therapeutic efficacy [16]; however, its use was not as widespread as that of other drugs, partly because it was not approved for COVID-19 treatment in Japan during the fifth COVID-19 wave. These shifts in treatment are likely to have influenced patient outcomes in the different COVID-19 waves. Moreover, thrombosis and co-infection have been associated with the worst outcomes [36, 37]. Recently, appropriate antibiotic use and prophylactic anticoagulation have been recommended, particularly in severe cases [36, 38, 39]. In this study, there were fewer cases with thrombotic and co-infection complications in the later COVID-19 waves than in the first COVID-19 wave. However, no data were available on whether prophylactic anticoagulation or antimicrobial agents were used appropriately. Nonetheless, appropriate antibiotic use and prophylactic anticoagulation may have reduced these complications in the later COVID-19 waves. Furthermore, the characteristics of patients who died did not differ significantly among the different COVID-19 waves. These results may indicate that the characteristics of patients who died remain constant despite advances in treatment, and these patients may have required further therapeutic intervention. Future studies are warranted to investigate this hypothesis.
The percentage of patients who required oxygen therapy was low in the second COVID-19 wave. This is because PCR testing capabilities had improved compared with that in the first COVID-19 wave, allowing for early diagnosis and treatment. In addition, there was an increase in the number of young people infected, and the elderly, a high-risk group for severe disease, had refrained from leaving their homes [10, 11, 40]. However, in the second COVID-19 wave, no vaccine or treatment was established. In addition, the mortality rate was not significantly different from that in the first COVID-19 wave in the group of patients who required oxygen. From the third COVID-19 wave onward, the number of patients increased more rapidly than that in the first and second COVID-19 waves, and the health system became strained [11]. The third COVID-19 wave had the highest percentage of patients who died without IMV. This may be because the third COVID-19 wave included the highest average aged patients and the largest number of elderly patients, which may have led to a policy of not using IMV even when respiratory failure was severe and ventilator management was necessary.
Our study has several limitations. First, the ratio of the actual number of infected people to the number of patients enrolled in this study was different, and there may have been a selection bias. The largest number of patients was registered in the third COVID-19 wave, but not the fifth COVID-19 wave, which included the largest number of actual infections in Japan. In the fourth and fifth COVID-19 waves, the number of infected patients was high, and a medical crisis occurred, which made the registrars very busy. It is considered that the registration of clinical data did not continue [13]. Second, this study only included hospitalized patients; therefore, it does not reflect the overall picture of COVID-19 in Japan. This applies in particular to time after the third COVID-19 wave when the number of hospitalized patients with mild disease decreased in Japan as a whole. Third, the direct impact of the vaccine on disease severity could not be examined in this study because it was not known whether the patients had been vaccinated. Vaccination has been reported to prevent hospitalization and development of severe symptoms [26]. This may explain differences in outcomes between COVID-19 waves after vaccination became widespread in Japan. Fourth, this study does not consider confounding factors. Previous reports showed that several comorbidities affect the severity of COVID-19. Although viruses and vaccines are confounding factors, the failure to adjust for these confounding factors is a limitation of our study, as a variety of other patient background factors may also affect the severity of COVID-19 [41,42,43,44,45]. Fifth, we could not adjust the data by willingness to accept mechanical ventilation or the decision not to use mechanical ventilation ventilator. Therefore, we may have underestimated the proportion of patients who were severely ill. Further studies are required to confirm these findings.
Conclusions
We have identified the diverse clinical characteristics of hospitalized patients with COVID-19 in each COVID-19 wave up to the fifth wave in Japan. We found that the characteristics and severity of hospitalized patients with COVID-19 changed with changes in social conditions and use of therapeutic agents in Japan. In the fifth COVID-19 wave in which the Delta variant was the primary source of infection, many patients required oxygenation; however, compared with those in other COVID-19 waves, fewer patients had severe outcomes, such as IMV use or death. These findings may help the Japanese health system respond to future COVID-19 waves.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- HFNC:
-
High-flow nasal cannula oxygen therapy
- IMV:
-
Invasive mechanical ventilation
References
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–33.
Ministry of Health. Labour and Welfare, new coronavirus infection. https://www.mhlw.go.jp/stf/covid-19/kokunainohasseijoukyou.html. Accessed 1 October 2022.
Salyer SJ, Maeda J, Sembuche S, Kebede Y, Tshangela A, Moussif M, et al. The first and second waves of the COVID-19 pandemic in Africa: a cross-sectional study. Lancet. 2021;397:1265–75.
Rampal L, Liew BS. Malaysia’s third COVID-19 wave—a paradigm shift required. Med J Malaysia. 2021;76:1–4.
Twohig KA, Nyberg T, Zaidi A, Thelwall S, Sinnathamby MA, Aliabadi S, et al. Hospital admission and emergency care attendance risk for SARS-CoV-2 delta (B.1.617.2) compared with alpha (B.1.1.7) variants of concern: a cohort study. Lancet Infect Dis. 2022;22:35–42.
Challen R, Brooks-Pollock E, Read JM, Dyson L, Tsaneva-Atanasova K, Danon L. Risk of mortality in patients infected with SARS-CoV-2 variant of concern 202012/1: matched cohort study. BMJ. 2021;372: n579.
Our world in data, coronavirus pandemic. https://ourworldindata.org/coronavirus. Accessed 1 October 2022.
Vahidy FS, Drews AL, Masud FN, Schwartz RL, Askary BB, Boom ML, et al. Characteristics and outcomes of COVID-19 patients during initial peak and resurgence in the Houston metropolitan area. JAMA. 2020;324:998–1000.
Ide S, Morioka S, Sugai K, Kimura A, Kajio Y, Ohmagari N, et al. Experience in dealing with COVID-19 pandemic with original phasing in our hospital. J J Disa st Med. 2022;27:151–8.
Takeuchi T, Kitamura T, Hirayama A, Katayama Y, Shimazu T, Sobue T. Characteristics of patients with novel coronavirus disease (COVID-19) during the first surge versus the second surge of infections in Osaka Prefecture, Japan. Glob Health Med. 2021;3:82–9.
Karako K, Song P, Chen Y, Tang W, Kokudo N. Overview of the characteristics of and responses to the three waves of COVID-19 in Japan during 2020–2021. BioSci Trends. 2021;15:1–8.
Clinical management of patients with COVID-19. A guide for frontline healthcare workers. https://www.mhlw.go.jp/content/000851077.pdf. Accessed 1 October 2022.
Kurahara Y, Kobayashi T, Shintani S, Matsuda Y, Tamiya A, Sugawara R, et al. Clinical characteristics of COVID-19 in Osaka, Japan: comparison of the first-third waves with the fourth wave. Respir Investig. 2021;59:810–8.
Vaccination schedule for the COVID-19. https://www.kantei.go.jp/jp/headline/kansensho/vaccine_supply.html. Accessed 1 October 2022.
Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384:693–704.
Grein J, Ohmagari N, Shin D, Diaz G, Asperges E, Castagna A, et al. Compassionate use of remdesivir for patients with severe Covid-19. N Engl J Med. 2020;382(24):2327–36.
WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, Shankar-Hari M, Vale CL, Godolphin PJ, Fisher D, Higgins JPT, et al. Association between administration of IL-6 antagonists and mortality among patients hospitalized for COVID-19: a meta-analysis. JAMA. 2021;326:499–518.
Hattori T, Saito A, Chiba H, Kuronuma K, Amishima M, Morinaga D, et al. Characteristics of COVID-19 patients admitted into two hospitals in Sapporo, Japan: analyses and insights from two outbreak waves. Respir Investig. 2021;59:180–6.
Tanaka H, Lee H, Morita A, Namkoong H, Chubachi S, Kabata H, et al. Clinical characteristics of patients with coronavirus disease (COVID-19): preliminary baseline report of Japan COVID-19 task force, a nationwide consortium to investigate Host Genetics of COVID-19. Int J Infect Dis. 2021;113:74–81.
Namkoong H, Edahiro R, Fukunaga K, Shirai Y, Sonehara K, Tanaka H, et al. A nation-wide consortium to elucidate Host Genetics of COVID-19 Pandemic in Japan. medRxiv. 2021;2021.
Kalil AC, Patterson TF, Mehta AK, Tomashek KM, Wolfe CR, Ghazaryan V, et al. Baricitinib plus remdesivir for hospitalized adults with Covid-19. N Engl J Med. 2021;384:795–807.
Rosenbaum L. Facing Covid-19 in Italy: ethics, logistics, and therapeutics on the epidemic’s front line. Recenti Prog Med. 2020;111:192–7.
Kerlin MP, Costa DK, Davis BS, Admon AJ, Vranas KC, Kahn JM. Actions taken by US hospitals to prepare for increased demand for intensive care during the first wave of COVID-19: a national survey. Chest. 2021;160:519–28.
Lancet T. India’s COVID-19 emergency. Lancet. 2021;397:1683.
Chen CY, Chen WC, Hsu CK, Chao CM, Lai CC. Clinical efficacy and safety of Janus kinase inhibitors for COVID-19: a systematic review and meta-analysis of randomized controlled trials. Int Immunopharmacol. 2021;99: 108027.
Tenforde MW, Self WH, Adams K, Gaglani M, Ginde AA, McNeal T, et al. Association between mRNA vaccination and COVID-19 hospitalization and disease severity. JAMA. 2021;326:2043–54.
Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. A trial of lopinavir-ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020;382:1787–99.
Iwabuchi K, Yoshie K, Kurakami Y, Takahashi K, Kato Y, Morishima T. Therapeutic potential of ciclesonide inhalation for COVID-19 pneumonia: report of three cases. J Infect Chemother. 2020;26:625–32.
Recommendations to avoid NHF and NPPV Handling of ventilators and other equipment used in patients with novel coronavirus pneumonia - From the perspective of preventing infection via medical equipment—ver. 2.2. https://www.jsicm.org/news/upload/COVID-19-ventilator-V2.2.pdf. Accessed 1 October 2022.
van de Veerdonk FL, Giamarellos-Bourboulis E, Pickkers P, Derde L, Leavis H, van Crevel R, et al. A guide to immunotherapy for COVID-19. Nat Med. 2022;28:39–50.
Vasileiou E, Simpson CR, Shi T, Kerr S, Agrawal U, Akbari A, et al. Interim findings from first-dose mass COVID-19 vaccination roll-out and COVID-19 hospital admissions in Scotland: a national prospective cohort study. Lancet. 2021;397:1646–57.
Matsuyama S, Kawase M, Nao N, Shirato K, Ujike M, Kamitani W, et al. The inhaled steroid ciclesonide blocks SARS-CoV-2 RNA replication by targeting the viral replication-transcription complex in cultured cells. J Virol. 2020;95.
Cai Q, Yang M, Liu D, Chen J, Shu D, Xia J, et al. Experimental treatment with favipiravir for COVID-19: an open-label control study. Engineering (Beijing). 2020;6:1192–8.
Özlüşen B, Kozan Ş, Akcan RE, Kalender M, Yaprak D, Peltek İB, et al. Effectiveness of favipiravir in COVID-19: a live systematic review. Eur J Clin Microbiol Infect Dis. 2021;40:2575–83.
Hassanipour S, Arab-Zozani M, Amani B, Heidarzad F, Fathalipour M, Martinez-de-Hoyo R. The efficacy and safety of favipiravir in treatment of COVID-19: a systematic review and meta-analysis of clinical trials. Sci Rep Sci Rep. 2021;11:11022.
Garcia-Vidal C, Sanjuan G, Moreno-García E, Puerta-Alcalde P, Garcia-Pouton N, Chumbita M, et al. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: a retrospective cohort study. Clin Microbiol Infect. 2021;27:83–8.
Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, et al. COVID-19 and thrombotic or thromboembolic disease: Implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75:2950–73.
Kaptein FHJ, Stals MAM, Huisman MV, Klok FA. Prophylaxis and treatment of COVID-19 related venous thromboembolism. Postgrad Med. 2021;133(Suppl 1):27–35.
Nishimoto Y, Yachi S, Takeyama M, Tsujino I, Nakamura J, Yamamoto N, et al. The current status of thrombosis and anticoagulation therapy in patients with COVID-19 in Japan: from the CLOT-COVID study. J Cardiol. 2022;80:285–91.
Terada M, Ohtsu H, Saito S, Hayakawa K, Tsuzuki S, Asai Y, et al. Risk factors for severity on admission and the disease progression during hospitalisation in a large cohort of patients with COVID-19 in Japan. BMJ Open. 2021;11: e047007.
Lee H, Chubachi S, Namkoong H, Tanaka H, Otake S, Nakagawara K, et al. Effects of mild obesity on outcomes in Japanese patients with COVID-19: a nationwide consortium to investigate COVID-19 host genetics. Nutr Diabetes. 2022;12:38.
Fukushima T, Chubachi S, Namkoong H, Otake S, Nakagawara K, Tanaka H, et al. U-shaped association between abnormal serum uric acid levels and COVID-19 severity: reports from the Japan COVID-19 Task Force. Int J Infect Dis. 2022;122:747–54.
Hendren NS, de Lemos JA, Ayers C, Das SR, Rao A, Carter S, et al. Association of body mass index and age with morbidity and mortality in patients hospitalized With COVID-19: Results From the American Heart Association COVID-19 cardiovascular disease registry. Circulation. 2021;143:135–44.
Zhao Q, Meng M, Kumar R, Wu Y, Huang J, Lian N, et al. The impact of COPD and smoking history on the severity of COVID-19: a systemic review and meta-analysis. J Med Virol. 2020;92:1915–21.
Huang I, Lim MA, Pranata R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia—a systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr. 2020;14:395–403.
Acknowledgements
We would like to thank all participants involved in this study and all members of the Japan COVID-19 Task Force, who regularly engaged in clinical and research work on COVID-19. All the members contributed to this study. Details are provided in the consortium name section.
Consortium name
Ho Lee1, Shotaro Chubachi1, #, Ho Namkoong2, #, Takanori Asakura1, Hiromu Tanaka1, Shiro Otake1, Kensuke Nakagawara1, Atsuho Morita1, Takahiro Fukushima1, Mayuko Watase1, Tatsuya Kusumoto1, Katsunori Masaki1, Hirofumi Kamata1, Makoto Ishii1, Naoki Hasegawa2, Norihiro Harada3, Tetsuya Ueda4, Soichiro Ueda5, Takashi Ishiguro6, Ken Arimura7, Fukuki Saito8, Takashi Yoshiyama9, Yasushi Nakano10, Yoshikazu Mutoh11, Yusuke Suzuki12, Koji Murakami13, Yukinori Okada14,15,16, Ryuji Koike17, Yuko Kitagawa18, Akinori Kimura19, Seiya Imoto20, Satoru Miyano21, Seishi Ogawa22, Takanori Kanai23, Koichi Fukunaga1, Kazuhisa Takahashi3, Toshio Naito24, Makoto Hiki25,26, Yasushi Matsushita27, Haruhi Takagi3, Ryousuke Aoki28, Ai Nakamura3, Sonoko Harada3,29, Hitoshi Sasano3, Katsunori Masaki1, Shinnosuke Ikemura1, Satoshi Okamori1, Hideki Terai1, Takanori Asakura1, Junichi Sasaki30, Hiroshi Morisaki31, Yoshifumi Uwamino32, Kosaku Nanki23, Yohei Mikami23, Sho Uchida2, Shunsuke Uno2, Rino Ishihara23, Yuta Matsubara23, Tomoyasu Nishimura2,33, Takunori Ogawa1, Toshiro Sato34, Masanori Azuma4, Ryuichi Saito4, Toshikatsu Sado4, Yoshimune Miyazaki4, Ryuichi Sato4, Yuki Haruta4, Tadao Nagasaki4, Yoshinori Yasui4, Yoshinori Hasegawa4, Ai Tada5, Masayoshi Miyawaki5, Masaomi Yamamoto5, Eriko Yoshida5, Reina Hayashi5, Tomoki Nagasaka5, Sawako Arai5, Yutaro Kaneko5, Kana Sasaki5, Taisuke Isono6, Shun Shibata6, Yuma Matsui6, Chiaki Hosoda6, Kenji Takano6, Takashi Nishida6, Yoichi Kobayashi6, Yotaro Takaku6, Noboru Takayanagi6, Etsuko Tagaya7, Masatoshi Kawana35, Yasushi Nakamori8, Kazuhisa Yoshiya8, Fukuki Saito8,22, Tomoyuki Yoshihara8, Daiki Wada8, Hiromu Iwamura8, Syuji Kanayama8, Shuhei Maruyama8, Takanori Hasegawa21, Kunihiko Takahashi21, Tatsuhiko Anzai21, Satoshi Ito21, Akifumi Endo36, Yuji Uchimura37, Yasunari Miyazaki38, Takayuki Honda38, Tomoya Tateishi38, Shuji Tohda39, Naoya Ichimura39, Kazunari Sonobe39, Chihiro Tani Sassa39, Jun Nakajima39, Masumi Ai40, Ken Ohta9, Hiroyuki Kokuto9, Hideo Ogata9, Yoshiaki Tanaka9, Kenichi Arakawa9, Masafumi Shimoda9, Takeshi Osawa9, Yukiko Nakajima10, Ryusuke Anan10, Ryosuke Arai10, Yuko Kurihara10, Yuko Harada10, Kazumi Nishio10, Tomonori Sato49, Reoto Takei49, Satoshi Hagimoto49, Yoichiro Noguchi49, Yasuhiko Yamano49, Hajime Sasano49, Sho Ota49, Sohei Nakayama12, Keita Masuzawa12, Tomomi Takano50, Kazuhiko Katayama51, Koji Murakami52, Mitsuhiro Yamada52, Hisatoshi Sugiura52, Hirohito Sano52, Shuichiro Matsumoto52, Nozomu Kimura52, Yoshinao Ono52, Hiroaki Baba53, Rie Baba14, Daisuke Arai14, Takayuki Ogura14, Hidenori Takahashi14, Shigehiro Hagiwara14, Genta Nagao14, Shunichiro Konishi14, Ichiro Nakachi14, Hiroki Tateno47, Isano Hase47, Shuichi Yoshida47, Shoji Suzuki47, Miki Kawada48, Hirohisa Horinouchi49, Fumitake Saito50, Keiko Mitamura51, Masao Hagihara52, Junichi Ochi50, Tomoyuki Uchida52, Ryuya Edahiro14,45, Yuya Shirai14,53, Kyuto Sonehara14,54, Tatsuhiko Naito14, Kenichi Yamamoto14, Shinichi Namba14, Ken Suzuki14, Takayuki Shiroyama53, Yuichi Maeda53, Takuro Nii53, Yoshimi Noda53, Takayuki Niitsu53, Yuichi Adachi53, Takatoshi Enomoto53, Saori Amiya53, Reina Hara53, Noa Sasa16,55, Shuhei Yamada56, Toshihiro Kishikawa16,55,57, Kazunori Tomono58, Kazuto Kato59, Shuhei Yamada56, Yuya Ueno55, Motoyuki Suzuki55, Norihiko Takemoto55, Hirotaka Eguchi55, Takahito Fukusumi55, Takao Imai55, Munehisa Fukushima55,60, Masatoshi Takagaki56,61, Haruhiko Kishima56, Hidenori Inohara55, Haruhiko Hirata53, Yoshito Takeda53, Atsushi Kumanogoh53,54,61,62, Naoki Miyazawa63, Yasuhiro Kimura63, Reiko Sado63, Hideyasu Sugimoto63, Akane Kamiya64, Naota Kuwahara65, Akiko Fujiwara65, Tomohiro Matsunaga65, Yoko Sato65, Takenori Okada65, Takashi Inoue66, Toshiyuki Hirano66, Keigo Kobayashi66, Hatsuyo Takaoka66, Koichi Nishi67, Masaru Nishitsuji67, Mayuko Tani67, Junya Suzuki67, Hiroki Nakatsumi67, Hidefumi Koh68, Tadashi Manabe68, Yohei Funatsu68, Fumimaro Ito68, Takahiro Fukui68, Keisuke Shinozuka68, Sumiko Kohashi68, Masatoshi Miyazaki68, Tomohisa Shoko69, Mitsuaki Kojima69, Tomohiro Adachi69, Motonao Ishikawa70, Kenichiro Takahashi71, Kazuyoshi Watanabe72, Yoshihiro Hirai73, Hidetoshi Kawashima73, Atsuya Narita73, Kazuki Niwa74, Yoshiyuki Sekikawa74, Hisako Sageshima75, Yoshihiko Nakamura76, Kota Hoshino76, Junichi Maruyama76, Hiroyasu Ishikura76, Tohru Takata 77, Takashi Ogura78, Hideya Kitamura78, Eri Hagiwara78, Kota Murohashi78, Hiroko Okabayashi78, Takao Mochimaru79,80, Shigenari Nukaga79, Ryosuke Satomi79, Yoshitaka Oyamada80, Nobuaki Mori81, Tomoya Baba82, Yasutaka Fukui82, Mitsuru Odate82, Shuko Mashimo82, Yasushi Makino82, Kazuma Yagi83, Mizuha Hashiguchi83, Junko Kagyo83, Tetsuya Shiomi83, Kodai Kawamura84, Kazuya Ichikado84, Kenta Nishiyama84, Hiroyuki Muranaka84, Kazunori Nakamura84, Satoshi Fuke85, Hiroshi Saito85, Tomoya Tsuchida86, Shigeki Fujitani87, Mumon Takita87, Daiki Morikawa87, Toru Yoshida87, Takehiro Izumo88, Minoru Inomata88, Naoyuki Kuse88, Nobuyasu Awano88, Mari Tone88, Akihiro Ito89, Toshio Odani90, Masaru Amishima91, Takeshi Hattori91, Yasuo Shichinohe92, Takashi Kagaya93, Toshiyuki Kita93, Kazuhide Ohta93, Satoru Sakagami93, Kiyoshi Koshida93, Morio Nakamura93, Koutaro Yokote94, Taka-Aki Nakada95, Ryuzo Abe95, Taku Oshima95, Tadanaga Shimada95, Kentaro Hayashi96, Tetsuo Shimizu96, Yutaka Kozu96, Hisato Hiranuma96, Yasuhiro Gon96, Namiki Izumi97, Kaoru Nagata97, Ken Ueda97, Reiko Taki97, Satoko Hanada97, Naozumi Hashimoto98, Keiko Wakahara98, Koji Sakamoto98, Norihito Omote98, Akira Ando98, Yu Kusaka99, Takehiko Ohba99, Susumu Isogai99, Aki Ogawa99, Takuya Inoue99, Nobuhiro Kodama100, Yasunari Kaneyama100, Shunsuke Maeda100, Takashige Kuraki101, Takemasa Matsumoto101, Masahiro Harada102, Takeshi Takahashi102, Hiroshi Ono102, Toshihiro Sakurai102, Takayuki Shibusawa102, Yusuke Kawamura103, Akiyoshi Nakayama103, Hirotaka Matsuo103, Yoshifumi Kimizuka104, Akihiko Kawana104, Tomoya Sano104, Chie Watanabe104, Ryohei Suematsu104, Makoto Masuda105, Aya Wakabayashi105, Hiroki Watanabe105, Suguru Ueda105, Masanori Nishikawa105, Ayumi Yoshifuji106 Kazuto Ito106, Saeko Takahashi107, Kota Ishioka107, Yusuke Chihara108, Mayumi Takeuchi108, Keisuke Onoi108, Jun Shinozuka108, Atsushi Sueyoshi108, Yoji Nagasaki109, Masaki Okamoto110,111, Yoshihisa Tokunaga110,111, Sayoko Ishihara112, Masatoshi Shimo112, Masafumi Watanabe113, Sumito Inoue113, Akira Igarashi113, Masamichi Sato113, Nobuyuki Hizawa114, Yoshiaki Inoue115, Shigeru Chiba116, Kunihiro Yamagata117, Hirayasu Kai117, Yuji Hiramatsu118, Satoru Fukuyama119, Keiko Kan-o119, Koichiro Matsumoto119, Yoshihiro Eriguchi120, Akiko Yonekawa120, Kensuke Kanaoka121, Shoichi Ihara121, Kiyoshi Komuta121, Koichiro Asano122, Tsuyoshi Oguma122, Yoko Ito122, Satoru Hashimoto123, Masaki Yamasaki123, Yu Kasamatsu124, Yuko Komase125, Naoya Hida125, Takahiro Tsuburai125, Baku Oyama125, Yuichiro Kitagawa126, Tetsuya Fukuta126, Takahito Miyake126, Shozo Yoshida126, Shinji Ogura126, Minoru Takada127, Hidenori Kanda127, Shinji Abe128, Yuta Kono128, Yuki Togashi128, Hiroyuki Takoi128, Ryota Kikuchi128, Shinichi Ogawa129, Tomouki Ogata129, Shoichiro Ishihara129, Arihiko Kanehiro130,131, Shinji Ozaki130, Yasuko Fuchimoto130, Sae Wada130, Nobukazu Fujimoto131, Kei Nishiyama132, Mariko Terashima133, Satoru Beppu133, Kosuke Yoshida133, Osamu Narumoto134, Hideaki Nagai134, Nobuharu Ooshima134, Mitsuru Motegi135, Akira Umeda136, Kazuya Miyagawa137, Hisato Shimada138, Mayu Endo139, Yoshiyuki Ohira140, Hironori Sagara140, Akihiko Tanaka140, Shin Ohta140, Tomoyuki Kimura140, Yoko Shibata141, Yoshinori Tanino141, Takefumi Nikaido141, Hiroyuki Minemura141, Yuki Sato141, Yuichiro Yamada142, Takuya Hashino142, Masato Shinoki142, Hajime Iwagoe143, Hiroshi Takahashi144, Kazuhiko Fujii144, Hiroto Kishi144, Tomoo Ishii145, Masayuki Kanai146, Tomonori Imamura146, Tatsuya Yamashita146, Masakiyo Yatomi147, Toshitaka Maeno147, Shinichi Hayashi148, Mai Takahashi148, Mizuki Kuramochi148, Isamu Kamimaki148, Yoshiteru Tominaga148, Mitsuyoshi Utsugi149, Akihiro Ono149, Toru Tanaka150, Takeru Kashiwada150, Kazue Fujita150, Yoshinobu Saito150, Masahiro Seike150, Masahiro Kanai151, Ryunosuke Saiki152, Yasuhito Nannya152, Takayoshi Hyugaji153, Eigo Shimizu153, Kotoe Katayama153, Satoru Miyawaki154, Meiko Takahashi155, Fumihiko Matsuda155, Yosuke Omae156, Katsushi Tokunaga156, Takafumi Ueno157.
1Division of Pulmonary Medicine, Department of Medicine, Keio University School of Medicine, Tokyo, Japan.
2Department of Infectious Diseases, Keio University School of Medicine, Tokyo, Japan.
3Department of Respiratory Medicine, Juntendo University Faculty of Medicine and Graduate School of Medicine, Tokyo, Japan.
4Department of Respiratory Medicine, Osaka Saiseikai Nakatsu Hospital, Osaka, Japan.
5JCHO (Japan Community Health Care Organization) Saitama Medical Center, Internal Medicine, Saitama, Japan.
6Department of Respiratory Medicine, Saitama Cardiovascular and Respiratory Center, Kumagaya, Japan.
7Department of Respiratory Medicine, Tokyo Women's Medical University, Tokyo, Japan.
8Department of Emergency and Critical Care Medicine, Kansai Medical University General Medical Center, Moriguchi, Japan.
9Fukujuji Hospital, Kiyose, Japan.
10Department of Internal Medicine, Kawasaki Municipal Ida Hospital, Kawasaki, Japan.
11Department of Infectious Diseases, Tosei General Hospital, Seto, Japan.
12Department of Respiratory Medicine, Kitasato University Kitasato Institute Hospital, Tokyo, Japan.
13Department of Respiratory Medicine, Tohoku University Graduate School of Medicine, Sendai, Japan.
14Department of Statistical Genetics, Osaka University Graduate School of Medicine, Suita, Japan.
15Laboratory for Systems Genetics, RIKEN Center for Integrative Medical Sciences, Kanagawa, Japan.
16Department of Genome Informatics, Graduate School of Medicine, the University of Tokyo, Tokyo, Japan.
17Medical Innovation Promotion Center, Tokyo Medical and Dental University, Tokyo, Japan.
18Department of Surgery, Keio University School of Medicine, Tokyo, Japan.
19Institute of Research, Tokyo Medical and Dental University, Tokyo, Japan.
20Division of Health Medical Intelligence, Human Genome Center, the Institute of Medical Science, the University of Tokyo, Tokyo, Japan.
21M&D Data Science Center, Tokyo Medical and Dental University, Tokyo, Japan.
22Department of Pathology and Tumor Biology, Kyoto University, Kyoto, Japan.
23Division of Gastroenterology and Hepatology, Department of Medicine, Keio University School of Medicine, Tokyo, Japan.
24.Department of General Medicine, Juntendo University Faculty of Medicine and Graduate School of Medicine, Tokyo, Japan.
25Department of Emergency and Disaster Medicine, Juntendo University Faculty of Medicine and Graduate School of Medicine, Tokyo, Japan.
26Department of Cardiovascular Biology and Medicine, Juntendo University Faculty of Medicine and Graduate School of Medicine, Tokyo, Japan.
27Department of Internal Medicine and Rheumatology, Juntendo University Faculty of Medicine and Graduate School of Medicine, Tokyo, Japan.
28Department of Nephrology, Juntendo University Faculty of Medicine and Graduate School of Medicine, Tokyo, Japan.
29Atopy (Allergy) Research Center, Juntendo University Graduate School of Medicine, Tokyo, Japan.
30Department of Emergency and Critical Care Medicine, Keio University School of Medicine, Tokyo, Japan.
31Department of Anesthesiology, Keio University School of Medicine, Tokyo, Japan.
32Department of Laboratory Medicine, Keio University School of Medicine, Tokyo, Japan.
33Keio University Health Center, Keio University School of Medicine, Tokyo, Japan.
34Department of Organoid Medicine, Keio University School of Medicine, Tokyo, Japan.
35Department of General Medicine, Tokyo Women’s Medical University, Tokyo, Japan.
36Clinical Research Center, Tokyo Medical and Dental University Hospital of Medicine, Tokyo, Japan.
37Department of Medical Informatics, Tokyo Medical and Dental University Hospital of Medicine, Tokyo, Japan.
38Respiratory Medicine, Tokyo Medical and Dental University, Tokyo, Japan.
39Clinical Laboratory, Tokyo Medical and Dental University Hospital of Medicine, Tokyo, Japan.
40Department of Insured Medical Care Management, Tokyo Medical and Dental University Hospital of Medicine, Tokyo, Japan.
41Department of Respiratory Medicine and Allergy, Tosei General Hospital, Seto, Japan.
42School of Veterinary Medicine, Kitasato University, Towada, Japan.
43Laboratory of Viral Infection I, Department of Infection Control and Immunology, Ōmura Satoshi Memorial Institute & Graduate School of Infection Control Sciences, Kitasato University, Tokyo, Japan.
44Department of Respiratory Medicine, Tohoku University Graduate School of Medicine, Sendai, Japan.
45Department of Infectious Diseases, Tohoku University Graduate School of Medicine, Sendai, Japan.
46Saiseikai Utsunomiya Hospital, Utsunomiya, Japan.
47Department of Pulmonary Medicine, Saitama City Hospital, Saitama, Japan.
48Department of Infectious Diseases, Saitama City Hospital, Saitama, Japan.
49Department of General Thoracic Surgery, Saitama City Hospital, Saitama, Japan.
50Department of Pulmonary Medicine, Eiju General Hospital, Tokyo, Japan.
51Division of Infection Control, Eiju General Hospital, Tokyo, Japan.
52Department of Hematology, Eiju General Hospital, Tokyo, Japan.
53Department of Respiratory Medicine and Clinical Immunology, Osaka University Graduate School of Medicine, Suita, Japan.
54Integrated Frontier Research for Medical Science Division, Institute for Open and Transdisciplinary Research Initiatives, Osaka University, Suita, Japan.
55Department of Otorhinolaryngology-Head and Neck Surgery, Osaka University Graduate School of Medicine, Suita, Japan.
56Department of Neurosurgery, Osaka University Graduate School of Medicine, Suita, Japan.
57Department of Head and Neck Surgery, Aichi Cancer Center Hospital, Nagoya, Japan.
58Division of Infection Control and Prevention, Osaka University Hospital, Suita, Japan.
59Department of Biomedical Ethics and Public Policy, Osaka University Graduate School of Medicine, Suita, Japan.
60Department of Otolaryngology and Head and Neck Surgery, Kansai Rosai Hospital, Hyogo, Japan.
61Department of Immunopathology, Immunology Frontier Research Center (WPI-IFReC), Osaka University,
62The Center for Infectious Disease Education and Research (CiDER), Osaka University, Suita, Japan.
63Department of Respirtory Medicine, Saiseikai Yokohamashi Nanbu Hospital, Yokohama, Japan.
64Department of Clinical Laboratory, Saiseikai Yokohamashi Nanbu Hospital, Yokohama, Japan.
65Internal Medicine, Internal Medicine Center, Showa University Koto Toyosu Hospital, Tokyo, Japan.
66Internal Medicine, Sano Kosei General Hospital, Sano, Japan.
67Ishikawa Prefectural Central Hospital, Kanazawa, Japan.
68Tachikawa Hospital, Tachikawa, Japan.
69Department of Emergency and Critical Care Medicine, Tokyo Women’s Medical University Medical Center East, Tokyo, Japan.
70Department of Medicine, Tokyo Women's Medical University Medical Center East, Tokyo, Japan.
71Department of Pediatrics, Tokyo Women's Medical University Medical Center East, Tokyo, Japan.
72Japan Community Health care Organization Kanazawa Hospital, Kanazawa, Japan.
73Department of Respiratory Medicine, Japan Organization of Occupational Health and Safety, Kanto Rosai Hospital, Kawasaki, Japan.
74Department of General Internal Medicine, Japan Organization of Occupational Health and Safety, Kanto Rosai Hospital, Kawasaki, Japan.
75Sapporo City General Hospital, Sapporo, Japan.
76Department of Emergency and Critical Care Medicine, Faculty of Medicine, Fukuoka University, Fukuoka, Japan.
77Department of Infection Control, Fukuoka University Hospital, Fukuoka, Japan.
78Kanagawa Cardiovascular and Respiratory Center, Yokohama, Japan.
79Department of Respiratory Medicine, National Hospital Organization Tokyo Medical Center, Tokyo, Japan.
80Department of Allergy, National Hospital Organization Tokyo Medical Center, Tokyo, Japan.
81Department of General Internal Medicine and Infectious Diseases, National Hospital Organization Tokyo Medical Center, Tokyo, Japan.
82Department of Respiratory Medicine, Toyohashi Municipal Hospital, Toyohashi, Japan.
83Keiyu Hospital, Yokohama, Japan.
84Division of Respiratory Medicine, Social Welfare Organization Saiseikai Imperial Gift Foundation, Inc., Saiseikai Kumamoto Hospital, Kumamoto, Japan.
85KKR Sapporo Medical Center, Department of respiratory medicine, Sapporo, Japan.
86Division of General Internal Medicine, Department of Internal Medicine, St. Marianna University School of Medicine, Kawasaki, Japan.
87Departmet of Emergency and Critical Care Medicine, St. Marianna University School of Medicine,
88Japanese Red Cross Medical Center, Tokyo, Japan.
89Matsumoto City Hospital, Matsumoto, Japan.
90Department of Rheumatology, National Hospital Organization Hokkaido Medical Center, Sapporo, Japan.
91Department of Respiratory Medicine, National Hospital Organization Hokkaido Medical Center, Sapporo, Japan.
92Department of Emergency and Critical Care Medicine, National Hospital Organization Hokkaido Medical Center, Sapporo, Japan.
93NHO Kanazawa Medical Center, Kanazawa, Japan.
94Department of Endocrinology, Hematology and Gerontology, Chiba University Graduate School of Medicine, Chiba, Japan.
95Department of Emergency and Critical Care Medicine, Chiba University Graduate School of Medicine, Chiba, Japan.
96Nihon University School of Medicine, Department of Internal Medicine, Division of Respiratory Medicine, Tokyo, Japan.
97Musashino Red Cross Hospital, Musashino, Japan.
98Department of Respiratory Medicine, Nagoya University Graduate School of Medicine, Nagoya, Japan.
99Ome Municipal General Hospital, Ome, Japan.
100Fukuoka Tokushukai Hospital, Department of Internal Medicine, Kasuga, Japan.
101Fukuoka Tokushukai Hospital, Respiratory Medicine, Kasuga, Japan.
102National Hospital Organization Kumamoto Medical Center, Kumamoto, Japan.
103Department of Integrative Physiology and Bio-Nano Medicine, National Defense Medical College, Tokorozawa, Japan.
104Division of Infectious Diseases and Respiratory Medicine, Department of Internal Medicine, National Defense Medical College, Tokorozawa, Japan.
105Department of Respiratory Medicine, Fujisawa City Hospital, Fujisawa, Japan.
106Department of Internal Medicine, Tokyo Saiseikai Central Hospital, Tokyo, Japan.
107Department of Pulmonary Medicine, Tokyo Saiseikai Central Hospital, Tokyo, Japan.
108Uji-Tokushukai Medical Center, Uji, Japan.
109Department of Infectious Disease and Clinical Research Institute, National Hospital Organization Kyushu Medical Center, Fukuoka Japan.
110Department of Respirology, National Hospital Organization Kyushu Medical Center, Fukuoka, Japan.
111Division of Respirology, Rheumatology, and Neurology, Department of Internal Medicine, Kurume University School of Medicine, Kurume, Japan.
112Department of Infectious Disease, National Hospital Organization Kyushu Medical Center, Fukuoka Japan.
113Department of Cardiology, Pulmonology, and Nephrology, Yamagata University Faculty of Medicine, Yamagata, Japan.
114Department of Pulmonary Medicine, Faculty of Medicine, University of Tsukuba, Tsukuba, Japan.
115Department of Emergency and Critical Care Medicine, Faculty of Medicine, University of Tsukuba, Tsukuba, Japan.
116Departmentof Hematology, Faculty of Medicine, University of Tsukuba, Tsukuba, Japan.
117Department of Nephrology, Faculty of Medicine, University of Tsukuba, Tsukuba, Japan.
118Department of Cardiovascular Surgery, Faculty of Medicine, University of Tsukuba, Tsukuba, Japan.
119Research Institute for Diseases of the Chest, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan.
120Department of Medicine and Biosystemic Science, Kyushu University Graduate School of Medical Sciences, Fukuoka, Japan.
121Daini Osaka Police Hospital, Osaka, Japan.
122Division of Pulmonary Medicine, Department of Medicine, Tokai University School of Medicine, Isehara, Japan.
123Department of Anesthesiology and Intensive Care Medicine, Kyoto Prefectural University of Medicine, Kyoto, Japan.
124Department of Infection Control and Laboratory Medicine, Kyoto Prefectural University of Medicine, Kyoto, Japan.
125Department of Respiratory Internal Medicine, St. Marianna University School of Medicine, Yokohama-City Seibu Hospital, Yokohama, Japan.
126Gifu University School of Medicine Graduate School of Medicine, Emergency and Disaster Medicine, Gifu, Japan.
127KINSHUKAI Hanwa The Second Hospital, Osaka, Japan.
128Department of Respiratory Medicine, Tokyo Medical University Hospital, Tokyo, Japan.
129JA Toride medical hospital, Toride, Japan.
130Okayama Rosai Hospital, Okayama, Japan.
131Himeji St. Mary’s Hospital, Himeji, Japan.
132Emergency & Critical Care, Niigata University, Niigata, Japan.
133Emergency & Critical Care Center, National Hospital Organization Kyoto Medical Center, Kyoto, Japan.
134National Hospital Organization Tokyo National Hospital, Kiyose, Japan.
135Fujioka General Hospital, Fujioka, Japan.
136Department of General Medicine, School of Medicine, International University of Health and Welfare Shioya Hospital, Ohtawara Japan.
137Department of Pharmacology, School of Pharmacy, International University of Health and Welfare Shioya Hospital, Ohtawara Japan.
138Department of Respiratory Medicine, International University of Health and Welfare Shioya Hospital, Ohtawara Japan.
139Department of Clinical Laboratory, International University of Health and Welfare Shioya Hospital, Ohtawara Japan.
140Department of General Medicine, School of Medicine, International University of Health and Welfare, Narita Japan.
141Department of Pulmonary Medicine, Fukushima Medical University, Fukushima, Japan.
142Kansai Electric Power Hospital, Osaka, Japan.
143Department of Infectious Diseases, Kumamoto City Hospital, Kumamoto, Japan.
144Department of Respiratory Medicine, Kumamoto City Hospital, Kumamoto, Japan.
145Tokyo Medical University Ibaraki Medical Center, Inashiki, Japan.
146Department of Emergency and Critical Care Medicine, Tokyo Metropolitan Police Hospital, Tokyo, Japan.
147Department of Respiratory Medicine, Gunma University Graduate School of Medicine, Maebashi, Japan.
148National hospital organization Saitama Hospital, Wako, Japan.
149Department of Internal Medicine, Kiryu Kosei General Hospital, Kiryu, Japan.
150Department of Pulmonary Medicine and Oncology, Graduate School of Medicine, Nippon Medical School, Tokyo, Japan.
151Department of Biomedical Informatics, Harvard Medical School, Boston, MA, USA.
152Department of Pathology and Tumor Biology, Kyoto University, Kyoto, Japan.
153Division of Health Medical Intelligence, Human Genome Center, the Institute of Medical Science, the University of Tokyo, Tokyo, Japan.
154Department of Neurosurgery, Faculty of Medicine, the University of Tokyo, Tokyo, Japan.
155Center for Genomic Medicine, Kyoto University Graduate School of Medicine, Kyoto, Japan.
156Genome Medical Science Project (Toyama), National Center for Global Health and Medicine, Tokyo, Japan.
157Department of Biomolecular Engineering, Graduate School of Tokyo Institute of Technology, Tokyo, Japan.
Funding
This study was supported by AMED (JP20nk0101612, JP20fk0108415, JP21jk0210034, JP21km0405211, JP21km0405217), JST CREST (JPMJCR20H2), MHLW (20CA2054), Takeda Science Foundation, Mitsubishi Foundation, and the Bioinformatics Initiative of Osaka University Graduate School of Medicine, Osaka University.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: HL, SC, HN, TA, KM, HK, MI, NH, and KF. Data curation: HL, KN, HT, SO, AM, TF, MW, and TK. Formal analysis: HL, SC. Methodology: HL, SC, TA, and HN. Supervision: HL, NH, KM, HK, MI, NH, NH, TU, SU, TI, KA, FS, TY, YN, YM, YS, KM, YO, RK, YK, AK, SI, SM, SO, TK, and KF. Visualization: HL and HN. Writing—original draft: HL, SC, and TA. Writing—review and editing: HL, SC, NH, TA, KM, HK, MI, NH, NH, TU, SU, TI, KA, FS, TY, YN, YM, YS, KM, YO, RK, YK, AK, SI, SM, SO, TK, and KF. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Keio University School of Medicine (ID:20200061), and written, or oral informed consent was obtained from all participants. The study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Supplementary Table 1.
Comparison of laboratory parameters.
Additional file 2. Supplementary Table 2.
Comparison of imaging findings.
Additional file 3. Supplementary Table 3.
Comparison of severity of COVID-19 patients.
Additional file 4. Supplementary Table 4.
Comparison of patient characteristics among in-hospital deaths.
Additional file 5. Supplementary Table 5.
Clinical characteristics of Japanese COVID-19 patients by infection waves with p value.
Additional file 6. Supplementary Table 6.
Complications after hospitalization by COVID-19 waves with p value.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lee, H., Chubachi, S., Namkoong, H. et al. Characteristics of hospitalized patients with COVID-19 during the first to fifth waves of infection: a report from the Japan COVID-19 Task Force. BMC Infect Dis 22, 935 (2022). https://doi.org/10.1186/s12879-022-07927-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07927-w