Abstract
Background
Mycobacterium (M) talmoniae isolated from a patient with cystic fibrosis was first described in 2017, and cases of M. talmoniae remain exceedingly rare.
Case presentation
A 51-year-old woman had respiratory symptoms for 10 years. Diffuse panbronchiolitis (DPB) was detected at the first visit at our hospital. A cavity lesion in the apex of the left lung was found, and sputum and bronchoalveolar lavage fluid were acid-fast bacillus (AFB) smear- and culture-positive besides Pseudomonas aeruginosa. M. talmoniae was finally identified, and the standard combination therapy for non-tuberculous mycobacteria (NTM) was administered for 2 y referring to the drug-susceptibility test. Thereafter, the AFB culture was negative, the wall thickness of the lung cavity was ameliorated, and oxygen saturation improved.
Conclusions
We encountered a rare case of M. talmoniae with DPB, for which standard combination therapy was effective. M. talmoniae may be considered a potential pathogen of lung disease, especially in patients with bronchiectatic lesions.
Similar content being viewed by others
Background
While the number of tuberculosis cases are decreasing, the increase in non-tuberculous mycobacteria (NTM) cases has become a global problem. NTM are environmental organisms that are frequently isolated from soil and water [1]. Although over 180 species have been discovered to date, only several species are reported to cause pulmonary disease [1]. The most commonly isolated species are the Mycobacterium avium complex (MAC), the M. abscessus complex (M. abscessus subsp. abscessus, M. abscessus subsp. massiliense, M. abscessus subsp. bolletii) [1]. The M. fortuitum group is a rare cause of pulmonary disease except in cases of achalasia and lipoid pneumonia [2, 3]. M. gordonae most often represents tap water contamination [4]. In Japan, a recent study showed that MAC accounts for nearly 90% of all NTM cases [5].
M. talmoniae was first described in 2017 and was isolated from human respiratory samples in the United States (US) [6]. It was classified as the most basal species of the slow-growing Mycobacterium clade [6]. In 2019, three cases of M. talmoniae isolation were reported in the US, and all patients had bronchiectatic lesions as underlying disease including cystic fibrosis (CF) [7].
Diffuse panbronchiolitis (DPB), which was first reported in Japan in 1969 [8], is mainly found in East Asia [9]. Although small numbers of case reports have recently been described, DPB remains a rare disease in Western countries excluding cases among Asian immigrants [10, 11]. The cause of DPB is unclear, but the disease is characterized by chronic inflammation in respiratory bronchioles and sinobronchial infection [12]. Immunogenetic studies revealed an association with human leukocyte antigen (HLA)-B54 in Japanese and HLA-A11 in Koreans [13]. Although low-dose, long-term erythromycin therapy for DPB, the effect of which is mainly attributed to an anti-inflammatory action, has drastically improved the survival rate [14, 15], DPB patients generally suffer from causative pathogens including Pseudomonas aeruginosa [13] and NTM, particularly MAC, M. kansasii, and M. chelonae [16]. Infections by these pathogens are related to reduced mucociliary clearance with bronchiectasis, which are characteristic findings in DPB and pathologically similar to CF.
This current report showed the rare case of M. talmoniae combined with DPB including the course of treatment for NTM.
Case presentation
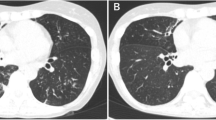
A 51-year-old woman had symptoms of cough and sputum for more than 10 years. Although the patient developed bronchiectasis at that time, it was not treated. Ten years later, in 2014, her symptoms of cough, sputum and breathlessness worsened, and she was referred to our hospital. As a medical history, she had more than 10 years of sinusitis. She did not have any relevant family history. At this initial visit, her height was 142.0 cm, body weight was 34.0 kg, and emaciation was remarkable. The patient did not have a fever, but a productive cough was heard during the examination. Coarse crackles were heard on auscultation. She had a part-time job in inventory despite a saturation of percutaneous oxygen (SpO2) rate of 91–92% at rest. Forced expiratory volume% in 1 s was dropped to 63.7%. A high-resolution computed tomography scan taken at the first consultation showed typical DPB findings, i.e., bilateral basal predominant bronchiectasis and centrilobular opacities with branching lines (Fig. 1). We diagnosed her with DPB, and she had HLA-B54 and HLA-A11. A cavity lesion in the apex of the left lung was also found (Fig. 2a). The sputum was acid-fast bacillus (AFB) smear-positive and culture-positive in liquid media after 6 days. Bronchoscopy was also performed, and bronchoalveolar lavage fluid was AFB smear-positive and culture-positive after 8 days. However, no NTM species corresponding to 17 types including M.avium, M.intracellulare, M.kansasii, M.marinum, M.simiae, M.scrofulaceum, M.gordonae, M.szulgai, M.gastri, M.xenopi, M.nonchromogenicum, M.terrae, M.triviale, M.fortuitum, M.chelonae, M.abscessus, M.peregrinum were identified with the DNA-DNA hybridization method. P. aeruginosa was also isolated from her sputum. She received treatment with long-term, low-dose erythromycin for DPB. Her condition had been stable, but the cavity enlarged and the cavity wall gradually thickened (Fig. 2a-b). Her sputum remained acid-fast bacillus smear-positive and culture-positive, which was considered to be a cause of the wall thickness. Respiratory samples were sent to the Research Institute of Tuberculosis, Japan Anti-tuberculosis Association to identify the mycobacterial species.
Comparison of the cavity lesion on coronal sections of high-resolution computed tomography. Images attached to the right shoulder are magnified views of cavity lesions. a A cavity lesion of the left lung apex was small at the first visit at our institution in 2014. b In 2017, the cavity lesion expanded and the wall thickened just before NTM treatment. c Repeat imaging in 2018, after NTM treatment, shows that the cavity wall is thinner
An isolate cultured on 2% Ogawa medium (Kyokuto Pharmaceuticals, Tokyo, Japan) was harvested and suspended in 500 μl of TE buffer. The suspension was boiled for 10 min for DNA extraction, centrifuged for 5 min at 12,000 xg, and 10 μl of the supernatant was used for PCR amplification of 16S rRNA (primer 285-rP2). The sequence was then analyzed by Applied Biosystems 3730xl DNA analyzer (Macrogen, Seoul, South Korea), and the result was subjected to BLAST homology search. The isolate showed 100% nucleotide homology to the 16S rRNA sequence of M. talmoniae type strain ATCC BAA-2683, while other species showed < 98% similarity. Thus, more than 2 years after her first visit, the patient was finally diagnosed with M. talmoniae infection at the end of 2016.
Susceptibility testing of the patient isolate was performed using BrothMIC NTM (Kyokuto Pharmaceuticals, Tokyo, Japan) which was the method based on the Clinical and Laboratory Standard Institute (CLSI) in 2003 and was commonly used in Japan. Table 1 showed some of the minimal inhibitory concentration (MIC) results for antimicrobials. It inferred to be susceptible to amikacin, clarithromycin, rifampicin and to be resistant to levofloxacin referring MAC in vitro MIC category decision by BrothMIC NTM. Levofloxacin was included in the BrothMIC NTM test instead of ciprofloxacin or moxifloxacin in Japan. Therefore, the patient was started on daily standard treatment for NTM (600 mg clarithromycin, 150 mg rifampicin, and 500 mg ethambutol). Approximately 5 months after the start of treatment, sputum was AFB smear-negative and culture-negative. She continued treatment for 2 years. The thickened wall of the giant cavity improved (Fig. 2c), and the SpO2 rate increased from 91 to 92% to 93–94%. Her productive cough and shortness of breath were improved, and she could take care of her parents. After 2 years of combination therapy, acid-fast bacillus smear and culture remained negative with every half year sputum inspection.
Discussion and conclusions
We encountered a case of M. talmoniae with DPB, in which standard combination therapy for NTM was effective. Clinical cases of M. talmoniae remain rare. Since M. talmoniae was first reported in 2017 [6], three previous isolations as clinical cases and only one clinical case requiring treatment of this NTM have been reported in the US to date [7]. In our case, NTM was found early in the clinical course, however, the species was not identified for 2.5 years.
NTM are environmental organisms that cause lung disease, especially in patients with pre-existing lung damage [17]. In our case, when the patient first visited another hospital in 2004, the cavity in the apex of the left lung was not detected. However, 10 years later, the cavity lesion appeared and gradually expanded 2 years later. In general, the local cavitary lesion in DPB is atypical. Kurashima et al. demonstrated that small nodules of MAC progress to cavities over a mean duration of 10 years in patients with middle lobe syndrome [18]. Therefore, in the present case, previous bronchiectatic lesions associated with DPB may have developed into the cavity lesion by NTM. Defects in the mucociliary transport system are assumed to be a predisposing factor to NTM infection, as observed in CF [19]. The first clinical case of M. talmoniae was detected in a CF patient [7]. Although DPB is more common than CF in East Asia, including Japan, reduced mucociliary clearance with bronchiectasis is an overlapping pathological condition in both diseases.
Previous papers on M. talmoniae was exceedingly few. The Davidson, et al. publication states that the M. talmoniae species shows highest similarity (only 97%) by 16S rRNA gene sequence to the type strain of M. simie and highest similarity (only 92%) to M. avium by the rpoB gene (less commonly used than 16S rRNA gene) [6]. According to their study, although antimicrobial susceptibility testing MIC values of M. talmoniae differed from the M. avium control strain, it showed similar values on clarithromycin, rifampin and ethambutol [6]. Another study reported three cases of M. talmoniae isolated from a human respiratory sample, and all three cases showed similar antimicrobial susceptibility which was susceptible to amikacin, clarithromycin, rifampin, and resistant to ciprofloxacin, linezolid, and minocycline [7]. Only one case with CF among them was treated by clarithromycin, rifampin, and ethambutol, and after 1 month of treatment her sputum became AFB smear and culture negative [7]. In our case, the M. talmoniae strain isolated from the patient’s respiratory samples was similarly susceptible to antimicrobials to clarithromycin, rifampicin and amikacin as seen in Table 1. Therefore, we treated the patient with standard combination therapy for NTM including clarithromycin, rifampicin, and ethambutol. Although symptoms of cough and sputum improved after low-dose erythromycin therapy, hypoxemia did not recover. However, after NTM treatment, both symptoms and clinical presentation, including the thickened giant cavity wall, improved. This result suggests that M. talmoniae was partially responsible for the patient’s clinical disease.
Although M. talmoniae infection remains uncommon, M. talmoniae should be considered as a potential pathogen of lung disease, especially in patients with bronchiectatic lesions.
Availability of data and materials
The classification reference databases were downloaded from National Center Biotechnology Information (https://www.ncbi.nlm.nih.gov/). The data used or analyzed in this case report and more detailed data are available from the corresponding author on reasonable request.
Abbreviations
- AFB:
-
Acid-fast bacillus
- CF:
-
Cystic fibrosis
- CLSI:
-
Clinical and Laboratory Standards Institute
- DPB:
-
Diffuse panbronchiolitis
- HLA:
-
Human leukocyte antigen
- M :
-
Mycobacterium
- MAC:
-
Mycobacterium avium complex
- MIC:
-
Minimal inhibitory concentration
- NTM:
-
Non-tuberculous mycobacteria
- SpO2 :
-
Saturation of percutaneous oxygen
- US:
-
The United States
References
Cowman S, van Ingen J, Griffith DE, Loebinger MR. Non-tuberculous mycobacterial pulmonary disease. Eur Respir J. 2019;54(1). https://doi.org/10.1183/13993003.00250-2019.
Hirata M, Kohno K, Murakami S, Yoneda S, Kajita Y, Fujita Y, et al. A case of recurrent aspiration pneumonia by achalasia. Nihon Kokyuki Gakkai Zasshi. 2002;40(2):149–53.
Lessing MP, Walker MM. Fatal pulmonary infection due to Mycobacterium fortuitum. J Clin Pathol. 1993;46(3):271–2.
Satta Y, Yamashita M, Matsuo Y, Kiyokawa H, Sato Y, Takemura H, et al. Non-tuberculous mycobacterial pseudo-outbreak of an intestinal culture specimen caused by a water tap in an endoscopy unit. Intern Med. 2020;59(22):2811–5.
Namkoong H, Kurashima A, Morimoto K, Hoshino Y, Hasegawa N, Ato M, et al. Epidemiology of pulmonary Nontuberculous mycobacterial disease, Japan. Emerg Infect Dis. 2016;22(6):1116–7.
Davidson RM, DeGroote MA, Marola JL, Buss S, Jones V, McNeil MR, et al. Mycobacterium talmoniae sp. nov., a slowly growing mycobacterium isolated from human respiratory samples. Int J Syst Evol Microbiol. 2017;67(8):2640–5.
Vasireddy R, Vasireddy S, Brown-Elliott BA, Greninger AL, Davidson RM, Ard KL, et al. Mycobacterium talmoniae, a Potential Pulmonary Pathogen Isolated from Multiple Patients with Bronchiectasis in the United States, Including the First Case of Clinical Disease in a Patient with Cystic Fibrosis. J Clin Microbiol. 2019;57(2). https://doi.org/10.1128/JCM.00906-18.
Yamanaka A, Saiki S, Tamura S, Saito K. Problems in chronic obstructive bronchial diseases, with special reference to diffuse panbronchiolitis. Naika. 1969;23(3):442–51.
Lin X, Lu J, Yang M, Dong BR, Wu HM. Macrolides for diffuse panbronchiolitis. Cochrane Database Syst Rev. 2015;1:CD007716.
Keicho N, Kudoh S. Diffuse panbronchiolitis: role of macrolides in therapy. Am J Respir Med. 2002;1(2):119–31.
Urbano Aranda Y, Garcia San Jose I, Lopez Gabaldon E. Diffuse panbronchiolitis: a very rare disease in Western countries. Arch Bronconeumol. 2012;48(5):184–5.
Homma H, Yamanaka A, Tanimoto S, Tamura M, Chijimatsu Y, Kira S, et al. Diffuse panbronchiolitis. A disease of the transitional zone of the lung. Chest. 1983;83(1):63–9.
Keicho N, Hijikata M. Genetic predisposition to diffuse panbronchiolitis. Respirology. 2011;16(4):581–8.
Kudoh S, Azuma A, Yamamoto M, Izumi T, Ando M. Improvement of survival in patients with diffuse panbronchiolitis treated with low-dose erythromycin. Am J Respir Crit Care Med. 1998;157(6 Pt 1):1829–32.
Poletti V, Casoni G, Chilosi M, Zompatori M. Diffuse panbronchiolitis. Eur Respir J. 2006;28(4):862–71.
Tsuji T, Tanaka E, Yasuda I, Nakatsuka Y, Kaji Y, Yasuda T, et al. Nontuberculous mycobacteria in diffuse panbronchiolitis. Respirology. 2015;20(1):80–6.
Aksamit TR. Mycobacterium avium complex pulmonary disease in patients with pre-existing lung disease. Clin Chest Med. 2002;23(3):643–53.
Kurashima A. Clinical study on development of nontuberculous mycobacterial lung disease. Kekkaku. 2004;79(12):737–41.
Olivier KN, Weber DJ, Wallace RJ Jr, Faiz AR, Lee JH, Zhang Y, et al. Nontuberculous mycobacteria. I: multicenter prevalence study in cystic fibrosis. Am J Respir Crit Care Med. 2003;167(6):828–34.
Acknowledgments
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
TS, MS and KN were involved in the clinical management of this patient. YI and SM performed the identification of M. talmoniae. This manuscript was initially drafted by TS, MS and KN, and then revised by other authors in this study. All authors approved the final manuscript.
Authors’ information (optional)
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written consent for case publication was obtained from the patient. The need for approval was waived off by the Independent Ethics Committee of Fukushima Medical University.
Consent for publication
Written consent for case publication was obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Suzuki, T., Saitou, M., Igarashi, Y. et al. Isolation of Mycobacterium talmoniae from a patient with diffuse panbronchiolitis: a case report. BMC Infect Dis 21, 251 (2021). https://doi.org/10.1186/s12879-021-05944-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-021-05944-9