Abstract
Background
Invasive candidal infection combined with bacterial bloodstream infection is one of the common nosocomial infections that is also the main cause of morbidity and mortality. The incidence of invasive Candidal infection with bacterial bloodstream infection is increasing year by year worldwide, but data on China is still limited.
Methods
We included 246 hospitalised patients who had invasive candidal infection combined with a bacterial bloodstream infection from January 2013 to January 2018; we collected and analysed the relevant epidemiological information and used machine learning methods to find prognostic factors related to death (training set and test set were randomly allocated at a ratio of 7:3).
Results
Of the 246 patients with invasive candidal infection complicated with a bacterial bloodstream infection, the median age was 63 years (53.25–74), of which 159 (64.6%) were male, 109 (44.3%) were elderly patients (> 65 years), 238 (96.7%) were hospitalised for more than 10 days, 168 (68.3%) were admitted to ICU during hospitalisation, and most patients had records of multiple admissions within 2 years (167/246, 67.9%). The most common blood index was hypoproteinemia (169/246, 68.7%), and the most common inducement was urinary catheter use (210/246, 85.4%). Moreover, the most frequently infected fungi and bacteria were Candida parapsilosis and Acinetobacter baumannii, respectively. The main predictors of death prognosis by machine learning method are serum creatinine level, age, length of stay, stay in ICU during hospitalisation, serum albumin level, C-Reactive protein (CRP), leukocyte count, neutrophil count, Procalcitonin (PCT), and total bilirubin level.
Conclusion
Our results showed that the most common candida and bacteria infections were caused by Candida parapsilosis and Acinetobacter baumannii, respectively. The main predictors of death prognosis are serum creatinine level, age, length of stay, stay in ICU during hospitalisation, serum albumin level, CRP, leukocyte count, neutrophil count, PCT and total bilirubin level.
Similar content being viewed by others
Background
Invasive candidal infection and bacterial bloodstream infections are common in hospitals [1, 2]. It is reported that approximately 1.5 million patients with invasive candidal infection die every year worldwide [3, 4]. Bacterial bloodstream infection is the seventh leading cause of death in North America and Europe [5]. In addition, in these regions, the average annual mortality is 29 cases per 100,000 population, and the total mortality is between 13 and 20% [5]. However, the epidemiological characteristics of both invasive candidal infection and bacterial bloodstream infections differ with geographic location and time [6,7,8,9,10,11,12]. In the past two decades, the incidence of non-Candida albicans infection has increased. A recent study from Japan revealed that Candida albicans was the infectious agent in 58.2% of all candidiasis cases in 2003 but only in 30% of cases in 2014. In addition, a study from China reported that Candida albicans was the causative agent in only 44.9% of invasive candidal infection cases [13], which is consistent with our previous study, which revealed that Candida albicans is no longer the most common invasive fungus [14]. The risk of death owing to invasive fungal and bacterial bloodstream infections puts enormous pressure on healthcare services, leading to a shortage of intensive care resources. However, in previous studies, the epidemiological characteristics and risk factors of invasive fungal infections complicated with bacterial bloodstream infections were rarely discussed, possibly owing to the limited capacity of some methods in analysing large datasets.
Machine learning techniques have the unique ability to deal with extensive data because they can process large datasets in a flexible and trainable manner and understand the complex relationship between variables [15]. Owing to their improved processing ability, various machine learning and artificial intelligence techniques are widely used to identify risk and prognostic factors of disease in patients to help clinicians. Therefore, we conducted a retrospective analysis of patients with invasive candidal infection concomitant with bacterial bloodstream infection and identified the prognostic indicators of death using machine learning methods.
Methods
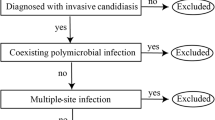
Patient selection
Patients were selected as previously described [14]. We collected all data on Candida, Cryptococcus and other yeast isolates recovered from the blood, ascitic fluid, peritoneal dialysate fluid, pus and tissues of patients with invasive candidal infection (2008 version of EORTC/MSG criteria). The onset of bacterial bloodstream infection or invasive candidal infection was defined as the date when the first positive result of blood culture was obtained. The data collected included patient characteristics at baseline, haematological diagnoses and chemotherapy, risk factors for invasive candidal infection, clinical features of invasive candidal infection, Candida test results, bacterial test results, antifungal prophylaxis and treatment and survival status at discharge. In addition, data regarding the management of patients receiving antifungal prophylaxis or therapy were recorded, including the date and nature of the change in treatment and survival status at discharge. The hospitalisation of each patient represented one event, and if a patient was re-hospitalised and received another round of treatment, he/she was considered a new event. Persistent candidal infections was defined as persistent if positive blood culture results were obtained for the same Candida species 7 days after the initiation of appropriate antifungal therapy [16]. We excluded non-Candida yeast samples and samples from non-sterile sources, such as faeces, urine, sputum, pharyngeal swabs and pus.
Microbiological tests
Aseptic humoral samples (8–10 mL) were collected and cultured for 5 days. Samples with positive results were transferred to blood agar plates, and subsequently, bacterial and fungal isolates were cultured at 35 °C for 48–72 h. Gram staining and microscopic examination were performed simultaneously. Strains (bacterial and fungal isolates) were identified on a VITEK 2 Compact system (Bio-Merieux SA, Marcy l ‘etoile, France), and susceptibility tests were performed using the ATB FUNGUS 3 kit (Bio-Merieux SA, Marcy l ‘etoile, France).
The minimum inhibitory concentration (MIC) was determined according to the CLSI m27-a3 and m27-s4 antifungal susceptibility test standards. The quality control strains used were Candida ATCC6258 and Candida albicans ATCC90028.
Machine learning methods
We pre-processed the data and deleted missing cases with 50% features, and the mean value of missing values was filled. The dataset was randomly divided into the training and test sets (7:3), with 70% patients in the training set and 30% patients in the test set. We used the random forest, logistic regression and support-vector machine algorithms to build a prediction model. Subsequently, the trained random forest model was analysed to evaluate the feature importance ranking.
Statistical analysis
The IBM SPSS Statistics for Windows version 20.0 software (IBM Corp., Armonk, NY, USA) was used for statistical analysis. Non-normally distributed quantitative data were expressed as median and quartile ranges [M (P25, P75)] and analysed using the Mann–Whitney test for intergroup comparisons. Qualitative data were represented by relative numbers, and the chi-square test was used for intergroup comparisons.
Definition and abbreviations
ICU, intensive care unit; SDD, susceptible-dose-dependent; PCT, procalcitonin; CRP, C-reactive protein; BDG, 1-3-β-d-glucan.
Prolonged hospitalisation was defined as hospital stay longer than 10 days. Surgery was defined as thoracic and abdominal surgeries. Recent surgery was defined as surgery performed 14 days before the first diagnosis of Candida infection. Abdominal surgery was defined as any surgery involving organs including the stomach, small intestine, colon or rectum, gallbladder, liver, pancreas, spleen and appendix. Concerning laboratory results, renal failure was defined as creatinine clearance < 60 mL/min, hypoalbuminaemia was defined as serum albumin concentration < 30 g/L and leukopaenia was defined as peripheral white blood cell count < 4 × 109cells/L. Prolonged ICU stay was defined as ICU stay for more than 10 days. Long-term and combined use of multiple antibiotics were defined as the use of antibiotics for more than 14 days and the simultaneous use of more than 2 antibiotics, respectively. Multiple bacterial infections were defined as infections with more than two types of bacteria simultaneously. Multiple fungal infections were defined as infections with more than two types of fungi simultaneously.
Results
Clinical features of patients
A total of 246 patients with invasive candidal infection complicated with bacterial bloodstream infection were included in this study. The median age of the patients was 63 years (53.25–74 years). Among the 246 patients, 159 (64.6%) were men, 109 (44.3%) were aged more than 65 years, 238 (96.7%) were hospitalised for more than 10 days, 168 (68.3%) had been admitted to ICU during hospitalisation and 167 (67.9%) had multiple admission records within the past 2 years. The common concomitant conditions of patients with invasive candidal infection complicated with bacterial bloodstream infection were hypoproteinaemia (169/246, 68.7% patients), surgery within the past 2 weeks (112/246, 45.5% patients), solid tumours (96/246, 39.0% patients), septic shock (58/246, 23.6% patients), diabetes (47/246, 19.1% patients), renal failure (36/246, 14.6% patients) and pancreatitis (25/246, 10.2% patients). Other common risk factors included the use of urinary catheter (210/246, 85.4% patients), central venous catheter (185/246, 75.2% patients), gastric tube (166/246, 67.5% patients), drainage catheter (168/246, 68.3% patients), invasive mechanical ventilation (153/246, 62.2% patients) and total parenteral nutrition (196/246, 79.7%). In addition, long-term use (181/246, 73.6%) and combined use of multiple antibiotics (162/246, 65.9%) were common in patients with invasive candidal infection complicated with bacterial bloodstream infection. Detailed data can be found in Additional file 1: Table S1.
The most common causative agent was Candida parapsilosis (infecting 92/246, 37.4% patients), followed by Candida guilliermondi (53/246, 21.5% patients), Candida albicans (49/246, 19.9% patients), Candida glabrata (26/246, 10.6% patients), Candida tropicalis (18/246, 7.3% patients), Candida krusei (4/246, 1.6% patients), Candida lusitaniae (2), Candida streptococcus (1) and Cryptococcus neoformans (1) (Fig. 1A).
Distribution of the pathogens found in the 246 hospitalized patients. A The most frequently infected fungi are Candida parapsilosis (92/246, 37.4%), followed by Candida guilliermondi (53/246, 21.5%), Candida albicans (49/246, 19.9%), Candida glabrata (26/246, 10.6%), Candida tropicalis (18/246, 7.3%), Candida krusei (4/246, 1.6%), Candida lusitaniae (2), Candida streptococcus (1), and Cryptococcus neoformans (1). B The most common bacterias infecting the patients were Acinetobacter baumannii (111/246, 45.1%), Enterococcus faecium (72/246, 29.3%), Pseudomonas aeruginosa (65/246, 26.4%), Escherichia coli (55/246, 22.4%), and Klebsiella pneumoniae (46/246, 18.7%)
Furthermore, 28 species of bacteria were isolated; of which, 15 (53.6%) were Gram-positive and 13 (46.4%) were Gram-negative. Moreover, Acinetobacter baumannii (111/246, 45.1% patients) was the most common causative agent of bacterial bloodstream infection, followed by Enterococcus faecium (72/246, 29.3% patients), Pseudomonas aeruginosa (65/246, 26.4% patients), Escherichia coli (55/246, 22.4% patients) and Klebsiella pneumoniae (46/246, 18.7% patients) (Fig. 1B). In addition, there were 73 (29.7%) cases of single and 173 (70.3%) cases of multiple bacterial bloodstream infections. Detailed data can be found in Additional file 2: Table S2.
In vitro antifungal susceptibility test
We obtained 239 isolates from 246 patients with drug sensitivity; of which, 19 (7.9%) isolates were resistant to at least one antifungal agent. Amphotericin B showed excellent results, as all strains were sensitive to it. The drug sensitivity of voriconazole and fluorouracil was good, achieving an efficiency of 96.6% (230/238) and 98.3% (235/239), respectively. In addition, the drug sensitivity of fluconazole and itraconazole was 85.8% (205/239) and 90.4% (216/239), respectively. Candida glabrata isolates were highly susceptible to fluconazole (18/26, 69.2%) and itraconazole (10/26, 38.5%) in a dose-dependent manner. Candida tropicalis isolates exhibited considerable resistance to fluconazole (5/17, 29.4%) and voriconazole (5/17, 29.4%), whereas Candida krusei isolates exhibited strong resistance to fluconazole (3/4, 75%). Detailed data can be found in Additional file 3: Table S3.
Risk factors for Candida albicans and non-Candida albicans infections
The demographic and clinical characteristics of patients with Candida albicans and non-Candida albicans infections are shown in Table 1. It was found that 34.69% patients with Candida albicans infection had diabetes; however, only 15.23% patients with candidiasis caused by a different Candida species had diabetes. Moreover, 81.63% patients with Candida albicans infection were admitted to ICU as opposed to 64.97% patients with candidiasis caused by a different Candida species. In addition, 65.31% patients with Candida albicans infection and 83.25% patients with candidiasis caused by a different Candida species were administered parenteral nutrition. Regarding catheterisation, 74.62% patients with catheter drainage had non-albicans candidiasis, whereas 42.86% patients with catheter drainage were infected with Candida albicans. In addition, patients with diabetes or those admitted to ICU had a higher risk of contracting Candida albicans infection, whereas parenteral nutrition and catheterisation increased the risk of non-albicans candidiasis. Differences were statistically significant.
Furthermore, the C-reactive protein (CRP) and procalcitonin (PCT) levels were markedly elevated in patients with invasive candidal infection complicated with bacterial bloodstream infection, especially in those with Candida albicans infection. In addition, the CRP and PCT levels were higher in patients with Candida albicans infection than in patients with non-Candida albicans infection, and the difference was statistically significant. However, both leukocyte and lymphocyte counts were within the normal range. Detailed data are provided in Table 1.
Analysis of risk factors in patients with persistent and non-persistent Candida infections
The demographic and clinical characteristics of patients with persistent and non-persistent Candida infection are shown in Table 2. Persistent Candida infection was associated with diabetes, longer stay in the ICU and renal failure. Differences were statistically significant.
Analysis of risk factors in patients with single and multiple candidal infections
Of the 246 patients with both Candida and bloodstream infections, 70 (28.45%) had multi-candidal infection and 176 (71.55%) patients had single candidal infection, and the demographic and clinical characteristics of patients are shown in Table 3.
Furthermore, the duration of hospital and ICU stays was longer in patients with multi-candidal infection than in patients with single candidal infection (hospital stay: 57 versus 42 days, respectively, based on the median; ICU stay: 22.5 versus 7 days, respectively, based on the median). In addition, patients with multi-candidal infection were more likely to have diabetes and develop septic shock. Furthermore, more than half (51.70%, 91/176) and approximately one-third (30%, 21/70) of post-surgical patients had multi-candidal infection. Moreover, when infected patients (not only post-surgical patients) were considered, 77.14% (84/176) patients with multi-candidal infection and 47.73% (54/70) patients with single candidal infection developed persistent infection, with increased CRP and PCT levels. The lymphocyte count was distinctly reduced in patients with single candidal infection (0.75 × 109/L based on the median) but only slightly reduced in patients with multi-candidal infection (1.02 × 109/L based on the median). Differences were statistically significant.
Prediction of risk factors of death using machine learning
We used random forest, logistic regression and support-vector machine algorithms to develop a prediction model, and the performance evaluation is shown in Table 4.
Figure 2 demonstrates the ROC curves of the prediction model. Based on analysis and training, it was found that the random forest model exhibited the best performance. A random forest model is usually used to examine the importance of different features. The most predictive characteristics of invasive candidal infection concomitant with bacterial bloodstream infection were identified to be serum creatinine, serum albumin, CRP, PCT and total bilirubin levels; age; length of stay in the hospital; stay in ICU during hospitalisation and leukocyte and neutrophil counts (Table 5).
Discussion
To date, there have been a few epidemiological studies on patients with concomitant invasive candidal infection and bacterial bloodstream infections. We included 246 patients with concomitant invasive candidal infection and bacterial bloodstream infections admitted to a provincial medical centre in northeast China between January 2013 and January 2018. Using machine learning techniques, we found that the main predictors of death were serum creatinine, serum albumin, CRP, PCT and total bilirubin levels; age; length of stay in the hospital; stay in ICU during hospitalisation and leukocyte and neutrophil counts. The random forest model with these 10 features showed satisfactory performance, and the AUC value in the training and test sets was 0.919.
Furthermore, the epidemiological survey revealed that 96.7% (238/246) patients were hospitalised for more than 10 days, and 68.3% (168/246) patients were admitted to ICU. Most patients had multiple admissions in the past 2 years (167/246, 67.9%) and had hypoproteinaemia (169/246, 68.7%). These conditions reflect the physical characteristics of patients, which are similar to those reported in recent studies [17, 18]. Other common causes of Candida infections included the use of urinary catheter (210/246, 85.4% patients), central venous catheter (185/246, 75.2% patients), gastric tube (166/246, 67.5% patients), drainage catheter (168/246, 68.3% patients), invasive mechanical ventilation (153/246, 62.2% patients) and total parenteral nutrition (196/246, 79.7% patients), suggesting that infections may be associated with invasive medical operations, especially owing to long-term catheter retention. Similar results have been reported in recent studies as well [19,20,21,22,23,24,25,26].
Candida parapsilosis was the most common causative fungal agent (92/246, 37.4% patients), followed by Candida guilliermondi (53/246, 21.5% patients), Candida albicans (49/246, 19.9% patients), Candida glabrata (26/246, 10.6% patients), Candida tropicalis (18/246, 7.3% patients) and Candida krusei (4/246, 1.6% patients). Furthermore, Acinetobacter baumannii (111/246, 45.1% patients) was the most common causative agent of bacterial bloodstream infection, followed by Enterococcus faecium (72/246, 29.3% patients), Pseudomonas aeruginosa (65/246, 26.4% patients), Escherichia coli (55/246, 22.4% patients) and Klebsiella pneumoniae (46/246, 18.7% patients). A total of 28 types of bacteria were cultured, with Gram-positive bacteria being the main pathogenic bacteria (15/28, 53.6%). In addition, the results indicated that the rate of Candida infection differed according to regions, which is an important factor that should be studied further [27, 28].
In this study, the main predictors of death were serum creatinine, serum albumin, CRP, PCT and total bilirubin levels; age; length of stay in the hospital; stay in ICU during hospitalisation and leukocyte and neutrophil counts. High serum creatinine level is a risk factor for bacterial bloodstream infection and may be associated with renal insufficiency [29, 30]. In addition, age is a significant prognostic risk factor for nosocomial infections, and elderly patients are more likely to present with underlying diseases, low immunity and decreased organ function, which makes them more susceptible to invasive candidal infection/bacterial bloodstream infection [31, 32]. The length of stay in the hospital is an important index influenced by many factors, including the demographic characteristics, treatment complexity, complications and discharge plan of patients, and can be used as a predictor of death [33, 34]. Studies have shown that the overall mortality rate of hospitalised patients increases with the increasing duration of ICU stay, possibly owing to complications resulting from long-term intensive care [35, 36]. In addition, serum albumin level is a nutritional index and an important indicator of morbidity and mortality in critically ill patients. Low serum albumin level is an important and unique predictor of mortality [37, 38]. CRP is a classic indicator of infection. Previous studies have shown that CRP can also be used as a prognostic indicator for hospitalised patients [39, 40]. In addition, this study shows that increased leukocyte counts indicate increased mortality in hospitalised patients with infection. Similar studies have shown that the death rate of patients with cancer and dengue increases with increasing leukocyte counts [41, 42]. Infections destroy the dynamic balance of the immune system and cause significant changes in the neutrophil count, which are closely related to mortality [43, 44]. Furthermore, PCT is a classic indicator of infection, and recent studies have shown that PCT can also be used as a prognostic indicator for hospitalised patients with infection [45, 46]. In addition, total bilirubin levels can be used as a prognostic indicator in patients with coronavirus infection, respiratory tract infection and cardiogenic shock, and increased serum bilirubin levels are independently associated with mortality [47,48,49].
However, this study had some limitations. First, this is a single-centre study. Therefore, the results and conclusions may be affected by geographical location, hospital management strategies, infection control policies and susceptibility models. Second, owing to a retrospective design, some key factors of concomitant invasive candidal infection and bacterial bloodstream infections may have been ignored. In addition, to the best of our knowledge, machine learning was used for the first time in this study to predict the risk factors of death and prognosis of concomitant invasive candidal infection and bacterial bloodstream infections. Moreover, the relatively small sample size may affect the credibility of the results. Therefore, further large-scale, multi-centre prospective studies should be conducted to validate the results of this study.
Conclusion
The most common Candida and bacterial species in patients with concomitant Candida and bacterial bloodstream infections in the First Hospital of the China Medical University were Candida parapsilosis and Acinetobacter baumannii, respectively. The main predictors of death were serum creatinine, serum albumin, CRP, PCT and total bilirubin levels; age; length of stay in the hospital; stay in ICU during hospitalisation and leukocyte and neutrophil counts.
Availability of data and materials
The data supporting the findings of this study from the corresponding author upon request. If someone wants to request the data from this study, please contact Xiuhao Guan.
References
Wilson J, Elgohari S, Livermore DM, Cookson B, Johnson A, Lamagni T, et al. Trends among pathogens reported as causing bacteraemia in England, 2004–2008. Clin Microbiol Infect. 2011;17(3):451–8.
Kullberg BJ, Arendrup MC. Invasive candidiasis. N Engl J Med. 2015;373(15):1445–56.
Brown GD, Denning DW, Gow NA, Levitz SM, Netea MG, White TC. Hidden killers: human fungal infections. Sci Transl Med. 2012;4(165):165rv13.
Kaushik N, Pujalte GG, Reese ST. Superficial fungal infections. Prim Care. 2015;42(4):501–16.
Goto M, Al-Hasan MN. Overall burden of bloodstream infection and nosocomial bloodstream infection in North America and Europe. Clin Microbiol Infect. 2013;19(6):501–9.
Suleyman G, Alangaden GJ. Nosocomial fungal infections: epidemiology, infection control, and prevention. Infect Dis Clin North Am. 2016;30(4):1023–52.
Perlroth J, Choi B, Spellberg B. Nosocomial fungal infections: epidemiology, diagnosis, and treatment. Med Mycol. 2007;45(4):321–46.
Tang CQ, Li JQ, Shou BM, Pan BH, Chen TS, Xiao YQ, et al. Epidemiology and outcomes of bloodstream infections in 177 severe burn patients from an industrial disaster: a multicentre retrospective study. Clin Microbiol Infect. 2018;24(2):199.e1-199.e7.
Schønheyder HC, Paul M. Placing the burden of bacteraemia in perspective. Clin Microbiol Infect. 2013;19(6):489–91.
Douglas NM, Hennessy JN, Currie BJ, Baird RW. Trends in bacteremia over 2 decades in the top end of the northern territory of Australia. Open Forum Infect Dis. 2020;7(11):ofaa472.
Rhodes J, Jorakate P, Makprasert S, Sangwichian O, Kaewpan A, Akarachotpong T, et al. Population-based bloodstream infection surveillance in rural Thailand, 2007–2014. BMC Public Health. 2019;19(Suppl 3):521.
Pfaller MA, Carvalhaes CG, Smith CJ, Diekema DJ, Castanheira M. Bacterial and fungal pathogens isolated from patients with bloodstream infection: frequency of occurrence and antimicrobial susceptibility patterns from the SENTRY Antimicrobial Surveillance Program (2012–2017). Diagn Microbiol Infect Dis. 2020;97(2):115016.
Xiao M, Sun ZY, Kang M, Guo DW, Liao K, Chen SC, et al. Five-year national surveillance of invasive candidiasis: species distribution and azole susceptibility from the China hospital invasive fungal surveillance net (CHIF-NET) Study. J Clin Microbiol. 2018;56(7).
Li Y, Gao Y, Niu X, Wu Y, Du Y, Yang Y, et al. A 5-year review of invasive fungal infection at an academic medical center. Front Cell Infect Microbiol. 2020;10:553648.
Goecks J, Jalili V, Heiser LM, Gray JW. How machine learning will transform biomedicine. Cell. 2020;181(1):92–101.
Kim SH, Yoon YK, Kim MJ, Sohn JW. Clinical impact of time to positivity for Candida species on mortality in patients with candidaemia. J Antimicrob Chemother. 2013;68(12):2890–7.
Zhong L, Zhang S, Tang K, Zhou F, Zheng C, Zhang K, et al. Clinical characteristics, risk factors and outcomes of mixed Candida albicans/bacterial bloodstream infections. BMC Infect Dis. 2020;20(1):810.
Bouza E, Burillo A, Muñoz P, Guinea J, Marín M, Rodríguez-Créixems M. Mixed bloodstream infections involving bacteria and Candida spp. J Antimicrob Chemother. 2013;68(8):1881–8.
Bell T, O’Grady NP. Prevention of central line-associated bloodstream infections. Infect Dis Clin North Am. 2017;31(3):551–9.
Luzum M, Sebolt J, Chopra V. Catheter-associated urinary tract infection, Clostridioides difficile Colitis, central line-associated bloodstream infection, and methicillin-resistant Staphylococcus aureus. Med Clin North Am. 2020;104(4):663–79.
Álvarez-Marín R, Navarro-Amuedo D, Gasch-Blasi O, Rodríguez-Martínez JM, Calvo-Montes J, Lara-Contreras R, et al. A prospective, multicenter case control study of risk factors for acquisition and mortality in Enterobacter species bacteremia. J Infect. 2020;80(2):174–81.
Odabasi Z, Mert A. Candida urinary tract infections in adults. World J Urol. 2020;38(11):2699–707.
Zhang W, Song X, Wu H, Zheng R. Epidemiology, species distribution, and predictive factors for mortality of candidemia in adult surgical patients. BMC Infect Dis. 2020;20(1):506.
Sitges-Serra A, Girvent M. Catheter-related bloodstream infections. World J Surg. 1999;23(6):589–95.
Fätkenheuer G, Cornely O, Seifert H. Clinical management of catheter-related infections. Clin Microbiol Infect. 2002;8(9):545–50.
Pappas PG, Lionakis MS, Arendrup MC, Ostrosky-Zeichner L, Kullberg BJ. Invasive candidiasis. Nat Rev Dis Primers. 2018;4:18026.
Buil JB, Meijer E, Denning DW, Verweij PE, Meis JF. Burden of serious fungal infections in the Netherlands. Mycoses. 2020;63(6):625–31.
Jun BG, Lee WC, Jang JY, Jeong SW, Kim YD, Cheon GJ, et al. Follow-up creatinine level is an important predictive factor of in-hospital mortality in cirrhotic patients with spontaneous bacterial peritonitis. J Korean Med Sci. 2018;33(12):e99.
Zhang V, Woo A, Scaduto C, Cruz M, Tan YY, Du H, et al. Systematic review on the definition and predictors of severe Clostridiodes difficile infection. J Gastroenterol Hepatol. 2021;36(1):89–104.
Aguirre-Avalos G, Mijangos-Méndez JC, Zavala-Silva ML, Coronado-Magaña H, Amaya-Tapia G. Bacteremia caused by Acinetobacter baumannii among patients in critical care. Gac Med Mex. 2009;145(1):21–5.
Wisplinghoff H, Ebbers J, Geurtz L, Stefanik D, Major Y, Edmond MB, et al. Nosocomial bloodstream infections due to Candida spp. in the USA: species distribution, clinical features and antifungal susceptibilities. Int J Antimicrob Agents. 2014;43(1):78–81.
Awad A, Bader-El-Den M, McNicholas J. Patient length of stay and mortality prediction: a survey. Health Serv Manage Res. 2017;30(2):105–20.
Hofstede SN, van Bodegom-Vos L, Kringos DS, Steyerberg E, Marang-van de Mheen PJ. Mortality, readmission and length of stay have different relationships using hospital-level versus patient-level data: an example of the ecological fallacy affecting hospital performance indicators. BMJ Qual Saf. 2018;27(6):474–83.
Moitra VK, Guerra C, Linde-Zwirble WT, Wunsch H. Relationship between ICU length of stay and long-term mortality for elderly ICU survivors. Crit Care Med. 2016;44(4):655–62.
Pintado MC, Villa P, Luján J, Trascasa M, Molina R, González-García N, et al. Mortality and functional status at one-year of follow-up in elderly patients with prolonged ICU stay. Med Intensiva. 2016;40(5):289–97.
Kendall H, Abreu E, Cheng AL. Serum albumin trend is a predictor of mortality in ICU patients with sepsis. Biol Res Nurs. 2019;21(3):237–44.
Touma E, Bisharat N. Trends in admission serum albumin and mortality in patients with hospital readmission. Int J Clin Pract. 2019;73(6):e13314.
Bozkurt I, Esen S. Association between severity grading score and acute phase reactants in patients with Crimean Congo hemorrhagic fever. Pathog Glob Health. 2021;115:496.
Zhang S, Zhang X, Yu W, Lin Z, Chen D. Infection biomarkers in assisting the judgement of blood stream infection and patient prognosis: a retrospective study incorporating principal components analysis. Ann Transl Med. 2020;8(23):1581.
Miyagi T, Miyata S, Tagami K, Hiratsuka Y, Sato M, Takeda I, et al. Prognostic model for patients with advanced cancer using a combination of routine blood test values. Support Care Cancer. 2021;29:4431.
Nandwani S, Bhakhri BK, Singh N, Rai R, Singh DK. Early hematological parameters as predictors for outcomes in children with dengue in northern India: a retrospective analysis. Rev Soc Bras Med Trop. 2021;54:e05192020.
Dong X, Wang C, Liu X, Bai X, Li Z. The trajectory of alterations in immune-cell counts in severe-trauma patients is related to the later occurrence of sepsis and mortality: retrospective study of 917 cases. Front Immunol. 2020;11:603353.
Duan Y, Ou X, Chen Y, Liang B, Ou X. Severe influenza with invasive pulmonary aspergillosis in immunocompetent hosts: a retrospective cohort study. Front Med (Lausanne). 2020;7:602732.
Covino M, Fransvea P, Rosa F, Cozza V, Quero G, Simeoni B, et al. Early procalcitonin assessment in the emergency department in patients with intra-abdominal infection: an excess or a need. Surg Infect (Larchmt). 2021;22:787.
Kakeya H, Yamada K, Kaneko Y, Yanagihara K, Tateda K, Maesaki S, et al. National trends in the distribution of Candida species causing candidemia in Japan from 2003 to 2014. Med Mycol J. 2018;59(1):E19–22.
Kurul Ş, Simons S, Ramakers C, De Rijke YB, Kornelisse RF, Reiss I, et al. Association of inflammatory biomarkers with subsequent clinical course in suspected late onset sepsis in preterm neonates. Crit Care. 2021;25(1):12.
Liu Z, Li J, Long W, Zeng W, Gao R, Zeng G, et al. Bilirubin levels as potential indicators of disease severity in coronavirus disease patients: a retrospective cohort study. Front Med (Lausanne). 2020;7:598870.
Fan H, Fan J, Chen S, Chen Y, Gao H, Shan L, et al. Prognostic significance of end-stage liver diseases, respiratory tract infection, and chronic kidney diseases in symptomatic acute hepatitis E. Front Cell Infect Microbiol. 2020;10:593674.
Bunte S, Walz R, Merkel J, Torregroza C, Roth S, Lurati Buse G, et al. Bilirubin-a possible prognostic mortality marker for patients with ECLS. J Clin Med. 2020;9(6):1727.
Acknowledgements
The authors thank the patients, their families, and all investigators who participated in the study.
Funding
National Science and Technology Major Projects of China, Grant/Award Number (2018ZX10101003 and 2018ZX10712001).
Author information
Authors and Affiliations
Contributions
LYL and GXH were responsible for the study concept and design. LYL and WYT were responsible for data acquisition and data extraction. Data analysis was performed by LYL, WYT and LJY. The paper was drafted by LYL and GXH. All authors supervised the study. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki. This study was approved by The Human Ethics Review Committee of the First Hospital of China Medical University (No. 2021-260). The ethics review board of the First Hospital of China Medical University exempted the acquisition of informed consent because this was a retrospective study. Patients’ data confidentiality was fully respected during data collection and the preparation of the manuscript.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Detailed data of patients with invasive Candida infection complicated with bacterial bloodstream infection.
Additional file 2.
Detailed data on bacterial species in patients with bacterial bloodstream infection.
Additional file 3.
Detailed data of drug sensitivity results.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Y., Wu, Y., Gao, Y. et al. Machine-learning based prediction of prognostic risk factors in patients with invasive candidiasis infection and bacterial bloodstream infection: a singled centered retrospective study. BMC Infect Dis 22, 150 (2022). https://doi.org/10.1186/s12879-022-07125-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07125-8