Abstract
Background
To gain insight into the impact of the COVID-19 pandemic and containment measures on the HIV epidemic and services, this study aims to describe HIV trends in 2020 and compare them with previous years.
Methods
Belgian national HIV surveillance data 2017–2020 were analysed for trends in HIV testing, HIV diagnoses, VL measurements, ART uptake and PrEP purchase. Descriptive statistics from 2020 are compared to annual averages from 2017 to 2019 (proportional difference, %).
Results
In 2020, 725 HIV infections were diagnosed in Belgium (− 21.5% compared to 2019). The decline was most pronounced during the first lockdown in April–May but also present in July–December. The number of HIV tests performed decreased by 17.6% in 2020, particularly in March–May and October–December (− 57.5% in April and -25.4% in November 2020 compared to monthly 2017–19 numbers). Diagnosis of acute HIV infections decreased by 47.1% in 2020 (n = 27) compared to 2019 (n = 51). Late HIV diagnoses decreased by 24.7% (95% CI [− 40.7%; -9.7%]) in 2020 compared to 2019. Of patients in care in 2019, 11.8% interrupted HIV care in 2020 compared to 9.1% yearly in the 3 previous years. The number of HIV patients with VL monitoring per month dropped in March–May 2020, whilst proportions of VL suppression and ART coverage remained above 86% and 98.5% respectively in 2020. PrEP purchases, number of purchasers and starters dropped during April–May 2020 (respectively − 45.7%, − 47.4%, − 77.9% in April compared to February 2020).
Conclusions
The significant decrease in HIV diagnoses in Belgium in 2020 coincided with the COVID-19 pandemic and following containment measures, particularly in April–May during the first lockdown. A slowdown of HIV transmission due to reduced HIV risk exposure is suggested by the halving in diagnosis of acute HIV infections in March-December 2020 compared to the previous year, and the adaptive decrease in PrEP use and PrEP initiation from April onwards. Despite a slight increase in HIV care interruptions, the indicators of quality of HIV care remained stable. Access to prevention, testing and care for all people living with HIV and at risk of acquiring HIV is a priority during and after times of pandemic.
Similar content being viewed by others
Background
The COVID-19 pandemic has created an unprecedented public health emergency worldwide. In response to multiple outbreaks from January 2020 onwards, global measures were put in place to contain the circulation of SARS-CoV-2. In Belgium, restrictions culminated during two lock-down periods in 2020: from the 18th of March with progressive reopening from the 4th of May, and from the 2nd of November with gradual release from the 1st of December. Travel restrictions, ban on public gatherings and the closure of schools and non-essential services were imposed, as well as the suspension of non-urgent medical care and prevention services.
Several observational studies have shown the major impact of the COVID-19 pandemic and the resulting measures on the provision of HIV services as well as on the evolution of the HIV epidemic [1,2,3]. Health promotion, prevention and support organisations tried to adapt their services to this exceptional situation of reduced physical contact and lock-down. In consequence, ongoing programs were interrupted or reprogrammed to focus on the urgent needs related to COVID-19 prevention and care [4]. Interruption of medical services had an impact on the provision of healthcare for people with HIV (PWH) and pre-exposure prophylaxis (PrEP). Moreover, health facilities and staff, particularly infectious disease specialists, were mobilized to contribute to the pandemic response. As a consequence, non-urgent HIV-related medical care was cancelled or converted to telephone or online consultations [5].
The objective of this study is to describe the trends of the HIV epidemic in the first year of the COVID-19 pandemic in Belgium and compare them with previous years.
Methods
Study setting and population
In Belgium, all HIV diagnoses and viral load measurements are performed by specialized AIDS Reference Laboratories (ARL). The HIV Reference Centers (HRC) are specialized tertiary care structures offering multi-disciplinary care for PWH. More than eighty percent of HIV patients are followed up in those centers. Alternatively, HIV patients are followed up in other hospitals and, although less frequently, in primary care.
PrEP delivery has been implemented and reimbursed in Belgium since June 2017. Emtricitabine/tenofovir as PrEP, in boxes of 30 or 90 pills, might be purchased from public pharmacies, and less frequently from hospital pharmacies (13% of purchases).
Access to HIV testing and care is covered by the national compulsory health insurance for Belgians and non-Belgians legally residing in Belgium. European Union (EU) nationals get similar access through their home country’s health insurance. For undocumented non-EU migrants, access to healthcare is ensured by a process of “Urgent medical aid”, although in practice administrative barriers and restrictions are often faced.
Data collection
As national HIV surveillance team from Sciensano, the Belgian institute for health, we collect individual HIV diagnostic and viral load data annually from the ARL, including demographic information while the HRC report routine individual demographic, medical, treatment and laboratory data from the patients in care. In addition, claim data on testing for HIV and on PrEP delivery in public pharmacies are obtained from the National Institute for Health and Disability Insurance. This allows for a national exhaustive surveillance covering all people tested for HIV, all those diagnosed with HIV, all those in HIV care and all people using PrEP (except those purchasing PrEP solely in hospital pharmacies).
Sciensano is legally entitled to conduct this HIV surveillance, which has been approved by an independent administrative authority protecting privacy and personal data [6].
Statistical analysis
We selected surveillance data from the 1st of January 2017 to the 31st of December 2020. Yearly and monthly trends in HIV tests, HIV diagnoses, viral load measurements, ART uptake and PrEP purchase were analysed. Missing data values were enriched through linkages between diagnosis and care registers. Additionally, multiple imputation was applied on the diagnosis data for remaining missing variables, as advised as an adjustment method to account for missing data in HIV surveillance in Europe [7]. This allowed monitoring of the trends in number of HIV diagnoses per demographic group without introducing a bias related to varying missing data over time. The R package “mice” was used to construct 10 multiply imputed datasets [8]. A non-parametric classification and regression tree was used as imputation method for all variables as this is known to preserve interactions between variables and is thus well suited to capture differential changes over time of different groups [9]. Descriptive statistics based on imputed data were pooled across multiply imputed datasets using Rubin’s rules [8] and presented as point estimates and 95% CI. Statistics related to the number of diagnoses, diagnostic tests and PrEP purchases are presented as point estimates as they are based on exhaustive and complete data.
Results
In 2020, 725 diagnoses of HIV infection were confirmed in Belgium, this is a decrease of 21.5% compared to 2019 (N = 926). In the 3 preceding years (2017–2019), no decline in the number of HIV diagnoses was recorded (mean yearly change = − 0.006%). The decline in the number of HIV diagnoses in 2020 compared to 2017–2019 was particularly pronounced in women (− 25.9%), people < 30 years of age (− 25.6%) and people of Belgian (− 34.6%) and Sub-Saharan African nationalities (-31.3%). Socio-demographic characteristics of diagnosed PWH are presented in Table 1.
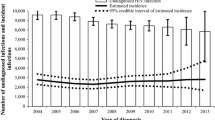
The decline in HIV diagnoses in 2020 was most pronounced during the first lockdown from April to May but was also noticed from July to the end of 2020 (Fig. 1). A clear monthly reduction of the number of HIV diagnoses was observed among Belgian MSM and heterosexuals throughout 2020 (Fig. 2). For non-Belgians, a higher variability per month was seen with a pronounced drop in April.
A total of 629 063 HIV tests were performed in 2020, representing a testing rate of 56 per 1000 population. Between 2019 and 2020, the number of tests performed decreased by 17.6%. The number of HIV tests carried out from March to May and from October to December 2020 decreased substantially compared to the monthly number of tests carried out in 2017–19 (− 57.5% in April and − 25.4% in November 2020). From March to May 2020, the ratio of new diagnoses per test was higher (1.5 new diagnoses/1000 tests) than the annual average of previous years of 1.2 new diagnoses/1000 tests. It reduced in the following months and was very low from July to September 2020 (0.9 new diagnoses/1000 tests) (Fig. 1).
The number of laboratory-identified acute infections, defined by the presence of p-24 antigen or plasma viral RNA in combination with a negative or indeterminate immunoassay result (InnoLIA or Geenius), decreased by 47.1% in 2020 compared to 2019 (n = 27 and n = 51 respectively). No acute infections were diagnosed in April and November 2020, and the number remained low (1–2 per month) in the following months until the end of the year, except for September (4 acute infections). Belgian MSM have the highest probability of being diagnosed during acute infection (54.5% of the acute infections between 2017 and 2020 were Belgian MSM), and it is among them that the largest decrease was observed (-67.5% in 2020 compared to 2019; 95% CI [− 89.4%; − 45.6%]).
In 2020, 34.2% of the infections were diagnosed late (defined as CD4 < 350 cells/mm3 or AIDS and no indication of a recent infection). The proportion of late diagnoses was higher among non-Belgians (37.1%) than among Belgians (27.8%). Overall, the number of late HIV diagnoses decreased by 24.7% (95% CI [− 40.7%; − 9.7%]) in 2020 compared to 2019. The decrease was most pronounced between March and May and between July and August, while the number of late diagnoses in the rest of the year was similar to previous years. The number of late diagnoses was reduced by 28.3% (95% CI [− 50.2%; − 6.4%]) among MSM, by 17.4% (95% CI [− 32.3%; − 2.4%]) among heterosexuals, by 40.6% (95% CI [− 57.8%; − 23.4%]) among Belgians and by 10.3% (95% CI [− 26.5%; + 5.8%]) among non-Belgians.
In 2020, 17,018 HIV patients were in care in Belgium. While the number of patients in HIV care increased steadily by a mean of 492 persons each year from 2017 to 2019, it reduced by 139 in 2020. Of the 17,157 patients in care in the preceding year, 2032 (11.8%) did not have a record of CD4 measurement, VL measurement or HRC medical visit in 2020. In comparison, in 2017–2019, an average of 9.1% was interrupting HIV care each year.
The monthly number of HIV patients with viral load monitoring decreased significantly during the first COVID-19 lockdown from March to May 2020 (Fig. 3). A slight catch-up was then observed in June. From July onwards, the number of patients undergoing virological monitoring was comparable to previous years. Throughout 2020, the proportion of VL suppression among monitored patients remained above 86%. Data on antiretroviral therapy (ART) in the HRC showed that ART coverage remained high among patients in HIV care at 98.5% in 2020.
Since June 2017, the number of PrEP users has steadily increased. In 2020, 3983 persons purchased PrEP in public pharmacies, which represents an increase of 12.1% compared to 2019. The overall number of PrEP pills purchased in 2020 remained stable compared to 2019 (respectively 776,790 vs 727,770). PrEP purchases and number of purchasers dropped during the months of April and May 2020 (by respectively 33,180 (− 45.7%) and 398 (− 47.4%) in April compared to February 2020) (Fig. 4). Number of PrEP starters also reduced during the lock-down by 134 (− 77.9%) in April compared to February 2020.
Discussion
Our study provided strong indications that the decrease in HIV diagnoses in Belgium in 2020 was linked to the COVID-19 pandemic and the imposed containment measures. Indeed, the decline of HIV diagnoses was most pronounced during the first lockdown in April–May. In the following months, with the exception of June, the number of diagnoses remained significantly lower than in previous years. In contrast, HIV care indicators such as viral suppression and ART coverage remained good though a slight increase in HIV care interruption was observed in 2020.
As also observed in other countries, the decrease in HIV diagnoses in Belgium largely coincided with a reduction in testing activities [1, 10]. This reduction was reported in health care facilities and in community based testing services which target specific key populations [4]. The amount of tests performed depends on the available and accessible offer and the clients’ or patients’ demand, which in turn is also influenced by (self-perceived) risk of HIV infection.
During the months of March to May 2020, whilst access to testing facilities was very limited leading to a decrease in test offer, the ratio of diagnoses per test was higher than the annual average of previous years. This suggests a restriction of testing towards those at high risk or with suggestive clinical symptoms. Between June and September, access to testing normalised with a similar number of tests per month as in previous years. The ratio of diagnoses per test was very low in the summer months, suggesting an extension of testing to less urgent or less specific indications, which were postponed during the lock-down period.
Several studies suggest that HIV transmission may have been reduced by the decrease in sexual interactions with casual partners due to the restriction of physical and social contacts during the periods of strict confinement [11]. An online survey among MSM in Belgium showed a sharp drop in the number of casual sex partners during the first lock-down period from March to May 2020 [12]. Similar results were observed in studies in the Netherlands [13], United Kingdom [14, 15] and Australia [16].
A first observation that is in line with those studies showing a lower risk of HIV transmission in this period is the halving of the number of acute HIV diagnoses from March 2020 to the end of the year compared to the previous year. Diagnoses during the acute phase of HIV infection have decreased significantly more than the HIV diagnoses in general, while during acute infection a large majority of patients present with clinical symptoms, which may draw clinicians’ to this differential diagnosis, as opposed to established HIV infection. However, it cannot be excluded that some diagnoses of acute infections may have been missed as HIV acute infection may mimic COVID-19 symptoms [17].
A second observation in the same direction is the decrease in the purchase of PrEP pills and the number of PrEP purchasers from April 2020 onwards, meaning that some users have reduced or suspended their PrEP use, and very few initiated PrEP. Studies among PrEP users indicated that they tailor their PrEP use according to their risk exposure [18,19,20]. Continued use of PrEP during periods of lockdown was found to be associated with having sex with casual partners [12]. It can therefore be assumed that PrEP use patterns were adapted by users according to the perceived needs, potentially allowing PrEP to continue playing its role in reinforcing combination prevention.
HIV diagnoses among heterosexuals are still mainly reported in people of sub-Saharan African origin followed by people of other non-Belgian nationalities. Among non-Belgians, the decrease in HIV diagnoses was mainly observed during the COVID-19 lockdown periods when travel restrictions were in place. The pandemic has had a major impact on international migration flows to Belgium (-15.5% international immigrations in 2020 compared to 2017–19 [21]) and in consequence, most likely, on the number of non-Belgian PWH whose diagnosis was confirmed after arrival in Belgium.
In parallel to the decrease in the overall number of HIV diagnoses, there was a decrease in the number of late diagnoses. On the one hand, travel restrictions and reduced migration during the lockdown periods may have had an impact on the number of late diagnoses among non-Belgians, although this number decreased only minimally compared to previous years. On the other hand, limited accessibility to testing facilities also played a role and may have increased the delay in diagnosis for some people, as reported in the Netherlands where more advanced disease was observed at entry in clinical care after the lockdown periods [22]. Though no rebound with an increase in late diagnoses post lock-down was noticed in Belgium until end 2020, which is a preliminary reassuring signal. The trend in late diagnoses in the following year will be monitored to reappraise the extent to which HIV diagnoses were missed in 2020.
As a result of the social and physical distancing, as well as shift from the infectious diseases dedicated staff to COVID-19 care, the organization of the HIV-care had to be adapted during the periods of lockdown, with an impetus for alternative strategies such as telemedicine [5, 23]. This adaptation of care is illustrated by the reduced number of viral load tests performed during the months of March to May, linked to the postponement of these tests in clinically stable patients. A similar trend was observed in a monocentric study in Belgium [23]. Nevertheless, the antiretroviral treatment coverage remained high in 2020 and very effective in controlling the viral load of HIV-positive patients in care. The feasibility and positive experience of this digital switch supports its use in future routine HIV care.
Similarly, prevention services had to be adapted during lock-down: renewal of the PrEP prescriptions could be done remotely by the physician allowing the collection of the PrEP pills at the pharmacy. Field prevention and support organizations reinvented their action package to adapt to the pandemic by informing PWH about COVID-19 vaccines and providing support in making vaccine appointments. The link with the community was maintained by switching to online prevention, support and sharing groups and supportive phone calls. Testing was supported through the distribution of HIV self-tests (T. Martin, Director Plateforme Prévention SIDA, personal communication, April 19, 2022). Harm-reduction services also had to adapt their service offer during the lock-down periods by limiting or stopping the public reception, introducing online support, adjusting syringe exchange programs and providing information and education on COVID-19 prevention [24].
Finally, structural inequalities related to poverty and migration may have been exacerbated during the COVID-19 pandemic, potentially limiting access to health services for vulnerable populations even more than before [25,26,27]. Our results show indeed a slight increase in HIV care interruption in 2020. The results of a study conducted among PWH revealed that the negative impact of COVID-19 was more important in the most vulnerable PWH. The reported reasons include an increased fear of COVID-19 infection, greater sense of isolation for PWH living alone, deterioration of financial situation especially for those in the informal economy, and increased uncertainty of legal status for asylum seekers. For some, this led to weight gain and bad habits such as alcohol use and other addictions (Thierry Martin, Director Plateforme Prévention SIDA, personal communication, April 19, 2022). Therefore it is essential, particularly during a pandemic period, that prevention and testing facilities as well as care are inclusive and accessible to all affected populations.
Conclusions
The pandemic and the containment measures affected several determinants of HIV infection, diagnosis and care as discussed above including access to prevention, testing and care services, sexual behaviour and migration dynamics. The COVID-19 pandemic significantly slowed down HIV transmission in 2020, mainly during the lockdown periods but also in the following months. Missed HIV diagnoses related to testing restrictions might have occurred but this will only be confirmed by looking at future trends. The resilient and adaptive health care system has made it possible to maintain the quality of HIV care in Belgium, although the number of HIV care interruptions increased slightly. After this long-lasting crisis, health policies should aim to support health professionals and organizations in resuming routine care and support for all PWH particularly for the most vulnerable which are at greater risk of loss to follow-up. Prevention and testing services should remain accessible during times of lockdown with an increased focus on those who continue to engage in high risk sexual practices during the pandemic.
Availability of data and materials
The data that support the findings of this study are available on request from the corresponding author [DVB] upon approval of a project proposal to the HIV surveillance Steering Committee and clearance by the Belgian Information Security Committee.
Abbreviations
- ART:
-
Antiretroviral therapy
- HIV:
-
Human Immunodeficiency virus
- HRC:
-
HIV reference center
- MSM:
-
Men having sex with men
- PrEP:
-
Pre-exposure prophylaxis
- PWH:
-
People with HIV
References
Darcis G, Vaira D, Moutschen M. Impact of coronavirus pandemic and containment measures on HIV diagnosis. Epidemiol Infect. 2020. https://doi.org/10.1017/S0950268820001867.
Rao A, Rucinski K, Jarrett BA, Ackerman B, Wallach S, Marcus J, et al. Perceived interruptions to HIV prevention and treatment services associated with COVID-19 for gay, bisexual, and other men who have sex with men in 20 countries. JAIDS J Acquir Immune Defic Syndr. 2021;87(1):644–51.
Jiang T, Liu C, Zhang J, Huang X, Xu J. Impact of the COVID-19 pandemic on the UNAIDS Six 95% HIV control targets. Front Med (Lausanne). 2022;18(9): 818054. https://doi.org/10.3389/fmed.2022.818054.
Simões D, Stengaard AR, Combs L, Raben D. EuroTEST COVID-19 impact assessment consortium of partners. Impact of the COVID-19 pandemic on testing services for HIV, viral hepatitis and sexually transmitted infections in the WHO European Region March to August 2020. Euro Surveill Bull Eur Sur Mal Transm Eur Commun Dis Bull. 2020. https://doi.org/10.2807/1560-7917.ES.2020.25.47.2001943.
Peek N, Sujan M, Scott P. Digital health and care in pandemic times: impact of COVID-19. BMJ Health Care Inform. 2020;27(1): e100166.
Comité de sécurité de l’information - Chambre sécurité sociale et santé. Délibération n° 14/017 du 18 février 2014, modifiée en dernier lieu le 7 avril 2020, dans le cadre de la surveillance épidémiologique du VIH et du sida en Belgique [Internet]. https://www.ehealth.fgov.be/ehealthplatform/file/view/AXGB4AUNix91GfOxg0HU?filename=14-017-f140-VIH%20et%20SIDA%20en%20Belgique-modifi%C3%A9e%20le%207%20avril%202020.pdf. Accessed 13 Apr 2022.
Rosinska M, Pantazis N, Janiec J, Pharris A, Amato-Gauci AJ, Quinten C, ECDC HIV/AIDS Surveillance Network. Potential adjustment methodology for missing data and reporting delay in the HIV Surveillance System, European Union/European Economic Area 2015. Euro Surveill. 2018;23(23):1700359. https://doi.org/10.2807/1560-7917.
van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(1):1–67.
Doove LL, Van Buuren S, Dusseldorp E. Recursive partitioning for missing data imputation in the presence of interaction effects. Comput Stat Data Anal. 2014;72:92–104.
Mitchell HD, Vilaplana TG, Mandal S, Ratna N, Glancy M, Shah A, et al. Effects of COVID-19 pandemic response on service provision for sexually transmitted infections, HIV, and viral hepatitis, England. Emerg Infect Dis. 2022;28(3):739–42. https://doi.org/10.3201/eid2803.211998.
Griffin M, Jaiswal J, Martino RJ, LoSchiavo C, Comer-Carruthers C, Krause KD, et al. Sex in the time of COVID-19: patterns of sexual behavior among LGBTQ+ individuals in the U.S. Arch Sex Behav. 2022;51(1):287–301.
Reyniers T, Rotsaert A, Thunissen E, Buffel V, Masquillier C, Van Landeghem E, et al. Reduced sexual contacts with non-steady partners and less PrEP use among MSM in Belgium during the first weeks of the COVID-19 lockdown: results of an online survey. Sex Transm Infect. 2021;97(6):414–9.
van Bilsen WPH, Zimmermann HML, Boyd A, Coyer L, van der Hoek L, Kootstra NA, Hoornenborg E, Prins M, Schim van der Loeff MF, Davidovich U, Matser A. Sexual behavior and its determinants during COVID-19 restrictions among men who have sex with men in Amsterdam. J Acquir Immune Defic Syndr. 2021;86(3):288–296. doi: https://doi.org/10.1097/QAI.0000000000002581.
Hyndman I, Nugent D, Whitlock GG, McOwan A, Girometti N. COVID-19 restrictions and changing sexual behaviours in HIV-negative MSM at high risk of HIV infection in London. UK Sex Transm Infect. 2021;97(7):521–4.
Wignall L, Portch E, McCormack M, Owens R, Cascalheira CJ, Attard-Johnson J, et al. Changes in sexual desire and behaviors among UK young adults during social lockdown due to COVID-19. J Sex Res. 2021;58(8):976–85.
Hammoud MA, Maher L, Holt M, Degenhardt L, Jin F, Murphy D, Bavinton B, Grulich A, Lea T, Haire B, Bourne A, Saxton P, Vaccher S, Ellard J, Mackie B, Batrouney C, Bath N, Prestage G. Physical distancing due to COVID-19 disrupts sexual behaviors among gay and bisexual men in Australia: implications for trends in hiv and other sexually transmissible infections. J Acquir Immune Defic Syndr. 2020;85(3):309–15. https://doi.org/10.1097/QAI.0000000000002462.
Stanford KA, McNulty MC, Schmitt JR, Eller DS, Ridgway JP, Beavis KV, et al. Incorporating HIV screening with COVID-19 testing in an urban emergency department during the pandemic. JAMA Intern Med. 2021;181(7):1001–3.
Gillespie D, Couzens Z, de Bruin M, Hughes DA, Jones A, Ma R, et al. PrEP use, sexual behaviour, and PrEP adherence among men who have sex with men living in wales prior to and during the COVID-19 pandemic. AIDS Behav. 2022. https://doi.org/10.1007/s10461-022-03618-4.
Ciaccio MD, Villes V, Michels D, Morel S, Delabre RM, Castro DR, et al. Impact of the early 2020 COVID-19 crisis and lockdown on PrEP use among men who have sex with men (MSM) in France. Sex Transm Infect. 2022;98(7):510–7. https://doi.org/10.1136/sextrans-2021-055189.
Stephenson R, Sullivan SP, Pitter RA, Hunter AS, Chavanduka TMD. Are we still having sex? Results of round two of the love and sex in the time of COVID survey with gay, bisexual and other men who have sex with men. AIDS Behav. 2022. https://doi.org/10.1007/s10461-022-03580-1.
Statbel - the Belgian statistical office. Migration. Total international migration (Belgian and stranger) 1948–2020. [Internet]. https://statbel.fgov.be/en/themes/population/migration#figures. Accessed 16 May 2022.
Hensley KS, Jordans CCE, van Kampen JJA, Mollema FPN, Gisolf EH, El Moussaoui R, et al. Significant impact of coronavirus disease 2019 (COVID-19) on human immunodeficiency virus (HIV) care in hospitals affecting the first pillar of the HIV care continuum. Clin Infect Dis. 2022;74(3):521–4. https://doi.org/10.1093/cid/ciab445.
El Moussaoui M, Lambert N, Maes N, Fombellida K, Vaira D, Moutschen M, Darcis G. Impact of the COVID-19 pandemic situation on HIV care in Liège. Belgium HIV Res Clin Pract. 2021;22(3):63–70.
Antoine J, Plettinckx E, van Baelen L, Gremeaux L. Analyse des conséquences de la crise du COVID-19 pour les centres de traitement spécialisés et les institutions en contact avec les personnes qui utilisent des drogues. 2020. https://feditobxl.be/site/wp-content/uploads/2020/04/sciensano-covid19-enqu%C3%AAte-aupr%C3%A8s-des-services-drogues-avril-2020.pdf. Accessed 22 Aug 2022. [in French]
Germain S, Yong A. COVID-19 highlighting inequalities in access to healthcare in England: a case study of ethnic minority and migrant women. Fem Leg Stud. 2020;28(3):301–10.
Nezafat Maldonado BM, Collins J, Blundell HJ, Singh L. Engaging the vulnerable: a rapid review of public health communication aimed at migrants during the COVID-19 pandemic in Europe. J Migr Health. 2020;1(1–2): 100004.
Beltran RM, Holloway IW, Hong C, Miyashita A, Cordero L, Wu E, et al. Social Determinants of Disease: HIV and COVID-19 Experiences. Curr HIV/AIDS Rep. 2022;19(1):101–12.
Acknowledgements
We acknowledge as collaborating authors to this study, the following members of the Belgian Research on AIDS and HIV Consortium (BREACH):
Nathalie Ausselet (HRC UCL-Namur), Marie-Luce Delforge (ARL Hôpital Erasme), Rémy Demeester (HRC CHU de Charleroi), Paul De Munter (HRC UZ Leuven), Eric Florence (HRC ITM), Jean-Christophe Goffard (HRC Hôpital Erasme), Benoït Kabamba (ARL UCL), Agnès Libois (HRC CHU Saint-Pierre), Rembert Mertens (HRC UZ Brussel), Peter Messiaen (HRC Jessa ziekenhuis), Michel Moutschen (HRC CHU de Liège), Denis Pierard (ARL UZ Brussel), Dolorès Vaira (ARL CHU de Liège), Linos Vandekerckhove (HRC UZ Gent), Dorien Vanden Bossche (ARL ITM), Sigi Van den Wijngaert (ARL CHU St Pierre), Kristel Van Laethem (ARL UZ Leuven), Jens Van Praet (HRC AZ Sint-Jan), Chris Verhofstede (ARL Universiteit Gent), Jean-Cyr Yombi (HRC Cliniques Universitaires Saint-Luc).
Funding
The Belgian HIV surveillance is financed by the National Institute for Sickness and Invalidity Insurance (INAMI/RIZIV). The design of the study, data collection, analysis, interpretation of results and writing of the manuscript was performed independently of the National Institute for Sickness and Invalidity Insurance.
Author information
Authors and Affiliations
Consortia
Contributions
DVB, JD designed the study. BS, MM, DVB performed the statistical analyses. DVB, BS, MM, JD interpreted the results with inputs from all authors. DVB drafted the manuscript. All authors read and critically revised the subsequent drafts of the manuscript. The collaborating authors from BREACH were in charge of data collection and transfer within their respective centres. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Sciensano, the Belgian institute of health, is legally entitled to conduct the HIV surveillance as part of its public health surveillance mandate in order to fulfil its mission of protecting and preserving the health and well-being of the population (https://etaamb.openjustice.be/fr/loi-du-25-fevrier-2018_n2018011241). Article 4.4 of that law explicitly states that Sciensano is authorized to collect, validate, analyze, report and archive data of a personal nature concerning public health and to perform quantitative and qualitative scientific analyses on the basis of the collected information. In accordance with the EU General Data Protection Regulation, the HIV surveillance conducted by Sciensano has been authorized by the Belgian administrative authority protecting privacy and personal data: the Information Security Committee Social Security and Health (https://www.ksz-bcss.fgov.be/fr/protection-des-donnees/comite-de-securite-de-linformation-csi). The authorization granted from the Information Security Committee Social Security and Health specifies that the HIV surveillance team is authorized to access the pseudonimized personal data used in this research within the frame of the national HIV surveillance [6]. In accordance with Article 14 of the General Data Protection Regulation, the above mentioned authorisation provides for an exemption from the obligation to inform data subjects as Sciensano has a legal mandate to conduct the HIV surveillance and the information obligation is likely to make the achievement of the objectives of its mandate impossible. The HIV surveillance complies with the WHO International Guidelines on the Ethics of Public Health Surveillance (https://www.who.int/publications-detail-redirect/who-guidelines-on-ethical-issues-in-public-health-surveillance). In addition, the collection of data from the HIV reference centres has been approved by the ethical committee of Ghent University Hospital ((RN B670201420495).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Van Beckhoven, D., Serrien, B., Montourcy, M. et al. Impact of COVID-19 on the Belgian HIV epidemic: slowdown of HIV transmission and testing and adaptation of care. BMC Infect Dis 22, 901 (2022). https://doi.org/10.1186/s12879-022-07879-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07879-1