Abstract
Background
Soil-transmitted helminth (STH) infections are still a major health problem, especially in resource-limited countries. The community-based prevalence of STH is unknown in Afghanistan. Main objectives of this study were to estimate the prevalence and associated factors of STH among children in Daman district of Kandahar province in Afghanistan.
Methods
This was a community-based cross-sectional study, with data collected during five months (June–October, 2020) from children living in five villages of Daman district in Kandahar, Afghanistan. All the stool samples were examined by saline wet mount method. Data were analyzed by using descriptive statistics, Chi square test, and multivariate logistic regression.
Results
A total of 1426 children were studied, with majority (61.8%) of males and the mean age of 6.3 years. The overall prevalence of any intestinal parasitic infection was 39.8%. The overall prevalence of STH infection was 22.7%, with Ascaris lumbricoides (18.7%) as the most prevalent STH species, followed by hookworm (7.5%) and Trichuris trichiura (1.4%). Single, double, and triple STH infections were present in 14.9%, 7.2%, and 0.6% of the children, respectively. Multivariate logistic regression revealed that not washing hands after defecating/before eating (AOR 7.0, 95% CI 3.4–14.0), living in mud house (AOR 3.5, 95% CI 1.6–7.4), walking barefoot (AOR 2.2, 95% CI 1.6–3.1), living in overcrowded house (AOR 1.6, 95% CI 1.1–2.3), and practicing open defecation (AOR 1.4, 95% CI 1.1–2.0) as the risk factors associated with the predisposition of rural children for getting STH in Daman district of Afghanistan.
Conclusions
Prevalence of STH is high among children of Daman district in Afghanistan. Most of the risk factors are related to poverty, decreased sanitation, and improper hygiene. Improvement of socioeconomic status, sanitation, and health education to promote public awareness about health and hygiene together with periodic mass deworming programs are better strategies for the control of STH infections in Afghanistan. Also, government and international donor agencies in Afghanistan should help in improving socio-economic status of the rural areas through provision of basic facilities such as piped water, electricity, good housing, and proper toilets.
Similar content being viewed by others
Background
Soil-transmitted helminths (STH) belong to a group of neglected tropical diseases, which mostly affect the tropical and subtropical regions. STH affect more than 1.5 billion people (24% of the world population) in Africa, Asia, and Latin America [1,2,3]. Approximately 267 million preschool-age and 568 million school-age children live in areas where STH transmission is very high [1].
Globally, the most prevalent STH is Ascaris lumbricoides (A. lumbricoides) (infecting approximately 1.2 billion people), followed by Trichuris trichiura (T. trichiura) (infecting nearly 795 million people) and hookworm (Ancylostoma duodenale and Necator americanus) which infects approximately 740 million people [4, 5]. School age children are at high risk of being infected with STH. This could be due to the reason that these children are more exposed to contaminated soil when they play, walk barefoot, eat soil, and do not practice good personal hygiene [6]. STH infections may cause many pathologic conditions [7], micronutrient impairment, and iron deficiency anemia [8,9,10]. Deworming campaigns in different countries of the world have shown to improve nutritional status, cognition, and school performance in school-age children [11,12,13].
Afghanistan has been suffering from military and civil conflict for the last four decades which, combined with natural disasters, has extremely weakened economic development [14]. The community-based prevalence of STH is unknown in Afghanistan. Diagnosis is mostly made on clinical basis without any laboratory confirmation. The insecurity and shortage of medical staff at all levels of the healthcare system hinders the implementation of epidemiological surveillance [15]. Healthcare system in Afghanistan is mostly dependent of international humanitarian aid [16]. The risk of parasitic diseases is estimated to be very high in Afghanistan [17].
Unfortunately, to our knowledge, there is currently no published data from Afghanistan to find the community-based prevalence and risk factors of STH in children. In 2003, workers with the World Health Organization (WHO) conducted a school-based survey with the help of Afghan ministry of public health and Afghan ministry of education. They collected fecal samples from 1,001 school children in four provinces of Afghanistan (Kabul, Kandahar, Nangarhar, and Farah) for soil-transmitted helminths (STH). This survey revealed that 47% of the school children were infected with STH, with predominant (41%) species of A. lumbricoides [18]. In 2017, a follow-up survey was conducted among school children aged 8–10 years to provide an update on STH epidemiology in Kabul, Balkh, Herat, Nangarhar, and Kandahar provinces of Afghanistan. In this survey, 26.6% of the children had at least one STH infection, with predominance of A. lumbricoides (25.7%) [19].In another hospital-based study in Afghanistan, 548 fecal samples were collected from the patients (both children and adults) with internal complaints who were admitted in two hospitals of Ghazni and Parwan provinces. Intestinal helminths were present in 144/386 (37.3%) of patients from Ghazni and Parwan provinces, respectively [15]. Main objectives of this community-based study were to estimate the prevalence of STH in children and also find the associated factors that predispose the rural children for getting STH in Daman district of Afghanistan.
Methods
Study design and study area
This was a community-based cross-sectional study, conducted during five-month-period (June–October, 2020). All the villages of Daman district with ≥ 50 houses each were selected for randomization using lottery method. After randomization, five villages (Azam Kala, Ghara Kalai, Mandisar, Mula Abdullah, and Khoshab) were selected for the study. Southern part of Daman district is covered with desert with nearly no inhabitants, while the northern part has cultivated lands and villages. Two seasonal rivers (Tarnak river and Arghistan river) and one running water canal from Arghandab river are flowing through the northern part of Daman district (Fig. 1). For stool samples examination, 3 health facilities were selected (Mandisar comprehensive health center, Khoshab basic health center, and Azam Kala basic health center) with every health facility within one kilometer distance from their nearby selected villages.
Map of Daman district in Kandahar province, Afghanistan. (1, Azam Kala village; 2, Ghara Kalai village; 3, Mandisar village; 4, Mula Abdullah village; 5, Khoshab village.)
Study population
The study population was composed of children with age < 15 years and permanent residents of Daman district in Kandahar province. All those children were excluded from the study who received any anti-helminthic treatment in the previous three months before the commencement of the study, having chronic diseases, not able to provide stool samples, or their parents/guardians refuse to participate in the study. A total of 1595 children were included to this study. Among these children, parents/guardians of 77 (4.8%) children refused to take part in the study while 92 (5.8%) failed to submit their fecal samples. So, data was collected from 1426 children.
Ethical considerations
Written informed consents were taken from parents or guardians of all the participants prior to the study. From children < 15 years old but old enough to answer were given the assent forms for the participation. Information of the participants will not be disclosed. Ethical approval was taken from Kandahar University Ethics Committee (code number KDRU-EC-2020.91). For data collection, only patients' initials were used. Prior to entering into the computer for analysis, the collected data was coded and de-identified.
Sample collection and laboratory procedures
Systematic random sampling was used for selecting the households while lottery method was used for selecting only one child from each household. A questionnaire was utilized in Pashto language with questions regarding general characteristics, economic status, general sanitation and environmental conditions, and laboratory examination. Data were collected/recorded on paper forms by experienced and trained investigators. Prior to data collection, meetings were conducted in the selected villages. A short briefing was given, during which the objectives and method of the study were clearly informed to the village elders and heads of the families, and prospective participants.
The case record form and other materials were pretested before the actual data collection. Persons responsible for data collection were well trained on how to conduct the interview and how to collect the stool samples. One day before sample collection, the caretakers of the children who agreed to participate in the study were provided with clean pre-labeled capped plastic container for stool collection along with instruction on correct placement of the stool into the containers. All the caretakers were instructed to collect the stool samples of the children from 8–11 am. As the assigned health facility were near to their villages, the assigned study volunteers in the villages would bring the stool samples immediately within 15 min to the laboratories of health facilities using motorbikes. In the laboratory, for the detection of intestinal parasites, saline wet mount method of stool examination was used. Although Kato–Katz technique is the preferred stool examination method for STH studies, but saline wet mount method was used in our study as this is the only available method in the public laboratories throughout Afghanistan. Stool examinations were performed by experienced medical laboratory technicians. All the stool samples were examined within 30 min after sample collection. So, there was no need for preservatives to store the samples. Some stool samples were randomly selected for quality control and examined by another experienced laboratory technician who was blinded for the previous test result. Also, to minimize the errors, data was double entered.
Data analysis
The data were entered into Microsoft Excel, cleaned, and imported to SPSS version 22 (Chicago, IL, USA) for statistical analysis. Descriptive analysis including frequency, mean, standard deviation (SD), and range was used to summarize demographic characteristics. Frequency and percentage were used to summarize categorical variables. Chi-square test (using crude odds ratio [COR]) was performed to assess the binary association between various categorical variables. All variables that were statistically significant in univariate analyses were assessed for independence in a multivariate logistic regression (using adjusted odds ratio [AOR]) to determine the factors associated with the predisposition of rural children for getting STH. A P-value of < 0.05 was statistically significant.
Results
As 169/1595 (10.6%) of the participants failed to submit their fecal samples, so the response rate of the study participants was 89.4% and the data was collected from 1426 children. Among 1426 children, 288 (20.2%) were the residents of Mandisar village, 287 (20.1%) Ghara Kalai village, 285 (20.0%) Khoshab village, 284 (19.9%) Mula Abdullah village, and 282 (19.8%) were the residents of Azam Kala village.
Mean (SD) age of these children was 6.3 (3.2) years with 331/1426 (23.2%) having less than five years of age. Male gender predominated (881/1426 [61.8%]) with 1285/1426 (90.1%) belonging to families with monthly income < 2500 Afghanis (< 30 USD). Nearly all (1387/1426 [97.3%]) mothers of these children were illiterate, while most (1161/1426 [81.4%]) of the guardians of their family were farmers (Table 1).
The overall prevalence of STH infection was 22.7% (324/1426 children). A. lumbricoides (18.7%, 267/1426) was the most prevalent STH species, followed by hookworm (7.5%, 107/1426), and T. trichiura (1.4%, 20/1426). Prevalence of intestinal protozoa infection was 17.9% (255/1426) while prevalence of overall any intestinal parasitic infection was 39.8% (567/1426). Giardia intestinalis was the most prevalent intestinal protozoa with a prevalence of 13.9%. Among the STH infected patients, single infection, double infection, and triple infections were present in 213/1426 (14.9%), 103/1426 (7.2%), and 8/1426 (0.6%) of the children, respectively (Table 2).
In Chi-square test, statistically significant variables responsible for increased STH infection were children from overcrowded families (COR 1.6, 95% CI [confidence interval] 1.2–2.1, and p-value 0.001), living in mud house (COR 4.1, 95% CI 2.0–8.5, and p-value < 0.001), practicing open defecation (COR 1.6, 95% CI 1.2–2.2, and p-value 0.001), not washing hands after defecation and before eating (COR 3.3, 95% CI 2.4–4.6, and p-value < 0.001), walking barefoot (COR 2.5, 95% CI 1.9–3.5, and p-value < 0.001), having untrimmed finger nails (COR 1.9, 95% CI 1.4–2.7, and p-value < 0.001), habit of nail biting (COR 1.5, 95% CI 1.1–2.1, and p-value 0.012), and consuming raw vegetables (COR 1.6, 95% CI 1.0–2.4, and p-value 0.035) (Table 3).
Multivariate logistic regression of the above-mentioned statistically significant variables revealed that not washing hands after defecating/before eating (AOR 7.0, 95% CI 3.4–14.0, and p-value < 0.001), living in mud house (AOR 3.5, 95% CI 1.6–7.4, and p-value 0.001), walking barefoot (AOR 2.2, 95% CI 1.6–3.1, and p-value < 0.001), living in overcrowded house (AOR 1.6, 95% CI 1.1–2.3, and p-value 0.023), and practicing open defecation (AOR 1.4, 95% CI 1.1–2.0, and p-value 0.023) as the risk factors associated with the predisposition of rural children for getting STH (Table 4).
Discussion
In this community-based cross-sectional study, we studied 1426 rural children during a five-month period (June–October, 2020). The prevalence of STH among children of Daman district was 22.7%. Main risk factors associated with the predisposition of children for getting STH were not washing hands after defecating/before eating, living in mud house, walking barefoot, living in overcrowded house, and practicing open defecation.
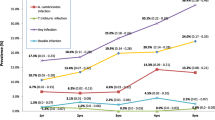
In our study, prevalence of STH in children was 22.7%. This prevalence is more than the studies conducted in Nepal (3.1%) [20], Indonesia (10.1%) [21], and China (14.1%) [22]. Contrary, prevalence in our study is less than reported in studies from India (75.6%) [23], Ethiopia (51.5%) [24], Malaysia (37%) [25], and Tajikistan (32%) [26]. The prevalence differences observed in different parts of the world (and even different areas of the same country) are multifactorial; including variations in stool examination techniques, geographical location, time of study, type of study, age of study participants, culture, socio-economic status, literacy levels/occupations of the parents or guardians, food consumption habits, and personal hygiene behaviors. Table 5 compares the prevalence of STH infections among our study and two other studies conducted in Kandahar in 2003 and 2017. In our study, the prevalence of STH is lower but prevalence hookworm is higher than other two studies conducted in Kandahar. The STH prevalence of 22.7% in our study is might be underestimated, due to the fact that we collected only one sample of stool sample instead of the standard three samples (as the caretakers of the study participants were not very cooperative) and used the method of saline wet mount microscopy for the diagnosis of STH. On the other hand, decreased STH prevalence can be contributed to the Afghanistan ministry of public health implementation of mass deworming interventions by among children throughout Afghanistan.
In our study, most prevalent STH was A. lumbricoides (18.7%). The A. lumbricoides as the most common STH has also been reported in studies from Nepal (26.6%) [27], India (69.6%) [23], and Nigeria (75.6% [28]). A study was conducted on 207 adults and 179 children visiting health facilities of Ghazni and Parwan provinces of Afghanistan. This study concluded that the most prevalent STH among children was A. lumbricoides (25.1% in Ghazni province and 10.8% in Parwan province) [15]. In 2003, a study conducted among school children of Kabul, Nangarhar, Farah, and Kandahar provinces of Afghanistan revealed that the most prevalent STH was A. lumbricoides with the prevalence of 41% (408/1001) in the school children of these four provinces of Afghanistan [18]. In 2017, another study conducted in Kabul, Balkh, Herat, Nangarhar and Kandahar provinces of Afghanistan showed that the most prevalent STH infection was the one with A. lumbricoides (25.7%) [19].
Our study showed that children who were not washing hand after defecation and before eating were having statistically significant STH. Protective effects of handwashing have also been reported from Iran [29], Uzbekistan [30], China [22], India [31] [32], Nepal [20], Lao [33], Indonesia [21], and Ethiopia [34].
In this study, living in mud house was a risk factor associated with increased STH infection in children. Similar results have been reported in other studies [23, 35]. It could be due to the reason that mud has the tendency to retain helminth ova even when it has been apparently cleaned [36].
Our study revealed that walking barefoot is a risk factor for having increased STH infection. Similar results have been reported from Nepal [37], Thailand [38], Indonesia [21], Malawi [39], Ethiopia [40], and Kenya [41]. Walking barefoot is especially a risk factor for hookworms, as their larvae in the soil can penetrate into unbroken skin. Although walking barefoot is not directly related to infections of other helminths, but it indirectly leads to the infection when child touches the contaminated feet and eat with unwashed hands afterwards [36].
Practicing open defecation was also a risk factor of increased STH infection in our study. This result is in accordance with researches reported from India [42], Indonesia [21], Vietnam [43], Nigeria [44], and Kenya [41]. The ova of STH are present in contaminated human feces. So open defecation and poor sanitation helps in the direct contamination of soil and easily spread of the STH infection from child to child. Poverty was the main cause of open defection in our study participants as they were not having toilets at their houses.
Limitations
There were some limitations in our study. We obtained only one fecal sample instead of the ideal three consecutive samples due to the level of cooperation and response of the parents and guardians. This might underestimate the real burden of STH. We did not find the intensity of STH in the study population. The only diagnostic method of saline wet mount microscopy used in our study has low sensitivity for the detection of STH infections. This was due to the fact that this was the only method available in the laboratories of our health facilities. Kato-Katz technique is not available in our laboratories. We did not get data of clinical symptoms and underlying diseases of the children, which can be confounding factors for STH. Additional studies should be performed in different parts of the country, including urban slums.
Conclusion
Based on the results of our study, it can be concluded that the prevalence of STH infection among children in Daman district of Kandahar province is 22.7%. Main risk factors associated with the predisposition of rural children for getting STH were not washing hands after defecating/before eating, living in mud house, walking barefoot, living in overcrowded house, and practicing open defecation.
We recommend that improvement of socioeconomic status, sanitation, and health education to promote public awareness about health and hygiene together with periodic mass deworming programs are better strategies for the control of STH infections in Afghanistan. Meanwhile, government and international donor agencies in Afghanistan should help in improving socio-economic status of the rural areas through provision of basic facilities such as piped water, electricity, good housing, and proper toilets.
Availability of data and materials
All the data and materials related to this study are available on request.
Change history
28 April 2022
A Correction to this paper has been published: https://doi.org/10.1186/s12879-022-07401-7
Abbreviations
- A. lumbricoides :
-
Ascaris lumbricoides
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- COR:
-
Crude odds ratio
- SD:
-
Standard deviation
- STH:
-
Soil-transmitted helminth
- WHO:
-
World Health Organization
References
World Health Organization. Soil-transmitted helminth infections. WHO. 2020 [cited 2021 Jul 5]. https://www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections
Kumar BH, Jain K, Jain R. A study of prevalence of intestinal worm infestation and efficacy of anthelminthic drugs. Med J Armed Forces India. Medical Journal Armed Forces India. 2014;70:144–8.
Salam N, Azam S. Prevalence and distribution of soil-transmitted helminth infections in India. BMC Public Health. 2017;17:201.
World Health Organization. Preventive chemotherapy in human helminthiasis. Coordinated use of anthelminthic drugs in control interventions: a manual for health professionals and programme managers. Geneva: WHO; 2006. http://apps.who.int/iris/bitstream/handle/10665/43545/9241547103_eng.pdf;jsessionid=1878429BB78FBA7DE153AFCEFDB93B05?sequence=1. Accessed 5 Sep 2021.
Parija S, Chidambaram M, Mandal J. Epidemiology and clinical features of soil-transmitted helminths. Trop Parasitol. 2017;7:81–5.
Hailegebriel T, Nibret E, Munshea A. Prevalence of Soil-transmitted helminth infection among school-aged children of Ethiopia: a systematic review and meta-analysis. Infect Dis Res Treat. 2020;13:1–14.
Awasthi S, Bundy DAP, Savioli L. Helminthic infections. Br Med J. 2003;1:431–3.
Crompton DWT. Ascariasis and childhood malnutrition. Trans R Soc Trop Med Hyg. 1992;86:577–9.
Crompton DWT, Nesheim MC. Nutritional impact of intestinal helminthiasis during the human life cycle. Annu Rev Nutr. 2002;1:35–59.
Oberhelman RA, Guerrero ES, Fernandez ML, Silio M, Mercado D, Comiskey N, et al. Correlations between intestinal parasitosis, physical growth, and psychomotor development among infants and children from rural Nicaragua. Am J Trop Med Hyg. 1998;58:470–5.
Girum T, Wasie A. The Effect of Deworming School Children on Anemia Prevalence: A Systematic Review and Meta-Analysis. Open Nurs J. 2018;12:155–61.
Opoku EC, Olsen A, Browne E, Hodgson A, Awoonor-Williams JK, Yelifari L, et al. Impact of combined intermittent preventive treatment of malaria and helminths on anaemia, sustained attention, and recall in Northern Ghanaian schoolchildren. Glob Health Action. 2016;9:32197.
Mireku MO, Davidson LL, Koura GK, Ouédraogo S, Boivin MJ, Xiong X, et al. Prenatal hemoglobin levels and early cognitive and motor functions of one-year-old children. Pediatrics. 2015;136:e76-83.
Wagner AL, Mubarak MY, Johnson LE, Porth JM, Yousif JE, Boulton ML. Trends of vaccine-preventable diseases in Afghanistan from the Disease Early Warning System, 2009±2015. PLoS ONE. 2017;12:e0178677.
Korzeniewski K, Chung WC, Augustynowicz A, Lass A, Ik KJ. Current status of intestinal parasitic infections among inhabitants of the Ghazni and Parwan Provinces Afghanistan. Fam Med Prim Care Rev. 2017;19:23–8.
Elyan DS, Monestersky JH, Wasfy MO, Noormal B, Oyofo BA. Capacity building of public health laboratories in Afghanistan: challenges and successes (2007–2011). East Mediterr Heal J. 2014;20:112–9.
Wallace MR, Hale BR, Utz GC, Olson PE, Earhart KC, Thornton SA, et al. Endemic infectious diseases of Afghanistan. Clin Infect Dis. 2002;34:S171-207.
Ramsan M, Gabrielli A-F, Tsogzolmaa D, Bojang B, Naumann C, Khoshal MH, et al. Distribution, prevalence and intensity of Soil-transmitted helminth infections among Afghan schoolchildren, 2003. J Helminthol. 2005;79:381–4.
Safi N, Warusavithana S, Shah Alawi SA, Atta H, Montresor A, Gabrielli AF. Elimination of morbidity due to soil-transmitted helminthiases among Afghan schoolchildren. Acta Trop. 2019;197:105035.
Tandukar S, Ansari S, Adhikari N, Shrestha A, Gautam J, Sharma B, et al. Intestinal parasitosis in school children of Lalitpur district of Nepal. BMC Res Notes. 2013;6:449.
Arta Suryantari SA. Prevalence, intensity and risk factors of soil transmitted helminths infections among elementary school students in Ngis village, Karangasem district. Bali Indones J Trop Infect Dis. 2019;7:137.
Balen J, Raso G, Li YS, Zhao ZY, Yuan LP, Williams GM, et al. Risk factors for helminth infections in a rural and a peri-urban setting of the Dongting Lake area, People’s Republic of China. Int J Parasitol. 2011;41:1165–73.
Ganguly S, Barkataki S, Karmakar S, Sanga P, Boopathi K, Kanagasabai K, et al. High prevalence of soil-transmitted helminth infections among primary school children, Uttar Pradesh, India, 2015. Infect Dis Poverty. 2017;6:139.
Abera B, Alem G, Yimer M, Herrador Z. Epidemiology of soil-transmitted helminths, Schistosoma mansoni, and haematocrit values among schoolchildren in Ethiopia. J Infect Dev Ctries. 2013;7:253–60.
Huat LB, Mitra AK, Jamil NIN, Dam PC, Mohamed HJJ, Muda WAMW. Prevalence and Risk Factors of Intestinal Helminth Infection Among Rural Malay Children. J Glob Infect Dis. 2012;4:10.
Matthys B, Bobieva M, Karimova G, Mengliboeva Z, Jean-Richard V, Hoimnazarova M, et al. Prevalence and risk factors of helminths and intestinal protozoa infections among children from primary schools in western Tajikistan. Parasit Vectors. 2011;4:1–13.
Khadka KS, Kaphle HP, Gurung K, Shah Y, Sigdel M. Study of Intestinal Parasitosis among School Going Children in Pokhara. Nepal J Heal Allied Sci. 2013;3:47–50.
Osazuwa OM, Imade P. A significant association between intestinal helminth infection and anaemia burden in children in rural communities of Edo state Nigeria. N Am J Med Sci. 2011;3:30–4.
Daryani A, Sharif M, Nasrolahei M, Khalilian A, Mohammadi A, Barzegar G. Epidemiological survey of the prevalence of intestinal parasites among schoolchildren in Sari, northern Iran. Trans R Soc Trop Med Hyg. 2012;106:455–9.
Gungoren B, Latipov R, Regallet G, Musabaev E. Effect of hygiene promotion on the risk of reinfection rate of intestinal parasites in children in rural Uzbekistan. Trans R Soc Trop Med Hyg. 2007;101:564–9.
Kaliappan SP, George S, Francis MR, Kattula D, Sarkar R, Minz S, et al. Prevalence and clustering of soil-transmitted helminth infections in a tribal area in southern India. Trop Med Int Heal. 2013;18:1452–62.
Awasthi S, Verma T, Kotecha P, Venkatesh V, Joshi V, Roy S. Prevalence and risk factors associated with worm infestation in pre-school children (6–23 months) in selected blocks of Uttar Pradesh and Jharkhand. India Indian J Med Sci. 2008;62:484–91.
Hohmann H, Panzer S, Phimpachan C, Southivong C, Schelp F. Relationship of intestinal parasites to the environment and to behavioral factors in children in the Bolikhamxay Province of Lao PDR. Southeast Asian J Trop Med Public Heal. 2001;32:4–13.
Nasr NA, Al-Mekhlafi HM, Ahmed A, Roslan MA, Bulgiba A. Towards an effective control programme of soil-transmitted helminth infections among Orang Asli in rural Malaysia. Part 1: Prevalence and associated key factors. Parasit Vectors. 2013;6:1–12.
Kattula D, Sarkar R, Ajjampur S, Minz S, Levecke B, Muliyil J, et al. Prevalence & risk factors for soil transmitted helminth infection among school children in south India. Indian J Med Res. 2014;139:76–82.
Anunobi JT, Okoye IC, Aguzie IO, Ndukwe YE, Okpasuo OJ. Risk of soil-transmitted helminthiasis among agrarian communities of Kogi state, Nigeria. Ann Glob Heal. 2019;85(120):1–13.
Parajuli RP, Umezaki M, Watanabe C. Behavioral and nutritional factors and geohelminth infection among two ethnic groups in the Terai region Nepal. Am J Hum Biol. 2009;21:98–104.
Jiraanankul V, Aphijirawat W, Mungthin M, Khositnithikul R, Rangsin R, Traub RJ, et al. Incidence and risk factors of hookworm infection in a rural community of central Thailand. Am J Trop Med Hyg. 2011;84:594–8.
Phiri K, Whitty CJ, Graham S, Ssembatya-Lule G. Urban/rural differences in prevalence and risk factors for intestinal helminth infection in southern Malawi. Ann Trop Med Parasitol. 2000;94:381–7.
Erosie L, Merid Y, Ashiko A, Ayine M, Balihu A, Muzeyin S, et al. Prevalence of Hookworm infection and haemoglobin status among rural elementary school children in Southern Ethiopia. Ethiop J Heal Dev. 2002;16:113–5.
Freeman MC, Chard AN, Nikolay B, Garn JV, Okoyo C, Kihara J, et al. Associations between school- and household-level water, sanitation and hygiene conditions and soil-transmitted helminth infection among Kenyan school children. Parasit Vectors. 2015;8:412.
Goel S, Tank R, Singh A, Khichi SK, Goyal P, Arya R. Prevalence and risk factors of soil transmitted helminths from rural field practice area of a tertiary care center from northern India. Int J Res Med Sci. 2017;4:1983–7.
Yajima A, Jouquet P, Trung D, Cam TDT, Cong DT, Orange D, et al. High latrine coverage is not reducing the prevalence of soil-transmitted helminthiasis in Hoa Binh province. Vietnam Trans R Soc Trop Med Hyg. 2009;103:237–41.
Edelduok E, Eyo J, Ekpe E. Soil-transmitted helminth infections in relation to the knowledge and practice of preventive measures among school children in rural communities in South-Eastern Nigeria. IOSR J Pharm Biol Sci. 2013;5:33–7.
Acknowledgements
We present our highest and sincere thanks to the authorities of Faculty of Medicine, Kandahar University, Kandahar Province Directorate of Public Health, and elders of villages in Daman district. We are also very thankful of the data collectors and all our study participants.
Funding
This study did not receive any specific funding. WR Taylor is part funded by Wellcome under grant 220211. For the purpose of Open Access, the author has applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission.
Author information
Authors and Affiliations
Contributions
Conceptualisation: BAR, BAM, MSS, MHS, WRT. Data curation: BAR, BAM. Formal analysis: BAR, MHW, MHS. Funding acquisition: No funding. Investigation: BAM, MHW, MSS. Methodology: BAR, BAM, WRT. Project administration: BAR, BAM, MSS, MHS. Resources: MHW, BAM. Software: BAR, MSS. Supervision: BAR, BAM. Validation: MHW, MSS. Visualisation: MHW, MSS. Writing—original draft: BAR, MHW. Writing – review & editing: BAR, BAM, MHW, MSS,, MHS, WRT. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consents were taken from parents or guardians of all the participants prior to the study. From children < 15 years old but old enough to answer were given the assent forms for the participation. Information of the participants will not be disclosed. Ethical approval was taken from Kandahar University Ethics Committee (code number KDRU-EC-2020.91). For data collection, only patients' initials were used. Prior to entering into the computer for analysis, the collected data was coded and de-identified.
Consent for publication
Not applicable.
Competing interests
All the authors do not have any competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
An error was identified in the Funding section. The current statement reads: There were no fundings for this study. The statement should read: This study did not receive any specific funding. WR Taylor is part funded by Wellcome under grant 220211. For the purpose of Open Access, the author has applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission. The original article has been updated.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rahimi, B.A., Mahboobi, B.A., Wafa, M.H. et al. Prevalence and associated risk factors of soil-transmitted helminth infections in Kandahar, Afghanistan. BMC Infect Dis 22, 361 (2022). https://doi.org/10.1186/s12879-022-07336-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07336-z