Abstract
Background
Identifying patients with hepatitis C virus (HCV) infection and enhancing the cascade of care are essential for eliminating HCV infection. This study aimed to estimate the prevalence of positive anti-HCV serology in Brasilia, Brazil, and evaluate the efficiency of the cascade of care for HCV-positive individuals.
Methods
This cross-sectional study analyzed 57,697 rapid screening tests for hepatitis C in individuals aged > 40 years between June 2018 and June 2019. HCV-positive patients were contacted and scheduled to undergo the HCV RNA viral test, genotyping, and transient elastography.
Results
The prevalence of positive serology was 0.27%. Among 161 patients with positive anti-HCV serology, 124 (77%) were contacted, 109 (67.7%) were tested for HCV RNA viral load, and 69 (42.8%) had positive results. Genotype 1 (75%) was the most prevalent genotype. Among 65 patients (94.2%) who underwent transient elastography, 30 (46.2%) presented with advanced fibrosis. Additionally, of the 161 patients, 55 (34.1%) were referred for treatment, but only 39 (24.2%) complied, with 36 (22.4%) showing sustained virological response. By the end of the study, 16 patients were still awaiting to receive medication.
Conclusions
The prevalence of HCV-positive patients was low in Brasilia, and the gaps in the cascade of care for these patients were significantly below the targets of HCV infection elimination. This study opens new avenues for eliminating HCV infection and suggests that partnerships with clinical laboratories to conduct anti-HCV tests are a useful strategy to improve HCV diagnosis.
Trial registration
Research Ethics Committee of the Faculty of Health Sciences of the University of Brasília - UNB (CAAE number 77818317.2.0000.0030) and by the Ethics Committee of the Health Science Teaching and Research Foundation - FEPECS/SES/DF (CAAE number 77818317.2.3001.5553).
Similar content being viewed by others
Background
Chronic hepatitis C is a global public health problem, with a risk of progression to cirrhosis and hepatocellular carcinoma (HCC) [1, 2]. Hepatitis C is also associated with several comorbidities, such as cardiovascular and metabolic disease [3]. In 2017, an estimated 71 million people (about 1% of the world population) had active hepatitis C virus (HCV) infection, according to the Global Hepatitis Report by the World Health Organization (WHO) [4, 5]. Despite recent advances in hepatitis C treatment, the number of people with advanced liver disease and the number of liver disease-related deaths are predicted to increase in the coming years, [6]. with about 40% of liver cancers expected to be caused by HCV by 2030 [7]. To address this issue, it is crucial that the number of diagnoses and the access to treatment in most countries must be increased at least fivefold [8]. Currently, the main challenge is improving the diagnosis of chronic hepatitis C and having patients commence treatment to prevent liver cirrhosis and HCC [7, 9, 10]. Therefore, expanding the knowledge of HCV infection is essential to establish new HCV prevention and elimination programs in Brazil [4, 11].
A strategic plan has been outlined recently to address HCV infection in Brazil. It comprises incorporating new, effective, affordable drugs guiding physicians in treating HCV patients, and promoting diagnostic campaigns in populations aged > 40 years, as recent studies have shown a higher prevalence of infection [8, 12, 13]. Studies assessing HCV prevalence in Brazil are scarce, and the HCV seroprevalence is estimated between 0.69 to 1.89% [6, 13, 14]. The first Brazilian nationwide hepatitis survey demonstrated an HCV seroprevalence of 1.38% in 19,503 individuals [13]. It is postulated that the HCV prevalence in Brazil increased with age and is higher in adults born between 1950 and 1980, with genotype 1 most prevalent of chronic infections [6, 13, 14]. These studies confirmed Brazil as a country with low endemicity for hepatitis C.
Hepatitis C is commonly diagnosed by serological tests. Anti-HCV antibodies can be detected by immunological methods; however, these methods are costly and require long procedure times [15, 16]. In 2011, the US Food and Drug Administration approved the use of rapid tests (RTs) to detect HCV infection. RTs are easy to perform, yield faster results, and are cheaper [15]. Because RT shares a sensitivity and specificity similar to other HCV serological methods, they do not need a laboratory structure and are a great approach to increasing HCV diagnosis [17]. Considering an HCV seroprevalence of 0.71% in Brazil (based on a mathematical modeling approach), it would be necessary to increase the number of RTs performed annually to improve diagnosis and treatment and establish an HCV elimination program in the country [18].
With the high efficacy of new direct antiviral agents (DAAs), in Brazil, the challenge exists in need to identify and treat infected patients [19]. However, the lack of an efficient cascade of care for chronic HCV infection in Brazil hinders the diagnosis of the disease and access to treatment, which are the most critical factors for eliminating HCV infection and reducing HCV-related mortality [20]. This descriptive, observational, cross-sectional study aimed to evaluate the efficiency of the cascade of care for HCV-positive patients among people aged > 40 years in Brasilia, Brazil. Since we have examined a large population distributed throughout the Brasilia, Federal District, Brazil, we also decided to estimate the prevalence of positive anti-HCV serology by RT in these subjects.
Methods
Study setting
This study was conducted in Brasilia, Federal District, Brazil, which has a total population of approximately 2.974 million and an estimated aged > 40 years population of approximately 1.070 million, according to the Brazilian Institute of Geography and Statistics (IBGE) and the country’s public health agencies.
Study subjects
This cross-sectional study was conducted between June 2018 and June 2019 as collaboration between the Brazilian Association of Hepatitis Carriers (ABPH) and the Sabin Laboratory. All subjects signed an informed consent form before participating in the study, in which the design design was approved by the Research Ethics Committee of the Faculty of Health Sciences of the University of Brasilia and the Ethics Committee of the Health Science Teaching and Research Foundation. Anti-HCV rapid tests (RTs) were performed free of charge for all individuals aged > 40 years at the Sabin Laboratory as screening tests to diagnose hepatitis C. The screening tests of the study subjects were carried out along with other requested blood tests. The Sabin Laboratory has several units in Brasilia, with an average attendance of approximately 500,000 people annually over the last 40 years, and holds international certifications, such as ISO 9001, ISO 14001, and ISO 31000, which attest to quality management processes.
Inclusion criteria
Patients included in the study were adults aged over 40 years. HCV tests were performed voluntarily and when patients were submitted to any other type of blood laboratory test ordered by different physicians that were collected at several units of Sabin Laboratory in the Federal District between June 2018 and June 2019.
Qualitative tests
The rapid anti-HCV test is an immunochromatographic qualitative test based on the use of captures antigens (core, NS3, NS4, and NS5) for selective identification of anti-HCV antibodies. If antibodies are present in the blood sample, they bind to capture antigen conjugates that are flowing through the membrane of the test device and are captured by antigens that are immobilized in the same area. This reaction produces a colored line in the test area. Conjugates that do not bind to the test area continue to flow and bind to immobilized reagents in the control area, also producing a colored line, demonstrating that the test reagents are working correctly [17, 21].
Both the WHO and the Brazilian Ministry of Health have established sensitivity (> 98% versus > 97%) and specificity (99.4% versus 99.4%) criteria to assess the quality of RTs for hepatitis C [22]. The Alere® rapid anti-HCV tests (Standard Diagnostics, South Korea; distributed by Bioeasy Diagnostica Ltda., Belo Horizonte and São Paulo, Brazil) were used in this study, and their sensitivity and specificity (100 and 92.7%, respectively) were compatible with the minimum criteria required [22, 23].
Blood sample collection
Blood samples for the rapid anti-HCV test were collected by routine venipuncture during other ordered blood tests at the several units of the Sabin Laboratory in the Federal District. The samples were sent to the Sabin Laboratory headquarters, where each sample was centrifuged, and the serum was used to the test. RTs were performed, and a qualified biochemical professional interpreted the results in compliance with quality and safety standards. The tests were conducted according to manufacturer instructions [21, 22].
Clinical investigation
Patients who tested positive were contacted by telephone and referred to the liver disease outpatient clinic of the Base Hospital Institute of the Federal District (IHBDF), a high-complexity public hospital in Brasilia, for consultation and further clinical investigation with HCV RNA viral load tests and genotyping using molecular biology techniques with real-time polymerase chain reaction (PCR). These tests were performed at the Central Public Health Laboratory of the Federal District or the Sabin Laboratory, and the results were retrieved from the electronic medical records. During the consultation, in addition to anamnesis and physical examination, transient elastography (TE) was performed.
Patients were considered lost to follow-up after three failed attempts to contact them by telephone or if they missed an appointment in the liver disease outpatient clinic at the IHBDF. Telephone calls were attempted at the time of the RT result, 30 days after the RT, and 3 months after the RT.
Liver fibrosis grade in patients was assessed by TE using Fibroscan® 502 (Echosens, Paris, France) during the hepatology consultations. Results of the liver stiffness measurement (LSM) were expressed in kilopascals (kPa), and those of the controlled attenuation parameter (CAP) measurement employed to quantify hepatic steatosis were described in decibels per meter (dB/m). The median values of 10 successful results of both measurements were obtained. A failure was defined as no single successful measurement, and an unreliable measurement was defined as an interquartile range to liver stiffness measurement ratio of > 0.30 [24,25,26].
Statistical analysis
Epidemiological information, test results, and treatment indicated for each patient were grouped in a spreadsheet using Microsoft Office Excel 2013 software. All data, including age, sex, address, and results of complementary examinations, were categorized. Data were normally distributed, and continuous variables were expressed as means ± standard deviation, while categorical variables were expressed as percentages. The t-test for independent samples was used to compare means, while the chi-square test was used to compare proportions. Results were considered statistically significant when p < 0.05.
To estimate the sample size, it has been taken into account the estimated aged > 40 years population in Federal District (1.070 million), the margin of error of 0.4% and the confidence level of 95%. This resulted the number of 56.837 individuals to be analyzed as a minimum goal to be achieved.
The data were analyzed in SPSS for Mac OS X© (v.20.0.0; SPSS, Inc., Chicago, IL, USA).
Results
Estimated prevalence at the Federal District
Overall, 62,449 RTs were conducted as screening tests for hepatitis C in individuals aged > 40 years. Of these tests, 58,730 were performed in patients residing in the Federal District; the remaining 3719 RTs were excluded because they were executed in patients from other states, and 1033 RTs were excluded because they were performed inappropriately in patients aged < 40 years. Therefore, a total of 57,697 RTs was included in the study.
Anti-HCV seroprevalence in the Federal District
In total, 181 patients had positive and valid RT results for HCV; among them, 161 resided in Brasilia, Federal District. Of the 161 patients, 124 (77%) were successfully contacted and were included in the study. It was not possible to contact the remaining 37 patients due to the lack of a valid telephone number or lack of response after three call attempts.
Considering the number of RTs performed in patients residing in the Federal District (57,697) and the number of HCV-positive patients (161), the prevalence found in this study was 0.27% (161/57,697).
In 21,291 RTs performed in male patients, 80 were positive (0.37%). Meanwhile, in 36,406 RTs performed in female patients, 81 were positive (0.22%), which was significantly lower than that in males (p < 0.001).
As shown in Table 1, HCV seroprevalence was higher in patients aged 50–69 years and lower in patients aged 40–49 years.
Cascade of care
As shown in Fig. 1, of 161 patients with positive anti-HCV RTs, 124 (124/161 = 77%) were contacted by telephone and requested to attend a medical consultation at the IHBDF hepatology outpatient clinic. Among them, 109 (109/161 = 67.7%) attended the appointment. Moreover, all of them were tested for HCV RNA using PCR, and 69 (69/161 = 42.8%) were positive. As a means of continuing the cascade of care, all 69 patients were genotyped, and 65 were referred for TE using FibroScan®, only 4 patients did not attend Fibroscan®. A total of 55 (55/161 = 34.1%) patients were referred for clinical treatment with oral DAA regimens. Among them, 39 (39/161 = 24.2%) started treatment, but the remaining 16 did not because they were still waiting to receive medication at the end of the study. Of the patients who were on treatment, 36 (36/161 = 22.4%) had sustained virologic response (SVR) after 12 weeks of treatment. The SVR rate during the post-treatment follow-up at 12 weeks was 92.3% (36/39). One of the patients did not achieve SVR, other died during treatment due to cirrhosis complications, and another abandoned the study during the follow-up.
The other 20 patients with positive anti-HCV RT results who were not residents of the Federal District were contacted by telephone and referred to the specialized service for liver diseases at the IHBDF for clinical investigation and propaedeutic but were not included in the cascade of care.
Of the 124 patients with positive RTs who were contacted by telephone, 70 (70/124 = 56.5%) had never been screened for hepatitis C, and they expressed interest in continuing the investigation to evaluate possible chronic HCV infection, as shown in Fig. 2. On the other hand, 54 patients (54/124 = 43.5%) already knew of their positive anti-HCV serology results, and 20 (20/124 = 16.1%) were already being monitored and had already received treatment. These 54 HCV-positive patients were also invited to participate in the study to attend consultations for clinical investigation with HCV RNA viral load tests and genotyping. Patients, who presented with HCV-positive RNA, despite their knowledge of the disease and previous treatment, were referred for clinical treatment.
Genotype results
Among the HCV genotypes from the 69 patients, genotype 1 (1a and 1b) was the most prevalent genotype (52 patients, 75%), followed by genotype 3 (11 patients, 16%) and genotype 2 (6 patients, 9%).
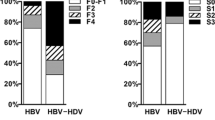
Liver fibrosis grade and disease severity
A total of 65 patients (94.2%) with HCV-positive RNA tests were referred for TE to determine liver fibrosis grade and disease severity. Among them, 30 (30/65 = 46.2%) showed advanced fibrosis (F3 and F4), 12 (12/65 = 18.5%) showed significant fibrosis (F2), and 22 (22/65 = 33.8%) showed mild fibrosis (F0 and F1). In one patient (1.5%), the LSM by TE was not successful.
As illustrated in Fig. 3, individuals aged > 70 years showed a higher prevalence of significant fibrosis (>F2) than those aged between 40 and 59 years.
To explore the relationship between genotype and severity of the liver disease, we analyzed the CAP and LSM values using FibroScan® according to genotype, as shown in Table 2. Because the genotype 2 categories consisted of only two patients, it was excluded from the analysis. Results of the t-test to compare genotype 1 with genotype 3 showed no significant difference. The distribution of patients with advanced fibrosis (F3 and F4) among all genotypes observed, also showed no statistically significant difference (p = 0.86), as shown in Table 3.
Discussion
This present study showed an estimated HCV prevalence of 0.27% among patients aged > 40 years, which is considered the risk group for HCV infection. This result displays a lower prevalence than was previously described by other studies in Brazil, which was between 0.69–1.89% [6, 13, 14]. In the Federal District, Pereira et all demonstrated an HCV seroprevalence of 1.09% in 1008 individuals aged 20–69 years [13]. A mathematical modeling approach published in 2018 estimated that 700,000 people were chronically infected with HCV in Brazil and that the current prevalence of positive anti-HCV serology in the Brazilian population is 0.71%, as estimated by the Brazilian Ministry of Health [18]. The reduced prevalence of HCV infection in our study could have resulted from selecting individuals aged over 40 years. Notwithstanding, this interpretation is unlikely because previous studies conducted in Brazil have shown a higher prevalence in the adult population over 40 years [6, 13]. Pereira et al observed a prevalence of 0,75% in individuals between 10 and 19 years, 1,36% in 20–39 year, 1,55% in 40–59 years and 3,41% in those with 60–69 years [13]. Also, it is postulated that 76% of HCV chronic infection in Brazil occurs in adults born between 1950 and 1980 [6]. It is conceivable that the selection criteria can explain this difference. This study was not primarily designed to estimate the prevalence of HCV infection in the Federal District.
It is estimated that 71 million people are infected with HCV worldwide, and this infection is a leading cause of cirrhosis; hepatocellular carcinoma; and liver transplantation [27,28,29]. According to the Brazilian Ministry of Health, an estimated 700,000 individuals are chronically infected with HCV in Brazil [11, 18]. Most of these individuals would be aged > 40 years because previous studies demonstrated that to eliminate HCV according to WHO targets, the screening of HCV infection and the cascade of care should focus on patients born between 1958 and 1978 [30]. Furthermore, since HCV infection is curable, the progression rate of this disease is expected to expand significantly in the next 15 years, causing not only an increase in cirrhosis and liver cancer cases but also an increase in treatment costs [7]. To address this challenge, it is necessary to increase the rate of diagnosis and treatment in most countries [8].
Currently, a minority of HCV patients are diagnosed or are aware that they are infected with HCV and may inadvertently transmit the infection to other individuals [28, 29, 31]. Moreover, only 5–16% of chronic hepatitis C cases have been treated [32, 33]. According to the WHO, HCV infection elimination shall reduce new infections by 90% and diminish mortality by 65% until 2030 [28, 29].
This goal can be achieved by improving the diagnosis and efficiency of the cascade of care of hepatitis C patients [34]. Our study showed enormous gaps in the cascade of care of these patients, starting with the difficulty of patient access to medical care and finally with a low number of patients treated. Recent studies have also shown several gaps in the cascade of care for chronic HCV infection, including low diagnostic rate, difficulty in access to care for recently diagnosed patients, high cost of tests (such as the HCV RNA test), and low rate of treatment [32]. In the USA, a recent systematic review and meta-analysis to identify gaps in the care of HCV-positive patients showed that only 50% of all HCV-positive patients had been diagnosed. Additionally, only 43% of them had access to outpatient care, and 27% had HCV RNA confirmed. Moreover, only 16% received treatment, and 9% achieved SVR [32]. Similar results were also observed in European Union countries, where only 34% of infected individuals were diagnosed with chronic hepatitis C, and only 5% of all HCV cases were treated [23].
The exact reason for the lower HCV prevalence in this present study is unknown. However, the improvement in the cascade of care by the Brazilian healthcare system might have contributed to the diminishing HCV infection rate in the last 10 years. Another potential bias could be the experimental design of this study because blood samples were collected in a laboratory where most of the patients had private health insurance. Nevertheless, this study investigated a large-scale general population of 57,697 patients in the Federal District, including those regions with lower income per capita.
In Brazil, a cross-sectional retrospective study of HCV-infected blood donors showed that about 40% of them did not have access to a specialist and treatment, suggesting the need for improved access to medical care [35]. To the best of our knowledge, there has been no published research evaluating the cascade of care for patients aged > 40 years who have positive anti-HCV serology in Brazil, making this present study the first to demonstrate such an assessment of care. Our results were disappointed in the follow-up of HCV-positive patients since only 22.3% of them achieving SVR. Besides that, it is interesting to notice that the 16 patients were awaiting treatment at the end of the study. Since they were enrolled, three to 4 months after the end of the protocol, the medicines were dispensed to them. Despite these gaps, similar or even worse results were observed in other studies. A systematic review that examined the treatment cascade of patients with chronic hepatitis C in the USA identified several gaps that resulted in an SVR rate of only 5–6% [32]. In another study on the continuum of care of patients with HCV infection conducted in Philadelphia—which included HCV testing for homeless people and residents of public housing aged > 40 years—Coyle et al. performed HCV RNA tests using PCR in 89% of patients and 62.5% of them were examined by a hepatology specialist [33]. Furthermore, only 6.4% of their patients initiated anti-HCV treatment. However, they did not describe how many patients achieved SVR [33]. In our study, 92.3% of treated patients achieved SVR, and a high SVR rate was also recently noted in another study that evaluated the cascade of care for hepatitis C in this era of DAAs [36].
TE and other forms of fibrosis measurement replaced liver biopsy for the assessment of the degree of fibrosis, for a better selection of and patient referral for treatment and follow-up, as well as for early identification of HCC [24]. Of HCV-positive patients in this study almost half of them (30 patients, 46.2%) showed advanced fibrosis. A recent Brazilian study demonstrated that among 2000 HCV-infected patients in Brazil, 31.3% had cirrhosis, of which 29.1% of cases were F0/F1, 19.1% were F2, and 18.6% were F3. Most of them were evaluated by liver biopsy (61.5%), followed by liver elastography (24.5%) and clinical diagnosis of cirrhosis (13.9%) [37, 38]. Another Brazilian study reported that hepatic fibrosis increased with advancing age [37].
The most common genotypes in the present study were genotypes 1 (1a and 1b), 3, and 2, similar to those reported in several previous studies in Brazil, including a multicenter evaluation [13, 38,39,40,41].
This study has some limitations. First, the general representativeness of the population of the Federal District was limited because this study was not designed to estimate the prevalence of HCV infection in the Federal District and, the study was conducted in the 106 units of the biggest private laboratory in the Federal District. However, this is the most extensive screening test program that has been executed in all regions of the Federal District, including those with a lower income per capita. Second, as patients were referred to a single central hepatology service, among several others, in the Federal District, the loss to follow-up may also not reflect the overall existing losses in all regions of the Federal District. Third, selection criteria, recruiting only patients aged over 40 years, although being the most prevalent age group of infection, may result in a lower prevalence of infection in this study compared to other Brazilian studies. It is also important to remember that the Centers for Disease Control and Prevention (CDC) recommends that adult HCV screening should focus on individuals belonging to the birth cohort between 1945 and 1965 because studies have shown that two-thirds of HCV-infected individuals in the US belong to this age group. Fourth, there are other available Hep C screening tests, including the detection of hepatitis C virus RNA in saliva samples, although we have not yet available these tests for free population screening in Brazil.
According to the WHO, to eliminate global HCV infection by 2030, it is essential to develop new strategies to improve the rate of diagnosis and enhance treatment [28]. To achieve this target, 90% of people with chronic hepatitis C need to be diagnosed and 80% of them must be treated [29]. Moreover, such target can be achieved through the use of RTs for HCV infection screening [22, 28]. Meanwhile, the gaps identified in the cascade of care of patients in this study suggest the urgent need to develop an effective strategy for the screening, diagnosis, and treatment of HCV infection, which is aimed at eliminating the disease and reducing related mortality.
The lower prevalence observed in this study demonstrates that not only is the disease less common than initially thought, but it is also a challenge to identify patients with such viral infection. Our screening approach using anti-HCV RTs conducted at laboratories was feasible and can be implemented in collaboration with private and public laboratories. Because the blood sample collection was performed independent of RT requests and the RTs were carried out using a serum that was collected for other laboratory blood tests, the cost of this screening approach consisted only of the cost of the RT and the cost of performing the test. Trained health professionals can perform the test. This simple procedure can enhance the diagnosis of new cases of chronic hepatitis C, thereby supporting the global efforts of the WHO to eliminate hepatitis C by 2030. Furthermore, determining the HCV prevalence and the quality of the cascade of care provided new trends for the healthcare system to propose new strategies for patients with hepatitis C, including the acquisition of both RTs and drugs for HCV infection treatment.
Conclusions
Our results revealed, in this sample, the lower prevalence of HCV than the others identified in previous studies and the similarity gaps in the cascade of care of patients with chronic HCV infection in Brazil to those of other developed countries, which is significantly below the targets of hepatitis C elimination. Our results also suggest that establishing partnerships with clinical laboratories to conduct rapid anti-HCV tests to detect and monitor disease is a cost-effective and feasible strategy that can be used to improve HCV diagnosis.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ABPH:
-
Brazilian Association of Hepatitis Carriers
- CAP:
-
controlled attenuation parameter
- DAA:
-
direct antiviral agent
- HCC:
-
hepatocellular carcinoma
- HCV:
-
hepatitis C vírus
- IBGE:
-
Brazilian Institute of Geography and Statistics
- IHBDF:
-
Base Hospital Institute of the Federal District
- LSM:
-
liver stiffness measurement
- PCR:
-
polymerase chain reaction
- RT:
-
rapid test
- SVR:
-
sustained virologic response
- TE:
-
transient elastography
- WHO:
-
World Health Organization
References
Wedemeyer H, Dore GJ, Ward JW. Estimates on HCV disease burden worldwide - filling the gaps. J Viral Hepat. 2015;22(Suppl 1):1–5.
Pawlotsky JM, Negro F, Aghemo A, et al. EASL recommendations on treatment of hepatitis C 2018. J Hepatol. 2018;69:461–511.
Babiker A, Jeudy J, Kligerman S, Khambaty M, Shah A, Bagchi S. Risk of cardiovascular disease due to chronic hepatitis C infection: areview. J Clin Transl Hepatol. 2017;5:343–62.
Cooke GS, Andrieux-Meyer I, Applegate TL, et al. Accelerating the elimination of viral hepatitis: a Lancet Gastroenterology & Hepatology Commission. Lancet Gastroenterol Hepatol. 2019;4:135–84.
WHO. Hepatitis C. 2017. http://www.who.int/mediacentre/factsheets/fs164/en/. Accessed 1 Feb 2003.
Wedemeyer H, Duberg AS, Buti M, et al. Strategies to manage hepatitis C virus (HCV) disease burden. J Viral Hepat. 2014;21(Suppl 1):60–89.
Razavi H, Waked I, Sarrazin C, et al. The present and future disease burden of hepatitis C virus (HCV) infection with today’s treatment paradigm. J Viral Hepat. 2014;21(Suppl 1):34–59.
Hagan LM, Schinazi RF. Best strategies for global HCV eradication. Liver Int. 2013;33:68–79.
Allison RD, Tong X, Moorman AC, et al. Increased incidence of cancer and cancer-related mortality among persons with chronic hepatitis C infection, 2006-2010. J Hepatol. 2015;63:822–8.
Millman AJ, Nelson NP, Vellozzi C. Hepatitis C: review of the epidemiology, clinical care, and continued challenges in the direct acting antiviral era. Curr Epidemiol Rep. 2017;4:174–85.
Kershenobich D, Razavi HA, Sánchez-Avila JF, et al. Trends and projections of hepatitis C virus epidemiology in Latin America. Liver Int. 2011;31(Suppl 2):18–29.
Mesquita F, Santos ME, Benzaken A, et al. The Brazilian comprehensive response to hepatitis C: from strategic thinking to access to interferon-free therapy. BMC Public Health. 2016;16:1132.
Pereira LM, Martelli CM, Moreira RC, et al. Prevalence and risk factors of hepatitis C virus infection in Brazil, 2005 through 2009: a cross-sectional study. BMC Infect Dis. 2013;13:60.
Bruggmann P, Berg T, Øvrehus AL, et al. Historical epidemiology of hepatitis C virus (HCV) in selected countries. J Viral Hepat. 2014;21(Suppl 1):5–33.
Kim MH, Kang SY, Lee WI. Evaluation of a new rapid test kit to detect hepatitis C virus infection. J Virol Methods. 2013;193:379–82.
Centers for Disease Control and Prevention (CDC). Testing for HCV infection: an update of guidance for clinicians and laboratorians. MMWR Morb Mortal Wkly Rep. 2013;62:362–5.
Zachary P, Ullmann M, Djeddi S, et al. Evaluation of three commercially available hepatitis C virus antibody detection assays under the conditions of a clinical virology laboratory. J Clin Virol. 2005;34:207–10.
Benzaken A, Catapan E, Girade R, et al. Hepatitis C elimination by 2030 is feasible in Brazil: a mathematical modelling approach. J Hepatol. 2018;68:S193.
Greenaway C, Makarenko I, Chakra CNA, et al. The effectiveness and cost-effectiveness of hepatitis c screening for migrants in the EU/EEA: a systematic review. Int J Environ Res Public Health. 2018;15:E2013.
Moore MS, Bocour A, Laraque F, Winters A. A surveillance-based hepatitis C care cascade, New York City, 2017. Public Health Rep. 2018;133:497–501.
Martínez JD, Garzón MA, Arteaga JM, et al. The SD BIOLINE rapid test for detection of antibodies to HCV among high-risk patients. Rev Colomb Gastroenterol. 2015;30:271–5.
Ivantes CAP, Silva D, Messias-Reason I. High prevalence of hepatitis C associated with familial history of hepatitis in a small town of South Brazil: efficiency of the rapid test for epidemiological survey. Braz J Infect Dis. 2010;14:483–8.
Shivkumar S, Peeling R, Jafari Y, Joseph L, Pant Pai N. Accuracy of rapid and point-of-care screening tests for hepatitis C: a systematic review and meta-analysis. Ann Intern Med. 2012;157:558–66.
Wong GL. Transient elastography: kill two birds with one stone? World J Hepatol. 2013;5:264–74.
Castéra L, Le Bail B, Roudot-Thoraval F, et al. Early detection in routine clinical practice of cirrhosis and oesophageal varices in chronic hepatitis C: comparison of transient elastography (FibroScan) with standard laboratory tests and non-invasive scores. J Hepatol. 2009;50:59–68.
Liu K, Wong VW, Lau K, et al. Prognostic value of controlled attenuation parameter by transient elastography. Am J Gastroenterol. 2017;112:1812–23.
Ferreira PRA. Brandão-Mello, et al. disease burden of chronic hepatitis C in Brazil. Braz J Infect Dis. 2015;19(4):363–8.
World Health Organization. Global hepatitis report, 2017. http://apps.who.int/iris/bitstream/handle/10665/255016/9789241565455-eng.pdf?sequence=1. Accessed 24 May 2018.
Thomas DL. Global elimination of chronic hepatitis. N Engl J Med. 2019;380:2041–50.
Kondili LA, Robbins S, Blach S, et al. Forecasting hepatitis C liver disease burden on real-life data. Does the hidden iceberg matter to reach the elimination goals? Liver Int. 2018;38:2190–8.
Mohamoud YA, Mumtaz GR, Riome S, Miller D, Abu-Raddad LJ. The epidemiology of hepatitis C virus in Egypt: a systematic review and data synthesis. BMC Infect Dis. 2013;13:288.
Yehia BR, Schranz AJ, Umscheid CA, Lo Re V 3rd. The treatment cascade for chronic hepatitis C virus infection in the United States: asystematic review andmeta-analysis. PLoS One. 2014;9:e101554.
Coyle C, Viner K, Hughes E, et al. Identification and linkage to care of HCV-infected persons in five health centers — Philadelphia, Pennsylvania, 2012-2014. MMWR Morb Mortal Wkly Rep. 2015;64:459–63.
World Health Organization. Global health sector strategy on viral hepatitis 2016–2021: towards ending viral hepatitis. 2016. http://apps.who.int/iris/bitstream/handle/10665/246177/WHO-HIV-2016.06-eng.pdf;jsessionid=2CFF0CFCC4FEAFB99EF989500F4F179D?sequence=1. Accessed 24 May 2018.
Machado SM, de Almeida NC, Pinho JRR, et al. Hepatitis C among blood donors: cascade of care and predictors of loss to follow-up. Rev Saude Publica. 2017;51:40.
Zuckerman A, Douglas A, Nwosu S, Choi L, Chastain C. Increasing success and evolving barriers in the hepatitis C cascade of care during the direct acting antiviral era. PLoS One. 2018;13:e0199174.
Oliveira AC, Bortotti AC, Nunes NN, El Bacha IA, Parise ER. Association between age at diagnosis and degree of liver injury in hepatitis C. Braz J Infect Dis. 2014;18:507–11.
Portari-Filho LH, Álvares-da-Silva MR, Gonzalez A, et al. How are HCV-infected patients being identified in Brazil: a multicenter study. Braz J Infect Dis. 2019;23:34–9.
Gonzaga RMS, Rodart IF, Reis MG, Ramalho Neto CE, Silva DW. Distribution of hepatitis C virus (HCV) genotypes in seropositive patients in the state of Alagoas, Brazil. Braz J Microbiol. 2008;39:644–7.
Vieira DS, Alvarado-Mora MV, Botelho L, Carrilho FJ, Pinho JR, Salcedo JM. Distribution of hepatitis c virus (HCV) genotypes in patients with chronic infection from Rondônia, Brazil. Virol J. 2011;8:165.
Gower E, Estes C, Blach S, Razavi-Shearer K, Razavi H. Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol. 2014;61(Suppl 1):S45–57.
Acknowledgements
The authors would like to thank the participants of this study, the Brazilian Association of Hepatitis Carriers (ABPH) and the Sabin Laboratory.
Funding
The Brazilian Association of Hepatitis Carriers (ABPH) donated the rapid tests used in this study. Sabin Laboratory provided the conditions to take the blood samples and perform the rapid anti-HCV tests. FARN is supported by a fellowship from the Brazilian Research Council (Conselho Nacional de Desenvolvimento Científico e Tecnológico – CNPq -grant number CNPq 309989/2014–0).
Author information
Authors and Affiliations
Contributions
DMCL – Conceptualization, data curation: investigation methodology validation Writing - original draft: writing-review & editing. EBS - Supervision writing-review & editing validation. JET - Writing-review & editing validation. TMGM - Writing-review & editing investigation methodology validation. ALRC - Writing-review & editing validation. MPR - Methodology formal analysis writing-review & editing. ACLCF - Writing-review & editing validation. BTAS - Writing-review & editing validation. FARN - Methodology supervision writing-review & editing validation. All authors read and approved the final manuscript.
Authors’ information
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All the subjects provided written informed consent before participating in the study, and the study design was approved by the Research Ethics Committee of the Faculty of Health Sciences of the University of Brasilia and the Ethics Committee of the Health Science Teaching and Research Foundation.
Consent for publication
Not applicable.
Competing interests
Alexandre Cunha has been on the Advisory board for Biofire/Biomerieux and is a regular consultant for Sabin Clinical Lab. Eric Bassetti Soares is an employee of Gilead Sciences.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Carvalho-Louro, D.M., Soares, E.B., Trevizoli, J.E. et al. Hepatitis C screening, diagnosis, and cascade of care among people aged > 40 years in Brasilia, Brazil. BMC Infect Dis 20, 114 (2020). https://doi.org/10.1186/s12879-020-4809-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-020-4809-2