Abstract
Background
Difficult-to-treat infections caused by rapidly growing mycobacteria (RGM) are increasingly observed in clinical settings. However, studies on antimicrobial susceptibilities and effective treatments against RGM in Japan are limited.
Methods
We conducted susceptibility testing of potential antimicrobial agents, including tigecycline and tebipenem, against RGM. Clinical RGM isolates were collected from a university hospital in Japan between December 2010 and August 2013. They were identified using matrix-assisted laser desorption/ionization time-of-flight mass spectrometry and the sequencing of 16S rRNA, rpoB, and hsp65 genes. The samples were utilized for susceptibility testing using 16 antimicrobials, with frozen broth microdilution panels.
Results
Forty-two isolates were obtained: 13, Mycobacterium abscessus complex; 12, Mycobacterium chelonae; 9, Mycobacterium fortuitum; and 8, M. fortuitum group species other than M. fortuitum. Different antimicrobial susceptibility patterns were observed between RGM species. Clarithromycin-susceptible strain rates were determined to be 0, 62, and 100% for M. fortuitum, M. abscessus complex, and M. chelonae, respectively. M. abscessus complex (100%) and >80% M. chelonae isolates were non-susceptible, while 100% M. fortuitum group isolates were susceptible to moxifloxacin. Linezolid showed good activity against 77% M. abscessus complex, 89% M. fortuitum, and 100% M. chelonae isolates. Regardless of species, all tested isolates were inhibited by tigecycline at very low minimal inhibitory concentrations (MICs) of ≤0.5 μg/mL. MICs of tebipenem, an oral carbapenem, were ≤4 μg/mL against all M. fortuitum group isolates.
Conclusions
Our study demonstrates the importance of correct identification and antimicrobial susceptibility testing, including the testing of potential new agents, in the management of RGM infections.
Similar content being viewed by others
Background
Rapidly growing mycobacteria (RGM) can cause various diseases in humans, including lung, skin and soft tissue, bone, and catheter-related blood stream infections, as well as disseminated infections. Mycobacterium abscessus complex, Mycobacterium chelonae, and Mycobacterium fortuitum complex are the most commonly encountered RGM strains clinically. Different strains belonging to the M. fortuitum group and Mycobacterium smegmatis and Mycobacterium mucogenicum group strains, which can cause human infections, account for <10% of rapidly growing mycobacterial infections [1, 2].
Recently, M. abscessus complex was divided into three subspecies, M. abscessus subsp. abscessus, M. abscessus subsp. bolletii, and M. abscessus subsp. massiliense, based on the multiple sequencing analyses of 16S rRNA and several housekeeping genes, such as rpoB, hsp65, secA, and sodA. M. abscessus subsp. abscessus and M. abscessus subsp. bolletii usually possess an inducible macrolide resistant gene, unlike M. abscessus subsp. massiliense [3]. M. fortuitum group comprises of more than 10 species, including M. fortuitum, Mycobacterium peregrinum, Mycobacterium senegalense, Mycobacterium septicum, Mycobacterium alvei, Mycobacterium houstonense, Mycobacterium boenickei, Mycobacterium conceptionense, Mycobacterium porcinum, Mycobacterium neworleansense, Mycobacterium brisbanense, and Mycobacterium mageritense, although some controversy about the classification of M. mageritense still exists [4, 5].
Difficult-to-treat infections caused by RGM are increasingly observed in clinical settings, especially by M. abscessus complex, which is considered one of the most resistant strains [3]. Additionally, inducible macrolide resistance, a recently recognized phenomenon, may restrict the therapeutic role of macrolides. This resistance may be related to the insufficient efficacy of clarithromycin-based treatment of M. abscessus subsp. abscessus infection, even when a particular isolate is initially shown to be sensitive to the drug [6, 7]. To date, only a small amount of data is available on antimicrobial susceptibilities of RGM isolated in Japan. Susceptibility of RGM to some antimicrobials can be tested in a limited number of reference laboratories, while an accurate identification of RGM at the species level is difficult for most of the clinical laboratories, resulting in limited susceptibility data as well.
The development of novel treatment options is necessary since the effective antimicrobial treatment options against RGM, in particular against M. abscessus subsp. abscessus, are limited [3]. Oral medications need to be investigated in addition to parenteral agents, since the long-term antimicrobial treatments are often required. Tigecycline, the first clinically available glycylcycline, has broad activity against multidrug-resistant bacteria, due to its low sensitivity to major mechanisms of tetracycline resistance [8]. Minimal inhibitory concentrations (MICs) of this drug were shown to be low against rapidly growing mycobacterial isolates tested throughout the world [9–14]. Tebipenem, a novel oral carbapenem that is approved for use in Japan, was recently showed to have potent in vitro activity against Mycobacterium tuberculosis [15], although the data are still not complete.
The purpose of this study was to examine the susceptibilities of RGM clinical isolates collected in Japan to 16 antimicrobial agents, including potential new agents, such as tigecycline and tebipenem. We placed particular emphasis on the correct identification of isolates at the species level, prior to the drug susceptibility testing.
Methods
Bacterial identification
Between December 2010 and August 2013, 71 strains of RGM were isolated from various clinical samples at the University of Tokyo Hospital, Japan. We identified these strains using matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) and the sequencing of three conserved genes (16S rRNA, rpoB, and hsp65). The MALDI Biotyper system and the Mycobacterium Library 1.0 database (Bruker Daltonics K.K., Kanagawa, Japan) were used for MALDI-TOF MS analyses.
Antimicrobial susceptibility testing
Susceptibility testing was performed according to Clinical and Laboratory Standards Institute (CLSI) guidelines M24-A2 [16], using frozen broth microdilution panels. The final drug concentration ranges were as follows: 4 to 128 μg/mL of amikacin, 1 to 16 μg/mL of tobramycin, 0.12 to 16 μg/mL of tigecycline, 0.25 to 16 μg/mL of minocycline, 0.25 to 8 μg/mL of ciprofloxacin, 0.25 to 8 μg/mL of moxifloxacin, 0.25 to 32 μg/mL of clarithromycin, 1 to 16 μg/mL of azithromycin, 2 to 64 μg/mL of linezolid, 1 to 64 μg/mL of imipenem, 1 to 64 μg/mL of meropenem, 0.25 to 2 μg/mL of faropenem, 0.5 to 4 μg/mL of tebipenem, 4 to 128 μg/mL of cefmetazole, 2 to 64 μg/mL of cefepime, and 1/19 to 8/152 μg/mL of trimethoprim/sulfamethoxazole. Tigecycline was purchased from Selleckchem (Houston, TX, USA). Frozen broth microdilution panels containing antimicrobial agents in 100 μL of cation-supplemented Muellar-Hinton broth were custom-fabricated by Eiken Chemical Co., Ltd. (Tokyo, Japan). According to the CLSI guidelines [16], the inoculum was prepared so that the final concentrations were 1 × 105 to 5 × 105 CFU/mL. Strains were incubated at 37 °C. If microbial growth in the control sample was sufficient, MICs were measured at day 3. Otherwise, the incubation period was prolonged, and MICs were measured at day 4 or 5. For clarithromycin, MIC measurements were performed at day 3 and day 14 to detect inducible macrolide resistance. In this study, clarithromycin MICs were determined at day 14 of incubation. M. fortuitum ATCC 6841 was used as a quality control reference strain.
The MIC breakpoints, indicating susceptible, intermediate, and resistant strains, were interpreted according to the CLSI criteria for amikacin, tobramycin, minocycline, ciprofloxacin, moxifloxacin, clarithromycin, linezolid, imipenem, meropenem, and trimethoprim/sulfamethoxazole [16]. To date, there are no consensus breakpoints for tigecycline, azithromycin, faropenem, tebipenem, cefmetazole, and cefepime. Because of this, a modified susceptibility breakpoint of ≤4 μg/mL for tigecycline proposed by Petrini [17] was used in this study (Table 1).
Results
Bacterial isolates and species identification
Among the investigated strains, 46 were identified as M. abscessus complex, M. chelonae, and M. fortuitum group (including M. fortuitum, M. mageritense, M. peregrinum, M. porcinum, and M. septicum). Despite the sequencing of housekeeping genes (rpoB and hsp65) and the use of MALDI-TOF MS, we were unable to distinguish between M. abscessus subsp. abscessus and M. abscessus subsp. bolletii correctly. Therefore, we have described isolates belonging to M. abscessus species as M. abscessus complex. Of these three clinically important species/groups of RGM (46 isolates), four isolates were excluded: we were not able to cultivate three of them for susceptibility testing and the results of MALDI-TOF MS and gene sequencing were disparate for one isolate. Therefore, we included a total of 42 isolates in this study. They were collected from sputum/respiratory specimens (n = 35), wounds (n = 3), blood (n = 1), ascites (n = 1), lymph node aspirate (n = 1), and ocular discharge sample (n = 1).
Among the 42 isolates included in this study, 13 isolates were identified as M. abscessus complex, 12 as M. chelonae, nine as M. fortuitum, four as M. mageritense, two as M. peregrinum, one as M. porcinum, and one as M. septicum.
Antimicrobial susceptibility
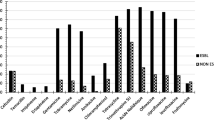
In this study, sufficient microbial growth in the growth control samples was observed after 72 h of incubation. The results of the susceptibility testing (MIC range, MIC50, MIC90, and percentage of susceptibility) to 16 antimicrobial agents are presented in Table 2. All isolates (n = 42) were highly susceptible to tigecycline, with MIC50 values of ≤0.12 μg/mL, MIC90 value of 0.25 μg/mL, and MIC range of ≤0.12–0.5 μg/mL.
Antimicrobial susceptibility patterns of RGM
M. abscessus complex
All isolates belonging to M. abscessus complex (n = 13) were susceptible to amikacin. However, they were all resistant to tobramycin and trimethoprim-sulfamethoxazole and not susceptible to fluoroquinolones (both moxifloxacin and ciprofloxacin). Seventy percent of the isolates and none of them were susceptible to imipenem and meropenem, respectively. Around two-thirds of the isolates were susceptible to clarithromycin and linezolid (Table 2).
M. chelonae
Among M. chelonae strains (n = 12), all isolates were susceptible to clarithromycin and linezolid, azithromycin MICs were shown to be ≤2 μg/mL for all isolates. The majority of M. chelonae isolates were susceptible to aminoglycosides: 83% were susceptible to tobramycin, used predominantly in the treatment of M. chelonae infections [16]. All M. chelonae isolates were resistant to minocycline, while they were susceptible to another tetracycline derivative, tigecycline. Susceptibility to different carbapenems was diverse, with 58% of isolates susceptible to imipenem and only 8% susceptible to meropenem (Table 2).
M. fortuitum
Similar to M. abscessus complex, among M. fortuitum strains (n = 9), all isolates were susceptible to amikacin and resistant to tobramycin. Many antimicrobial agents showed activity or had low MICs in vitro against M. fortuitum. All M. fortuitum isolates were susceptible to fluoroquinolones (ciprofloxacin and moxifloxacin), and around two-thirds of isolates were susceptible to imipenem and meropenem. Furthermore, the MIC90 values of tebipenem and cefmetazole against M. fortuitum isolates were lower compared with the values against M. abscessus complex and M. chelonae. All isolates were found to be susceptible to tigecycline, although 44% were resistant to minocycline. However, all M. fortuitum isolates were not susceptible to clarithromycin and had high MICs (>16 μg/mL) to azithromycin (Table 2).
Other M. fortuitum group
Other M. fortuitum group isolates, M. mageritense (n = 4), M. peregrinum (n = 2), M. porcinum (n = 1), and M. septicum (n = 1), generally had good sensitivity to fluoroquinolones, carbapenems (including tebipenem), cefmetazole, and linezolid; however, only a small number of these strains had been included in this study. Additionally, similar to M. fortuitum, all these isolates, except M. peregrinum, showed poor sensitivity to clarithromycin. M. fortuitum group isolates were not susceptible to minocycline, while they all were susceptible to tigecycline (Table 2).
Discussion
In this study, conducted in Japan, antimicrobial susceptibility patterns of different species of RGM were found to vary. However, rapidly growing mycobacterial strains, regardless of species, showed good sensitivity to tigecycline. Although a susceptibility breakpoint of ≤4 μg/mL was used for tigecycline [17] in this study, the growth of all isolates was inhibited by tigecycline at very low MICs, that is, ≤0.5 μg/mL. To date, most of the RGM worldwide remain sensitive to tigecycline in vitro. The MIC values of tigecycline against a total of 122 rapidly growing mycobacterial isolates (including 50 tetracycline-resistant isolates) collected in USA [9], 40 isolates obtained in Taiwan [10], 25 isolates collected in Turkey [11], 160 isolates in Taiwan [12], and 57 isolates obtained in Korea [13] were ≤4 μg/mL. The MIC ranges in the first four studies were reported to be ≤0.06–1 μg/mL, 0.064–2 μg/mL, 0.12–1 μg/mL, and 0.0625–4 μg/mL, respectively; the MIC range was not reported in the Korean study. However, in a recent study conducted in China, it was shown that tigecycline MIC values against two or three of 73 RGM isolates were somewhat high, with an MIC of 8 μg/mL [14].
It was previously reported that tigecycline may have a promising role in the treatment of multi-drug resistant RGM infections, not only in vitro but also in vivo. A study following 52 patients with M. abscessus and M. chelonae infections, where prior therapy attempts had failed, showed that tigecycline-containing regimens administered for ≥1 month resulted in clinical improvement in more than 60% of the patients [18]. However, both CLSI and European Committee on Antimicrobial Susceptibility Testing (EUCAST) have not defined tigecycline MIC breakpoints for RGM yet. Additionally, tigecycline has not been approved for the treatment of mycobacterial infections, demonstrating a need for further clinical studies and appropriate approvals, in order to develop new treatment options.
Macrolides are one of the most important drugs used for the treatment of RGM. However, we observed that a relatively large number of isolates showed resistance to macrolides, with important differences in susceptibility patterns among species; the obtained rates of clarithromycin-susceptible strains were 0, 62, and 100% of M. fortuitum, M. abscessus complex, and M. chelonae, respectively. Additionally, M. mageritense strain, which comprises 10% of all isolates in this study, shows intrinsic resistance to macrolides [2]. Inducible resistance to macrolides can occur during the application of macrolide-containing regimen during the treatment of infections caused by several RGM species. The erythromycin ribosome methyltransferase genes, erm(38) and erm(41), have been reported to confer inducible macrolide resistance to M. fortuitum and M. abscessus subsp. abscessus, respectively [6, 19], while erm(41) is absent from M. chelonae [6]. Inducible resistance may be at least partially responsible for the difficulties observed during the treatment of M. abscessus infections [20].
Previously, approximately 80% of M. fortuitum samples were shown to be susceptible to clarithromycin [19], which was not observed in this study. In a study conducted in Spain, of 89 M. fortuitum clinical isolates, 75 (84.3%) were shown to harbor the erm gene, while 42 (47.2%) were not susceptible to clarithromycin [21]. Regional differences in clarithromycin susceptibility and the prevalence of erm gene in the clinical isolates of M. fortuitum may exist. Further studies investigating this issue are necessary.
Azithromycin susceptibility breakpoint is not defined by the CLSI and EUCAST, and CLSI lists clarithromycin as a class representative of a new generation of macrolides, which includes azithromycin, for the RGM susceptibility testing [16]. However, to date, no conclusive results about the equivalence of the clinical effects of clarithromycin and azithromycin therapies in the patients with M. abscessus infections were obtained. In the experimental models of M. abscessus subsp. abscessus and M. abscessus subsp. massiliense infections, clarithromycin induced erm(41) expression, leading to a higher induction of macrolide resistance compared with the effects of azithromycin on M. abscessus subsp. abscessus. As a result, clarithromycin was shown to have a lower effect against M. abscessus subsp. abscessus in vitro and in vivo compared with azithromycin, while both of these macrolides showed comparable effects against M. abscessus subsp. massiliense infections [7]. In order to ensure the efficient treatment using macrolides, a correct identification of subspecies of M. abscessus complex (including M. abscessus subsp. abscessus and M. abscessus subsp. massiliense) is clinically important, although we have not performed this identification, as it is technically cumbersome.
Carbapenem is one of the available treatment options for RGM infections. Imipenem was demonstrated to be more efficient against M. abscessus complex, M. chelonae, and M. fortuitum than meropenem in this study. In Japan, faropenem (an oral penem) and tebipenem (an oral carbapenem) are approved for clinical use. Tebipenem MIC values were shown to be ≤4 μg/mL against all isolates belonging to M. fortuitum group (including M. fortuitum, M. mageritense, M. peregrinum, M. porcinum, and M. septicum) in this study, while the MICs of this compound against the majority of M. abscessus complex and M. chelonae isolates were >4 μg/mL (Table 2). Since concentrations higher than 4 μg/mL are achievable in human serum at therapeutic doses [15], tebipenem may represent an orally available drug of choice for the treatment of infections caused by M. fortuitum group strains. Further clinical studies are necessary to evaluate these new agents against difficult-to-treat RGM infections.
Many RGM strains, with the exception of M. mageritense, showed sensitivity to amikacin. Tobramycin was active only against M. chelonae and M. septicum. CLSI discourages clinical use of tobramycin for the treatment of infections caused by M. abscessus or M. fortuitum group. As the information on M. mageritense susceptibility to amikacin remains limited, it should be further investigated.
In this study, we used M. fortuitum ATCC 6841 as a control strain, which represents one of the potential limitations of this study, as the current CLSI-recommended quality control strain is M. peregrinum ATCC 700686.
Conclusions
We performed susceptibility testing of 16 antimicrobial agents against 42 isolates of M. abscessus complex, M. chelonae, and M. fortuitum group collected in Japan, which were correctly identified using MALDI-TOF MS and 16S rRNA, rpoB, and hsp65 gene sequencing. Tigecycline was able to inhibit the growth of all tested isolates at very low MICs of ≤0.5 μg/mL, regardless of species and tetracycline resistance. Tebipenem showed MIC values of ≤4 μg/mL against all isolates of M. fortuitum group. We have showed that the patterns of antimicrobial susceptibility clearly differ among RGM species, and that the correct identification of RGM species (and even subspecies) and antimicrobial susceptibility testing, including the identification of novel agents, are important for the treatment of RGM infections.
Abbreviations
- RGM:
-
Rapidly growing mycobacteria
- MICs:
-
Minimal inhibitory concentrations
- MALDI-TOF MS:
-
Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry
- CLSI:
-
Clinical and Laboratory Standards Institute
- EUCAST:
-
European Committee on Antimicrobial Susceptibility Testing
References
De Groote MA, Huitt G. Infections due to rapidly growing mycobacteria. Clin Infect Dis. 2006;42(12):1756–63.
Nash KA, Andini N, Zhang Y, Brown-Elliott BA, Wallace Jr RJ. Intrinsic macrolide resistance in rapidly growing mycobacteria. Antimicrob Agents Chemother. 2006;50(10):3476–8.
Howard ST. Recent progress towards understanding genetic variation in the Mycobacterium abscessus complex. Tuberculosis. 2013;93(Suppl):S15–20.
Lamy B, Marchandin H, Hamitouche K, Laurent F. Mycobacterium setense sp. nov., a Mycobacterium fortuitum-group organism isolated from a patient with soft tissue infection and osteitis. Int J Syst Evol Microbiol. 2008;58(Pt 2):486–90.
Mediavilla-Gradolph MC, De Toro-Peinado I, Bermudez-Ruiz MP, Garcia-Martinez Mde L, Ortega-Torres M, Montiel Quezel-Guerraz N, et al. Use of MALDI-TOF MS for Identification of Nontuberculous Mycobacterium Species Isolated from Clinical Specimens. Biomed Res Int. 2015;2015:854078.
Nash KA, Brown-Elliott BA, Wallace Jr RJ. A novel gene, erm(41), confers inducible macrolide resistance to clinical isolates of Mycobacterium abscessus but is absent from Mycobacterium chelonae. Antimicrob Agents Chemother. 2009;53(4):1367–76.
Choi GE, Shin SJ, Won CJ, Min KN, Oh T, Hahn MY, et al. Macrolide treatment for Mycobacterium abscessus and Mycobacterium massiliense infection and inducible resistance. Am J Respir Crit Care Med. 2012;186(9):917–25.
Doan TL, Fung HB, Mehta D, Riska PF. Tigecycline: a glycylcycline antimicrobial agent. Clin Ther. 2006;28(8):1079–106.
Wallace Jr RJ, Brown-Elliott BA, Crist CJ, Mann L, Wilson RW. Comparison of the in vitro activity of the glycylcycline tigecycline (formerly GAR-936) with those of tetracycline, minocycline, and doxycycline against isolates of nontuberculous mycobacteria. Antimicrob Agents Chemother. 2002;46(10):3164–7.
Huang YC, Liu MF, Shen GH, Lin CF, Kao CC, Liu PY, et al. Clinical outcome of Mycobacterium abscessus infection and antimicrobial susceptibility testing. J Microbiol Immunol Infect. 2010;43(5):401–6.
Cavusoglu C, Gurpinar T, Ecemis T. Evaluation of antimicrobial susceptibilities of rapidly growing mycobacteria by Sensititre RAPMYCO panel. New Microbiol. 2012;35(1):73–6.
Huang CW, Chen JH, Hu ST, Huang WC, Lee YC, Huang CC, et al. Synergistic activities of tigecycline with clarithromycin or amikacin against rapidly growing mycobacteria in Taiwan. Int J Antimicrob Agents. 2013;41(3):218–23.
Kim SY, Kim CK, Bae IK, Jeong SH, Yim JJ, Jung JY, et al. The drug susceptibility profile and inducible resistance to macrolides of Mycobacterium abscessus and Mycobacterium massiliense in Korea. Diagn Microbiol Infect Dis. 2015;81(2):107–11.
Pang H, Li G, Zhao X, Liu H, Wan K, Yu P. Drug Susceptibility Testing of 31 Antimicrobial Agents on Rapidly Growing Mycobacteria Isolates from China. Biomed Res Int. 2015;2015:419392.
Horita Y, Maeda S, Kazumi Y, Doi N. In vitro susceptibility of Mycobacterium tuberculosis isolates to an oral carbapenem alone or in combination with beta-lactamase inhibitors. Antimicrob Agents Chemother. 2014;58(11):7010–4.
CLSI. Susceptibility testing of Mycobacteria, Nocardia, and other aerobic actinomycetes; Approved Standard–Second edition. CLSI document M24-A2. Wayne: Clinical and Laboratory Standards Institute; 2011.
Petrini B. Mycobacterium abscessus: an emerging rapid-growing potential pathogen. APMIS. 2006;114(5):319–28.
Wallace Jr RJ, Dukart G, Brown-Elliott BA, Griffith DE, Scerpella EG, Marshall B. Clinical experience in 52 patients with tigecycline-containing regimens for salvage treatment of Mycobacterium abscessus and Mycobacterium chelonae infections. J Antimicrob Chemother. 2014;69(7):1945–53.
Nash KA, Zhang Y, Brown-Elliott BA, Wallace Jr RJ. Molecular basis of intrinsic macrolide resistance in clinical isolates of Mycobacterium fortuitum. J Antimicrob Chemother. 2005;55(2):170–7.
Koh WJ, Jeon K, Lee NY, Kim BJ, Kook YH, Lee SH, et al. Clinical significance of differentiation of Mycobacterium massiliense from Mycobacterium abscessus. Am J Respir Crit Care Med. 2011;183(3):405–10.
Esteban J, Martin-de-Hijas NZ, Garcia-Almeida D, Bodas-Sanchez A, Gadea I, Fernandez-Roblas R. Prevalence of erm methylase genes in clinical isolates of non-pigmented, rapidly growing mycobacteria. Clin Microbiol Infect. 2009;15:919–23.
Acknowledgements
None.
Funding
This work was a self-funded project of the Department of Infectious Diseases, University of Tokyo.
Availability of data and materials
The data supporting the findings in this article are available upon request to the corresponding author.
Authors’ contributions
SH designed the study, performed data analysis, and wrote the manuscript. YO and MO participated in the laboratory analysis. YN and KM revised the manuscript critically for important intellectual content. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
There was no need for ethical approval because this study did not involve humans and animals.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hatakeyama, S., Ohama, Y., Okazaki, M. et al. Antimicrobial susceptibility testing of rapidly growing mycobacteria isolated in Japan. BMC Infect Dis 17, 197 (2017). https://doi.org/10.1186/s12879-017-2298-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-017-2298-8