Abstract
Background
Mycobacterial time to positivity (TTP) in liquid culture media has predictive value for longer term outcomes in pulmonary tuberculosis, but has not been thoroughly studied in nontuberculous mycobacterial pulmonary disease. This study sought to evaluate for association between TTP and sputum culture conversion to negative in pulmonary disease caused by Mycobacterium avium complex (MAC).
Methods
Data from the CONVERT trial (NCT02344004) that evaluated efficacy of guideline-based-therapy with or without amikacin liposome inhalation suspension in adults with refractory MAC-PD (Mycobacterium avium complex pulmonary disease) were analyzed. We evaluated TTP measures for sputum obtained prior to study treatment initiation and at monthly visits, assessing reproducibility of measures as well as association of TTP with culture conversion on treatment.
Results
Data from 71 participants with at least one screening visit TTP value were analyzed. For participants who provided more than one sputum sample at a given visit, there was moderate between-sample reliability, with median intraclass correlation coefficient 0.62 (IQR 0.50, 0.70). Median TTP at screening was longer in those participants who subsequently achieved vs. did not achieve culture conversion (10.5 [IQR 9.4] days vs. 4.2 [IQR 2.8] days, p = 0.0002). Individuals with culture conversion by study treatment month 6 were more likely to have a screening TTP > 5 days compared to those who did not achieve culture conversion (OR 15.4, 95% CI 1.9, 716.7, p = 0.0037) and had increasing TTPs over time.
Conclusions
TTP prior to and on treatment is associated with microbiological treatment response in patients with MAC-PD.
Similar content being viewed by others
Background
The prevalence of non-tuberculous mycobacterial pulmonary disease (NTM-PD) is increasing, and species from the Mycobacterium avium complex (MAC) are the most common etiology [1,2,3]. Current guidelines for treatment of MAC pulmonary disease (MAC-PD) recommend a prolonged course of combination antimicrobial therapy [4]. Despite treatment, outcomes remain sub-optimal and conversion of sputum cultures to negative, considered a surrogate for pathogen eradication, is not universally achieved; a meta-analysis reported a sputum culture conversion rate of 60% and a recent expanded systematic review reported a culture conversion rate of 56.5% [5,6,7]. In addition, treatment is often associated with patient intolerance and systemic toxicities [4]. Therefore, there is a need for development of novel therapeutics with both improved efficacy and tolerability.
Currently, there are no reliable biomarkers that predict response to therapy for NTM-PD, leaving clinicians to rely heavily on results from respiratory cultures as an objective measure of clinical response. However, reliance on respiratory culture conversion is problematic because this outcome takes months to achieve, thereby delaying assessment of a patient’s response to treatment and presenting a barrier for clinical trials. This gap in knowledge highlights the critical need for an early marker of microbiological efficacy against NTM. For pulmonary tuberculosis, time-to-positivity (TTP) of Mycobacterium tuberculosis in liquid culture media correlates well with conventional colony forming unit (cfu) counting, pre-treatment TTP inversely correlates with treatment response, and change in TTP over time on treatment is a biomarker of therapeutic response [8,9,10]. For MAC-PD, TTP correlates well with conventional sputum cfu counting, prompting new research to investigate correlation with treatment outcomes [11].
We sought to assess the relationship between TTP and microbiologic response to treatment of MAC-PD using existing data collected in the CONVERT trial (NCT02344004), which evaluated the addition of amikacin liposome inhalation suspension to guideline-based therapy in patients with refractory MAC-PD [12]. Participants in the CONVERT trial provided sputum specimens at pre-specified intervals prior to and during study treatment, with culture conversion to negative as the primary trial outcome, thus providing an opportune sample for our secondary investigation. Preliminary results of our study have been previously reported in the form of an abstract [13].
Methods
Prior to enrollment and participation in the CONVERT trial, informed consent was obtained from all subjects and/or their legal guardians. Methodology of the initial Phase III clinical trial is described and summarized below. Our secondary data analysis, also described below, was determined to be exempt human subjects research, under Exemption 4, by the IRB of the Medical University of South Carolina. All methods described were carried out in accordance with relevant guidelines and regulations.
CONVERT trial
The trial enrolled adults with treatment-refractory MAC-PD who had MAC positive sputum or bronchoscopy cultures at the time of study eligibility screening. Baseline was defined as the interval of time from 2 days prior to initiation of study treatment to the day of study treatment start. The CONVERT primary endpoint was the proportion of participants achieving culture conversion to negative, based on cultures from sputum obtained monthly from baseline through month 6 and considering the results of liquid and solid media cultures. For a given participant, culture conversion was considered to be achieved if there were 3 consecutive monthly negative sputum cultures, with all sputum samples collected at each visit required to be culture-negative. To meet the primary endpoint, month 4 was the latest visit at which a negative sputum culture could first be detected. The protocol specified that at least two and preferably three sputum specimens were to be obtained from each participant at each assessment. Each sputum specimen was collected on consecutive days prior to a scheduled visit, except for screening specimens, which were collected during the week following the screening visit. If a participant was not able to spontaneously expectorate, sputum induction was attempted once at the study visit. Participants were instructed to refrain from administration of the inhaled study treatment on the days that sputum was obtained, starting 2 days prior to each scheduled visit. Sputum specimens were refrigerated until shipped to a designated study laboratory within 2 days of collection.
In the laboratory, sputum was digested and decontaminated using N-acetyl-l-cysteine/sodium hydroxide (final concentration of sodium hydroxide 1%). After centrifugation, the sediment was resuspended in phosphate buffered saline and cultured on Lowenstein–Jensen solid agar and in Mycobacteria Growth Indicator Tubes (MGIT, Becton, Dickinson & Company, Franklin Lakes, NJ) using the MGIT 960 system, which automatically flags positive cultures and calculates the TTP. MGIT inoculation volume was 0.5 mL, and MGIT cultures were incubated for 6 weeks before being reported as negative. Mycobacteria were identified using a commercial DNA probe assay that includes a general MAC probe as well as species-specific probes for M. avium, M. intracellulare and M. chimaera (InnoLiPA Mycobacteria v2, Innogenetics, Ghent, Belgium).
Secondary TTP data analysis
Summaries were performed on existing data from the CONVERT trial using the subset of the intention to treat analysis population with available TTP data, rather than an a priori design with powering for the comparisons of interest. Confidence intervals (CIs) and corresponding p-values should be regarded as nominal. All analyses were performed on available data without imputations. Baseline demographics were summarized using descriptive statistics. The intraclass correlation coefficient (ICC) was used to describe between-sample reliability for those participants who provided more than one sample at a given visit and was derived using random effect coefficient modeling. Bland–Altman methodology was used to assess TTP reproducibility between screening and baseline visits, a period during which each participant’s treatment was held constant. Comparison of TTP between sputum culture converters and non-converters was performed via logistic regression. Comparative analyses were not adjusted for multiplicity; hence p-values are nominal.
Results
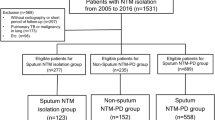
Participants
The CONVERT study used three reference laboratories for microbiological testing using broth culture as per CONVERT study protocol, however precise to the hour TTP data were available only from the Radboudumc Center for Infectious Diseases laboratory, the Netherlands. Thus, although the CONVERT study enrolled 336 participants overall, only 71 participants had at least one screening TTP value and were included in the current analysis. Baseline demographics, treatment assignment, and culture conversion rates for this subset of participants as well as those included in the CONVERT intention to treat analysis population are shown in Table 1. Compared to the larger CONVERT population, our sample included a higher proportion of Caucasians, lower proportion with culture conversion, and variability in underlying lung pathology, but otherwise was similar.
Within-participant reproducibility of TTP measures
TTP data were available for 945 sputum cultures obtained at a total of 414 study visits. For those 414 visits, 99 (24%) had one evaluable sputum specimen, 99 (24%) had two evaluable sputum specimens, and 216 (52%) had three evaluable sputum specimens (Additional file 1: Table S1). For those participants who provided more than one sample at a given visit, there was moderate between-sample reliability, with intraclass correlation coefficient (ICC) ranging between 0.39 and 0.74 (median 0.62, IQR 0.50, 0.70, Additional file 1: Table S2). Bland–Altman analysis of TTP reproducibility between screening and baseline visits showed median difference of − 0.1 days (95% CI − 0.48, 0.56) with 95% limits of agreement − 3.9, 3.69 days when individuals’ shortest TTP values were used, and median difference of 0.06 days (95% CI − 0.80, 0.63) with 95% limits of agreement − 5.14, 5.27 days when individuals’ longest TTP values were used (Fig. 1).
Reproducibility between screening and baseline time to positivity of Mycobacterium avium complex in liquid culture. Bland–Altman scatter diagrams of the differences between baseline visit time to positivity (TTP) and screening visit TTP plotted against the median of the two measures for the shortest TTP values (a) and the longest TTP values (b). The solid line shows the median and the short horizontal dashed lines represent the 95% confidence intervals of the median. Long horizontal dashed lines represent the 95% limits of agreement, defined as the median difference plus and minus 1.96 times the standard deviation of the differences
Association of screening TTP with culture conversion
The median TTP at screening was longer in those participants who eventually achieved culture conversion compared to those who did not: 10.5 (IQR 9.4) days vs. 4.2 (IQR 2.8) days, p = 0.0002 when the shortest measured screening TTP was used for each participant; and 10.9 (IQR 7.0) days vs. 6.3 (IQR 4.3) days, p = 0.0013 (Table 2) when the longest measured TTP was used for each participant.
Figure 2 shows the shortest TTP measured at screening for each participant, demonstrating that all participants who subsequently achieved culture conversion had a screening TTP of at least 5 days or more. Individuals with sputum culture conversion to negative by study treatment month 6 were significantly more likely to have a screening TTP > 5 days than those who did not achieve culture conversion (OR 15.4, 95% CI 1.9, 716.7; p = 0.0037); using a screening TTP threshold of > 7 days yielded OR 6.6, 95% CI 1.3, 37.5; p = 0.0192.
Distribution of shortest time to positivity measured at screening, by converter status. Distribution of screening time to positivity (TTP) by culture conversion status. Red bars represent participants who subsequently achieved culture conversion to negative by month 6 of study participation, and blue bars represent participants who did not achieve culture conversion. TTP values are rounded up to the next whole day; for participants with more than one screening TTP value, the shortest TTP value was used
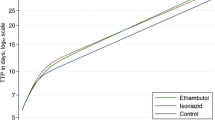
Association of TTP change over time with culture conversion
Figure 3 and Additional file 1: Table S3 show the median TTPs measured at all study visits, stratified by participant culture conversion status. Among participants who did not achieve culture conversion the median TTPs ranged from 4.2 to 4.9 days, without appreciable change over time. Among participants who achieved culture conversion the median TTPs ranged from 10.5 to 22.5 days and increased over time.
Discussion
Our study extends the current evidence base for TTP as a measure of MAC bacillary burden in two main ways [11]. First, there was a significant inverse association between screening TTP and sputum culture conversion to negative in adults with refractory MAC-PD. This aligns well with clinical observations that individuals with cavitary MAC-PD, which can be accompanied by high bacterial loads reflected by positive sputum smears, have poorer outcomes than those with noncavitary MAC-PD [14]. Second, TTP increased over time in individuals with eventual culture conversion but not in those without culture conversion, and supports exploration of the use of longitudinal TTP measures for treatment response monitoring. Analogous findings have been described for pulmonary tuberculosis—in the laboratory setting TTP correlates with the size of a bacterial inoculum, and in the clinical setting TTP can be used as an alternative to cumbersome colony forming unit quantitation in evaluating response to tuberculosis treatment, both at the individual patient level and as a clinical trial outcome measure [9, 10, 15].
Our results confirm and extend the results of retrospective studies reported recently by others who have investigated the role of TTP in MAC-PD [16, 17]. As in our study, Danho et al. observed longer baseline TTPs in patients who subsequently had versus did not have conversion of cultures to negative, and TTP increased over the 1st months of treatment in individuals who converted cultures to negative. Our study provides useful new information about the within-participant reproducibility of MAC TTP measurements across sputum specimens obtained over 2 to 3 days around each study visit as well as over a longer interval of time in the absence of a change in treatment (i.e. as measured at screening and baseline visits). Reproducibility of the measure was moderate to good, but not perfect, and probably reflects several factors including intensity of cough and/or participant effort, diurnal variation in cough and/or sputum production, and airways whose contents are represented in the expectorated sputum specimen. At the individual participant level, TTP variability between the screening and baseline visits was slightly less when the shortest, rather than the longest, TTPs were analyzed. For this reason and because the shorter TTP is likely to reflect the greater bacterial burden, we elected to use the shorter TTP in our analyses.
Identification of biomarkers for NTM treatment response has been identified as a research priority both by clinicians/investigators and individuals with NTM-PD [18]. TTP is operationally attractive because the TTP value is automatically calculated and reported by MGIT system instruments; while clinical results reporting algorithms may require adjustment to incorporate TTP results, no new technology or instrumentation is needed. The identification of association between TTP at screening and subsequent on-treatment culture conversion has implications for clinical trial design. Consideration should be given to stratified randomization based on pre-intervention bacillary burden as assessed by TTP in order to ensure balance of treatment groups with respect to this prognostic variable.
There are important limitations of our study. Our analyses included only the subset of trial participants for whom TTP data were available. Consequently, the sample size was relatively small overall and especially with regard to participants who achieved culture conversion. Disease was assumed to be stable in the time between screening and baseline assessment, however no detailed objective data was collected to fully support this assumption. We were also unable to explore potential associations between TTP and radiographic features or other clinical severity indices, since this information was not captured systematically during the phase 3 trial. Outcome was expressed as culture conversion status by month 6 of study treatment in order to align with the primary outcome of the CONVERT trial. While our analysis demonstrated a clear signal supporting clinical utility of TTP, larger prospective studies that explore other outcomes and systematically gather detailed baseline severity data may be able to rigorously identify nuanced relationships between TTP and other microbiological or clinical endpoints.
Conclusions
Our study population, reflecting the CONVERT trial study population, had refractory MAC-PD with persistently positive cultures despite long-term antibiotic therapy prior to study entry whereas tuberculosis studies incorporating TTP have been performed in treatment-naïve individuals. This is a major methodologic difference and antimicrobial treatment may impact mycobacterial TTP through multiple mechanisms. However, CONVERT participants were representative of an important large subset of NTM-PD patients in which a predictive biomarker is particularly needed. Our promising findings in a clinically complex patient population highlight the importance of further investigation of TTP in MAC-PD, including in treatment naïve populations.
While our findings are not conclusive, they are supportive that TTP may serve as a useful biomarker of treatment response in patients with MAC-PD. Our findings provide rationale for incorporation of TTP measurements into clinical trials of novel therapies for MAC-PD and into clinical practice.
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and its additional information files].
Abbreviations
- TTP:
-
Time to positivity
- MAC:
-
Mycobacterium avium Complex
- MAC-PD:
-
Mycobacterium avium Complex pulmonary disease
- NTM:
-
Non-tuberculous mycobacteria
- NTM-PD:
-
Non-tuberculous mycobacterial pulmonary disease
- CFU:
-
Colony forming unit
- MGIT:
-
Mycobacteria growth indicator tube
- CI:
-
Confidence interval
- ICC:
-
Intraclass coefficient
- IQR:
-
Interquartile range
- OR:
-
Odds ratio
References
Jones MM, Winthrop KL, Nelson SD, Duvall SL, Patterson OV, Nechodom KE, Findley KE, Radonovich LJ Jr, Samore MH, Fennelly KP. Epidemiology of nontuberculous mycobacterial infections in the U.S. Veterans Health Administration. PLoS ONE. 2018;13:e0197976.
Hoefsloot W, van Ingen J, Andrejak C, Angeby K, Bauriaud R, Bemer P, Beylis N, Boeree MJ, Cacho J, Chihota V, Chimara E, Churchyard G, Cias R, Daza R, Daley CL, Dekhuijzen PN, Domingo D, Drobniewski F, Esteban J, Fauville-Dufaux M, Folkvardsen DB, Gibbons N, Gomez-Mampaso E, Gonzalez R, Hoffmann H, Hsueh PR, Indra A, Jagielski T, Jamieson F, Jankovic M, Jong E, Keane J, Koh WJ, Lange B, Leao S, Macedo R, Mannsaker T, Marras TK, Maugein J, Milburn HJ, Mlinko T, Morcillo N, Morimoto K, Papaventsis D, Palenque E, Paez-Pena M, Piersimoni C, Polanova M, Rastogi N, Richter E, Ruiz-Serrano MJ, Silva A, da Silva MP, Simsek H, van Soolingen D, Szabo N, Thomson R, Tortola Fernandez T, Tortoli E, Totten SE, Tyrrell G, Vasankari T, Villar M, Walkiewicz R, Winthrop KL, Wagner D, Nontuberculous Mycobacteria Network European Trials Group. The geographic diversity of nontuberculous mycobacteria isolated from pulmonary samples: an NTM-NET collaborative study. Eur Respir J. 2013;42:1604–13.
Furuuchi K, Morimoto K, Yoshiyama T, Tanaka Y, Fujiwara K, Okumura M, Izumi K, Shiraishi Y, Mitarai S, Ogata H, Kurashima A, Yoshimori K, Ohta K, Goto H, Sasaki Y. Interrelational changes in the epidemiology and clinical features of nontuberculous mycobacterial pulmonary disease and tuberculosis in a referral hospital in Japan. Respir Med. 2019;152:74–80.
Daley CL, Iaccarino JM, Lange C, Cambau E, Wallace RJ, Andrejak C, Bottger EC, Brozek J, Griffith DE, Guglielmetti L, Huitt GA, Knight SL, Leitman P, Marras TK, Olivier KN, Santin M, Stout JE, Tortoli E, van Ingen J, Wagner D, Winthrop KL. Treatment of nontuberculous mycobacterial pulmonary disease: an official ATS/ERS/ESCMID/IDSA clinical practice guideline: executive summary. Clin Infect Dis. 2020;71:e1–36.
Kwak N, Park J, Kim E, Lee CH, Han SK, Yim JJ. Treatment outcomes of Mycobacterium avium complex lung disease: a systematic review and meta-analysis. Clin Infect Dis. 2017;65:1077–84.
Henkle E, Novosad SA, Shafer S, Hedberg K, Siegel SAR, Ku J, Varley C, Prevots DR, Marras TK, Winthrop KL. Long-term outcomes in a population-based cohort with respiratory nontuberculous mycobacteria isolation. Ann Am Thorac Soc. 2017;14:1120–8.
Flume P, Cline K, Jumadilova Z, Mange K, Winthrop K. Relationship between culture conversion and clinical outcomes in Mycobacterium avium complex lung disease: a systematic review [abstract]. Chest. 2020;158:A315.
Pheiffer C, Carroll NM, Beyers N, Donald P, Duncan K, Uys P, van Helden P. Time to detection of Mycobacterium tuberculosis in BACTEC systems as a viable alternative to colony counting. Int J Tuberc Lung Dis. 2008;12:792–8.
Epstein MD, Schluger NW, Davidow AL, Bonk S, Rom WN, Hanna B. Time to detection of Mycobacterium tuberculosis in sputum culture correlates with outcome in patients receiving treatment for pulmonary tuberculosis. Chest. 1998;113:379–86.
Hesseling AC, Walzl G, Enarson DA, Carroll NM, Duncan K, Lukey PT, Lombard C, Donald PR, Lawrence KA, Gie RP, van Helden PD, Beyers N. Baseline sputum time to detection predicts month two culture conversion and relapse in non-HIV-infected patients. Int J Tuberc Lung Dis. 2010;14:560–70.
Pennings LJ, Zweijpfenning S, Ruth MM, Wattenberg M, Boeree MJ, Hoefsloot W, van Ingen J. Mycobacterium avium complex bacteria remain viable in sputum during storage and refrigeration. Diagn Microbiol Infect Dis. 2018;92:309–10.
Griffith DE, Eagle G, Thomson R, Aksamit TR, Hasegawa N, Morimoto K, Addrizzo-Harris DJ, Oonnell AE, Marras TK, Flume PA, Loebinger MR, Morgan L, Codecasa LR, Hill AT, Ruoss SJ, Yim JJ, Ringshausen FC, Field SK, Philley JV, Wallace RJ Jr, van Ingen J, Coulter C, Nezamis J, Winthrop KL, Group CS. Amikacin liposome inhalation suspension for treatment-refractory lung disease caused by Mycobacterium avium complex (CONVERT). A prospective, open-label, randomized study. Am J Respir Crit Care Med. 2018;198:1559–69.
Mingora CM, Garcia B, Mange K, Yuen D, Flume P, Dorman S. Time-to-detection as a potential surrogate marker for treatment outcomes in patients with non-tuberculous mycobacterial disease [abstract]. Am J Respir Crit Care Med. 2020;201:A4369.
Koh WJ, Moon SM, Kim SY, Woo MA, Kim S, Jhun BW, Park HY, Jeon K, Huh HJ, Ki CS, Lee NY, Chung MJ, Lee KS, Shin SJ, Daley CL, Kim H, Kwon OJ. Outcomes of Mycobacterium avium complex lung disease based on clinical phenotype. Eur Respir J. 2017;50:1602503.
Bark CM, Okwera A, Joloba ML, Thiel BA, Nakibali JG, Debanne SM, Boom WH, Eisenach KD, Johnson JL. Time to detection of Mycobacterium tuberculosis as an alternative to quantitative cultures. Tuberculosis (Edinb). 2011;91:257–9.
Danho R, Schildkraut JA, Zweijpfenning SMH, et al. Mycobacterium growth indicator tube time-to-positivity can serve as an early biomarker of treatment response in Mycobacterium avium complex pulmonary disease. Chest. 2022;161(2):370–2.
Edwards BD, Brode SK, Mehrabi M, Marras TK. Time to positive culture detection predicts Mycobacterium avium pulmonary disease severity and treatment initiation. Ann Am Thorac Soc. 2021. https://doi.org/10.1513/AnnalsATS.202107-765OC (published online ahead of print, 2021 Dec 1).
Daley CL, Winthrop KL. Mycobacterium avium complex: addressing gaps in diagnosis and management. J Infect Dis. 2020;222:S199–211.
Acknowledgements
Not applicable.
Funding
Insmed Incorporated, Bridgewater, New Jersey supported the CONVERT clinical trial and supported the data analyses for this study. Dr. Dorman was supported, in part, by National Institutes of Health Grant award NIH K24AI104830. Dr. Flume was supported, in part, by the National Center for Advancing Translational Sciences of the National Institutes of Health under Grant Number UL1 TR001450. Dr. Mingora was supported, in part, by the Medical University of South Carolina institutional post-doctoral training grant from the National Institutes of Health, Grant award NIH-T32-HL144470.
Author information
Authors and Affiliations
Contributions
CMM: Conceived and designed study, analyzed data, and wrote the manuscript. BAG: Conceived and designed the study and edited the manuscript. KCM: Contributed data and edited the manuscript. DWY, MC: Contributed and analyzed data. JvI: Contributed and analyzed data, edited the manuscript. PAF, SED: Conceived and designed the study, analyzed data, and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Prior to enrollment and participation in the CONVERT trial, informed consent was obtained from all subjects and/or their legal guardians. Our secondary data analysis was determined to be exempt human subjects research, under Exemption 4, by the IRB of the Medical University of South Carolina. All methods described were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
CMM has received grant funding from the National Institutes of Health. This relationship is outside of the submitted work.
BAG has received grant funding from the CHEST foundation, through grant sponsored by Insmed. He hahs also collected personal fees from Insmed, Synspira, and CMEducation Resources, LLC. These relationships are outside of the submitted work.
KCM, DWY, MC is an employee of Insmed Incorporated. This is relationship is outside of the submitted work.
JvI received reimbursement of laboratory activities with the context of the clinical trail that yielded the data for this manuscript and was member of advisory board.
PAF has received grant funding and personal fees from Insmed Pharmaceuticals. These relationships are outside of the submitted work.
SED has received grant funding from the Centers for Disease Control and Prevention as well as the National Institutes of Health. These relationships are outside of the submitted work. SED also reports that Insmed Incorporated has supported the data analysis for this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table S1. Summary of time to positivity (TTP) counts, by visit. Table S2. Repeatability of time to positivity, by visit. Table S3. Summary statistics of shortest time to positivity, in days, by visit for participants with at least one screening time to positivity value.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mingora, C.M., Garcia, B.A., Mange, K.C. et al. Time-to-positivity of Mycobacterium avium complex in broth culture associates with culture conversion. BMC Infect Dis 22, 246 (2022). https://doi.org/10.1186/s12879-022-07250-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07250-4